Abstract
Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder and is associated with significant morbidity. We sought to present an updated systematic review of the literature on the accuracy of screening questionnaires for OSA against polysomnography (PSG) as the reference test. Using the main databases (including Medline, Cochrane Database of Systematic Reviews and Scopus) we used a combination of relevant keywords to filter studies published between January 2010 and April 2017. Population-based studies evaluating the accuracy of screening questionnaires for OSA against PSG were included in the review. Thirty-nine studies comprising 18 068 subjects were included. Four screening questionnaires for OSA had been validated in selected studies including the Berlin questionnaire (BQ), STOP-Bang Questionnaire (SBQ), STOP Questionnaire (SQ), and Epworth Sleepiness Scale (ESS). The sensitivity of SBQ in detecting mild (apnea-hypopnea index (AHI) ≥ 5 events/hour) and severe (AHI ≥ 30 events/hour) OSA was higher compared to other screening questionnaires (range from 81.08% to 97.55% and 69.2% to 98.7%, respectively). However, SQ had the highest sensitivity in predicting moderate OSA (AHI ≥ 15 events/hour; range = 41.3% to 100%). SQ and SBQ are reliable tools for screening OSA among sleep clinic patients. Although further validation studies on the screening abilities of these questionnaires on general populations are required.
Keywords: Obstructive Sleep Apnea, Surveys and Questionnaires, Validation, Sensitivity
Introduction
Obstructive sleep apnea (OSA) is the most common sleep breathing disorder and manifests as repeated apneas and hypopneas during sleep.1-3 OSA increases the risk of hypertension, glucose intolerance, cardiovascular, and cerebrovascular disorders.4-7 Untreated OSA is also associated with daytime sleepiness, cognitive dysfunction, and increased risk of automobile accidents.8-10 Polysomnography (PSG) is the gold standard for the diagnosis of OSA, but it is an expensive and time-consuming and requires trained personnel. PSG is a noninvasive technique that involves overnight monitoring of several physiological variables including electroencephalography, eye movements, and muscle tone as well as respiratory effort, airflow, and oxygen saturation.11 Therefore, different clinical models have been developed to evaluate patients at high risk for OSA.12-14 Screening questionnaires are simple, low-cost tools that can be used to prioritize patients eligible for PSG.
OSA screening questionnaires (OSA-SQs) were evaluated in surgical patients in a systematic review by Abrishami et al.15 In addition to being easy-to-use, the STOP and STOP-Bang questionnaires were found to have a higher methodological quality. Over the past few years, the accuracy of OSA-SQs has been an area of growing research interest and a number of studies have been published on the subject. This systematic review aimed to assess the accuracy of OSA-SQs including the Berlin questionnaire (BQ), STOP-Bang questionnaire (SBQ), STOP questionnaire (SQ), and Epworth Sleepiness Scale (ESS), based on an updated search of the literature.
We performed a literature search using Medline, Cochrane Database of Systematic Reviews, and Scopus for articles published between January 2010 and April 2017 using the following terms: OSA or OSAHS (obstructive sleep apnea hypopnea syndrome), hypopnea or hypopnoea, obstructive sleep apnea or sleep apnea syndrome and sensitivity, specificity, validity, or validation, sleep apnea questionnaires, and screening sleep apnea. The reference list of identified studies was also searched manually to detect eligible studies for inclusion. The flow diagram of study selection process is depicted in Figure 1.
Figure 1.
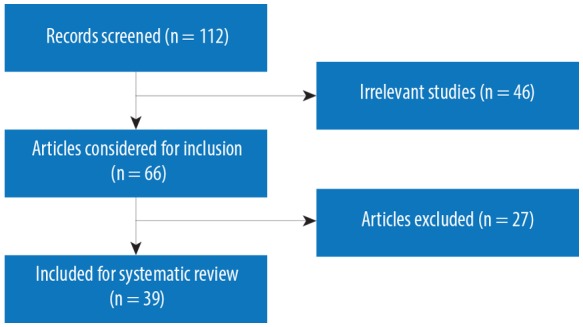
Flow diagram of study selection.
Two authors independently reviewed the titles and abstracts of the search results and disagreements were solved in group discussion. The studies had to meet the following criteria to be included: a) participant age > 18 years; b) the accuracy of the screening questionnaire had been assessed against various apnea-hypopnea indexes (AHI) or respiratory disturbance indexes (RDI) based on PSG as the gold standard; and c) studies were published in English. We also included studies if the validity of screening questionnaires was reported as a secondary outcome. Letters to the editor, review articles, case reports, and commentaries were excluded.
Two independent reviewers extracted the following information from each study that met the inclusion criteria: name of the first author, country and year of publication, study design, number of participants, age, gender, body mass index (BMI), neck circumference, validation tool (various types of PSG included), sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) for each AHI or RDI cut-off point including, AHI or RDI of ≥ 5 events/hour (mild OSA), ≥ 15 events/hour (moderate OSA), and ≥ 30 events/hour (severe OSA).
Thirty-nine studies qualified for inclusion in the present review,11,16-54 with sample sizes ranging from 30 to 4770. These studies were carried out in seven different geographic regions including, North America,17,18,20,22,27,38,47,50,52 West Asia,11,16,24,29,30,42,51,53 East Asia,25,26,28,32,36,49,54 Europe,19,31,37,39,43,45,46 South Asia,40,48 North Africa,21,44 and South America.23,33-35 The results of our analysis of the relevant studies are presented below for each of the four OSA-SQs.
