Abstract
Objective:
Recent research suggests that disordered gambling and psychosis co-occur at higher rates than expected in the general population. Gamblers with psychosis also report greater psychological distress and increased gambling severity. However, the mechanism by which psychosis leads to greater gambling symptomology remains unknown. The objective of the present research was to test whether impulsivity mediated the relationship between comorbid psychosis and gambling severity.
Method:
The sample consisted of 394 disordered gamblers voluntarily seeking treatment at a large university hospital in São Paulo, Brazil. A semistructured clinical interview (Mini-International Neuropsychiatric Interview) was used to diagnosis the presence of psychosis by registered psychiatrists. Severity of gambling symptoms was assessed using the Gambling Symptom Assessment Scale, and the Barratt Impulsiveness Scale–11 provided a measure of impulsivity.
Results:
Of the sample, 7.2% met diagnostic criteria for psychosis. Individuals with a dual diagnosis of psychosis did not report greater gambling severity. Conversely, dual diagnoses of psychosis were associated with greater levels of impulsivity. Higher levels of impulsivity were also associated with greater gambling severity. Importantly, support for our hypothesised mediation model was found such that impulsivity mediated the association between disordered gambling and psychosis and gambling severity.
Conclusion:
Impulsivity appears to be a transdiagnostic process that may be targeted in treatment among disordered gamblers with a dual diagnosis of psychosis to reduce problematic gambling behaviours.
Keywords: psychosis, disordered gambling, impulsivity, mediation
Abstract
Objectif:
La recherche récente suggère que le jeu pathologique et la psychose sont co-occurrents à un taux plus élevé qu’escompté dans la population générale. Les joueurs souffrant de psychose déclarent aussi une plus grande détresse psychologique et une gravité accrue du jeu. Toutefois, le mécanisme par lequel la psychose entraîne une plus grande symptomatologie du jeu demeure inconnu. L’objectif de la présente recherche était de vérifier si l’impulsivité servait de médiateur à la relation entre la psychose comorbide et la gravité du jeu pathologique.
Méthode:
L’échantillon consistait en 394 joueurs pathologiques cherchant volontairement un traitement à un grand hôpital universitaire de São Paulo, au Brésil. Une entrevue clinique semi-structurée (MINI) a servi à diagnostiquer la présence de psychose par des psychiatres agréés. La gravité des symptômes de jeu a été évaluée à l’aide de l’échelle d’évaluation des symptômes du jeu, et l’échelle d’impulsivité de Barratt – 11 mesurait l’impulsivité.
Résultats:
Dans l’échantillon, 7,2% satisfaisaient aux critères diagnostiques de la psychose. Les personnes ayant un double diagnostic de psychose ne déclaraient pas une plus grande gravité du jeu. À l’inverse, les diagnostics doubles de psychose étaient associés à de plus hauts niveaux d’impulsivité. Les niveaux élevés d’impulsivité étaient aussi associés à une gravité accrue du jeu. Surtout, notre hypothèse de modèle de médiation s’est confirmée du fait que l’impulsivité médiait l’association entre le jeu pathologique et la psychose et la gravité du jeu.
Conclusion:
L’impulsivité semble être un processus transdiagnostique qui peut être ciblé en traitement chez les joueurs pathologiques qui ont un double diagnostic de psychose afin de réduire les comportements de jeu problématiques.
Disordered gambling and psychosis are both rare psychiatric disorders, with prevalence rates estimated to be 1% to 2%1 and 1% to 3%,2 respectively. There is empirical evidence to suggest, however, that these disorders co-occur at greater rates compared to the general population. Studies examining the co-occurrence of these 2 rare disorders have found that disordered gamblers are 3.5 to 3.8 times more likely to be diagnosed with psychosis.3,4 Similarly, 12.2% to 19.2% of individuals with psychosis meet criteria for disordered gambling,5–7 suggesting that disordered gamblers are at an increased risk of psychosis and vice versa.
