Abstract
Background:
Literature suggests a positive impact of self-administration of medication during hospitalization on medication adherence and safety, and on patient satisfaction. However, self-administration is not a common practice in Belgian hospitals. The aim of this study was to describe patients’ willingness towards self-administration of medication while in hospital.
Methods:
A cross-sectional observational study was conducted in three Belgian hospitals in November and December 2015. All patients of 14 randomly selected wards were asked to participate. The structured questionnaire comprised patient characteristics, their willingness and attitude towards self-administration of medication, perceived ability to self-administer during hospitalization, and prerequisites and perceived consequences.
Results:
In total, 124 patients participated (36% of all eligible patients). The main reasons not to participate were the patients’ physical and mental condition (30%) and the absence of patients during the time of data collection (23%). The majority of the 124 participating patients had a positive attitude towards the implementation of self-administration; 83.9% were willing to self-administer their medication while in hospital. Most important prerequisites were self-administration at home before and after hospitalization, patients’ motivation, and a regular evaluation of the patients’ competences. Patients acknowledged benefits such as an increase in autonomy, independence and medication knowledge. Patients did not expect self-administration would cause important safety issues.
Conclusion:
The majority of patients, capable of participating in the study, would want to self-administer medication during hospitalization. They had a positive attitude towards self-administration of medication. Nevertheless, patients stated important conditions which need to be considered in order to implement self-administration.
Keywords: attitudes, hospital, nursing, patient, perspectives, SAM, self-administration of medication
Introduction
Background
Administration of medication in acute care settings is traditionally a nursing responsibility. Nevertheless, self-administration of medication by patients during their hospitalization has been reported in literature since 1959.1 It relates to the process in which patients prepare and consume medications themselves rather than a health professional taking on this role.
There are two systematic reviews on self-administration of medication by hospitalized patients that describe the structure and implementation of several self-administration of medication schemes and self-administration of medication programmes.2,3 Studies on self-administration described advantages compared with administration of medication by nurses, such as an increased patient satisfaction and an improvement of adherence to pharmacotherapy and self-care competence.2–4
The prevalence of self-administration has not been studied extensively. A Flemish prevalence study indicated 22% in a total population of 1269 hospitalized patients self-administered at least one medication during their hospitalization. According to the opinion of the head nurses in this study, almost twice this number of hospitalized patients would have been able to self-administer their medication during hospitalization (41%). The decision-making process of allowing self-administration was mostly shared between the treating physician, the nurse, and the patient. Therefore, requiring an engagement of every stakeholder. Although, hospital pharmacists were not involved in the decision-making process, they remain responsible for medication provision in hospitals and should be involved in self-administration of medication.5,6 A study by McLeod and colleagues which took place in English National Health Service (NHS) hospitals showed the majority of surgical and medical wards (93%) did have a patient self-administration policy.7
In implementing self-administration of medication, the patients’ attitude, as a key stakeholder, is essential. Studies on the opinion or attitudes of patients towards self-administration of medication are however scarce. A study by Deeks and Byatt showed self-administering patients had a significantly better overall impression of care, and were significantly more willing to self-administer medication if hospitalized again.4 In a qualitative study by Manias and colleagues patients described benefits of self-administration, such as: increased patient control, it allows respect for patient knowledge, it encourages a more sharing nurse–patient relationship, and it helps to reinforce the patients’ knowledge about medication.8 Another qualitative descriptive research on healthcare providers’ and patients’ perspectives on self-administration of medication during the patients’ hospital stay identified some important perspectives concerning patients. Participants were convinced self-administration would lead to more satisfied patients, who feel more autonomous and independent. Moreover, patients indicated the benefit of being in control of their own medication, they would not have to disturb nurses in order to question them concerning when and which type of medication would be administered. Patients suggested this approach would result in safer medication management. Although, patients were very positive, they also acknowledged the possibility of medication being abused or stolen by other patients. Also, a possible challenge could be the use of medication from the hospital formulary, resulting in difficulties recognizing generic or brand alternatives.9
To increase levels of implementation, patients’ attitude towards self-administration of medication in hospital has to be known, acknowledged, and taken into account in change management. The presence of qualitative studies concerning this topic allowed the research team to develop a questionnaire. This made it possible to investigate the willingness and attitude of a larger sample of patients.
This study aimed to describe the willingness of Flemish hospitalized patients to self-administer medication and their attitude towards it. Secondary, this study aimed to describe the association of several factors with the willingness to self-administer medication, and to describe the ability of patients to self-administer as well as prerequisites and perceived consequences of self-administration. These results will be taken into account when developing a self-administration of medication policy in Belgian hospitals.
Methods
Design
An observational cross-sectional study was conducted in three Belgian hospitals. Hospitalized patients were questioned in a structured interview on their willingness and attitude towards self-administration of medication.
Participants
In each of two university hospitals and one general hospital, five different wards were randomly selected and invited to participate. The following wards were excluded because of their specific medication management process: paediatrics, emergency departments, intensive care units, operating theatres, and day hospitals. One ward refused to participate due to time restraints. All hospitalized patients, on the day of data collection (n = 342) on these wards were first screened in consultation with the head nurse. Patients were excluded if they were deemed to be too ill to participate, not present on the ward at the time of data collection, not able to speak Dutch, or aged younger than 18 years. The remaining patients were informed about the study and asked to sign informed consent in case of participation (see Table 1).