Berlin questionnaire (BQ)
The BQ was developed in 1999 and includes three sections. The first section is about snoring, the second section is about daytime fatigue and sleepiness, and the last section is about medical history and anthropometric measures such as hypertension and BMI. If two or more categories were positive, the patient is considered high risk for OSA.55 BQ was evaluated in 29 out of the 39 eligible studies with a total 9444 subjects. Table 1 shows the characteristics and demographic information pertaining to these studies. Over half of the studies had < 150 subjects with the mean age ranging from 32 to 69.4 years. Only two studies28,46 assessed the BQ accuracy in the general population, while the subjects in 13 studies were all sleep clinic patients. The remaining 14 studies dealt with a mix of subjects or patient populations. Overnight PSG was used as the validation tool in 23 out of the 29 studies dealing with the BQ. Alternative methods in other studies were type II PSG (full in-home overnight PSG that records all items of standard PSG),17,25 type III PSG22,34,46 that typically measure between four and seven physiologic variables, including two respiratory variables (e.g., respiratory effort and airflow), a cardiac variable (e.g., heart rate or an electrocardiogram), and arterial oxyhemoglobin saturation via pulse oximetry, and daytime PSG.24
Table 1. Overview of studies included looking at the accuracy of screening questionnaires for obstructive sleep apnea against polysomnography (PSG) as the reference test.
| Study | No. of patients | Patient type | Age, years | Male, % | Body mass index, kg/m2 | Validation tool |
|---|---|---|---|---|---|---|
| Ong et al. 201036 | 314 | Sleep clinic patients | 46.8 ± 15 | 70.5 | 27.9 ± 6 | Lab PSG |
| Sagaspe et al. 201043 | 123 | Sleep clinic patients | 47 ± 13.2 | 67.5 | - | Lab PSG |
| Gantner et al. 201025 | 143 | Patients with high cardiovascular risk | 62.2 ± 7.6 | 58 | 26.6 ± 3.7 | Level II PSG |
| Silva et al. 201147 | 4770 | General population | 62.4 ± 10.3 | 51.5 | - | Level II PSG |
| Saleh et al. 201144 | 100 | Sleep clinic patients | 45.63 ± 9.67 | 51 | 36.34 ± 10.70 | Lab PSG |
| Srijithesh et al. 201148 | 121 | Acute stroke patients | 56.5 | - | Lab PSG | |
| Sforza et al. 201146 | 643 | General population | 65.6 ± 0.03 | 40.90 | 25.3 ± 0.2 | Level III PSG |
| Enciso et al. 201122 | 84 | Dental clinic patients | 54.93 ± 12.63 | 77.38 | 26.60 ± 3.74 | Two-night ambulatory somnography |
| Thurtell et al. 201150 | 30 | Patients with idiopathic intracranial hypertension | 32 ± 6.3 | 20 | 24.4 ± 4.1 | Lab PSG |
| Martinez et al. 201234 | 57 | Patients with angina complaints | 54 ± 6.9 | 46 | 23 ± 11 | Level III PSG |
| Hesselbacher et al. 201227 | 1897 | Sleep clinic patients | 53.84 ± 15 | 57.56 | 35.42 ± 5 | Lab PSG |
| El-Seyed et al. 201221 | 234 | Sleep clinic patients | 50.38 ± 11.29 | 58.5 | 37.77 ± 9.54 | Lab PSG |
| Firat et al. 201224 | 85 | Bus drivers | - | 100 | 29.1 ± 3.8 | Daytime PSG |
| Amra et al. 201311 | 157 | Sleep clinic patients | 52.3 ± 13.6 | 55.4 | 31.5 ± 6 | Lab PSG |
| Bouloukaki et al. 201319 | 189 | Clinic outpatients | 47 ± 13 | 61.9 | 35.0 ± 25.1 | Lab PSG |
| Kang et al. 201328 | 1305 | General population | 52.78 ± 16.55 | 47.7 | 22.81 ± 4.86 | Lab PSG |
| Best et al. 201317 | 82 | Patients with treatment resistant depression | 47.1 ± 9 | 26.83 | 33.34 ± 8.6 | Level II PSG |
| Yunus et al. 201354 | 150 | Clinic outpatients | 44.7 ± 11.5 | 64 | 36.3 ± 11.2 | Lab PSG |
| Boynton et al. 201320 | 219 | Sleep clinic patients | 46.3 ± 13.9 | 44.8 | 33.43 ± 8.76 | Lab PSG |
| Pereira et al. 201338 | 128 | Sleep clinic patients | 50 ± 12.3 | 65.62 | 31 ± 6.6 | Lab PSG |
| Scarlata et al. 201345 | 254 | Clinic outpatients | 65.8 ± 12.1 | 68.6 | 38.5 ± 7.7 | Lab PSG |
| Vana et al. 201352 | 47 | Sleep clinic patients | 46.4 ± 13.2 | 34 | 36.3 ± 9.2 | Lab PSG |
| Pataka et al. 201437 | 1853 | Sleep clinic patients | 52 ± 14 | 74.42 | 32.8 ± 7 | Lab PSG |
| Karakoc et al. 201429 | 217 | Surgical population | 42.5 ± 10.7 | 88 | 28.10 ± 4.1 | Lab PSG |
| Margallo et al. 201433 | 422 | Patients with resistant hypertension | 62.4 ± 9.9 | 31 | 31.2 ± 5.7 | Lab PSG |
| Ha et al. 201426 | 141 | Sleep clinic patients | 44.82 ± 12 | 81.6 | 25.33 ± 5 | Lab PSG |
| Ulasli et al. 201451 | 1450 | Sleep clinic patients | 50 ± 9.83 | 62.96 | 31.25 ± 9.09 | Lab PSG |
| Kim et al. 201532 | 592 | Sleep clinic patients | 47.8 ± 12.7 | 83.5 | 24.7 ± 3.5 | Lab PSG |
| Alhouqani et al. 201516 | 193 | Sleep clinic patients | 42.87 ± 11.83 | 77.7 | 34.90 ± 8.60 | Lab PSG |
| Sadeghniiat-Haghighi et al. 201542 | 603 | Sleep clinic patients | 45.8 ± 12.7 | 74.8 | 29.18 ± 5.9 | Lab PSG |
| Yuceege et al. 201553 | 433 | Sleep clinic patients | 47.5 ± 10.5 | 65.82 | 31.1 ± 5.6 | Lab PSG |
| Nunes et al. 201535 | 40 | Coronary artery bypass grafting patients | 56 ± 7 | 73 | 30 ± 4 | Lab PSG |
| Nunes et al. 201535 | 41 | Abdominal surgery patients | 56 ± 8 | 68 | 29 ± 5 | Lab PSG |
| Faria et al. 201523 | 91 | Patients with chronic obstructive pulmonary disease | 69.4 ± 9.6 | 63.7 | 23.6 ± 3.9 | Lab PSG |
| Popevic et al. 201639 | 100 | Commercial drivers | 43.4 ± 10.7 | 100 | 29.0 ± 5.7 | Lab PSG |
| Khaledi-Paveh et al. 201630 | 100 | Sleep clinic patients | 45.66 ± 11.83 | 60 | 29.5 ± 6.1 | Lab PSG |
| Kicinski et al. 201631 | 123 | Sleep clinic patients | 54.6 ± 11.1 | 66.40 | 33.5 ± 5.2 | Lab PSG |
| Tan et al. 201649 | 242 | General population | 48.3 ± 14 | 50.4 | 26.2 ± 5 | Level 3 PSG |
| Bhat et al. 201618 | 85 | Sleep clinic patients | 50.5 ± 12.6 | 70.6 | 32 ± 1.55 | Lab PSG/Level III PSG |
| Prasad et al. 201740 | 210 | Sleep clinic patients | 46.5 ± 13.7 | 72.9 | 31.9 ± 7.4 | Lab PSG |
Table 2 shows the BQ data for the sensitivity, specificity, PPV, and NPV for one or more AHI cut-off points as reported in the selected studies. The BQ highest sensitivity (97.3%) and NPV (95.4%) for the detection of OSA was found at AHI cutoffs ≥ 30 events/hour. However, the BQ had the highest detection specificity for moderate OSA (91.7%). Our analysis indicates a PPV ranging from 11.5% to 91% at AHI ≥ 5 events/hour.
