Abstract
Objective:
We examine the association between rates of homicide resulting in a mental health disposition (termed mentally abnormal homicide [MAH]) and homicides without such a disposition, as well as to province-wide psychiatric hospitalisation and incarceration rates.
Method:
In this population-based study, we investigate all adult homicide perpetrators (n = 4402) and victims (n = 3783) in Ontario from 1987 to 2012. We present annual rates of mentally abnormal and non–mentally abnormal homicide and position them against hospitalisation and incarceration rates.
Results:
Among the total sample of homicide accused, 3.7% were mentally abnormal. Most (82.5%) had a psychotic disorder at the time of the offense. Contrasted with declining hospitalisation, incarceration, and population homicide rates, the rate of MAH remained constant at an average of .07 perpetrators per 100,000 population. The rate of MAH was not associated with discharges from or average length of stay in psychiatric hospitals (ρ = 0.10; 0.34, P > 0.10), incarceration rates (ρ = 0.16, P = 0.42), or the total homicide rate (ρ = 0.25, P = 0.22). The proportion of MAH perpetrators with a substance use disorder increased modestly over time (β = 0.35, R 2 = 0.12, P = 0.08).
Conclusions:
The rate of MAH has not changed appreciably over the past 25 years. Declining psychiatric service utilisation was not associated with the rate of homicide committed by people with mental illness and, secondarily, was not linked to increases in the population homicide or incarceration rates. Substance use has become a more prevalent problem for this population.
Keywords: homicide, psychiatric services, mentally ill persons, forensic mental health
Abstract
Objectif:
Nous examinons l’association entre les taux d’homicide résultant d’une disposition de santé mentale (appelée homicide mentalement anormal [HMA]) et les homicides sans cette disposition, ainsi que les taux d’hospitalisation psychiatrique et d’incarcération à l’échelle de la province.
Méthode:
Dans cette étude dans la population, nous investiguons tous les adultes auteurs d’homicide (n = 4 402) et les victimes (n = 3 783) en Ontario de 1987 à 2012. Nous présentons les taux annuels des homicides mentalement anormaux et de ceux qui ne le sont pas, et nous les positionnons par rapport aux taux d’hospitalisation et d’incarcération.
Résultats:
Au sein de l’échantillon total des accusés d’homicide, 3,7% étaient mentalement anormaux. La majorité (82,5%) souffrait d’un trouble psychotique au moment de l’infraction. Contrairement aux taux à la baisse d’hospitalisation, d’incarcération et d’homicide dans la population, le taux d’HMA demeurait constant avec une moyenne de 0,07 coupable par 100 000 de population. Le taux d’HMA n’était pas associé aux congés ou à la durée moyenne de séjour dans des hôpitaux psychiatriques (ρ = 0,10; 0,34, p > 0,10), aux taux d’incarcération (ρ = 0,16, p = 0,42), ni au taux total des homicides (ρ = 0,25, p = 0,22). La proportion des coupables d’HMA ayant un trouble d’utilisation de substances augmentait modestement avec le temps (β = 0,35, R 2 = 0,12, p = 0,08).
Conclusions:
Le taux d’HMA n’a pas sensiblement changé au cours des 25 dernières années. L’utilisation diminuée des services psychiatriques n’était pas associée au taux des homicides commis par des personnes souffrant de maladie mentale, et deuxièmement, elle n’était pas liée aux augmentations dans la population des taux d’homicide ou d’incarcération. L’utilisation de substances est devenue un problème plus prévalent pour cette population.