Table 1.
Flowchart of participants in the study.
| n | % | |
|---|---|---|
| Hospitalized patients on included wards | 342 | 100.0 |
| Step 1: Screening in consultation with head nurse | ||
| Excluded because of: | ||
| Too ill to participate | 100 | 29.3 |
| Not present during study | 78 | 22.8 |
| Not able to speak Dutch | 17 | 5.0 |
| Step 2: Providing oral and written informed consent for patients | ||
| Refused to participate | 23 | 6.7 |
| Participating patients in the study | 124 | 36.3 |
| Hospitalized on: | ||
| Surgical ward | 64 | 51.6 |
| Medical ward | 53 | 42.7 |
| Geriatric ward | 4 | 3.2 |
| Rehabilitation ward | 3 | 2.4 |
Data collection
A self-developed structured questionnaire was used. Firstly, patients were questioned about their characteristics (demographic data and routines of managing chronic medication at home). Secondly, they were questioned about their ability to self-administer medication in hospital. This concerned their own opinion on their ability to self-administer. If they already took chronic medication at home, it concerned the ability to self-administer these medications during hospitalization. If they did not take any chronic medication, it concerned their ability to self-administer medication they got during that particular hospital stay. Thirdly, their attitude towards self-administration of medication in hospital was questioned by a set of five questions. They could be answered with the use of a four-point Likert scale: strongly disagree, disagree, agree, and strongly agree. Fourthly, one explicit question on the patients’ opinion on being keen to self-administer questioned their actual willingness to self-administer with the use of a six-point Likert scale; absolutely not willing, not willing, rather not willing, rather willing, willing, absolutely willing. In the end, their opinion on prerequisites and consequences of self-administration of medication in hospital were assessed (see Table 2 for the structure of the questionnaire and Table 3, Figures 3 and 4 for the items).
Table 2.
Structured overview of the patient questionnaire.
| Structured patient questionnaire | n of questions |
|---|---|
| 1. Patient characteristics | |
| a. Demographic data | 7 |
| b. Medication management chronic medication | 2 |
| 2. Ability to self-administer medication in hospital | 1 |
| 3. Attitude towards self-administration of medication in hospital | 5a |
| 4. Willingness to self-administer medication in hospital | 1b |
| 5. Opinion on prerequisites for self-administration of medication | 8a |
| 6. Opinion on consequences of self-administration of medication | 7a |
4-point Likert scale: strongly disagree-disagree-agree-strongly agree.
6-point Likert scale: absolutely not willing, not willing, rather not willing, rather willing, willing, absolutely willing.
Table 3.
The attitude of patients towards self-administration of medication in hospital.
| I think that… n = 118 |
Disagreea
(%) |
Agreea
(%) |
|---|---|---|
| 1. Patients should be able to continue their own home routines of medication preparation and administration when hospitalized. | 14.2 | 85.8 |
| 2. If I wish to self-administer and I am able to, I should be allowed to do so during a hospital stay. | 19.7 | 80.3 |
| 3. Patients should be stimulated to self-administer medication during hospitalization so they can learn how to take medication correctly. | 27.4 | 72.6 |
| 4. It is always the duty of nurses to prepare and administer medication, even for patients who would be able who do this themselves. | 59.8 | 40.2 |
| 5. I can only self-administer my medication during hospitalization if a healthcare professional monitors me. | 55.7 | 44.3 |
| Total opinion on self-administration of medicationb | ||
| Median [range] | 8 [0–12] | |
| Mean (SD) | 7.5 (2.7) | |
Disagree: sum of % patients who indicated strongly disagree and disagree; Agree: sum of % patients who indicated agree and strongly agree.
The total opinion was calculated by adding statement 1–4. Statement 4 was initially negative and therefore recoded into a positive statement. The internal consistency of this scale is α = 0.786.
SD, standard deviation.
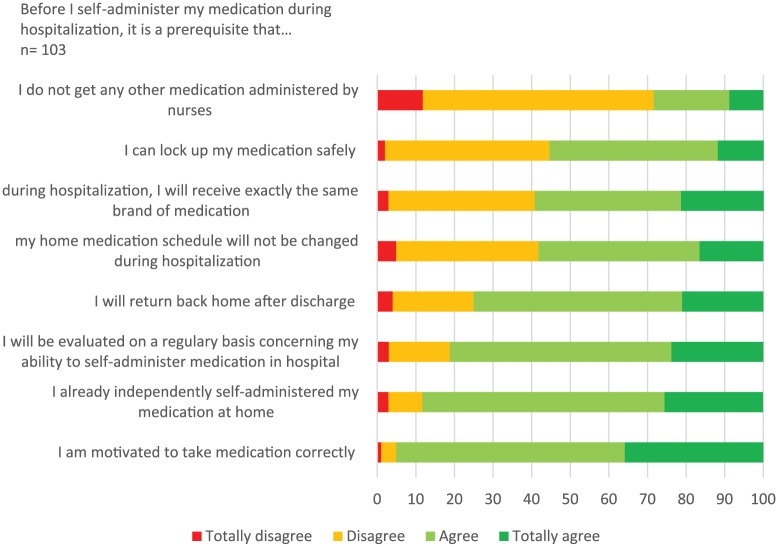
Figure 3.
