Abstract
Objective:
There is a dearth of information on people with first-episode psychosis who do not access specialized early psychosis intervention (EPI) services. We sought to estimate the proportion of incident cases of nonaffective psychosis that do not access these services and to examine factors associated with EPI admission.
Methods:
Using health administrative data, we constructed a retrospective cohort of incident cases of nonaffective psychosis in the catchment area of the Prevention and Early Intervention Program for Psychoses (PEPP) in London, Ontario, between 1997 and 2013. This cohort was linked to primary data from PEPP to identify EPI users. We used multivariate logistic regression to model sociodemographic and service factors associated with EPI admission.
Results:
Over 50% of suspected cases of nonaffective psychosis did not have contact with EPI services for screening or admission. EPI users were significantly younger, more likely to be male (odds ratio [OR] 1.58; 95% confidence interval [CI] 1.24 to 2.01), and less likely to live in areas of socioeconomic deprivation (OR 0.51; 95% CI 0.36 to 0.73). EPI users also had higher odds of psychiatrist involvement at the index diagnosis (OR 7.35; 95% CI 5.43 to 10.00), had lower odds of receiving the index diagnosis in an outpatient setting (OR 0.50; 95% CI 0.38 to 0.65), and had lower odds of prior alcohol-related (OR 0.42; 95% CI 0.28 to 0.63) and substance-related (OR 0.68; 95% CI 0.50 to 0.93) disorders.
Conclusions:
We need a greater consideration of patients with first-episode psychosis who are not accessing EPI services. Our findings suggest that this group is sizable, and there may be sociodemographic and clinical disparities in access. Nonpsychiatric health professionals could be targeted with interventions aimed at increasing detection and referral rates.
Keywords: first-episode psychosis, early intervention, access to care, health administrative data
Abstract
Objectif :
Il y a une pénurie d’information sur les personnes au premier épisode de psychose qui n’ont pas accès à des services spécialisés d’intervention en psychose précoce (IPP). Nous avons cherché à estimer la proportion de cas incidents de psychose non affective qui n’ont pas accès à ces services, et à examiner les facteurs associés à une hospitalisation pour IPP.
Méthodes:
À l’aide de données de santé administratives, nous avons construit une cohorte rétrospective de cas incidents de psychose non affective dans la région du programme d’intervention précoce pour les psychoses (PEPP) de London, Ontario, entre 1997 et 2013. Cette cohorte a été liée aux données primaires du PEPP pour identifier les utilisateurs d’IPP. Nous avons utilisé la régression logistique multivariée pour modeler les facteurs sociodémographiques et des services associés à l’hospitalisation pour IPP.
Résultats:
Plus de 50 % des cas soupçonnés de psychose non affective n’ont pas eu de contact avec le programme d’IPP pour un dépistage ou une hospitalisation. Les utilisateurs d’IPP sont significativement plus jeunes, plus susceptibles d’être de sexe masculin (RC = 1,58; IC à 95 % 1,24 à 2,01), et moins susceptibles d’habiter dans une région socio-économique défavorisée (RC = 0,51; IC à 95 % 0,36 à 0,73). Les utilisateurs d’IPP avaient aussi des probabilités plus élevées de voir un psychiatre au premier diagnostic (RC = 7,35; IC à 95 % 5,43 à 10,00), avaient moins de probabilités de recevoir le premier diagnostic dans un contexte ambulatoire (RC = 0,50; IC à 95 % 0,38 à 0,65), et avaient moins de probabilités de troubles antérieurs liés à l’alcool (RC = 0,42; IC à 95 % 0,28 à 0,63) et à une substance (RC = 0,68; IC à 95 % 0,50 à 0,93).
Conclusions:
Nous devons tenir compte davantage des patients au premier épisode de psychose qui n’ont pas accès aux services d’IPP – nos résultats suggèrent qu’il s’agit d’un groupe considérable, et qu’il peut y avoir des disparités sociodémographiques et cliniques de l’accès. Les professionnels de la santé non psychiatriques pourraient être ciblés pour des interventions visant à accroître les taux de détection et de référence.
Early psychosis intervention (EPI) services have been implemented in numerous countries around the world, reflecting optimism about the prospects for recovery if comprehensive care is offered early in the course of the illness. These programs are based on evidence that illness trajectories are determined in the first 2 to 5 years after onset1 and that delays in treatment of the first episode are associated with poor clinical and functional outcomes.2–4 These services provide comprehensive phase-specific treatment during the early stages of illness5 and have been shown to be both effective6–8 and cost-effective9–12 for improving outcomes in first-episode psychosis. Some jurisdictions have also demonstrated the benefits of going beyond EPI services through initiatives such as informational campaigns, which have been shown to increase the case identification and referral rate to EPI services.13
There is a large body of evidence suggesting that sociodemographic-, clinical-, and service-level factors impact the pathways to specialized care for people with first-episode psychosis.14–16 However, less is known about the accessibility of EPI services, including information about people with first-episode psychosis who are not in EPI services and who instead receive care from other service providers or no care at all. In fact, we are not aware of any prior studies that have attempted to examine disparities in access to EPI services. With this notable gap in knowledge comes the implicit assumption that nearly all cases of first-episode psychosis are detected and treated by these programs.