A potential reason for the increased rate of comorbidity between the 2 disorders may be due to similar dysfunctions in brain pathology and psychological processes common to both. For example, both disordered gambling and psychosis are linked to abnormalities in dopamine and serotonin transmission,8–10 disruption of motivation and reward systems, impaired impulse control, and reward-directed behavioural disturbance10–12—dysfunctions that may also manifest in increased risk of psychopathology. Indeed, disordered gamblers with psychosis are at greater risk of poly-comorbid psychopathology and suicidality compared to disordered gamblers without psychosis.3
Recent empirical studies have also highlighted that disordered gamblers with psychosis may experience greater gambling severity and more cognitive distortions around gambling.13 Corroborating these findings, disordered gamblers with psychosis report significantly more problems with gambling, including spending more hours gambling per week and greater psychosocial impairments associated with their gambling.3 Despite recent accumulating evidence of greater gambling severity among this dual-diagnosis population, the mechanism by which the dual diagnosis of gambling and psychosis leads to increased gambling severity remains unknown. In the present research, we propose that impulsivity may represent one potential mechanism that may account for the relationship between disordered gamblers with a dual diagnosis of psychosis and increased gambling severity.
The Mediating Role of Impulsivity
Impulsivity is defined as “a predisposition toward rapid, unplanned reactions to internal or external stimuli without regards to the negative consequences to these reactions.”14 Impulsivity is widely thought of as a multidimensional construct composed of various psychological facets, including cognitive, affective, and motor components.15 Recently, impulsivity has been conceptualised from a transdiagnostic perspective, in which high levels of impulsivity constitute an underlying pathology that may lead to the manifestation of a wide array of psychological symptoms.16 Providing support for this supposition, impulsivity has been suggested to be a core feature of addictive disorders, including disordered gambling,17 as well as psychosis.18,19
In terms of the association between impulsivity and disordered gambling, disordered gamblers consistently report greater levels of impulsivity compared to nongamblers.20 The significant role of impulsivity in disordered gambling has also been demonstrated using behavioural tasks. For example, delay-discounting tasks show that disordered gamblers are more likely to prefer smaller immediate rewards over larger delayed rewards, which is associated with greater gambling severity.21 Impulsivity is also a core feature of psychosis. High levels of impulsivity have been identified in studies using both self-report measures22 as well as behavioural assessments of impulsivity.23 In fact, impulsivity is one of the most commonly reported behavioural characteristics in psychosis,24 which may manifest in increased risk of problematic engagement with addictive disorders, including disordered gambling.
Elevated rates of impulsivity may have some important clinical implications in the treatment of disordered gambling. For example, among disordered gamblers, impulsivity is associated with greater severity of gambling symptomology.25 Furthermore, previous studies have found that higher levels of impulsivity have been associated with worse treatment outcomes, including increased likelihood of treatment failure (i.e., dropout).26–28 Unfortunately, most treatment models for disordered gambling do not adequately incorporate strategies to reduce impulsivity, which potentially reduces treatment efficacy. If impulsivity is shown to be a mediating mechanism, then it may be possible to target impulsivity during treatment to improve outcomes both among disordered gamblers and disordered gamblers with a dual diagnosis of psychosis.
In sum, the extant literature has identified impulsivity as a key clinical feature of both disordered gambling and psychosis, which suggests that a dual diagnosis of disordered gambling and psychosis may be associated with increased impulsivity. In turn, increased impulsivity may be the mechanism by which disordered gamblers with psychosis experience greater gambling severity. Providing support for this supposition, it has been postulated that impulsivity may be the mechanism that links psychosis with addictive disorders.29 However, no study to date has empirically tested this assertion or assessed whether impulsivity mediates the association between a dual diagnosis of disordered gambling and psychosis and increased gambling severity. The aim of the present research was to fill this empirical gap.
Methods
Participants and Procedures
Disordered gamblers who were voluntarily seeking treatment (N = 349) were recruited at the Gambling Outpatient Unit of the Institute of Psychiatry at the University of São Paulo Hospital in Brazil between 2006 and 2015. Ethics approval was obtained from the ethics committee of the Clinics Hospital of the University of São Paulo, and informed consent was obtained from all participants prior to data collection. Patients were clearly told at the outset that treatment was not contingent upon research participation.