Prerequisites for self-administration of medication.
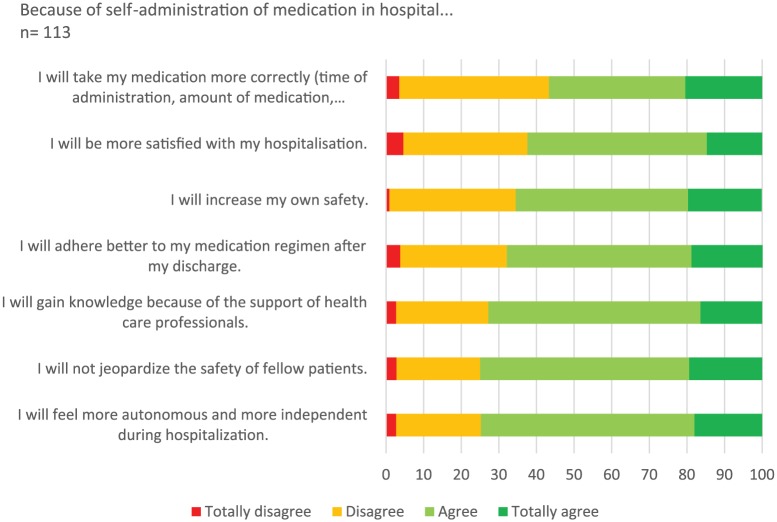
Figure 4.
Consequences of self-administration of medication.
The questionnaire was developed using results from a previous prevalence study on self-administration of medication,5 and a literature review on potential influencing factors of self-administration, benefits and prerequisites for self-administration of medication.4,8,9 The questionnaire was completed, if needed with the help of the interviewer who wrote down the answers for the participant. Data collection was conducted between November and December 2015.
Study outcomes
The primary outcome of this study was the willingness of patients to self-administer medication during hospitalization and their attitude towards self-administration of medication.
The secondary outcome of this study were the patient characteristics associated with the patients’ willingness to self-administer, the ability of patients to self-administer, prerequisites for self-administration of medication, and perceived consequences of self-administration.
Ethical considerations
Permission of the ethics committee of Antwerp University Hospital was received (reference B300201422410). Each patient signed an informed consent document before participating in this study. All collected data were coded.
Data analysis
The Statistical Package for Social Sciences (SPSS) version 24.0 (SPSS Inc, Chicago, IL, USA) was used to analyse the data. Kolmogorov–Smirnov and Shapiro–Wilk tests showed nonnormality of the distributions of age, number of chronic medications taken, the total attitude of patients towards self-administration of medication and their willingness to self-administer. Nonparametric statistics were used to analyse these data. Discontinuous data were described using frequency distributions. Continuous data were described using a mean value and standard deviation if normally distributed, or using a median and range if non-normally distributed. A p-value ⩽0.05 was considered as statistically significant.
The willingness of patients to self-administer medication during hospitalization was questioned with the use of a six-point Likert scale. The attitude of patients towards self-administration of medication in hospital was questioned by a set of five questions, which could be answered with the use of a four-point Likert scale. Out of this set of questions, the first four questions were combined into a scale to describe the overall attitude towards self-administration of medication (see Table 3 for the content of these questions). Before including all questions into this scale, question four was recoded from a negative into a positive statement. The scale was constructed with the use of a sum score of the four questions, resulting in a number between 0 and 12. The higher the number, the more positive the attitude of the patients. The internal consistency of this scale was calculated with Cronbach’s alpha.
Results
Population
In total 36.3% of all eligible patients (n = 124) participated in the study (see Table 1). The main reasons not to participate were the patients’ illness (29.3%), the patient was not present during the time of research (22.8%), and the patient refused to participate (6.7%). Patients were recruited from surgical (51.6%), medical (42.7%), geriatric (3.2%) and rehabilitation wards (2.4%).
Table 4 shows the characteristics of all included hospitalized patients; 46.0% were male, the mean age was 60 years old. Primary education was the highest educational level of 15.3%, over half of the population completed secondary education (55.6%), and 16.1% obtained a Bachelor’s degree. More extended knowledge of the healthcare system could be expected in 18.9%, currently working in healthcare. Most of the patients remained in hospital in the past 2 years, most of them were hospitalized 1–5 nights (29.0%). Of a total of 124 patients, 77.1% took chronic medications at home. They took five different medications on average. The majority of included patients (92.6%) did completely self-manage these medications at home.
Table 4.
Participant characteristics.
| Participant characteristics (n = 124) | |
|---|---|
| Male (%) | 46.0 |
| Age (median [range]) | 60.5 [18–97] |
| Age (mean (SD)) | 59.6 (18.5) |
| Level of education (%) | |
| None | 4.8 |
| Primary school | 15.3 |
| Secondary school | 55.6 |
| Bachelor | 16.1 |
| Master | 8.1 |
| Educated in healthcare (%) | 18.9 |
| Working in healthcare (%) | 18.9 |
| Hospitalized nights in the past 2 years (%) | |
| 0 | 15.3 |
| 1–5 | 29.0 |
| 6–10 | 13.7 |
| 11–15 | 4.0 |
| 16–30 | 15.3 |
| >30 | 22.6 |
| Chronic medication intake at home | |
| Yes (%) | 77.1 |
| mean (SD) | 4.5 (3.5) |
| Chronic medication management at home (%) (n = 94) | |
| Self-management | 92.6 |
| Aid for preparing | 4.3 |
| Aid for preparing and taking | 3.2 |
SD, standard deviation.