Publicity surrounding violent behavior, especially homicides, committed by individuals with serious mental illness (SMI) is a major source of fear and stigma towards this population and has contributed to rising public safety concerns and calls for greater restrictions on those with SMI.1 These concerns have risen since the period of deinstitutionalisation, with increasing numbers of people with SMI now in contact with the public.2 Contemporaneously, crime rates rose in most Western countries between 1960 and the 1990s, possibly fueling existing stigma towards persons with SMI.3
Studies from western Europe, Australia, and New Zealand have examined whether the rate of homicide associated with SMI (mentally abnormal homicide, or MAH) has changed over this time period, finding that MAH rates have been static3,4 or have fallen.5 In England and Wales, MAH rates increased alongside the total homicide rate from the 1950s to 1970s but then fell progressively while total homicides continued to rise.5 An Australian study found that rates of criminal conviction for those with schizophrenia rose during the major period of deinstitutionalisation (1975-1995) but only to the same degree as violent crime rates in the general population.6,7 In Germany, no change was found in attempted and completed homicides among those with schizophrenia when calculated prior to (1955-1964) or following deinstitutionalisation (1992-1996).8
Rebutting earlier suggestions,9 recent meta-analytic findings from developed countries show that rates of homicide by persons with schizophrenia correlate strongly with population homicide rates.10 Supporting these findings is research demonstrating that risk factors for violence in the general population also contribute to the violence committed by those with SMI (e.g., poverty, substance misuse, inadequate social supports)11–13 and that similar sociological factors affect both population homicide rates and MAH.5
Recent studies have also explored the effect of mental health services and laws on rates of MAH. The decline in MAH in England and Wales, for example, has been attributed to improvements in psychiatric care and service organisation.5 In a cross-sectional study of homicide, mental health service characteristics, and civil commitment law across 50 US states, population homicide rates were inversely correlated with the quality of mental health services and the permissiveness of civil commitment laws.14 In a Swedish sample, treatment with adequate doses of antipsychotic (for persons with psychosis) or mood-stabilising (for persons with bipolar disorder) medication resulted in significant reductions in violent and nonviolent behavior.15 Similarly, persons with SMI released from prisons in the United Kingdom who received antipsychotic medication showed reductions in violence risk.16
The Ontario Context
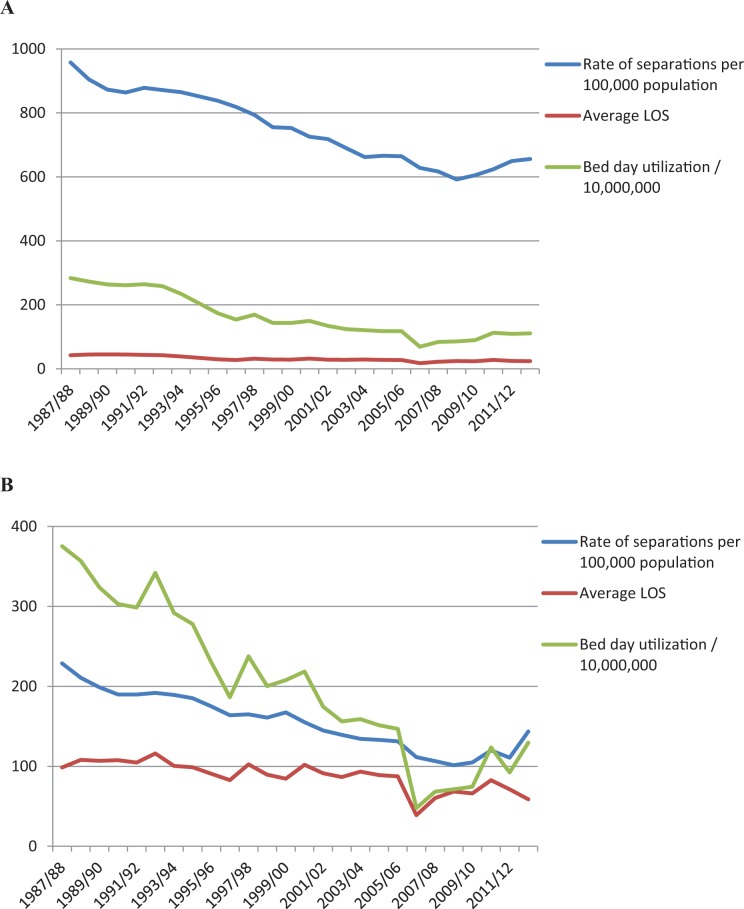
Deinstitutionalisation occurred progressively across Ontario from the 1970s.17 The number of inpatient beds within psychiatric hospitals fell from 3.6 per 1000 population in 1965 to 0.9 by 1980. This process continued into the 2000s. As shown in Figure 1, the annual rate of separations (discharges, deaths) for all mental health–related admissions in Ontario fell from 957.5 per 100,000 population in 1987-1988 to 655.9 in 2012-2013 (a 32% decrease). The average length of stay for each admission fell from 42.5 days in 1987-1988 to 24.1 days in 2012-2013 (a 43% decrease), and bed day utilisation (calculated as the population-adjusted separation rate × length of stay) fell by 61%. In contrast, spending on community mental health services increased significantly over this period. The notion that deinstitutionalisation resulted in increased numbers of mentally ill persons in prisons continues to be of widespread concern; however, there are no studies of changing prevalence of SMI in Canadian prisons.
Figure 1.
Annual number of separations, average length of stay, and bed day utilisation for all mental health (A) and psychiatric hospital (B) admissions in Ontario, 1987 to 2012. Separations refer to the discrete number of discharges from all psychiatric hospitals in Ontario and include patient deaths. LOS, length of stay (days).
With respect to the nature of mental health law, Ontario’s civil commitment laws fall into the ‘legalistic’ grouping of mental health legislation as described by Winick18 and others.19 Such legislation has emphasised civil liberties over clinical needs, which can make clinicians reluctant to use civil commitment in other than emergency situations. Lower rates of civil commitment have been found to result in higher levels of criminal justice involvement in the United States,20 but no record of the rate of usage of civil commitment is centrally recorded in Ontario. Consequently, it is difficult to investigate whether rates of usage have affected MAH rates over time.