Measures
Psychosis
The Portuguese version of the Mini-International Neuropsychiatric Interview (MINI)30 was used by registered psychiatrists to make a diagnosis of psychosis. The diagnoses of psychosis in the present research include any disorders in the psychosis spectrum (e.g., schizophrenia, schizoaffective disorder) but exclude mood disorders with psychotic features. The MINI is a brief semistructured psychiatric interview that has demonstrated strong psychometric properties, including reliable diagnoses, compared to the Composite International Diagnostic Interview (CIDI) and the Structured Clinical Interview for the DSM (SCID). Compared to the SCID, Sheehan and colleagues31 reported the following measures of agreement for a clinical diagnosis of psychosis: κ = 0.76, sensitivity = 0.88, specificity = 0.92, positive predictive value = 0.77, and negative predicted value = 0.96. Similar measures of agreement were reported when comparing the MINI to the CIDI: κ = 0.70, sensitivity = 0.87, specificity = 0.89, positive predictive value = 0.70, and negative predicted value = 0.96.32
Gambling severity
Gambling symptom severity was assessed using a Portuguese version of the Gambling Symptom Assessment Scale (G-SAS).33 The GSAS is a 12-item self-report measure that provides an overall indication of gambling severity, including preoccupation with gambling, loss of control over one’s gambling behaviour, and psychological and interpersonal harms caused by gambling. The original validation of the G-SAS reported a test-retest reliability of .704 and demonstrated good convergent validity with the Pathological Gambling–Clinical Global Impression.34 In a subsequent study,33 the G-SAS demonstrated good reliability (test-retest) and validity compared to the Problem Gambling–Yale Brown Obsessive Compulsive Scale and physician-rated Clinical Global Impression Scale. Each item on the G-SAS is rated on a 0- to 4-point Likert scale, with higher scores indicating more severe gambling symptoms. The internal consistency of the G-SAS in the present sample was α = .93.
Impulsivity
The Portuguese version of the Barratt Impulsiveness Scale–11 (BIS-11)35 was used to provide a measure of impulsivity and is arguably the most widely used self-report measure of impulsivity.36 The BIS-11 contains 30 items that assess various aspects of impulsivity and is anchored from 0 (rarely/never) to 4 (almost always/always). The items are summed to provide an overall score, with elevated scores indicating greater levels of impulsivity. The BIS-11 has demonstrated excellent psychometric properties in both clinical and nonclinical populations and has been shown to reliably differentiate between nonaddiction and addiction populations, including disordered gamblers.36 Indeed, the internal consistency from the current sample was α = .73.
Analytic Plan
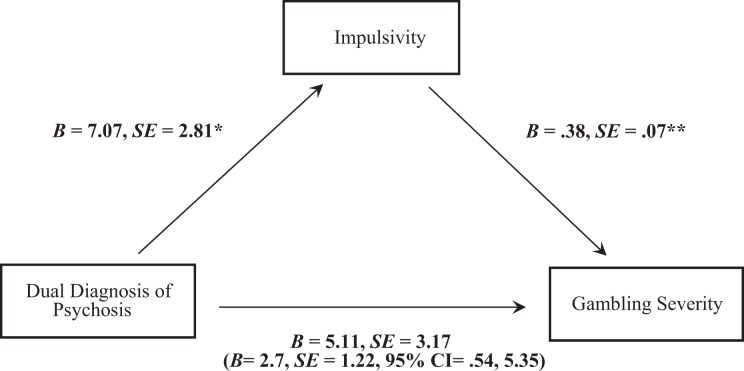
To test our mediation model, we first used Baron and Kenny’s 3-step test of mediation37 to assess the associations between a dual diagnosis of disordered gambling and psychosis, impulsivity, and gambling severity (see Figure 1). In the first step of the model, we tested whether a dual diagnosis of disordered gambling and psychosis was associated with increased gambling severity. Next, we tested whether disordered gamblers with psychosis reported greater levels of impulsivity and whether increased impulsivity was associated with greater gambling severity when controlling for dual diagnosis. In the final step, we assessed whether impulsivity weakened the association between disordered gamblers with psychosis and increased gambling severity (i.e., mediation). We then obtained bias-corrected 95% bootstrapped confidence intervals (CIs) of this indirect effect with 10,000 iterations using Preacher and Hayes’s38 PROCESS macro (model 4). The number of disordered gamblers with psychosis (n = 25) was at the minimum level for regression-based mediation models, and therefore we chose to bootstrap with 10,000 iterations to provide more stability to our model. Support for mediation is found when the 95% CIs of the indirect effect do not cross zero. Bootstrapping techniques have become the gold standard for testing mediation as it provides increased power and is a nonparametric test (i.e., does not assume normal distribution). Furthermore, simulation tests show that bootstrapping is the most valid method of testing mediation.39
Figure 1.
Mediation model with dual diagnosis of psychosis as the independent variable (coded : 0 = no psychosis, 1 = psychosis), impulsivity as the mediator, and gambling severity as the dependent variable. The unstandardized coefficients and standard error shown in parentheses reflect the inclusion of the mediator in the equation. *p < .05, **p < .01.