Medication use in the population was related to age. Patients who were taking chronic medication at home were significantly older, compared with those who were not (respectively 62.8 years and 46.1 years, Mann–Whitney U, p < 0.001). Furthermore, a positive correlation between the age and the number of chronic medications taken at home was found (Spearman’s rho, r = 0.298, p = 0.006).
Patients’ willingness and attitude towards self-administration of medication in hospital
Figure 1 shows the actual willingness of patients to self-administer medication in hospital, if their health condition would allow them to do so. The majority of patients, stated that they were willing to self-administer their medication in hospital (83.9%). The patients’ attitude towards self-administration of medication was questioned in five questions (see Table 3).
Figure 1.
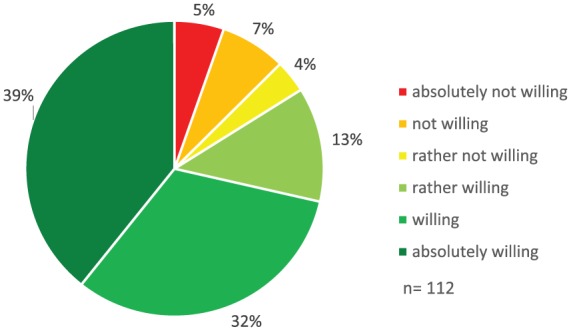
Willingness of patients to self-administer medication in hospital.
The results indicated that patients were convinced they should be able to proceed their home routines of medication management while in hospital (85.8%). In addition, patients stated if they wished to and were able to self-administer, they should be allowed to do so in hospital (80.3%). Furthermore, participating hospitalized patients in this study agreed with the statement ‘Patients should be stimulated to self-administer medication during hospitalization so they can learn how to take medication correctly’ (72.6%). This is in line with the almost 60% of the participants in this study whom did not agree with the quote ‘it is always the duty of nurses to prepare and administer medication, even for patients who would be able who do this themselves.’ When self-administering medication, 55.7% of the patients did not agree that healthcare professionals need to monitor the medication administration of the patients.
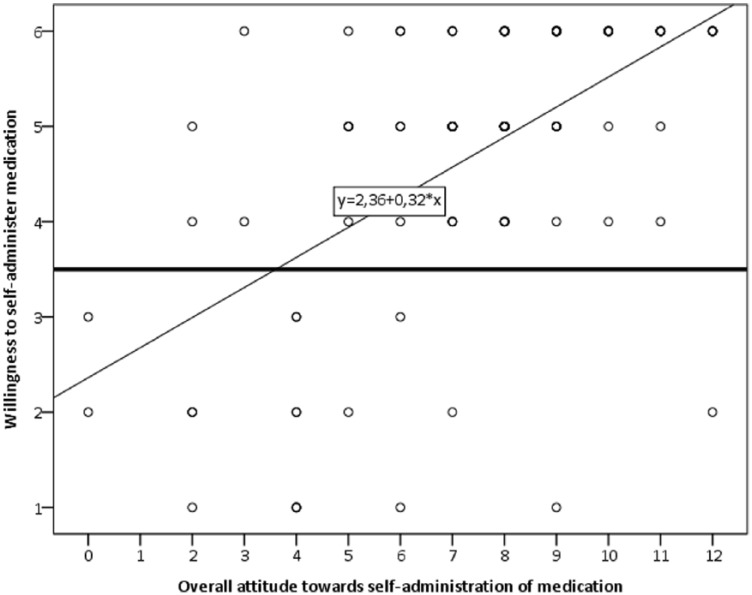
As shown in Figure 2, the willingness of patients positively correlated with the patients’ overall attitude towards self-administration of medication (Spearman’s rho, r = 0.570, p = <0.001). This overall attitude was calculated by four questions, that were integrated into a scale defining the overall attitude of patients towards self-administration of medication in hospital (α = 0.786).
Figure 2.
Relationship between willingness to self-administration of medication and the overall attitude towards self-administration of medication.
n = 111, Spearman’s rho, r = 0.570, p ⩽ 0.001.
Willingness of patients: 1 = absolutely not willing, 2 = not willing, 3 = rather not willing, 4 = rather willing, 5 = willing, 6 = absolutely willing.
Attitude towards self-administration of medication: calculated from questions 1 to 4 (α = 0.786); range from 0 to 12.
Association between patient characteristics and their willingness to self-administer medication
As described in Table 5, patients in this study who were willing to self-administer medication tended to be younger compared with those who were not [one-way analysis of variance (ANOVA), p = 0.345], and did self-administer their chronic medication more often at home (Kruskall–Wallis, p = 0.306). The only factor significantly related to the willingness of patients to self-administer was their own perceived ability to self-administer medication in hospital. Patients who were convinced of their own ability to self-administer were more willing to do so compared with those who stated they would need partial or full help with self-administering medication in hospital (Kruskall–Wallis, p < 0.001).
Table 5.