Table 2. Predictive parameters of the screening questionnaires.
| Study | AHI ≥ 5 | AHI ≥ 15 | AHI ≥ 30 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity % | Specificity % |
PPV % | NPV % | Sensitivity % |
Specificity % |
PPV % | NPV % | Sensitivity % |
Specificity % | PPV % | NPV % | |
| Berlin | ||||||||||||
| Sagaspe et al. 201043 | 72 | 73 | 63 | 76 | 61 | 43 | 71 | 53 | 16 | |||
| Gantner et al. 201025 | - | - | - | - | 89 | 35 | 76 | 58 | 92 | 26 | 49 | 81 |
| Saleh et al. 201144 | 97 | 90 | 96 | 93 | - | - | - | - | - | - | - | - |
| Srijithesh et al. 201148 | 68.2 | 58.8 | 68.2 | 58.8 | - | - | - | - | - | - | - | - |
| Sforza et al. 201146 | - | - | - | - | 76.69 | 39.34 | 63.17 | 55.44 | - | - | - | - |
| Enciso et al. 201122 | - | - | - | - | 67.9 | 54.8 | 72 | 50 | - | - | - | - |
| Thurtell et al. 201150 | 83.3 | 58.3 | 75 | 70 | - | - | - | - | - | - | - | - |
| Martinez et al. 201234 | - | - | - | - | 72 | 50 | 53 | 70 | - | - | - | - |
| El-Seyed et al. 201221 | 95.07 | 25 | 92.79 | 33.33 | 95.48 | 7.41 | 87.11 | 20 | 97.3 | 10.71 | 74.23 | 60 |
| Firat et al. 201224 | - | - | - | - | 45.6 | 84.6 | 77.1 | 56.8 | - | - | - | - |
| Amra et al. 201311 | 84.0 | 61.5 | 96.0 | 25.8 | 87.9 | 36.7 | 75.3 | 58.0 | 87.8 | 26.5 | 51.5 | 70.9 |
| Bouloukaki et al. 201319 | 76 | 40 | 94 | 12 | 84 | 61 | 86 | 52 | 79 | 39 | 80 | 36 |
| Kang et al. 201328 | 69 | 83 | - | - | 89 | 63 | - | - | - | - | - | - |
| Best et al. 201317 | 25.0 | 85.4 | 56.5 | 60.0 | 24.5 | 91.7 | 35.5 | 93.3 | - | - | - | - |
| Yunus et al. 201354 | 92 | 17 | 97 | 29 | - | - | - | - | - | - | - | - |
| Pereira et al. 201338 | 86 | 25 | 91.7 | 15.8 | 91 | 28 | 73.4 | 57.9 | 89 | 18 | 45.9 | 68.4 |
| Pataka et al. 201437 | 71.8 | 17.2 | 11.5 | 80.2 | 78 | 18 | 16.5 | 80.4 | 90 | 28.5 | 56 | 74 |
| Karakoc et al. 201429 | 83.4 | 22.2 | 76.4 | 30.8 | 89.3 | 22.6 | 42.1 | 76.9 | - | - | - | - |
| Margallo et al. 201433 | 68 | 46 | 85 | 24 | 69 | 40 | 58 | 50 | 76 | 40 | 39 | 77 |
| Ha et al. 201426 | 75 | 30.29 | 83.17 | 28.21 | 75 | 32.14 | 62.38 | 46.15 | 80.39 | 32.58 | 40.59 | 74.36 |
| Ulasli et al. 201451 | 73.1 | 44.5 | - | - | 76.4 | 39.5 | - | - | 80.3 | 35.3 | - | - |
| Kim et al. 201532 | 71.5 | 32.0 | 84.3 | 18.0 | 75.5 | 35.4 | 62.1 | 50.6 | - | - | - | - |
| Yuceege et al. 201553 | - | - | - | - | 84.2 | 31.7 | 48.7 | 63.4 | - | - | - | - |
| Nunes et al. 201535 | - | - | - | - | 67 | 26 | 50 | 42 | - | - | - | - |
| Nunes et al. 201535 | - | - | - | - | 82 | 62 | 61 | 83 | - | - | - | - |
| Faria et al. 201523 | 40 | 68.4 | 25 | 81.2 | - | - | - | - | - | - | - | - |
| Popevic et al. 201639 | 50.9 | 86.0 | 82.9 | 56.9 | 78.3 | 77.9 | 51.4 | 92.3 | 75 | 70.4 | 25.7 | 95.4 |
| Khaledi-Paveh et al. 201630 | 77.3 | 23.1 | 68 | 22 | 58.5 | 45.7 | - | - | 30.8 | 80 | - | - |
| Kicinski et al. 201631 | - | - | - | - | 93.10 | 16.20 | 1.11 | 42 | - | - | - | - |
| Prasad et al. 201740 | 33.5 | 39.1 | 83 | 40 | 87.5 | 37.8 | 72.1 | 62.2 | 89.4 | 32.1 | 56.4 | 75.6 |
| STOP-Bang | ||||||||||||
| Ong et al. 201036 | 84.7 | 52.6 | 84.4 | 53.2 | 91.1 | 40.4 | 60.8 | 81.3 | 95.4 | 35.0 | 43.5 | 93.5 |
| Silva et al. 201147 | - | - | - | - | 87 | 43.3 | - | - | 70.4 | 59.5 | ||