The Current Study
We investigated whether the rate of homicide by people with SMI has changed over the period from 1987 to 2012, specifically in relation to hospitalisation, incarceration, and population homicide rates. We further examined victim characteristics of MAH and non-MAH homicide perpetrators to investigate who is at risk for homicide victimisation and whether rates of different psychiatric and substance use disorders for MAH perpetrators have changed over time. This represents the first comprehensive analysis of these trends in North America and provides data against which public concern regarding the risk posed by individuals with SMI may be evaluated.
Homicide, because of its high clearance rate and minimal reporting bias, is a unique means of studying epidemiological shifts in the prevalence of serious violence through time. Over the study period, the criminal responsibility defense was largely unchanged, presenting an opportunity to examine population homicide against homicides resulting in a mental health disposition (unfit to stand trial [UST] or not criminally responsible on account of mental disorder [NCRMD]) and arrive at a reliable population-level measure of the relationship between SMI and homicidal violence.
Method
We reviewed all homicides in Ontario from 1987 to 2012 to compute the population homicide rate as well as the rate of MAH. A variety of sources were used (below) as there is not one single database that provides information on all homicide perpetrators and events. For MAH perpetrators, we collected information on psychiatric diagnosis and whether the individual recidivated following the homicide. Victim information was collected for both MAH and non-MAH perpetrators. All study procedures were approved by the institutional review board at the Centre for Addiction and Mental Health.
We included all adults aged 18 years and older who had been accused of murder (first or second degree), manslaughter, or infanticide or who had been found UST or NCRMD on such charges. Prior to 1992, the term not guilty by reason of insanity (NGRI) was in use; however, the wording of the legal test for criminal responsibility, which is closely based on the M’Naghten standard,21 did not change materially following the introduction of NCRMD. A UST-accused person was defined as a MAH perpetrator who was deemed unfit for at least 2 years or who was found permanently UST. If a UST-accused person became fit to proceed and returned to court, the final disposition (e.g., criminally responsible, NCRMD) determined which class of homicide he or she was placed in. Time frames for MAH events were defined by the date of the offense, while time frames for non-MAH were defined by the year the homicide was reported by police.
Data Sources
Ontario Review Board
The Ontario Review Board (ORB) oversees all individuals adjudicated NGRI/NCRMD or UST in the province of Ontario. ORB records available to review included psychiatric reports and legal disposition documents, both of which contain detailed information pertaining to the psychosocial, legal, and mental health histories of the accused, as well as the synopsis of the offense(s).
Ontario court reports
Court files are available to the public through 2 online legal databases: CriminalSource and LexisNexis. Files include evidence, sentencing, appeal, and trial hearings, and they typically contain detailed information about the homicide, facts of the case, legal proceedings, and outcomes. Court files also contain information about the victim-perpetrator relationship and evidence of psychiatric problems at the time of the incident. We searched for individuals found UST or NGRI/NCRMD on charges of murder, manslaughter, or infanticide to supplement ORB records (above) and ensure the completeness of our list of MAH perpetrators.
Statistics Canada and the Homicide Survey
Non-MAH rates and victim characteristics were obtained from Statistics Canada and the Homicide Survey, a mandatory nationwide survey completed by police following every homicide event. This survey has been the primary mechanism for the collection of national homicide statistics in Canada since 1961. The survey contains extensive information about the offense, the victim, and the accused. Ontario population and incarceration statistics were retrieved from Statistics Canada.22 The latter included all adults sentenced to provincial or federal prisons in the province of Ontario.
Ontario Mental Health Reporting System
Information on psychiatric hospitalisation rates was obtained through the Ontario Mental Health Reporting System (OMHRS), a reporting system that collects information about individuals admitted to designated adult mental health beds in Ontario for each fiscal year, drawn from 68 participating hospitals. We retrieved the following data from the OMHRS for the fiscal years 1987-1988 to 2012-2013: 1) number of separations (discharges, deaths) per 100,000 adult population and 2) length of stay (days) per 100,000 adult population for admissions to psychiatric hospitals, admissions to general hospitals for mental health reasons, and all mental health–related admissions.