Relationship between patient characteristics and their attitude towards self-administration of medication.
| n | Willingness to self-administer medication in hospital | p-value | ||||||
|---|---|---|---|---|---|---|---|---|
| absolutely not willing | not willing | rather not willing | rather willing | willing | absolutely willing | |||
| Age (years, mean) | 112 | 74.2 | 63.8 | 60.5 | 59.0 | 58.6 | 58.3 | 0.345 |
| MM at home (%) | ||||||||
| Self-administration+ | 80 | 6.3 | 6.3 | 2.5 | 12.5 | 28.8 | 43.8 | 0.306 |
| Partial help+ | 4 | 0.0 | 0.0 | 0.0 | 25.0 | 50.0 | 25.0 | |
| Full help+ | 2 | 50.0 | 0.0 | 50.0 | 0.0 | 0.0 | 0.0 | |
| Ability to self-administer in hospital (%) | ||||||||
| Self-administrationa | 84 | 2.4 | 4.8 | 1.2 | 8.3 | 36.9 | 46.4 | <0.001 |
| Partial helpb | 15 | 6.7 | 6.7 | 6.7 | 26.7 | 26.7 | 26.7 | |
| Full helpc | 9 | 33.3 | 33.3 | 0.0 | 22.2 | 11.1 | 0.0 | |
Self-administration: patients self-administer their medication completely independently.
Partial help: patients receive partial help and administer medication independent.
Full help: patients are fully dependent on nurses for medication management.
MM, medication management.
Patients’ ability to self-administer medication in hospital
Patients were questioned about their opinion concerning their own ability to self-administer medication during their hospitalization (see Table 6).
Table 6.
Patients’ perception of their own ability to self-administer medication in hospital.
| n | Ability to self-administer medication in hospital | p-valued | |||
|---|---|---|---|---|---|
| Self-administrationa | Partial helpb | Full helpc | |||
| Chronic medication intake at home (%) | |||||
| Yes | 85 | 80.0 | 14.1 | 5.9 | 0.896 |
| No | 26 | 80.8 | 3.8 | 15.4 | |
Self-administration: patients able to self-administer their medication completely independently. bPartial help: self-administer them independent if they got some help in for example filling their medication box.
Full help: be fully dependent on the administration of medication by nurses.
Mann–Whitney test.
If they stated they did take chronic medication, they were questioned about their ability to self-administer these. A total of 80.0% indicated they would be able to self-administer their chronic medication completely independently in hospital, 14.1% would self-administer them independently if they got some help in for example filling their medication box, and 5.9% would be fully dependent on the administration of medication by nurses. If they stated they did not take any chronic medication at home, they were questioned about their ability to self-administer their prescribed medication during hospitalization. A total of 80.8% indicated they would be able to self-administer their medication completely independently, 3.8% would self-administer them independently if they got some help in for example filling their medication box, and 15.4% would be fully dependent on the administration of medication by nurses.
Prerequisites for self-administration of medication
Patients were questioned about important prerequisites for self-administration of medication (see Figure 3).
The majority of participants indicated that patients had to be motivated to self-administer (95.1%) and should already be self-administering medication at home before their hospitalization (88.2%). On top of this, patients acknowledged the importance of a regular evaluation of the patients’ ability to self-administer (81.2%). The prospect of returning home after discharge was another important condition (75.0%). Most patients would not mind a combination of self-administered medication and medication administered by nurses (71.6%). Opinions on locking up self-administered medication, receiving the exact same brand of medication during self-administration, and changes in the home medication schedule during hospitalization were divided. Some patients thought these prerequisites to be necessary, others did not. No significant differences between patient characteristics and prerequisites could be found.
Perceived consequences of self-administration of medication
Hospitalized patients were questioned about the perceived consequences of self-administration of medication in hospital (see Figure 4).
A total of three out of four patients were convinced that self-administration would increase their autonomy and the feeling of being independent, it would not jeopardize the safety of other patients, and they would also gain knowledge on the medication through the support they would receive from healthcare professionals. Patients also suggested that self-administration would result in an increased compliance after their discharge (68%) and it would even increase their own safety while in hospital (65.4%). A smaller percentage of the patients indicated that, self-administration would make them more satisfied about their hospital stay (62.4%). Over half of the patients were convinced self-administration would lead to patients taking their medication more correctly compared with administration of medication by nurses (56.7%).