We did not collect age of onset for psychosis, which would have helped to establish temporality between the independent variable (IV) and dependent variable (DV). We proceeded to test a mediation model with the following theoretical justification: (1) the age of onset for gambling problems in the present sample was 39.29 (SD, 12.92), and (2) the age of onset for psychosis is typically early to mid-20s for men and late 20s for women.40 As such, it is plausible that, on average, the onset of psychosis preceded the onset of gambling problems, which helps to partly address the issue of temporality. Finally, we controlled for gender in our mediation analysis as women were more likely to be diagnosed with psychosis and reported greater levels of gambling severity in our sample.
Results
Preliminary Results
Table 1 provides a summary of the demographic characteristics of the sample. The rate of psychosis in the present sample was 7.2% (n = 25). The results found that disordered gamblers with psychosis were more likely to be female and reported lower years of formal education. No other demographic differences were found, Ps > 0.35.
Table 1.
Comparison of Demographic Characteristics between Disordered Gamblers with and without Psychosis.
| Disordered Gamblers without Psychosis (n = 324) | Disordered Gamblers with Psychosis (n = 25) | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | n | % | M (SD) | n | % | M (SD) | Test | P Value |
| Age | 47.1 (12.6) | 47.6 (10.1) | U = 0.15a | 0.880 | ||||
| Sex | χ2 = 5.61 | 0.018b* | ||||||
| Male | 191 | 60.3 | 9 | 36.0 | ||||
| Female | 126 | 39.7 | 16 | 64.0 | ||||
| Ethnic group | 0.224c | |||||||
| Caucasian | 225 | 72.3 | 14 | 58.3 | ||||
| African American | 23 | 7.4 | 5 | 20.8 | ||||
| Mixed race | 48 | 15.4 | 5 | 20.8 | ||||
| Asian | 11 | 3.5 | 0 | 0.0 | ||||
| Other | 3 | 1.0 | 0 | 0.0 | ||||
| Marital status | 0.380c | |||||||
| In a relationship | 161 | 51.9 | 11 | 44.0 | ||||
| Single | 89 | 28.7 | 12 | 48.0 | ||||
| Other | 59 | 19.4 | 2 | 8.0 | ||||
| Sexual orientation | 0.714c | |||||||
| Heterosexual | 295 | 94.6 | 25 | 100.0 | ||||
| Homosexual | 13 | 4.2 | 0 | 0.0 | ||||
| Bisexual | 3 | 1.0 | 0 | 0.0 | ||||
| Years of education | 11.3 (4.6) | 9.6 (6.3) | U = –2.11a | 0.035* | ||||
| Income ($USD) | 5242.27 (6861.66) | 3532.40 (2951.95) | U = –0.93a | 0.354 | ||||
aMann-Whitney U.
bChi-square.
cFisher’s exact test was used as expected cell counts were less than 5.
*P < 0.05.
Main Results
Table 2 provides correlations and means/standard deviations (on the diagonal) for our variables of interest. In regards to our main analysis, no significant differences were found between disordered gamblers with and without psychosis on gambling severity (B = 5.11; SE = 3.17; t = 1.30; P = 0.196; 95% CI, –2.14 to 10.36). Conversely, disordered gamblers with psychosis reported significantly higher levels of impulsivity (B = 7.07; SE = 2.81; t = 2.51; P = 0.013; 95% CI, 1.52-12.61). Impulsivity was also significantly associated with greater gambling severity, even when controlling for a dual diagnosis of psychosis (B = .38; SE = .07; t = 5.24; P < 0.001; 95% CI, .23-.53).
Table 2.
Correlations between Dual Diagnosis of Psychosis, Gambling Severity, and Impulsivity (Means and Standard Deviations on the Diagonal).
| Psychosis | Gambling Severity | Impulsivity | |
|---|---|---|---|
| Psychosis | n = 25 | ||
| Gambling severity | .12a | 26.09 (11.18) | |
| Impulsivity | .17a* | .34** | 73.12 (10.39) |
Mediation Analysis
Although a nonsignificant direct effect of comorbid psychosis and gambling severity was observed, we proceeded to test the hypothesised mediation model as advances in mediation analysis no longer require a significant direct effect when proposing a significant indirect effect.38,41,42 The results of the bootstrapping found that the bias-corrected 95% CI of the indirect effect was estimated to lie between .54 and 5.35 (B = 2.70; SE = 1.22), thus providing support for our hypothesised mediation model (Figure 1). The association between psychosis and gambling severity weakened when impulsivity was included in the model (B = 1.41; SE = 3.03; t = .47; P = 0.642; 95% CI, –4.57 to 7.39). We also ran the above mediation analysis with the DSM-5 40 symptom count for gambling disorder as an alternate measure of gambling severity. The pattern of results remained consistent, providing further support for our mediation model.