Statistical Analysis
Homicide rates per 100,000 population from 1987 to 2012 were calculated based on the total number MAH and non-MAH perpetrators (perpetrator-based analysis) and victims of MAH and non-MAH perpetrators (victim-based analysis). Perpetrator- and victim-based homicide rates were analysed using Poisson generalised linear models (GLMs) with year, perpetrator type (MAH, non-MAH), and their interaction entered as predictors. Rates of hospital separations and length of stay were analysed using Poisson GLMs, with fiscal year entered as the predictor. Incarceration rates were analysed using Poisson regression. Spearman correlations tested whether homicide rates from 1987 to 2012 were associated with markers of psychiatric service utilisation (i.e., number of separations, length of stay) and incarceration rates in Ontario during this period. Quasi-Poisson models were adopted when over- or underdispersion was detected. Proportion data were analysed using χ2. Our threshold for statistical significance was P < 0.05 (2-sided, uncorrected). All analyses were conducted using R.23
Results
Homicide Rates
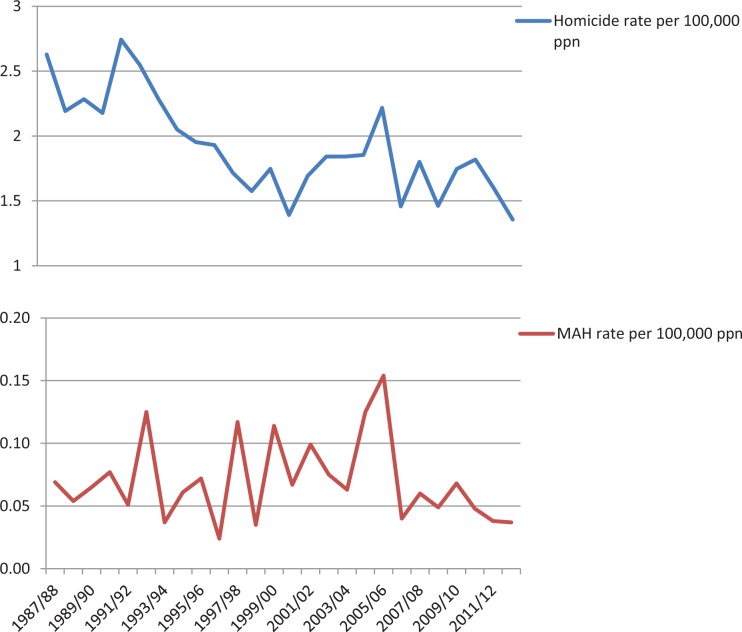
The total number of adults accused of committing homicide in Ontario from 1987 to 2012 was 4402 (Table 1). Of these, 163 (3.7%) were MAH perpetrators (140 NCRMD, 14 NGRI, 9 UST) and 4239 were non-MAH perpetrators (96.3%). There was a mean (SD) of 6.30 (3.1) MAH perpetrators, or 0.07 (0.03) per 100,000 population, compared to a mean (SD) of 163.0 (22.3) non-MAH perpetrators, or 1.85 (0.37) per 100,000 population. Homicide rates (perpetrator based) decreased significantly from 1987 to 2012 (Table 2, Figure 2). Although the interaction of year × perpetrator type was not significant, separate models showed a significant decline in annual non-MAH perpetrator rates from 1987 to 2012, whereas no change was detected in annual rates of MAH perpetrators. Consistent with this, we found no significant association between annual rates of MAH and non-MAH perpetrators (ρ = 0.18, P = 0.39) and overall homicide perpetrator rates (ρ = 0.25, P = 0.22) during this period. Identical results were obtained using victim-based incidence rates.
Table 1.
Homicide Rates for Ontario, 1987 to 2012.
| Year | No. of MAHs | Total No. of Homicides | % of MAHs | Ontario Adult Population | Rate of Homicides per 100,000 | Rate of MAHs per 100,000 |
|---|---|---|---|---|---|---|
| 1987 | 5 | 191 | 2.62 | 7,267,343 | 2.628 | 0.069 |
| 1988 | 4 | 163 | 2.45 | 7,435,864 | 2.192 | 0.054 |
| 1989 | 5 | 175 | 2.86 | 7,661,302 | 2.284 | 0.065 |
| 1990 | 6 | 170 | 3.53 | 7,810,501 | 2.177 | 0.077 |
| 1991 | 4 | 217 | 1.84 | 7,910,556 | 2.743 | 0.051 |
| 1992 | 10 | 204 | 4.90 | 8,007,234 | 2.548 | 0.125 |
| 1993 | 3 | 185 | 1.62 | 8,096,360 | 2.285 | 0.037 |
| 1994 | 5 | 168 | 2.98 | 8,195,312 | 2.050 | 0.061 |
| 1995 | 6 | 162 | 3.70 | 8,296,379 | 1.953 | 0.072 |
| 1996 | 2 | 162 | 1.23 | 8,394,933 | 1.930 | 0.024 |
| 1997 | 10 | 146 | 6.85 | 8,517,706 | 1.714 | 0.117 |
| 1998 | 3 | 136 | 2.21 | 8,633,924 | 1.575 | 0.035 |
| 1999 | 10 | 153 | 6.54 | 8,760,152 | 1.747 | 0.114 |
| 2000 | 6 | 124 | 4.84 | 8,915,752 | 1.391 | 0.067 |
| 2001 | 9 | 154 | 5.84 | 9,104,253 | 1.692 | 0.099 |
| 2002 | 7 | 171 | 4.09 | 9,290,313 | 1.841 | 0.075 |
| 2003 | 6 | 174 | 3.45 | 9,449,515 | 1.841 | 0.063 |
| 2004 | 12 | 178 | 6.74 | 9,601,187 | 1.854 | 0.125 |
| 2005 | 15 | 216 | 6.94 | 9,742,807 | 2.217 | 0.154 |
| 2006 | 4 | 144 | 2.78 | 9,878,522 | 1.458 | 0.040 |
| 2007 | 6 | 180 | 3.33 | 9,995,106 | 1.801 | 0.060 |
| 2008 | 5 | 148 | 3.38 | 10,125,086 | 1.462 | 0.049 |
| 2009 | 7 | 179 | 3.91 | 10,250,705 | 1.746 | 0.068 |
| 2010 | 5 | 189 | 2.65 | 10,393,957 | 1.818 | 0.048 |
| 2011 | 4 | 168 | 2.38 | 10,529,806 | 1.595 | 0.038 |
| 2012 | 4 | 145 | 2.76 | 10,694,594 | 1.356 | 0.037 |
MAH, mentally abnormal homicide. Includes persons found not criminally responsible on account of mental disorder and persons found unfit to stand trial.