Discussion
Main findings: willingness and attitude towards self-administration of medication
The study resulted in valuable insights into the willingness and attitude of hospitalized patients concerning self-administration of medication in hospital. Patients indicated they were very willing to self-administer medication, and they judged themselves capable to do so while in hospital. The majority of the patients would appreciate it, if healthcare providers would facilitate this. They had an overall positive attitude towards self-administration of medication. These findings are consistent with those of Deeks and colleagues who described patients who already self-administered medication were significantly more likely to be willing to self-administer medication again during a future hospitalization.4 Also, a qualitative study by Manias and colleagues and Vanwesemael and colleagues indicated patients were positive about self-administration of medication.8,9
Patients were very positive towards maintaining their own home routines in medication management in hospital. Literature indicated this comes with an extra benefit, as it may contribute to increased adherence. A systematic review and meta-analysis on medication adherence difficulties identified that creating a habit-based intervention that links the patients’ daily routines to medication administration, results in an increased adherence. When practicing self-administration of medication in hospital, both patients and healthcare professionals can work together to create those links (e.g. take medication right before breakfast).10 A systematic review on self-administration of medication programmes confirmed the increase of compliance and decrease of medication errors.2
Although, there definitely is a reason to believe self-administration benefits adherence, this might still be very much influenced by the patients’ drug regimen. Research by Vanwesemael and colleagues indicated the complexity of a patients’ drug regimen as an important obstacle to implement self-administration. A relevant quote underpinned this issue; ‘Medication for kidney patients is so delicate, so precise that they (care team) want to have it all in their own hands. We will rarely be able to put a red star next to a kidney patient [mark of self-management of medication].’ (Nurse 1). This study not only highlighted a complex regimen as an obstacle, also changes due to medical examinations that influenced the drug regimen.9
Also, patients in this study indicated self-administration as a possibility to learn how to take medication correctly. This might impact medication-related problems after discharge. A Dutch study on patients’ medication-related problems after hospital discharge (n = 124) indicated 15% of the population experienced medication-related problems (e.g. the indication and how to use the medication was not clear) and 27% reported side effects after hospital discharge.11 Allowing patients to already self-administer medication in hospital provides a certain amount of days to observe the patients’ medication management. When observing medication errors, healthcare professionals have the opportunity to detect errors in patients’ home routines, and are able to react and implement interventions. A systematic review on the effects of self-administration of medication confirms the positive effect on increased knowledge about medication and medication regimens.3 Concerning patients, being able to already self-administer in hospital allows them to practice unfamiliar medication administration routes before being discharged.8,9 In conclusion, observing and evaluating patients’ self-administration of medication management is of great importance. Yet, in order to be able to sufficiently and correctly evaluate this medication management, it is necessary that patients stay hospitalized for a sufficiently long period of time.
Secondary outcomes
The association between patient characteristics and their willingness to self-administer was reported. Younger patients tended to be more willing to self-administer their medication. This result seems to be consistent with other research which found self-administering patients were on average younger compared with nonself-administering patients (self-administering patients: 52.7 years; nonself-administering patients: 66.4 years; p < 0.001).5 The current study did not investigate the association between patient characteristics such as functional status, disease severity, or length of stay and their willingness to self-administer. A previous study however indicated self-administering patients were mostly women, had a lower number of different medications per day before and after their hospitalization. Self-administering patients mostly came from their own home environment and returned back there after discharge. Also, self-administering patients had a better general health status and were less depending on nursing aid during their hospital stay.5
The participating patients were asked to judge for themselves whether they would be able to self-administer their medication in hospital. If they already took chronic medication at home, it concerned this medication. If they did not take any medication at home before hospitalization, it concerned the medication administered during their hospitalization. There were no significant differences found between the group of patients who already took chronic medication at home or patients who did not and their own perceived ability to self-administer. Overall, patients judged themselves capable to self-administer. Nevertheless, this cannot be the only evaluation before actually performing self-administration in hospital. Literature clearly described the necessity of an assessment to objectively define the actual competencies and ability of the patient. This assessment should take several aspects into account, that is, specific conditions related to the patients; mental and physical condition, conditions related to the type of medication; high/low-risk medication, intravenous medication.9
Important prerequisites for self-administration of medication were questioned. More than half of the patients did not consider it necessary to have healthcare professionals monitor patients while self-administering medication. This might be explained by the majority of patients estimating themselves able to self-administer medication in hospital. They assumed by being able to self-administer, they did not need any monitoring while doing so.
Compared with patients indicating monitoring is not really needed, 81% considered it necessary that patients were regularly evaluated on their ability to self-administer medication. These findings highlight another aspect namely evaluation of the patients’ competences in order to self-administer medication. Patients do think it is necessary to evaluate patients on their capabilities or competences to self-administer. At this moment, several existing self-administration of medication programmes include a tool to evaluate patients’ competences in order to self-administer.3 Nevertheless, only two articles described the validation of a tool, named Self-Administration of Medication (SAM). This tool aimed to objectively determine patients’ ability to self-administer.12,13 These findings confirm the need for further research on the validation of tools in different patient populations. If patients are deemed capable to self-administer their medication, patients did not consider it necessary to be monitored by professionals. Yet, from the healthcare professional point of view a monitoring system for self-administration is recommended. In Belgium, it is possible to allow self-administration of medication. Yet, if implemented, this has to be noted in the patients’ personal medical file, and it has to be clearly described which medication is self-administered and which is administered by the nurses. Healthcare providers have a duty of care and a duty of surveillance at all time. If any problems occur during self-administration, these have to be noted in the medical files. The treating physician is then held responsible (Care Inspection of the Flemish Division of Wellbeing, Public Health and Family, personal communication, October 2015). The duty of care and surveillance allows healthcare providers to identify possible medication errors and implement patient tailored interventions. Again, these interventions might prevent medication errors occurring after hospital discharge.2,3,5
Participants in this study indicated some prerequisites for self-administration of medication, for example, only patients who already self-administered medication at home before hospitalization, and will be self-administering after discharge should be allowed to self-administer medication. These study findings might be combined with previous study findings from Vanwesemael and colleagues resulting in a list of prerequisites for patients before allowing self-administration of medication in hospital.5
From this study, we are able to conclude that patients believe it is possible to combine self-administration of medication and administration of medication by nurses. Nevertheless, it was suggested that combining both should be communicated clearly with the patient in order to prevent a lack of clarity. Also, communicating clearly about any changes in the medication schedule is considered important, because 58.2% of the patients stated, ‘not changing the medication schedule from home during hospitalization’ as a prerequisite for self-administration. This communication might prevent problems concerning the medication schedule after discharge.