| El-Seyed et al. 201221 | 97.55 | 26.32 | 93.43 | 50 | 97.74 | 3.7 | 86.93 | 20 | 98.65 | 5.36 | 73.37 | 60 |
| Firat et al. 201224 | - | - | - | - | 87 | 48.7 | 66.6 | 76 | - | - | - | - |
| Boynton et al. 201320 | 82.2 | 48.0 | 84.2 | 44.4 | 93.2 | 40.5 | 58.2 | 87.0 | 96.8 | 33.1 | 36.4 | 96.3 |
| Pereira et al. 201338 | 90 | 42 | 93.7 | 29.4 | 93 | 28 | 73.9 | 64.7 | 96 | 21 | 48.6 | 88.2 |
| Pataka et al. 201437 | 90 | 4.9 | 12.2 | 76.8 | 94 | 5.5 | 17 | 84 | 98.7 | 9.9 | 52.7 | 88.4 |
| Ha et al. 201426 | 81.08 | 57.14 | 88.24 | 43.24 | 85.71 | 45.45 | 70.59 | 67.57 | 86.27 | 34.09 | 43.14 | 81.08 |
| Alhouqani et al. 201516 | 90.24 | 31.03 | 88.10 | 36.00 | 96.75 | 30.00 | 70.83 | 84.00 | 97.70 | 21.70 | 50.60 | 92.00 |
| Kim et al. 201532 | 97.0 | 18.6 | 85.9 | 54.6 | 98.0 | 10.6 | 60.6 | 78.8 | - | - | - | - |
| Sadeghniiat-Haghighi et al. 201542 | 91.6 | 45.2 | 78.2 | 71.6 | 97.1 | 35.2 | 56.9 | 93.3 | 98 | 29.4 | 41.8 | 96.6 |
| Tan et al. 201649 | - | - | - | - | 66.2 | 74.7 | 50.6 | 85.0 | 69.2 | 67.1 | 20.2 | 94.8 |
| Prasad et al. 201740 | 89 | 43.5 | 84.9 | 52.6 | 93.4 | 39.2 | 73.8 | 76.3 | 96.2 | 32.1 | 58.1 | 89.5 |
| STOP | ||||||||||||
| Silva et al. 201147 | - | - | - | - | 62 | 56.3 | - | - | 68.8 | 59.5 | - | - |
| El-Seyed et al. 201221 | 91.67 | 25 | 92.57 | 22.73 | 94.35 | 25.93 | 89.3 | 41.18 | 95.95 | 19.64 | 72.55 | 64.71 |
| Firat et al. 201224 | - | - | - | - | 41.3 | 92.3 | 86.4 | 57.1 | - | - | - | - |
| Boynton et al. 201320 | 74.6 | 34.0 | 79.2 | 28.3 | 80.6 | 34.5 | 52.2 | 66.7 | 83.9 | 31.8 | 32.7 | 83.3 |
| Pataka et al. 201437 | 91.7 | 6.4 | 12.8 | 84 | 92.7 | 6.6 | 17.3 | 72 | 97 | 11 | 52.3 | 78.4 |
| Ha et al. 201426 | 74.77 | 50.00 | 85.57 | 33.33 | 76.19 | 40.00 | 65.98 | 52.38 | 80.39 | 36.36 | 42.27 | 76.19 |
| Sadeghniiat-Haghighi et al. 201542 | 86.3 | 46.5 | 81.9 | 54.8 | 91.1 | 37.1 | 61.5 | 79 | 94.1 | 30.7 | 40.2 | 91.1 |
| Nunes et al. 201535 | - | - | - | - | 100 | 5 | 54 | 100 | - | - | - | - |
| Nunes et al. 201535 | - | - | - | - | 88 | 13 | 42 | 60 | - | - | - | - |
| Prasad et al. 201740 | 87.8 | 43.5 | 84.7 | 50 | 91.9 | 39.2 | 73.5 | 72.5 | 95.2 | 33 | 58.2 | 87.5 |
| Epworth Sleepiness Scale | ||||||||||||
| Silva et al. 201147 | - | - | - | - | 39 | 71.4 | 46.1 | 70.4 | - | - | ||
| Hesselbacher et al. 201227 | - | - | - | - | 54 | 57 | 64 | 47 | - | - | - | - |
| El-Seyed et al. 201221 | 72.55 | 75 | 96.73 | 21.13 | 75.71 | 48.15 | 90.54 | 23.23 | 79.73 | 46.43 | 79.73 | 46.43 |
| Scarlata et al. 201345 | - | - | - | - | - | - | - | - | - | - | - | - |
| Vana et al. 201352 | 31.3 | 53.3 | 58.8 | 26.7 | - | - | - | - | - | - | - | - |
| Pataka et al. 201437 | 33.3 | 50.6 | 9.1 | 83.6 | 44.5 | 52.1 | 17 | 81 | 57 | 62.4 | 59 | 60 |
| Ulasli et al. 201451 | 46.9 | 60 | - | - | 49.9 | 61.1 | - | - | 52.8 | 58.2 | - | - |
| Faria et al. 201523 | 60 | 73.7 | 37.5 | 87.5 | - | - | - | - | - | - | - | - |
| Kicinski et al. 201631 | - | - | - | - | 53.20 | 58.80 | 1.90 | 79 | - | - | - | - |
| Bhat et al. 201618 | - | - | - | - | 46.2 | 65.2 | 75 | 34.9 | - | - | - | - |
| Prasad et al. 201740 | 55.5 | 67.4 | 85.9 | 29.8 | 59.6 | 66.2 | 76.4 | 47.1 | 66.4 | 65.1 | 65.1 | 66.4 |
AHI: apnea-hypopnea index; PPV: positive predictive value; NPV: negative predictive value.