Table 2.
Rates and Associations between Psychiatric Service Utilisation, Homicide, and Incarceration in Ontario, 1987 to 2012.
| Rate Change, 1987-2012 | Association with Homicide Rates | |||||
|---|---|---|---|---|---|---|
| MAH Rate | Non-MAH Rate | |||||
| β (SE) | P Value | Spearman ρ | P Value | Spearman ρ | P Value | |
| No. of separations per 100,000 adult population | ||||||
| Psychiatric hospitals | –0.028 (0.002) | <0.001 | 0.10 | 0.61 | 0.67 | <0.001 |
| General hospitals | –0.016 (0.001) | <0.001 | 0.10 | 0.62 | 0.72 | <0.001 |
| All mental health–related admissions | –0.018 (0.001) | <0.001 | 0.12 | 0.57 | 0.72 | <0.001 |
| Length of stay per 100,000 adult population | ||||||
| Psychiatric hospitals | –0.049 (0.004) | <0.001 | 0.20 | 0.32 | 0.69 | <0.001 |
| General hospitals | –0.046 (0.005) | <0.001 | –0.12 | 0.55 | 0.62 | <0.001 |
| All mental health–related admissions | –0.048 (0.003) | <0.001 | 0.18 | 0.38 | 0.71 | <0.001 |
| Total population homicide rate (perpetrator based) | –0.019 (0.003) | <0.001 | ||||
| MAH | –0.007 (0.013) | 0.61 | — | — | — | — |
| Non-MAH | –0.019 (0.003) | <0.001 | — | — | — | — |
| Adult incarceration rate | –0.002 (0.001) | 0.08 | –0.16 | 0.42 | 0.22 | 0.28 |
MAH, mentally abnormal homicide. Includes persons found not criminally responsible on account of mental disorder and persons found unfit to stand trial. —, data values are not applicable for these cells.
Figure 2.
Rates of mentally abnormal and nonabnormal homicide in Ontario, 1987 to 2012.
Associations between MAH and Psychiatric Hospitalisation and Incarceration Rates
A modest decline was found in the annual adult incarceration rate in Ontario from 1987 to 2012 (Table 2). Describing ongoing deinstitutionalisation of mental health care in Ontario, significant annual declines occurred in the number of separations from and length of stay in psychiatric hospitals, in general hospitals, and for all mental health–related admissions per 100,000 population (Table 2, Figure 1).
We then tested whether homicide rates were associated with population hospitalisation and incarceration rates. As shown in Table 2, MAH rates (perpetrator based) were not associated with any measure of psychiatric service utilisation or incarceration from 1987 to 2012. Conversely, non-MAH rates were positively associated with all measures of hospitalisation, but not incarceration rates, from 1987 to 2012. Thus, we observed a decline in both population homicide rates and indicators of psychiatric service utilisation but no association between these indicators and MAH.
Homicide Victims
We had information for 3783 victims of homicide by MAH (n = 170, 4.5%) and non-MAH (n = 3613, 95.5%) perpetrators. Victim type included family (e.g., spouse, parents, grandparents, children, siblings), other intimates/acquaintance (e.g., boyfriend/girlfriend, friend, neighbor, business relationship), and stranger. A significantly greater proportion of MAH perpetrator victims were family members, while a significantly greater proportion of non-MAH perpetrator victims were other intimates/acquaintances and strangers (Table 3). Of all victims killed by strangers, 15 were killed by mentally unwell persons, while 695 were killed by non–mentally abnormal perpetrators.
Table 3.
