Abstract
Thrombotic storm (TS) is a rare disease, especially with thrombus in the heart of pediatric patient. We present a case of a 4-year-old boy, who was diagnosed with TS during his first hospitalization due to lower extremity deep venous thrombosis, pulmonary embolism, and thrombosis of the inferior vena cava, cerebral, left internal jugular, portal, renal, and iliac veins. He was eventually prescribed with rivaroxaban to control thrombosis after 30 days of successive use of low-molecular-weight heparin, unfractionated heparin, and warfarin, which were demonstrating little effect on preventing thrombosis, and the patient was intolerant to argatroban. While his lupus anticoagulant ratio was slightly above the normal range and no other potential causes such as congenital thrombophilia, severe infection, malignancy, and trauma were confirmed, we suspected antiphospholipid antibody syndrome and prescribed glucocorticoid and rituximab to control the disease. After 36 days of admission, ultrasonography showed recanalization of the former thrombus. One month after discharge, a tumor embolus resembling a mass emerged in his right atrium under effective anticoagulant therapy. During his second admission, he underwent surgical thrombectomy, and pathological examination confirmed the mass to be a platelet-rich thrombus rather than tumor embolus or infection. Considering the suspected antiphospholipid antibody syndrome as the cause of the TS, we prescribed aspirin combined with rivaroxaban to prevent thrombosis. In this case, surgery and pathology shed light on the type of thrombus that emerged from the inferior vena cava and traveled to the heart, which is the possible potential cause of TS. It also changed our therapeutic strategy to antiplatelet therapy combined with anticoagulant therapy to control the disease.
Keywords: cardiac, thrombosis, thrombotic storm
Introduction
Thrombotic storm (TS) is a rare disease that manifests through hypercoagulable clinical conditions with at least two arterial and/or venous thromboembolic events, typically at unusual sites.1 It progresses rapidly, and depending on the affected blood vessels, it often leads to severe complications.2 TS has multiple causes, which make it difficult to diagnose the primary disease.1 Some patients have to face cardiopulmonary insufficiency and even amputation during follow-up.3 In China, data on children with TS are limited. Given the scarce and life-threatening traits of this disease, it is critical to recognize the disease and to determine suitable management. We describe a patient diagnosed with TS, which was highly suspected to be caused by antiphospholipid antibody syndrome (APS), who had a thrombus that emerged in the right atrium (RA).
Case report
A 4-year-old boy diagnosed with TS was admitted to our hospital again, as echocardiography showed an isoechoic to hyperechoic mass that emerged from his RA during follow-up visit. One month prior, the boy was initially admitted to our hospital with symptoms of intermittent headache and vomiting for 20 days and left lower limb swelling for 1 day. Ultrasonography and magnetic resonance imaging (MRI) showed thrombi in the cerebral venous sinus, inferior vena cava (IVC), left internal jugular, portal, left renal, common iliac, internal iliac, and external iliac veins. Echocardiography showed an enlarged right heart, pulmonary hypertension, and pulmonary embolisms (PEs). The enhanced lung computed tomography (CT) scan showed bilateral pneumonia and multiple PEs.
During his first hospitalization, the patient was examined for conditions which could drive the pathogenesis of thrombosis, such as factor V Leiden mutation, protein C and S deficiency, APS, severe infection, trauma, systemic lupus erythematosus, and malignancy. The evaluation showed that only his lupus anticoagulant (LA) ratio was slightly positive (1.22–1.53), whereas other indicators (e.g. protein C, protein S, platelet factor4 (PF4)-heparin antibodies, tumor markers, bone marrow cytology, extractable nuclear antigen, anticardiolipin antibodies, and anti-β2-glycoprotein I antibodies) were within the normal range. Besides, his family history of thrombosis was negative. Severe infection and history of trauma were both excluded. Thus, a suspected diagnosis of APS was made according to the onset age, major thrombotic event, and positive LA ratio.