STOP-Bang questionnaire (SBQ)
The SBQ includes four subjective (STOP: Snoring, tiredness, observed apnea, and high blood pressure) and four demographics items (BANG: BMI,56 Age, Neck circumference, Gender). A score of 5–8 is categorized as high risk for OSA.57
For the SBQ, we included 13 studies with a total 9584 subjects and sample sizes ranging from 85 to 4770. The studies mostly included sleep clinic patients with an age range of 42.8 to 62.4 years old [Table 1]. Overnight laboratory PSG was used as the validation tool in 10 studies.24,47,49 The highest sensitivity and NPV were reported at AHI thresholds of ≥ 30 events/hour. The PPV value ranged between 12.2% and 93.7% at AHI cutoffs ≥ 5 events/hour. The SBQ showed the highest specificity (74.7%) in detecting moderate OSA [Table 2].
STOP Questionnaire (SQ)
The SQ is a concise and easy-to-use screening tool for OSA with high sensitivity. SQ can classify patients as being at high risk of having OSA if they answer yes to two or more questions.57 SQ was evaluated in nine studies (8196 subjects) of which six studies were carried out on sleep clinic patients and three on the general, community population,47 surgical patients,35 and bus drivers.24 The number of subjects in the studies varied from 40 to 4770 and the mean age was 44.8–62.4 years. Two studies used type II and daytime PSG for validation,24,47 while the others used overnight laboratory PSG. Our review indicates that the SQ had the highest prediction sensitivity (100%), specificity (92.3%), and NPV (100%) in the case of moderate OSA, while in the case of mild OSA the PPV ranged from 12.8% to 92.5% [Table 2].
Epworth Sleepiness Scale (ESS)
The ESS is an eight-item questionnaire to measure daytime sleepiness; it uses a four-point Likert response format (0–3), and the score ranges from 0 to 24. An ESS score ≥ 11 indicates excessive daytime sleepiness and high risk for OSA.58 Eleven of the 39 studies investigated the accuracy of ESS with a total of 11 014 subjects. The sample size in the 11 studies ranged from 47 to 4770 with an average age between 46.4 and 69.4 years. Eight of the 11 studies were conducted on sleep clinic patients, while the remaining three studies were carried out on respiratory patients,23 the general population,47 and clinic outpatients.45 The laboratory PSG was used by the majority of the reviewed studies [Table 1]. The highest ESS sensitivity was observed at AHI ≥ 30 events/hour and ranged between 46.1% and 79.73%. However, the highest values for specificity (75%), NPV (87.5%), and PPV (96.7%) were found in mild OSA with a decreasing trend from mild to severe OSA [Table 2].
Discussion
Sleep apnea is a common and potentially serious disorder in which breathing stops and repeatedly restarts during sleep. Hundreds of such breathing interruptions can occur over the course of a single night with each interruption lasting 10 to 20 seconds. Following each of the long apneic periods, the individual is jolted out of the normal sleep phase - the sleep rhythm is disrupted and the individual suffers from fatigue and daytime sleepiness. Other indicative signs of serious sleep apnea include long apneic periods (> 15 seconds), loud snoring, choking or gasping during sleep, irritability, headache, depression, and nightmares. If untreated, sleep apnea can lead to serious disorders including obesity, diabetes, hypertension, and stroke. There are three main types of sleep apnea depending on their cause. The most common variety is OSA, which results from upper airway obstruction because of hypotonia and collapse of the posterior pharyngeal muscles. OSA is characterized by cyclic loud snoring, which is a common problem in obese individuals and patients with endocrine disorders such as hypothyroidism and acromegaly. A common cause of OSA in children is hypertrophy of the tonsils and/or the adenoids. Central sleep apnea results from the reduced central respiratory drive. Complex sleep apnea is a combination of both obstructive and central apneas.59
In light of the profound impact of OSA on the health and quality of life,5,18,40 it is essential that patients are adequately screened to receive the necessary medical care. It is estimated that over 80% of people with moderate to severe OSA remain undiagnosed.60 Thus, a screening tool is necessary to stratify patients based on their clinical symptoms and anthropometric risk factors.
Some easy-to-use questionnaires have been developed as low-cost alternatives to PSG for detecting OSA. In this review, we assessed the accuracy of four self-reported OSA-SQs against PSG as the reference test. The SBQ had the highest sensitivity for the prediction of mild and severe OSA (97.55% and 98.7%, respectively). However, the BQ showed the highest specificity for the detection of mild and severe OSA (90% and 80%, respectively). Compared to other questionnaires, the SQ had the highest sensitivity (100%) and specificity (92.3%) for predicting moderate OSA. The validity of our results for the general population may be questioned based on the fact that most of the subjects in the studies we reviewed were sleep clinic patients where the prevalence of OSA is relatively high. In addition, there is no standard definition of OSA unifying the various validation studies. Features of an appropriate screening questionnaire vary according to the population being surveyed. For example, cultural differences in urban and rural populations require the questionnaire is modified according to those being surveyed. However, it must be noted that it was not our objective of this review. Diagnosis of true positive OSA patients in a clinical setting using a questionnaire with high sensitivity minimizes negative health consequences and avoids unnecessary and costly diagnostic tests. PSG, the gold standard for OSA diagnosis, is an expensive and time-demanding procedure. Therefore, it is necessary to decrease the number of false-positive subjects in the general population using a screening tool with high specificity. An effective screening tool must also have a high sensitivity to minimize the number of false negatives.