Discussion
Disordered gamblers with a dual diagnosis of psychosis remain an understudied population, despite recent research suggesting that they represent a high-risk clinical group. The present research adds to a growing understanding of potential factors that may lead these individuals to experience significantly elevated levels of psychopathology and distress. In the present research, we found that impulsivity is a potential mechanism leading disordered gamblers with psychosis to experience significantly greater gambling severity compared to disordered gamblers without psychosis. These results make theoretical sense given the important role of impulsivity in the manifestation of both disordered gambling and psychosis, as well as increased severity of gambling problems.
An interesting finding of the present research is that women were more likely to be diagnosed with psychosis and in turn exhibited greater levels of impulsivity. This finding at first may seem go against the extant literature, which consistently finds that men are more likely to be diagnosed with psychosis43 and are more likely to be impulsive.44 However, amongst people diagnosed with psychosis, previous research on gender differences has found that women are in fact more likely to experience greater levels of impulsivity than men.45,46 As the present research hypothesised impulsivity as the mechanism that may lead to greater gambling severity, it is plausible that the greater proportion of women in our sample with psychosis may be due to the elevated levels of impulsivity among women with psychosis leading to greater gambling severity and thus being more likely to seek treatment than male gamblers with psychosis.
The finding that impulsivity is elevated amongst disordered gamblers with a dual diagnosis of psychosis converges with previous research that has examined impulsivity among gamblers with comorbid psychiatric disorders. For example, impulsivity has been found to be elevated amongst disordered gamblers with comorbid substance use disorders, including alcohol47,48 as well as mood disorders.49 These findings are not surprising when examined from the influential pathways model of problem and pathological gambling.50 According to the pathways model, impulsivity is a key characteristic of the pathway 3 gamblers, who are likely to present with the greatest impairments in gambling severity, distress, and comorbid psychiatric disorders. Furthermore, it is thought that impulsivity is heightened during periods of negative affect (i.e., urgency), which may further increase gambling severity and distress. Given impulsivity has been linked to a wide array of comorbid psychiatric disorders (including psychosis) and that it is linked to greater severity suggests the important role impulsivity may play in the expression of comorbid disorders and the need to be targeted during treatment for disordered gambling.
The results of the present research have important clinical implications. Recent advances in the study of psychopathology have moved from symptom-based models towards those emphasising clusters of syndromes and transdiagnostic approaches that cut across psychopathology.51,52 Impulsivity has been identified as one key potential transdiagnostic factor, which may underlie the expression of various psychiatric disorders, including addictive disorders and psychosis.53 Identifying underlying psychological processes has immense treatment benefits in that targeting and treating these processes can be more efficient in alleviating psychopathology54 and can reduce secondary psychiatric symptoms in comparison to treatments targeting a single disorder. For example, transdiagnostic treatments for anxiety disorders often result in not only reduced symptoms of anxiety but also ameliorate symptoms of depression.55
Applied to the context of the present research, treatment strategies that help disordered gamblers with psychosis (and disordered gamblers without psychosis) to make less impulsive choices may be an effective strategy in decreasing problematic gambling behaviour. A potential treatment strategy that could be applied in this context is working memory training. There is evidence suggesting that working memory training can effectively increase self-control and reduce impulsivity (e.g., delayed reward discounting).56 While working memory training has yet to be examined in populations of pathological gamblers, it has shown promise as an adjunctive treatment for individuals with other addictions57 and individuals with psychosis.58 These results suggest that working memory training may be an efficient and effective method of reducing gambling symptoms, particularly those with an already elevated risk of impulsivity such as individuals with a dual diagnosis of disordered gambling and psychosis.
A second clinically significant finding in the present research is that, while the rates of comorbid psychosis were not as high as comorbid mood or substance use disorders typically found among gamblers,59 7.2% is a significant prevalence and is approximately 3 times higher than rates of psychosis found in the local population.60 Moreover, previous research suggests that disordered gamblers with psychosis represent a uniquely high-risk population, as individuals with this dual diagnosis present with greater levels of impairment and distress, including suicidality.3 As such, we hope that the present research further highlights the need for clinicians who specialise in the treatment of disordered gamblers to be cognisant of the potential dual diagnosis of psychosis and the potential need for critical care.