He was prescribed low-molecular-weight heparin, unfractionated heparin, and warfarin successively, by which the disease progress was not slowed down as expected after 30 days of treatment. Notably, the international normalized ratio had already reached 2.89 after warfarin therapy (0.09 mg/kg/day) for 4 days; while considering that the thrombus in the IVC was reaching the RA within a length of 1 cm, we used argatroban, a small molecule direct thrombin inhibitor, to prevent disease from deterioration, with the informed consent from patient’s parents. However, it aroused anaphylactic shock and disseminated intravascular coagulation 2 h later. We discontinued argatroban and prescribed antiallergic drugs, prothrombin complex concentrates, and plasma to stabilize the condition. In an attempt to inhibit thrombosis, we finally chose rivaroxaban after obtaining the parent’s written informed consent, an active direct factor Xa inhibitor, which is taken by mouth, which was well tolerated by the patient. Apart from the anticoagulants, he received immunosuppressors (a glucocorticoid and rituximab), plasma transfusion, and antibiotics as well. After 36 days of admission, ultrasonography showed thrombus recanalization in the IVC, left renal vein, and left internal jugular vein. The boy was discharged from the hospital and followed up in an outpatient clinic. During a follow-up visit, his echocardiography showed an isoechoic to hyperechoic mass in the RA (Figure 1). The mass, which was 47.1 mm × 21.8 mm, from the IVC to the RA, passed through the tricuspid valve into the right ventricle (RV) in diastole while the former thrombi in other vessels had already vanished. To determine the properties of the mass, we performed ultrasound, contrast-enhanced CT, MRI, positron emission tomography–CT, and assessed tumor markers; however, all results were negative. The bone marrow smear, peripheral blood smear, and bone marrow myelodysplasia/myeloproliferative neoplasm test results were negative.
Figure 1.
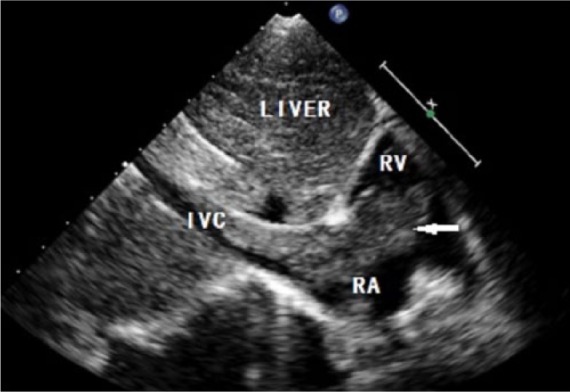
Echocardiography showing an isoechoic to hyperechoic mass (arrow) emerged from the IVC to the RA, passing through the tricuspid valve into the RV in diastole. RA: right atrium; RV: right ventricle; IVC: inferior vena cava.
Physicians from hematology, oncology, cardiac surgery, and the intensive care unit consulted and decided to perform a cardiac operation to excise the thrombus. After receiving an informed consent from the patient’s guardian, cardiac surgeons performed the operation, during which they found a huge embolus (40 mm × 30 mm), which was reddish, hard, and fragile; it could be seen in the RA, was connected to the IVC, and invaded the tricuspid valve. The surgeons removed the embolus and cleaned the IVC.
With regard to the pathological findings, light microscopic examination showed a platelet-rich thrombus, scattered with lymphocytes, neutrophils, and eosinophils, without tumor components (Figure 2). Based on the histopathological features, as well as the consideration of APS as the cause of the disease, we administered antiplatelet therapy to prevent recurrence of thrombosis.
Figure 2.

Light microscopic examination showing platelet-rich thrombus, scattered with lymphocytes, neutrophils, and eosinophils, without tumor components.
Since then, the patient has taken aspirin combined with rivaroxaban for more than 1 year. During follow-up, we found no new thromboses by Doppler ultrasonography. Echocardiography showed no abnormal mass within the heart chamber or IVC. The coagulation function test indicated prothrombin time of 12.0–12.2 s, fibrinogen of 2.88–3.77 g/L, activated partial thromboplastin time of 32.4–36.9 s, d-dimer of 0.05 mg/L, and antithrombin-III of 100%−108%. The LA turned negative 6 months after surgery, with other indicators related to APS remained negative. No aggravation or recurrence occurred during the patient’s follow-up period.