There was no standard definition for OSA in various studies that investigated the validity of OSA screening questionnaires against PSG. A recent meta-analysis indicated that the BQ has a moderate sensitivity and specificity in the general population for detecting hypopnea defined as a 3% oxygen desaturation. However, its sensitivity decreased when the hypopnea definition of 4% oxygen desaturation was applied.39 Based on these observations it is clear that the definition of OSA significantly affects the accuracy of validation studies.
Therefore, it is necessary to test the validity of various OSA-SQs in the general population against the reference standard PSG. Because sleep clinic patients constituted the majority of the subjects in the reviewed studies, it is not possible to extend our conclusions to the general population.
Conclusion
SBQ and SQ are appropriate screening tools to determine OSA in sleep clinic patients. Further validation studies designed specifically for the general population are necessary.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
References
- 1.Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 2008. Aug;31(8):1079-1085. [PMC free article] [PubMed] [Google Scholar]
- 2.Young T, Finn L, Peppard PE, Szklo-Coxe M, Austin D, Nieto FJ, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 2008. Aug;31(8):1071-1078. [PMC free article] [PubMed] [Google Scholar]
- 3.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 2002. May;165(9):1217-1239. 10.1164/rccm.2109080 [DOI] [PubMed] [Google Scholar]
- 4.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 2000. May;342(19):1378-1384. 10.1056/NEJM200005113421901 [DOI] [PubMed] [Google Scholar]
- 5.Punjabi NM, Ahmed MM, Polotsky VY, Beamer BA, O’Donnell CP. Sleep-disordered breathing, glucose intolerance, and insulin resistance. Respir Physiol Neurobiol 2003. Jul;136(2-3):167-178. 10.1016/S1569-9048(03)00079-X [DOI] [PubMed] [Google Scholar]
- 6.Redline S, Yenokyan G, Gottlieb DJ, Shahar E, O’Connor GT, Resnick HE, et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med 2010. Jul;182(2):269-277. 10.1164/rccm.200911-1746OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Nieto FJ, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med 2001. Jan;163(1):19-25. 10.1164/ajrccm.163.1.2001008 [DOI] [PubMed] [Google Scholar]
- 8.George CF, Boudreau AC, Smiley A. Effects of nasal CPAP on simulated driving performance in patients with obstructive sleep apnoea. Thorax 1997. Jul;52(7):648-653. 10.1136/thx.52.7.648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pichel F, Zamarrón C, Magán F, Rodríguez JR. Sustained attention measurements in obstructive sleep apnea and risk of traffic accidents. Respir Med 2006. Jun;100(6):1020-1027. 10.1016/j.rmed.2005.09.036 [DOI] [PubMed] [Google Scholar]
- 10.Ruehland WR, Rochford PD, O’Donoghue FJ, Pierce RJ, Singh P, Thornton AT. The new AASM criteria for scoring hypopneas: impact on the apnea hypopnea index. Sleep 2009. Feb;32(2):150-157. 10.1093/sleep/32.2.150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amra B, Nouranian E, Golshan M, Fietze I, Penzel T. Validation of the persian version of berlin sleep questionnaire for diagnosing obstructive sleep apnea. Int J Prev Med 2013. Mar;4(3):334-339. [PMC free article] [PubMed] [Google Scholar]
- 12.Kushida CA, Littner MR, Morgenthaler T, Alessi CA, Bailey D, Coleman J, Jr, et al. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep 2005. Apr;28(4):499-521. 10.1093/sleep/28.4.499 [DOI] [PubMed] [Google Scholar]
- 13.Ramachandran SK, Josephs LA. A meta-analysis of clinical screening tests for obstructive sleep apnea. Anesthesiology 2009. Apr;110(4):928-939. 10.1097/ALN.0b013e31819c47b6 [DOI] [PubMed] [Google Scholar]
- 14.Manzar MD, Moiz JA, Zannat W, Spence DW, Pandi-Perumal SR, Hussain ME, Ahmed S. BaHammam Validity of the Pittsburgh Sleep Quality Index in Indian University Students. Oman Med J 2015. May;30(3):193-202. 10.5001/omj.2015.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abrishami A, Khajehdehi A, Chung F. A systematic review of screening questionnaires for obstructive sleep apnea. Can J Anaesth 2010. May;57(5):423-438. 10.1007/s12630-010-9280-x [DOI] [PubMed] [Google Scholar]
- 16.Alhouqani S, Al Manhali M, Al Essa A, Al-Houqani M. Evaluation of the Arabic version of STOP-Bang questionnaire as a screening tool for obstructive sleep apnea. Sleep Breath 2015. Dec;19(4):1235-1240. 10.1007/s11325-015-1150-x [DOI] [PubMed] [Google Scholar]
- 17.Best MW, Fitzpatrick M, Milev R, Bowie CR, Jokic R. Utility of the Berlin questionnaire for predicting obstructive sleep apnea in individuals with treatment-resistant depression. Sleep Breath 2013. Dec;17(4):1221-1227. 10.1007/s11325-013-0827-2 [DOI] [PubMed] [Google Scholar]
- 18.Bhat S, Upadhyay H, DeBari VA, Ahmad M, Polos PG, Chokroverty S. The utility of patient-completed and partner-completed Epworth Sleepiness Scale scores in the evaluation of obstructive sleep apnea. Sleep Breath 2016. Dec;20(4):1347-1354. 10.1007/s11325-016-1370-8 [DOI] [PubMed] [Google Scholar]