Limitations
A limitation of the present research is the cross-sectional nature of the study. Although the present research provides preliminary support that impulsivity is an important mechanism that leads disordered gamblers with psychosis to experience greater severity of gambling problems, longitudinal studies are needed to infer causality. However, in the present research, we examined theoretically plausible mediation pathways, as the age of onset for problem gambling in the sample is significantly older than the typical age of onset for psychosis, suggesting that the onset of psychosis generally preceded the onset of gambling. Second, the sample consisted of treatment-seeking gamblers, which may reduce the generalisability of results; however, the results of our present research may have greater clinical utility. Third, the present sample cannot speak to specific DSM-5 40 psychotic disorders. As such, it is not known whether the association between psychosis and impulsivity and gambling severity is dependent on chronicity or severity. Fourth, the data collection in the present sample ranged 10 years, which may introduce historical threats. That said, the Gambling Outpatient Unit of the Institute of Psychiatry at the University of São Paulo Hospital was under the direction of the senior author (H.T.) throughout the duration of the study, which provides stability in data collection. Indeed, no major changes to the recruitment or protocol occurred during the study period, which helps to control for historical threats. Last, there are likely other mechanistic factors that are important in understanding the relationship between this dual-diagnosis population and increased psychopathology, such as emotional dysregulation, reliance on maladaptive coping strategies, and that gambling may fill a social need among disordered gamblers with psychosis.13 Future research assessing other potential mediators would be highly informative.
Conclusion
Disordered gamblers with a dual diagnosis of psychosis represent a high-risk population. Yet, there is a paucity of empirical literature assessing clinical and psychological correlates in this population. The present research aimed to add to our growing understanding in this population by examining impulsivity as a mechanism by which disordered gamblers with psychosis experience greater gambling severity. These results highlight the need for further research on disordered gamblers with psychosis, as well as the need for sophisticated treatments in working with this population in clinical practice.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Hodgins DC, Stea JN, Grant JE. Gambling disorders. Lancet. 2011;378(9806):1874–1884. [DOI] [PubMed] [Google Scholar]
- 2. Perala J, Suvisaari J, Saarni SI, et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch Gen Psychiatry. 2007;64:19–28. [DOI] [PubMed] [Google Scholar]
- 3. Cassetta B, Kim HS, Hodgins DC, et al. Disordered gambling and psychosis: demographic and clinical correlates. Schizophr Res. In press. [DOI] [PubMed] [Google Scholar]
- 4. Cunningham-Williams RM, Cottler LB, Compton WM III, et al. Taking chances: problem gamblers and mental health disorders—results from the St. Louis epidemiologic catchment area study. Am J Public Health. 1998;88(7):1093–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Aragay N, Roca A, Garcia B, et al. Pathological gambling in a psychiatric sample. Compr Psychiatry. 2012;53(1):9–14. [DOI] [PubMed] [Google Scholar]
- 6. Desai RA, Potenza MN. A cross sectional study of problem and pathological gambling in patients with schizophrenia/schizoaffective disorder. J Clin Psychiat. 2009;70(9):1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Haydock M, Cowlishaw S, Harvey C, et al. Prevalence and correlates of problem gambling in people with psychotic disorders. Compr Psychiatry. 2015;58:122–129. [DOI] [PubMed] [Google Scholar]
- 8. Blaszczynski A, Nower L. A pathways model of problem and pathological gambling. Addiction. 2002;97(5):487–499. [DOI] [PubMed] [Google Scholar]
- 9. Meltzer HY, Massey WB, Horiguchi M. Serotonin receptors as targets for drugs useful to treat psychosis and cognitive impairment in schizophrenia. Curr Pharm Biotechnol. 2012;13(8):1572–1586. [DOI] [PubMed] [Google Scholar]