A study by Manias and colleagues showed several patients were worried about possible misuse of their medication by others.8 This result was also discussed by Vanwesemael and colleagues this study suggested lockers to safely store medication and prevent other patients from abusing or stealing medication.9 However, findings in this study indicated patients did not fully agree on the fact that a locker for storing their medication is necessary. In the end, it should always be stated clearly in the hospital self-administration of medication policy whether it is essential to lock away self-administered medication or where to store this (e.g. inside a locker).
At the end of the questionnaire, possible perceived consequences of self-administration of medication were questioned. These study findings are in line with previous quantitative and qualitative research. Specifically, an increased autonomy or feeling of being independent, increased patient satisfaction, gaining knowledge on medication, and increasing compliance after discharge were previously described.3,4,8 This study added more insights into the patients’ beliefs about the safety of self-administration: they did not especially worry about their own or others safety while self-administering.
Implications for practice
The main objective of this study was to gain an insight in the willingness and attitude of hospitalized patients towards self-administration of medication. Given the very positive results and the willingness of patients to self-administer, focus on increasing the implementation of this concept in daily practice is of foremost importance.
While in our study patients who were willing to self-administer were younger, this did not reach statistical significance. Previous research did prove self-administering patients tended to be younger, more healthier and rather independent during their hospital stay. Also, these patients were more prevalent on surgical short-stay wards, psychiatric wards, surgical wards, and medical wards. These observations give insight in the implementation of self-administration on different types of wards and their patients who would self-administer medication during hospitalization.5
When implementing self-administration of medication in hospital, some barriers should be overcome. Due to hospital admission, patients will receive medication from the current hospital formulary.6 This might result in patients receiving other types or brands of medication. From the study results it is not possible to conclude whether this might be a major obstacle for implementing safe self-administration of medication. Nevertheless, it has to be considered how to tackle problems concerning recognisability of medication. This might be an opportunity to strengthen a multi-disciplinary team approach to achieve better and safer medication management in consultation with the patient.14 On top of this, previous literature already mentioned medication shortages in hospital pharmacies, which have a significant influence on medication management.15
When allowing patients to self-administer medication, the current routines of medication management will change. These changes and differences compared with administration of medication by nurses should be well described; protocols or procedures for self-administration of medication could enhance clarity on both the process and the role of every stakeholder (patient, nurse, practitioner, hospital pharmacist). In order to realize these protocols, it is recommended to question patients, nurses, practitioners, and hospital pharmacists in a qualitative study concerning their opinions on self-administration of medication, possible barriers or facilitators within their organization or ward. Afterwards, a protocol could be developed and tested for validation in daily practice. As this study showed, important aspects which should be included in a self-administration of medication protocol consist of (1) a tool to screen patients’ competences before allowing them to self-administer, (2) a monitoring tool to monitor the intake of self-administered medication, (3) a support tool to both support patients while self-administering (e.g. provide education on medication preparation or intake), and healthcare providers (e.g. additional information on medication or how to educate patients). When testing and validating a self-administration of medication protocol, we should try to investigate how to overcome any organizational restraints in order to improve patients care, without jeopardizing the patient safety.
Implementing self-administration of medication implies that patients need to be hospitalized for a sufficiently long period of time. At first, there will be time needed to assess the patients’ capability and willingness to self-administer. Secondly, the process of self-administration should be started, medication should be prepared, patients might need to be educated concerning their (newly prescribed) medication. Thirdly, patients should be monitored while self-administering, in order to be able to assess their actual abilities and, if needed, provide interventions to improve adherence or medication knowledge.9
Because of the inclusion of several aspects such as supporting, screening, monitoring and empowering patients, the term self-administration of medication does not fully cover all these aspects. Therefore, it is suggested to install the term self-management of medication in hospital, which tries to define a broader range of aspects which need to be looked into when self-administering medication in hospital.
Strengths and limitations
A strength of this study was the random inclusion of several wards in two university and one general hospital. Due to this sample, a diversity of patients were included in the study sample. Also, a random inclusion of surgical, medical, geriatric and rehabilitation wards resulted in attitudes from different types of patients hospitalized for different types of medical backgrounds.
Despite including a very diverse sample, the total number of participating patients was rather low. It is not possible to make statements concerning the willingness and attitude of all hospitalized patients towards self-administration of medication. The main reason for this is that 29% of the eligible patients did not participate in the study due to the severity of their illnesses. Therefore, the results of this study reflected the willingness of the healthier or fitter rather than the acutely or severely ill hospitalized patients. Also, because of the use of a questionnaire, it could have been more likely that only patients with a more positive attitude participated in the study.
On the other hand, as the findings of our study confirm previous findings in international qualitative studies we can assume they are generalizable for this type of hospitalized patients internationally.