- 19.Bouloukaki I, Komninos ID, Mermigkis C, Micheli K, Komninou M, Moniaki V, et al. Translation and validation of Berlin questionnaire in primary health care in Greece. BMC Pulm Med 2013. Jan;13:6. 10.1186/1471-2466-13-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boynton G, Vahabzadeh A, Hammoud S, Ruzicka DL, Chervin RD. Validation of the STOP-BANG Questionnaire among Patients Referred for Suspected Obstructive Sleep Apnea. J Sleep Disord Treat Care 2013. Sep;2(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.El-Sayed IH. Comparison of four sleep questionnaires for screening obstructive sleep apnea. Egyptian Journal of Chest Diseases and Tuberculosis. 2012;61(4):433-441 . 10.1016/j.ejcdt.2012.07.003 [DOI] [Google Scholar]
- 22.Enciso R, Clark GT. Comparing the Berlin and the ARES questionnaire to identify patients with obstructive sleep apnea in a dental setting. Sleep Breath 2011. Jan;15(1):83-89. 10.1007/s11325-010-0328-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Faria AC, da Costa CH, Rufino R. Sleep Apnea Clinical Score, Berlin Questionnaire, or Epworth Sleepiness Scale: which is the best obstructive sleep apnea predictor in patients with COPD? Int J Gen Med 2015. Aug;8:275-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Firat H, Yuceege M, Demir A, Ardic S. Comparison of four established questionnaires to identify highway bus drivers at risk for obstructive sleep apnea in Turkey. Sleep Biol Rhythms 2012;10(3):231-236 . 10.1111/j.1479-8425.2012.00566.x [DOI] [Google Scholar]
- 25.Gantner D, Ge JY, Li LH, Antic N, Windler S, Wong K, et al. Diagnostic accuracy of a questionnaire and simple home monitoring device in detecting obstructive sleep apnoea in a Chinese population at high cardiovascular risk. Respirology 2010. Aug;15(6):952-960. 10.1111/j.1440-1843.2010.01797.x [DOI] [PubMed] [Google Scholar]
- 26.Ha SC, Lee DL, Abdullah VJ, van Hasselt CA. Evaluation and validation of four translated Chinese questionnaires for obstructive sleep apnea patients in Hong Kong. Sleep Breath 2014. Dec;18(4):715-721. 10.1007/s11325-013-0889-1 [DOI] [PubMed] [Google Scholar]
- 27.Hesselbacher S, Subramanian S, Allen J, Surani S, Surani S. Body mass index, gender, and ethnic variations alter the clinical implications of the epworth sleepiness scale in patients with suspected obstructive sleep apnea. Open Respir Med J 2012;6:20-27. 10.2174/1874306401206010020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kang K, Park KS, Kim JE, Kim SW, Kim YT, Kim JS, et al. Usefulness of the Berlin Questionnaire to identify patients at high risk for obstructive sleep apnea: a population-based door-to-door study. Sleep Breath 2013. May;17(2):803-810. 10.1007/s11325-012-0767-2 [DOI] [PubMed] [Google Scholar]
- 29.Karakoc O, Akcam T, Genc H, Yetkin S, Piskin B, Gerek M. Use of the Berlin Questionnaire to screen at-risk patients for obstructive sleep apnea. B-ENT 2014;10(1):21-25. [PubMed] [Google Scholar]
- 30.Khaledi-Paveh B, Khazaie H, Nasouri M, Ghadami MR, Tahmasian M. Evaluation of Berlin Questionnaire Validity for Sleep Apnea Risk in Sleep Clinic Populations. Basic Clin Neurosci 2016. Jan;7(1):43-48. [PMC free article] [PubMed] [Google Scholar]
- 31.Kiciński P, Przybylska-Kuć SM, Tatara K, Dybała A, Zakrzewski M, Mysliński W, et al. Reliability of the Epworth Sleepiness Scale and the Berlin Questionnaire for screening obstructive sleep apnea syndrome in the context of the examination of candidates for drivers. Med Pr 2016. Dec;67(6):721-728. 10.13075/mp.5893.00494 [DOI] [PubMed] [Google Scholar]
- 32.Kim B, Lee EM, Chung YS, Kim WS, Lee SA. The utility of three screening questionnaires for obstructive sleep apnea in a sleep clinic setting. Yonsei Med J 2015. May;56(3):684-690. 10.3349/ymj.2015.56.3.684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Margallo VS, Muxfeldt ES, Guimarães GM, Salles GF. Diagnostic accuracy of the Berlin questionnaire in detecting obstructive sleep apnea in patients with resistant hypertension. J Hypertens 2014. Oct;32(10):2030-2036, discussion 2037. 10.1097/HJH.0000000000000297 [DOI] [PubMed] [Google Scholar]
- 34.Martinez D, da Silva RP, Klein C, Fiori CZ, Massierer D, Cassol CM, et al. High risk for sleep apnea in the Berlin questionnaire and coronary artery disease. Sleep Breath 2012. Mar;16(1):89-94. 10.1007/s11325-010-0460-2 [DOI] [PubMed] [Google Scholar]
- 35.Nunes FS, Danzi-Soares NJ, Genta PR, Drager LF, Cesar LA, Lorenzi-Filho G. Critical evaluation of screening questionnaires for obstructive sleep apnea in patients undergoing coronary artery bypass grafting and abdominal surgery. Sleep Breath 2015. Mar;19(1):115-122. 10.1007/s11325-014-0971-3 [DOI] [PubMed] [Google Scholar]
- 36.Ong TH, Raudha S, Fook-Chong S, Lew N, Hsu AA. Simplifying STOP-BANG: use of a simple questionnaire to screen for OSA in an Asian population. Sleep Breath 2010. Dec;14(4):371-376. 10.1007/s11325-010-0350-7 [DOI] [PubMed] [Google Scholar]
- 37.Pataka A, Daskalopoulou E, Kalamaras G, Fekete Passa K, Argyropoulou P. Evaluation of five different questionnaires for assessing sleep apnea syndrome in a sleep clinic. Sleep Med 2014. Jul;15(7):776-781. 10.1016/j.sleep.2014.03.012 [DOI] [PubMed] [Google Scholar]