- 10. Potenza MN, Steinberg MA, McLaughlin SD, et al. Gender-related differences in the characteristics of problem gamblers using a gambling helpline. Am J Psychiatry. 2001;158(9):1500–1505. [DOI] [PubMed] [Google Scholar]
- 11. Griffiths MD. Betting your life on it: problem gambling has clear health related consequences. BMJ. 2004;329(7474):1055–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Potenza MN, Chambers RA. Schizophrenia and pathological gambling. Am J Psychiatry. 2001;158(3):497–498. [DOI] [PubMed] [Google Scholar]
- 13. Yakovenko I, Clark CM, Hodgins DC, et al. A qualitative analysis of the effects of a comorbid disordered gambling diagnosis with schizophrenia. Schizophr Res. 2016;171(1):50–55. [DOI] [PubMed] [Google Scholar]
- 14. Moeller FG, Barratt ES, Dougherty DM, et al. Psychiatric aspects of impulsivity. Am J Psychiatry. 2001;158(11):1783. [DOI] [PubMed] [Google Scholar]
- 15. Hodgins DC, Holub A. Components of impulsivity in gambling disorder. Int J Ment Health Addict. 2015;13(6):699–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Johnson SL, Carver CS, Joormann J. Impulsive responses to emotion as a transdiagnostic vulnerability to internalizing and externalizing symptoms. J Affect Disord. 2013;150(3):872–878. [DOI] [PubMed] [Google Scholar]
- 17. Nower L, Blaszczynski A. Development and validation of the Gambling Pathways Questionnaire (GPQ). Psychol Addict Behav. 2017;31(1):95–109. [DOI] [PubMed] [Google Scholar]
- 18. Kester HM, Sevy S, Yechiam E, et al. Decision-making impairments in adolescents with early-onset schizophrenia. Schizophr Res. 2006;85(1-3):113–123. [DOI] [PubMed] [Google Scholar]
- 19. Ouzir M. Impulsivity in schizophrenia: a comprehensive update. Aggress Violent Behav. 2013;18(2):247–254. [Google Scholar]
- 20. Tavares H, Gentil V. Pathological gambling and obsessive-compulsive disorder: towards a spectrum of disorders of volition. Rev Bras Psiquiatr. 2007;29(2):107–117. [DOI] [PubMed] [Google Scholar]
- 21. MacKillop J, Amlung MT, Few LR, et al. Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology (Berl). 2011;216(3):305–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Enticott PG, Ogloff JRP, Bradshaw JL. Response inhibition and impulsivity in schizophrenia. Psychiatry Res. 2008;157(1-3):251–254. [DOI] [PubMed] [Google Scholar]
- 23. Dixon MR, Marley J, Jacobs EA. Delay discounting by pathological gamblers. J Appl Behav Anal. 2003;36:449–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee TY, Kim SN, Jang JH, et al. Neural correlate of impulsivity in subjects at ultra-high risk for psychosis. Prog Neuropsychopharmacol Biol Psychiatry. 2013;45:165–169. [DOI] [PubMed] [Google Scholar]
- 25. Brevers D, Cleeremans A, Verbruggen F, et al. Impulsive action but not impulsive choice determines problem gambling severity. PLoS One. 2012;7(11):e50647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Merkouris SS, Thomas SA, Browning CJ, et al. Predictors of outcomes of psychological treatments for disordered gambling: a systematic review. Clin Psychol Rev. 2016;48:7–31. [DOI] [PubMed] [Google Scholar]
- 27. Ramos-Grille I, Gomà-i-Freixanet M, Aragay N, et al. Predicting treatment failure in pathological gambling: the role of personality traits. Addict Behav. 2015;43:54–59. [DOI] [PubMed] [Google Scholar]
- 28. Ramos-Grille I, Gomà-i-Freixanet M, Aragay N, et al. The role of personality in the prediction of treatment outcome in pathological gamblers: a follow-up study. Psychol Assess. 2013;25(2):599. [DOI] [PubMed] [Google Scholar]
- 29. Gut-Fayand A, Dervaux A, Olié JP, et al. Substance abuse and suicidality in schizophrenia: a common risk factor linked to impulsivity. Psychiatry Res. 2001;102(1):65–72. [DOI] [PubMed] [Google Scholar]
- 30. Amorim P. Mini International Neuropsychiatric Interview (MINI): validation of a short structured diagnostic psychiatric interview. Rev Bras Psiquiatr. 2000;22(3):106–115. [PubMed] [Google Scholar]
- 31. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry, 1997;12(5):232–241. [Google Scholar]
- 32. Lecrubier Y, Sheehan DV, Weiller E, et al. The Mini International Neuropsychiatric Interview (MINI): a short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry. 1997;12(5):224–231. [Google Scholar]