The current study addresses this gap in knowledge by linking primary data from an EPI program to population-based health administrative data. The objectives of the current study were 1) to estimate the proportion of incident cases of nonaffective psychotic disorder that access EPI services and 2) to examine the sociodemographic-, clinical-, and service-level factors that are associated with the use of these services. We hypothesized a priori that most patients with first-episode psychosis were using EPI services and that there would be significant differences in the characteristics of users and nonusers of EPI services.
Methods
Study Setting
The hospital-based Prevention and Early Intervention Program for Psychoses (PEPP) in London, Ontario, is the only EPI program serving a defined catchment area of nearly 425 000 people. Core features of PEPP include early case detection, rapid assessment of suspected cases, and provision of comprehensive pharmacological and psychosocial interventions using assertive case management.17 PEPP was established in 1997 to provide services to people with first-episode psychosis who meet the following inclusion criteria: a) aged 16 to 50 years; b) diagnosis of nonaffective psychotic disorder; c) less than 30 days of prior treatment with antipsychotic medication; d) absence of a developmental disability or organic psychosis; and e) no outstanding criminal charges that would warrant ongoing contact with the criminal justice system and consequently prevent engagement with the program. The program does not accept patients with nonaffective psychosis or those who have an attenuated psychosis syndrome. Referrals are accepted from a wide range of medical and nonmedical sources, including self-referral, family members, schools and universities, police services, primary care, and other mental health services.
Cohort Creation
We used a retrospective cohort design to identify incident cases of nonaffective psychotic disorder presenting to services within the EPI catchment area, based on the postal code of health care providers. These encounters are covered by the Ontario Health Insurance Plan, which is the publicly funded universal health system that provides medically necessary services for nearly the entire population. The cohort was constructed using linked population-based health administrative data from the Institute for Clinical Evaluative Sciences (ICES) composed of the following databases:
The Registered Persons Database (1990–2014) includes age at the index diagnosis, gender, rural residence, neighbourhood-level income quintile, and mortality information, where relevant.
The Immigration, Refugees and Citizenship Canada (1985–2014) includes information on all migrants who landed in Ontario.
The Ontario Health Insurance Plan (1991–2014) contains information on all physician services and outpatient visits.
The Ontario Mental Health Reporting System (2005–2014) contains information on inpatient mental health hospitalizations to designated psychiatry beds.
The Discharge Abstract Database (1988–2014) includes data on acute hospitalizations not reported to the Ontario Mental Health Reporting System and psychiatric hospitalizations prior to 2005.
The National Ambulatory Care Reporting System (2000–2014) contains information on visits to the emergency department (ED).
Using these databases, we identified cases arising since the inception of the program (1997–2013), defined as people between the ages of 16 and 50 years with either A) 1 hospitalization with a primary discharge diagnosis of nonaffective psychosis or B) at least 2 physician or ED visits for nonaffective psychosis in any 12-month period. This algorithm has been previously validated against medical chart diagnoses for the identification of patients with psychotic disorders.18 Cases were excluded if there was a diagnosis of nonaffective psychosis prior to cohort inception, and the exclusion period for prevalent cases was up to 20 years depending on the year of onset and the database used. The date of the first hospitalization or physician visit for a psychotic disorder was assigned as the index date.
As a post hoc exclusion, we removed people from the cohort who had never had their diagnosis confirmed by either a psychiatrist or an inpatient admission and had no service contacts for nonaffective psychosis after meeting our case definition, as these people were likely “false positives.” We also excluded people who had fewer than 2 contacts with any type of service in the catchment area in the 6-month period after their index diagnosis, as these people were considered lost to follow-up.
EPI Program Data Linkage
The cohort was linked to primary data from the EPI program. There is no means of identifying program clients in the administrative databases, so this linkage was required to identify EPI clients. A deterministic linkage was performed using health insurance numbers (96% linkage rate), and the data were subsequently encrypted to protect privacy as per ICES data linkage protocols. People within the cohort who were also represented in the PEPP data were classified as EPI users.
To rule out people who had been screened for the program but were subsequently found to be ineligible, we linked the physician registration numbers and dates of tenure of all psychiatrists working in the EPI program. The intake process involves an initial consultation with a program psychiatrist once the client has met the preliminary screening criteria. Program psychiatrists would generally not have been seeing patients outside of the context of the program. Thus, all people who were not admitted to the program, but who had a visit with a program psychiatrist on record, were classified as EPI screened. All remaining cohort members were classified as nonusers of EPI services.