Conclusion
The majority of patients were very positive towards self-administration of medication, and they were definitely willing to effectively self-administer their medication in hospital. This positive attitude will facilitate the implementation of self-administration of medication. The stated prerequisites such as a motivated patient, and a regular evaluation of the patients’ abilities should be considered before allowing patients to self-administer medication in hospital. Patients acknowledged some positive benefits such as increased autonomy, independence, and knowledge on their medication. They were not worried about jeopardizing the safety of others, nor were they worried about their own safety when self-administering medication in hospital. In future research, it is important to implement self-administration of medication in hospital with the use of a well-designed and validated protocol, and to study outcomes such as patient satisfaction, knowledge, medication errors, and adherence after discharge in order to objectively investigate the impact of self-administration of medication.
Footnotes
Authors’ note: Toke Vanwesemael is also affiliated to the Departement of Healthcare, Thomas More University College, Lier, Belgium.
Funding: Research for this paper was financially supported by the Thomas More University College.
Conflict of interest statement: The authors declare that there is no conflict of interest.
ORCID iD: Toke Vanwesemael  https://orcid.org/0000-0003-3030-4024
https://orcid.org/0000-0003-3030-4024
Contributor Information
Toke Vanwesemael, Department of Nursing Science and Midwifery, Centre for Research and Innovation in Care (CRIC), Nurse and Pharmaceutical Care (NuPhac), Faculty of Medicine and Health Sciences, University of Antwerp, Universiteitsplein 1, 2610 Wilrijk, Belgium.
Koen Boussery, Pharmaceutical Care Unit, Faculty of Pharmaceutical Sciences, Ghent University, Ghent, Belgium.
Patricia van den Bemt, Department of Hospital Pharmacy, Erasmus University Medical Center’s Gravendijkwal, CE Rotterdam, The Netherlands.
Tinne Dilles, Department of Healthcare, Thomas More University College, Lier, Belgium; Department of Nursing Science and Midwifery, Centre for Research and Innovation in Care (CRIC), Nurse and Pharmaceutical Care (NuPhac), Faculty of Medicine and Health Sciences, University of Antwerp, Wilrijk, Belgium.
References
- 1. Parnell MA. Medicines at the bedside. Am J Nurs 1959; 59: 1417–1418. [PubMed] [Google Scholar]
- 2. Wright J, Emerson A, Stephens M, et al. Hospital inpatient self-administration of medicine programmes: a critical literature review. Pharm World Sci 2006; 28: 140–151. [DOI] [PubMed] [Google Scholar]
- 3. Richardson SJ, Brooks HL, Bramley G, et al. Evaluating the effectiveness of self-administration of medication (SAM) schemes in the hospital setting: a systematic review of the literature. PLoS One 2014; 9: e113912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Deeks PA, Byatt K. Are patients who self-administer their medicines in hospital more satisfied with their care? J Adv Nurs 2000; 31: 395–400. [DOI] [PubMed] [Google Scholar]
- 5. Vanwesemael T, Van Rompaey B, Petrovic M, et al. SelfMED: self-administration of medication in hospital: a prevalence study in flanders, Belgium. J Nurs Scholarsh 2017; 49: 277–285. [DOI] [PubMed] [Google Scholar]
- 6. Royal decree setting out the standards which hospital pharmacies must meet to be authorized. 1991. Available at: www.ejustice.just.fgov.be/cgi_loi/change_lg.pl?language=nl&la=N&table_name=wet&cn=1991030433
- 7. McLeod M, Ahmed Z, Barber, et al. A national survey of inpatient medication systems in English NHS hospitals. BMC Health Serv Res 2014; 14: 93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Manias E, Beanland C, Riley R, et al. Self-administration of medication in hospital: patients’ perspectives. J Adv Nurs 2004; 46: 194–203. [DOI] [PubMed] [Google Scholar]
- 9. Vanwesemael T, Boussery K, Manias E, et al. Self-management of medication during hospitalisation: healthcare providers’ and patients’ perspectives. J Clin Nurs 2018; 27: 753–768. [DOI] [PubMed] [Google Scholar]
- 10. Conn VS, Ruppar TM, Enriquez M, et al. Medication adherence interventions that target subjects with adherence problems: systematic review and meta-analysis. Res Social Adm Pharm 2016; 12: 218–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Eibergen L, Janssen MJA, Blom L, et al. Informational needs and recall of in-hospital medication changes of recently discharged patients. Res Social Adm Pharm 2018; 14: 146–152. [DOI] [PubMed] [Google Scholar]
- 12. Anderson J, Manias E, Kusljic S, et al. Testing the validity, reliability and utility of the Self-Administration of Medication (SAM) tool in patients undergoing rehabilitation. Res Social Adm Pharm 2014; 10: 204–216. [DOI] [PubMed] [Google Scholar]
- 13. Manias E, Beanland CJ, Riley RG, et al. Development and validation of the self-administration of medication tool. Ann Pharmacother 2006; 40: 1064–1073. [DOI] [PubMed] [Google Scholar]
- 14. Adhikari R, Tocher J, Smith P, et al. A multi-disciplinary approach to medication safety and the implication for nursing education and practice. Nurse Educ Today 2014; 34: 185–190. [DOI] [PubMed] [Google Scholar]
- 15. Preece D, Price R. PS-076 The problem of medicines shortages in hospitals across Europe: the European Association of Hospital Pharmacists (EAHP) Survey. Eur J Hosp Pharm Sci Pract 2014; 21: A174–A175. [Google Scholar]