- 33. Kim SW, Grant JE, Potenza MN, et al. The Gambling Symptom Assessment Scale (G-SAS): a reliability and validity study. Psychiatry Res. 2009;166(1):76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kim SW, Grant JE. An open naltrexone treatment study in pathological gambling disorder. Int Clin Psychopharmacol. 2001;16(5):285–289. [DOI] [PubMed] [Google Scholar]
- 35. Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt Impulsiveness Scale. J Clin Psychol. 1995;51:768–774. [DOI] [PubMed] [Google Scholar]
- 36. Stanford MS, Mathias CW, Dougherty DM, et al. Fifty years of the Barratt Impulsiveness Scale: an update and review. Pers Individ Dif. 2009;47(5):385–395. [Google Scholar]
- 37. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. [DOI] [PubMed] [Google Scholar]
- 38. Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–731. [DOI] [PubMed] [Google Scholar]
- 39. Hayes AF. Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun Monogr. 2009;76(4):408–420. [Google Scholar]
- 40. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed Washington (DC): American Psychiatric Association; 2013. [Google Scholar]
- 41. MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wu AD, Zumbo BD. Understanding and using mediators and moderators. Soc Indic Res. 2008;87(3):367–392. [Google Scholar]
- 43. Aleman A, Kahn RS, Selten JP. Sex differences in the risk of schizophrenia: evidence from meta-analysis. Arch Gen Psychiatry. 2003;60(6):565–571. [DOI] [PubMed] [Google Scholar]
- 44. Cross A. Sex differences in impulsivity: a meta-analysis. Psychol Bull. 2011;137(1):97–130. [DOI] [PubMed] [Google Scholar]
- 45. Goldstein JM, Link BG. Gender and the expression of schizophrenia. J Psychiatr Res. 1988;22(2):141–155. [DOI] [PubMed] [Google Scholar]
- 46. Leung MD, Psych CM. Sex differences in schizophrenia, a review of the literature. Acta Psychiatr Scand. 2000;101(401):3–38. [DOI] [PubMed] [Google Scholar]
- 47. Petry NM. Pathological gamblers, with and without substance abuse disorders, discount delayed rewards at high rates. J Abnorm Psychol. 2001;110(3):482. [DOI] [PubMed] [Google Scholar]
- 48. Kräplin A, Bühringer G, Oosterlaan J, et al. Dimensions and disorder specificity of impulsivity in pathological gambling. Addict Behav. 2014;39(11):1646–1651. [DOI] [PubMed] [Google Scholar]
- 49. Lister JJ, Milosevic A, Ledgerwood DM. Psychological characteristics of problem gamblers with and without mood disorder. Can J Psychiatry. 2015;60(8):369–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Blaszczynski A, Nower L. A pathways model of problem and pathological gambling. Addiction. 2001;97(5):487–499. [DOI] [PubMed] [Google Scholar]
- 51. Kotov R, Krueger RF, Watson D, et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psych. In press. [DOI] [PubMed] [Google Scholar]
- 52. Nolen-Hoeksema S, Watkins ER. A heuristic for developing transdiagnostic models of psychopathology: explaining multifinality and divergent trajectories. Perspect Psychol Sci. 2011;6(6):589–609. [DOI] [PubMed] [Google Scholar]
- 53. Robbins TW, Gillan CM, Smith DG, et al. Neurocognitive endophenotypes of impulsivity and compulsivity: towards dimensional psychiatry. Trends Cogn Sci. 2012;16(1):81–91. [DOI] [PubMed] [Google Scholar]
- 54. Krueger RF, Eaton NR. Transdiagnostic factors of mental disorders. World Psychiatry. 2015;14(1):27–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Craske MG. Transdiagnostic treatment for anxiety and depression. Depress Anxiety. 2012;29(9):749–753. [DOI] [PubMed] [Google Scholar]
- 56. Bickel WK, Yi R, Landes RD, et al. Remember the future: working memory training decreases delay discounting among stimulant addicts. Biol Psychiatry. 2011;69(3):260–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Houben K, Wiers RW, Jansen A. Getting a grip on drinking behavior: training working memory to reduce alcohol abuse. Psychol Sci. 2011;22(7):968–975. [DOI] [PubMed] [Google Scholar]
- 58. Wykes T, Huddy V, Cellard C, et al. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168(5):472–485. [DOI] [PubMed] [Google Scholar]
- 59. Lorains FK, Cowlishaw S, Thomas SA. Prevalence of comorbid disorders in problem and pathological gambling: systematic review and meta-analysis of population surveys. Addiction. 2011;106(3):490–498. [DOI] [PubMed] [Google Scholar]
- 60. Andrade L, Walters EE, Gentil V, et al. Prevalence of ICD-10 mental disorders in a catchment area in the city of Sao Paulo, Brazil. Soc Psychiatry Psychiatr Epidemiol. 2002;37(7):316–325. [DOI] [PubMed] [Google Scholar]