Characteristics of Homicide Victims and MAH Perpetrators.
| MAH Perpetrators | Non-MAH Perpetrators | χ2 (P) | |
|---|---|---|---|
| Victim type, % (95% confidence interval) | |||
| Family | 60.6 (52.8, 68.0) | 34.3 (32.7, 35.9) | 47.9 (<0.001) |
| Other intimate/acquaintance | 30.0 (23.2, 37.5) | 49.3 (47.7, 51.0) | 23.5 (<0.001) |
| Stranger | 9.4 (5.5, 14.8) | 16.4 (15.2, 17.6) | 5.35 (<0.05) |
| Diagnosis, n (%) | |||
| Psychosis | 132 (82.5) | — | — |
| Schizophrenia only | 85 (53.1) | — | — |
| Mood/anxiety without psychosis | 18 (11.3) | — | — |
| Neurocognitive/developmental | 12 (7.5) | — | — |
| Paraphilia | 2 (1.3) | — | — |
| Personality disorder (PD) | 28 (17.5) | — | — |
| Antisocial PD | 15 (9.4) | — | — |
| Substance use disorder | 66 (41) | — | — |
MAH, mentally abnormal homicide. Includes persons found not criminally responsible on account of mental disorder and persons found unfit to stand trial. —, data values are not applicable for these cells.
Characteristics of Mentally Abnormal Homicide Perpetrators
Diagnostic information for 98.2% (n = 160) of MAH perpetrators was obtained. Most MAH perpetrators had a psychotic disorder, the largest proportion being schizophrenia-spectrum disorders (Table 3). Substance-related disorder information was available for 98.8% (n = 161) of MAH perpetrators, almost half of whom had a comorbid substance abuse disorder. A significant increase was found in the annual proportion of MAH perpetrators with a schizophrenia-spectrum disorder from 1987 to 2012 (β = 0.445, SE = 0.005, P < 0.05, R 2 = 0.20), while the annual proportion of MAH perpetrators with a comorbid substance abuse disorder showed a trend towards increasing over time (β = 0.35, SE = 0.007, P = 0.08, R 2 = 0.12).
Prior forensic patient status was available for 152 (93.3%) of the MAH perpetrators. For almost all (n = 150, 98.7%), their homicide offence was their first presentation to forensic services. Posthomicide recidivism while under the authority of the ORB was low: just 6 (3.9%) MAH perpetrators reoffended following their NCRMD/UST finding, 5 of whom were violent recidivists (assault being most common). There was no homicide recidivism in the MAH perpetrators.
Discussion
We found no significant change in the rate of mentally abnormal homicide in Ontario over the past 25 years. Although the rate of homicide in the general population progressively fell, the rate of MAH remained unchanged. MAH rate was unrelated to the markers of psychiatric service utilisation described in this study and suggests that significant declines in the provision of inpatient mental health services have not been associated with an increase in the rate of serious violence among those with SMI. Furthermore, decreasing institutional psychiatric services was not associated with a rise in incarceration. The oft-quoted ‘Penrose effect’24 would have predicted that as psychiatric hospital numbers fell, homicide rates should have risen and prison numbers should have risen. Neither of these trends was observed in this study.
The average annual MAH rate of 0.07 per 100,000 persons is at the lower end of rates found in developed nations, noted to be on the order of 0.02 to 0.36.9,10 In keeping with the literature,4,25 victims of homicide by people with SMI are more often family members, unlike non-MAH perpetrators, who more frequently kill strangers and acquaintances.
The observed rate of MAH in this study did not decrease in parallel with the general population homicide rate, as Large and colleagues10 might have predicted. This suggests that MAH rates may have been driven in part by factors independent of those that influence non-MAH rates in this relatively low homicide rate jurisdiction. Other studies have suggested that increasing expenditures on community mental health services might contribute to lower MAH.5,26 While the current study can only provide an indirect assessment of this association given the known increases in expenditures over the study period, it is an important line of inquiry with clear financial and public safety implications. It may follow from Segal14 that improved expenditure on mental health services and better mental health laws could be associated with lowering population homicide rates, although these observations are from the United States, which has a higher homicide rate than Canada and comparatively lower expenditures on mental health services. Spending on community mental health services increased over this study period, but mental health legislation continues to be restrictive. Further study is needed to determine if the increase in spending, on one hand, or the nature of mental health legislation, on the other, has had direct effects on the rate of MAH over time.