Discussion
Kitchens et al.1 suggested that TS has certain clinical characteristics; for example, it affects younger individuals, presents as two or more arterial or venous thromboemboli, has an unusual location, is progressive or has a recent unexplained recurrence, is refractory to acute therapy, has an atypical response to therapy, and so on.1 Triggers of TS include infection,4 inflammation, trauma, medications, and overlapping diseases such as APS. Kitchens suggested that TS is a phenomenon of which “thrombosis begets thrombosis.”4 Studies have indicated that antiphospholipid antibody is either absent or present at a low level in children with TS during the acute course of the disease, but children become positive for this antibody later during the follow-up period.5 Our patient’s symptoms manifested as generalized phlebothrombosis combined with PE during his first hospitalization; thus, he was diagnosed as having TS with suspected APS. With effective treatment of anticoagulation and immunosuppression therapy, the enormous mass with its tumor embolus–like morphology emerged from the RA less than 1 month after recanalization of the former thrombus, which indicated that the primary disease may be malignant, although there was insufficient evidence of a solid tumor or hematopoietic tumor according to radiography, pathology, and immunology examinations. As the disease progressed, the neoplastic neck of the mass became narrow, and the length of its extrusion into the RV increased. Inter-hospital consultation suggested that malignancy should not be excluded even though there was no sufficient evidence. Patients should immediately undergo surgery to excise the progressively enlarged mass which was life threatening, and as we could not confirm its nature, it might as well affect our therapeutic options. However, there were two risks associated with cardiac operation: (1) hemorrhage and poor healing of incisions during and after the surgery because of anticoagulation and immunosuppression therapy, and (2) hypercoagulability during extracorporeal circulation due to non-heparinization during the patient’s first hospitalization. Fortunately, the embolectomy was successful, and the mass inside the RA was confirmed to be a platelet-rich thrombus instead of a tumor or infection according to pathological examination results. Considering that the thrombus was emerged from IVC to the RA under the condition of recanalization of others during anticoagulant therapy, as well as its pathological features and the suspected diagnosis of APS, we prescribe aspirin combined with rivaroxaban to prevent thrombosis from relapse.
This case shows that a thrombus emerging from the IVC to the heart within a short period can appear like a giant tumor. Previously, we considered that the thrombus in the venous system was fibrinous, but the pathology of the mass indicated that it could be a platelet-rich thrombus, and antiplatelet therapy would be needed. We still could not identify whether it was related to the potential cause of TS, like APS, which was suspected in our patient. Further investigation is needed for the mechanism of how a platelet-rich thrombus forms inside the IVC and extends to the heart, as well as the way to prevent this condition in patients with TS.
Acknowledgments
J.-Y.M. and X.Z. contributed equally to this work. They take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The report was supported by Beijing Natural Science Foundation of China (7152053), National Natural Science Foundation of China (81700287), Beijing Municipal Science and Technology Project titled “The Capital Characteristic Clinical Application Research” (Z141107002514130), and Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (ZY201404).
Informed consent: The patient’s parents provided informed consent to publish this case.
ORCID iD: Jing-Yao Ma  https://orcid.org/0000-0003-3737-0876
https://orcid.org/0000-0003-3737-0876
References
- 1. Kitchens CS, Erkan D, Brandao LR, et al. (2011) Thrombotic storm revisited: Preliminary diagnostic criteria suggested by the thrombotic storm study group. The American Journal of Medicine 124: 290–296. [DOI] [PubMed] [Google Scholar]
- 2. Manco-Johnson MJ, Wang M, Goldenberg NA, et al. (2012) Treatment, survival, and thromboembolic outcomes of thrombotic storm in children. The Journal of Pediatrics 161: 682.e1–688.e1. [DOI] [PubMed] [Google Scholar]
- 3. Maggi U, Rossi G, Avesani EC, et al. (2013) Thrombotic storm in a teenager with previously undiagnosed ulcerative colitis. Pediatrics 131: e1288–e1291. [DOI] [PubMed] [Google Scholar]
- 4. Kitchens CS. (1998) Thrombotic storm: When thrombosis begets thrombosis. The American Journal of Medicine 104: 381–385. [DOI] [PubMed] [Google Scholar]
- 5. Miret C, Cervera R, Reverter JC, et al. (1997) Antiphospholipid syndrome without antiphospholipid antibodies at the time of the thrombotic event: Transient “seronegative” antiphospholipid syndrome? Clinical and Experimental Rheumatology 15: 541–544. [PubMed] [Google Scholar]