- 38.Pereira EJ, Driver HS, Stewart SC, Fitzpatrick MF. Comparing a combination of validated questionnaires and level III portable monitor with polysomnography to diagnose and exclude sleep apnea. J Clin Sleep Med 2013. Dec;9(12):1259-1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Popević MB, Milovanović A, Nagorni-Obradović L, Nešić D, Milovanović J, Milovanović AP. Screening commercial drivers for obstructive sleep apnea: translation and validation of Serbian version of Berlin Questionnaire. Qual Life Res 2016. Feb;25(2):343-349. 10.1007/s11136-015-1087-3 [DOI] [PubMed] [Google Scholar]
- 40.Prasad KT, Sehgal IS, Agarwal R, Nath Aggarwal A, Behera D, Dhooria S. Assessing the likelihood of obstructive sleep apnea: a comparison of nine screening questionnaires. Sleep Breath 2017. Dec;21(4):909-917. 10.1007/s11325-017-1495-4 [DOI] [PubMed] [Google Scholar]
- 41.Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O’Connor GT, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med 2009. Aug;6(8):e1000132. 10.1371/journal.pmed.1000132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sadeghniiat-Haghighi K, Montazeri A, Khajeh-Mehrizi A, Ghajarzadeh M, Alemohammad ZB, Aminian O, et al. The STOP-BANG questionnaire: reliability and validity of the Persian version in sleep clinic population. Qual Life Res 2015. Aug;24(8):2025-2030. 10.1007/s11136-015-0923-9 [DOI] [PubMed] [Google Scholar]
- 43.Sagaspe P, Leger D, Taillard J, Bayon V, Chaumet G, Philip P. Might the Berlin Sleep Questionnaire applied to bed partners be used to screen sleep apneic patients? Sleep Med 2010. May;11(5):479-483. 10.1016/j.sleep.2010.01.007 [DOI] [PubMed] [Google Scholar]
- 44.Saleh AB, Ahmad MA, Awadalla NJ. Development of Arabic version of Berlin questionnaire to identify obstructive sleep apnea at risk patients. Ann Thorac Med 2011. Oct;6(4):212-216. 10.4103/1817-1737.84775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Scarlata S, Pedone C, Curcio G, Cortese L, Chiurco D, Fontana D, et al. Pre-polysomnographic assessment using the Pittsburgh Sleep Quality Index questionnaire is not useful in identifying people at higher risk for obstructive sleep apnea. J Med Screen 2013. Dec;20(4):220-226. 10.1177/0969141313511591 [DOI] [PubMed] [Google Scholar]
- 46.Sforza E, Chouchou F, Pichot V, Herrmann F, Barthélémy JC, Roche F. Is the Berlin questionnaire a useful tool to diagnose obstructive sleep apnea in the elderly? Sleep Med 2011. Feb;12(2):142-146. 10.1016/j.sleep.2010.09.004 [DOI] [PubMed] [Google Scholar]
- 47.Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J Clin Sleep Med 2011. Oct;7(5):467-472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Srijithesh PR, Shukla G, Srivastav A, Goyal V, Singh S, Behari M. Validity of the Berlin Questionnaire in identifying obstructive sleep apnea syndrome when administered to the informants of stroke patients. J Clin Neurosci 2011. Mar;18(3):340-343. 10.1016/j.jocn.2010.04.048 [DOI] [PubMed] [Google Scholar]
- 49.Tan A, Yin JD, Tan LW, van Dam RM, Cheung YY, Lee CH. Predicting obstructive sleep apnea using the STOP-Bang questionnaire in the general population. Sleep Med 2016. Nov - Dec;27-28:66-71. 10.1016/j.sleep.2016.06.034 [DOI] [PubMed] [Google Scholar]
- 50.Thurtell MJ, Bruce BB, Rye DB, Newman NJ, Biousse V. The Berlin questionnaire screens for obstructive sleep apnea in idiopathic intracranial hypertension. J Neuroophthalmol 2011. Dec;31(4):316-319. 10.1097/WNO.0b013e31821a4d54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ulasli SS, Gunay E, Koyuncu T, Akar O, Halici B, Ulu S, et al. Predictive value of Berlin Questionnaire and Epworth Sleepiness Scale for obstructive sleep apnea in a sleep clinic population. Clin Respir J 2014. Jul;8(3):292-296. 10.1111/crj.12070 [DOI] [PubMed] [Google Scholar]
- 52.Vana KD, Silva GE, Goldberg R. Predictive abilities of the STOP-Bang and Epworth Sleepiness Scale in identifying sleep clinic patients at high risk for obstructive sleep apnea. Res Nurs Health 2013. Feb;36(1):84-94. 10.1002/nur.21512 [DOI] [PubMed] [Google Scholar]
- 53.Yüceege M, Fırat H, Sever Ö, Demir A, Ardıç S. The effect of adding gender item to Berlin Questionnaire in determining obstructive sleep apnea in sleep clinics. Ann Thorac Med 2015. Jan-Mar;10(1):25-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yunus A, Seet W, Mohamad Adam B, Haniff J. Validation of the Malay version of Berlin questionaire to identify Malaysian patients for obstructive sleep apnea. Malays Fam Physician 2013. Apr;8(1):5-11. [PMC free article] [PubMed] [Google Scholar]
- 55.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 1999. Oct;131(7):485-491. 10.7326/0003-4819-131-7-199910050-00002 [DOI] [PubMed] [Google Scholar]
- 56.Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 2000. Apr;283(14):1829-1836. 10.1001/jama.283.14.1829 [DOI] [PubMed] [Google Scholar]
- 57.Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 2008. May;108(5):812-821. 10.1097/ALN.0b013e31816d83e4 [DOI] [PubMed] [Google Scholar]
- 58.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991. Dec;14(6):540-545. 10.1093/sleep/14.6.540 [DOI] [PubMed] [Google Scholar]
- 59.Peracchia C, Anaizi NH. Control of breathing. Lung function in health and disease. 1st ed. 2014. p. 197-214. [Google Scholar]
- 60.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 1993. Apr;328(17):1230-1235. 10.1056/NEJM199304293281704 [DOI] [PubMed] [Google Scholar]