MAH perpetrators were most often diagnosed with a psychotic disorder, and the homicide offense almost always represented their first presentation to forensic mental health services. Nielssen and Large27 found that 40% of MAHs were committed by people with a psychotic illness before treatment had been received; in a Canadian context, a sample of first-episode psychosis patients in 3 Ontario cities had a mean duration of untreated psychosis of 66 months.28 Data from our forensic patient population (n = 370) show that the average duration of active symptoms prior to receiving inpatient care is lengthy (mean [SD], 3.60 [4.89] years) and suggests that access to early engagement with mental health services may be one of the most important factors in reducing MAH as well as other types of violent offending among those with SMI. Factors that influence access include stigma, recognition of early symptoms, and easy access to first-episode care, issues that have been roundly criticized in Ontario.29
Alongside psychosis, we observed rising comorbid substance misuse in the MAH population. Similar findings have been reported among homicide offenders with schizophrenia in England and Wales.30 Drug and alcohol misuse can trigger or exacerbate symptoms of psychosis and confer additional violence risk for persons with psychosis.6,31–33 It is possible that rising substance misuse may have contributed to poorer outcomes for a subset of persons with SMI, effectively blunting a reduction in MAH that might otherwise have occurred with improved community mental health service provision. Over this study period, Ontario has seen a large rise in immigration with increasing social diversity and diagnostic complexity among those who have a mental illness and who commit homicide. The higher rate of substance misuse may have worsened outcomes of psychotic illness for those presenting with higher levels of diagnostic complexity, at the same time as improved resourcing for mental health services may have lessened the burden of illness on others.
The study has limitations. First, the low base rate and variance associated with the rate of MAH in this study may have suppressed the magnitude of association observed with the indicators of psychiatric service utilisation examined. Second, the Homicide Survey is of accused, not convicted, offenders, which leaves open some variations in rates. However, when analyses were performed using victim or perpetrator rates, the results were unchanged. We also did not have access to the murder-suicide population. This group has been found to have features of both mentally normal and abnormal homicide profiles.34 Furthermore, there is a lack of good-quality health sector data on community service expenditures, psychiatric service levels and utilisation over time, and an absence of data on the rates of civil commitment orders. Improved measures of community mental health service provision and civil commitment use in Ontario would permit a better exploration of the interplay between these factors, as well as their relation to SMI-related violence.
Conclusions
Notwithstanding the limitations delineated above, this the first North American study to examine population-based rates of MAH over time and in relation to population homicide rates, indicators of mental health service provision, and criminal justice involvement. The implication that SMI has not contributed to an increase in societal risk over the past 25 years is an important public health message and of reassurance to the movement to eliminate stigma against people with SMI. Rather than reinstitutionalising patients, current findings suggest that improving services to reduce the duration of untreated psychosis and substance misuse may be more effective treatment objectives to address the problem of SMI-related violence.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. McGinty EE, Webster DW, Jarlenski M, et al. News media framing of serious mental illness and gun violence in the United States, 1997-2012. Am J Public Health. 2014;104(3):406–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Torrey EF. Violent behavior by individuals with serious mental illness. Psychiatr Serv. 1994;45(7):653–662. [DOI] [PubMed] [Google Scholar]
- 3. Taylor PJ, Gunn J. Homicides by people with mental illness: myth and reality. Br J Psychiatry. 1999;174(1):9–14. [DOI] [PubMed] [Google Scholar]
- 4. Simpson AIF, McKenna B, Moskowitz A, et al. Homicide and mental illness in New Zealand, 1970-2000. Br J Psychiatry. 2004;185(5):394–398. [DOI] [PubMed] [Google Scholar]
- 5. Large M, Smith G, Swinson N, et al. Homicide due to mental disorder in England and Wales over 50 years. Br J Psychiatry. 2008;193(2):130–133. [DOI] [PubMed] [Google Scholar]
- 6. Mullen PE, Burgess P, Wallace C, et al. Community care and criminal offending in schizophrenia. Lancet. 2000;355(9204):614–617. [DOI] [PubMed] [Google Scholar]
- 7. Wallace C, Mullen PE, Burgess P. Criminal offending in schizophrenia over a 25-year period marked by deinstitutionalization and increasing prevalence of comorbid substance use disorders. Am J Psychiatry. 2004;161(4):716–727. [DOI] [PubMed] [Google Scholar]
- 8. Erb M, Hodgins S, Freese R, et al. Homicide and schizophrenia: maybe treatment does have a preventive effect. Crim Behav Ment Health. 2001;11(1):6–26. [DOI] [PubMed] [Google Scholar]
- 9. Coid J. The epidemiology of abnormal homicide and murder followed by suicide. Psychol Med. 1983;13(4):855–860. [DOI] [PubMed] [Google Scholar]
- 10. Large M, Smith G, Nielssen O. The relationship between the rate of homicide by those with schizophrenia and the overall homicide rate: a systematic review and meta-analysis. Schizophr Res. 2009;112(1):123–129. [DOI] [PubMed] [Google Scholar]
- 11. Bonta J, Law M, Hanson K. The prediction of criminal and violent recidivism among mentally disordered offenders: a meta-analysis. Psychol Bull. 1998;123(2):123–142. [DOI] [PubMed] [Google Scholar]
- 12. Fisher WH, Silver E, Wolff N. Beyond criminalization: Toward a criminologically informed framework for mental health policy and services research. Adm Policy Ment Health. 2006;33(5):544–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Junginger J, Claypoole K, Laygo R, et al. Effects of serious mental illness and substance abuse on criminal offenses. Psychiatr Serv. 2006;57(6):879–882. [DOI] [PubMed] [Google Scholar]
- 14. Segal SP. Civil commitment law, mental health services, and US homicide rates. Soc Psychiatry Psychiatr Epidemiol. 2012;47(9):1449–1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fazel S, Zetterqvist J, Larsson H, et al. Antipsychotics, mood stabilisers, and risk of violent crime. Lancet. 2014;384(9949):1206–1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Igoumenou A, Kallis C, Coid J. Treatment of psychosis in prisons and violent recidivism. BJPsych Open. 2015;1(2):149–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sealy P, Whitehead PC. Forty years of deinstitutionalization of psychiatric services in Canada: an empirical assessment. Can J Psychiatry. 2004;49(4):249–257. [DOI] [PubMed] [Google Scholar]
- 18. Winick BJ. Civil commitment. A therapeutic jurisprudence model. Durham (NC): Carolina Academic; 2005. [Google Scholar]
- 19. Gray JE, O’Reilly RL. Supreme Court of Canada’s “beautiful mind” case. Int J Law Psychiatry. 2009;32(5):315–322. [DOI] [PubMed] [Google Scholar]
- 20. Monahan J, Redlich AD, Swanson J, et al. Use of leverage to improve adherence to psychiatric treatment in the community. Psychiatr Serv. 2005;56(1):37–44. [DOI] [PubMed] [Google Scholar]
- 21. R. v M’Naghten, 10 Cl. and F. 200, 8 Eng.Rep. 718 (1843).
- 22. Statistics Canada. Adult correctional services, average counts of adults in provincial and territorial programs (2015); [cited 2015 Mar 20]. Available from: http://www.statcan.gc.ca/daily-quotidien/170301/dq170301c-cansim-eng.htm
- 23. R Core Team. R: A language and environment for statistical computing. Vienna (Austria): R Foundation for Statistical Computing; 2014. [Google Scholar]
- 24. Penrose LS. Mental disease and crime: outline of a comparative study of European statistics. Br J Med Psychol. 1939;18(1):1–15. [Google Scholar]
- 25. Crocker AG, Nicholls TL, Seto MC, et al. The national trajectory project of individuals found not criminally responsible on account of mental disorder in Canada. Part 2: the people behind the label. Can J Psychiatry. 2015;60(3):106–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fazel S, Buxrud P, Ruchkin V, et al. Homicide in discharged patients with schizophrenia and other psychoses: a national case-control study. Schizophr Res. 2010;123(2):263–269. [DOI] [PubMed] [Google Scholar]
- 27. Nielssen O, Large M. Rates of homicide during the first episode of psychosis and after treatment: a systematic review and meta-analysis. Schizophr Bull. 2010;36(4):702–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Malla A, Schmitz N, Norman R, et al. A multisite Canadian study of outcome of first-episode psychosis treated in publicly funded early intervention services. Can J Psychiatry. 2007;52(9):563–571. [DOI] [PubMed] [Google Scholar]
- 29. Select Committee on Mental Health and Addictions. Navigating the journey to wellness: the comprehensive mental health and addictions action plan for Ontarians (2009); [cited 2017 Feb 6]. Available from http://www.ontla.on.ca/committee-proceedings/committee-reports/files_pdf/Select%20Report%20ENG.pdf
- 30. Swinson N, Flynn SM, While D, et al. Trends in rates of mental illness in homicide perpetrators. Br J Psychiatry. 2011;198(6):485–489. [DOI] [PubMed] [Google Scholar]
- 31. Elbogen EB, Johnson SC. The intricate link between violence and mental disorder: results from the national epidemiologic survey on alcohol and related condition. Arch Gen Psychiatry. 2009;66(2):152–161. [DOI] [PubMed] [Google Scholar]
- 32. Eronen M, Tilhonen J, Hakola P. Schizophrenia and homicidal behavior. Schizophr Bull. 1996;22(1):83–89. [DOI] [PubMed] [Google Scholar]
- 33. Van Dorn R, Volavka J, Johnson N. Mental disorder and violence: is there a relationship beyond substance use? Soc Psychiatry Psychiatr Epidemiol. 2012;47(3):487–503. [DOI] [PubMed] [Google Scholar]
- 34. Moskowitz A, Simpson AIF, McKenna B, et al. The role of mental illness in homicide-suicide in New Zealand, 1991-2000. J Forens Psychiatry Psychol. 2006;17(3):417–430. [Google Scholar]