The Health Sciences Research Ethics Board at the University of Western Ontario granted approval for the linkage of primary data to the ICES data holdings. Patient-level data were linked using unique coded identifiers, and the de-identified data sets were analyzed on site at the ICES. We followed the RECORD guidelines for observational studies using routinely collected data (Online Supplement 1), and a description of codes and algorithms used to create the variables is presented in Online Supplement 2.
Sociodemographic-, Clinical-, and Service-Level Variables
We extracted available sociodemographic data, including age at the index date, gender, neighbourhood-level income quintile, migrant status, rurality of residence, and whether the primary place of residence was outside of the EPI catchment area. We also extracted information on several clinical factors, including the type of index diagnosis (schizophrenia, delusional disorder, other), whether the index diagnosis was made by a psychiatrist, location of the index diagnosis (inpatient v. outpatient), and whether there was a history of contact with services for an alcohol- or substance-related disorder. Finally, we constructed several binary indicators of service use for other mental health reasons in the 6-month period prior to the index diagnosis, including whether there was a family physician, psychiatrist, or ED visit for a mental health reason as well as prior psychiatric hospitalizations.
Statistical Analyses
We compared the sociodemographic, clinical, and service use characteristics of EPI users and nonusers with standardized differences, and values of greater than 10% were considered indicative of significant between-group differences.19 There were minimal missing data (<1%) for the covariates of interest, and those with missing data were excluded.
We used logistic regression models to examine the association between the sociodemographic, clinical, and service use factors and the odds of admission to the EPI program. We computed unadjusted, sociodemographic-adjusted, clinical-adjusted, service-adjusted, and fully adjusted models. However, the findings did not differ substantially across the analyses; therefore, we present the results of the fully adjusted model. All results are presented as odds ratios (ORs) with corresponding 95% confidence intervals (CIs), with the models comparing EPI users to a nonuser reference group. Analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
Results
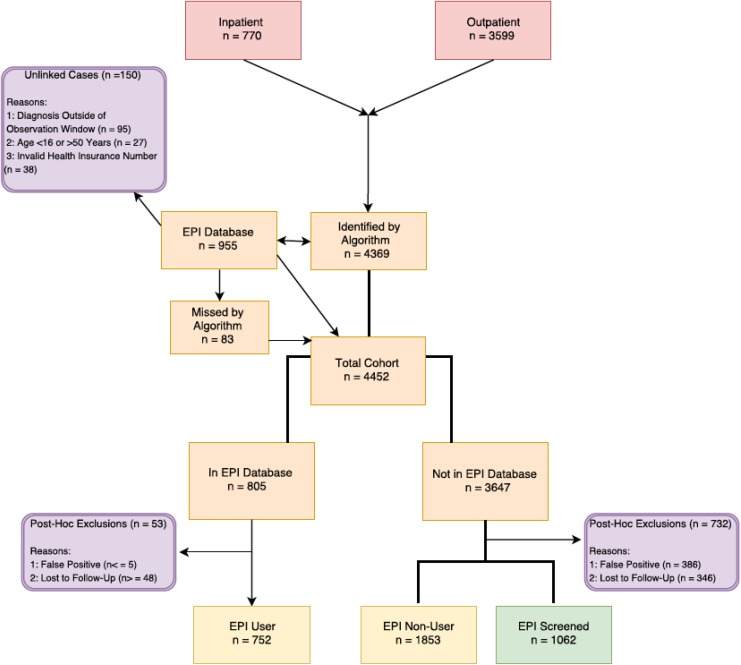
A flowchart showing the construction of our study cohort is presented in Figure 1. Our final sample was composed of 752 EPI users, 1062 EPI-screened people, and 1853 nonusers. These numbers indicate that over 50% of suspected cases of incident nonaffective psychosis do not have contact with the EPI program for screening or admission.
Figure 1.
Flowchart showing the creation of the study cohort of incident cases of nonaffective psychotic disorder in the catchment area of the Prevention and Early Intervention for Psychosis Program (PEPP) between 1997 and 2013. Cases were identified by a validated algorithm in the health administrative data, and this cohort was linked to primary data from the PEPP to identify users of early psychosis intervention (EPI) services. We excluded people who had never had the diagnosis of a psychotic disorder confirmed by a psychiatrist and had no subsequent contacts for psychosis after entering the study cohort (false positives). We also excluded people who had fewer than 2 contacts with any type of health services in the catchment area after the diagnosis (lost to follow-up). We additionally removed people who had contact with a PEPP psychiatrist but were not admitted to the program (EPI screened), for a final comparison of EPI users and nonusers.
The baseline characteristics of the study sample are presented in Table 1, and the results of the multivariate logistic regression analysis are presented in Table 2. Our findings suggest a clear gradient by age, with decreasing odds of being treated in the EPI program across increasing age strata (age 46–50 years v. age 16–20 years: OR 0.03; 95% CI 0.01 to 0.05). In comparison to nonusers, EPI users were more likely to be male (OR 1.58; 95% CI 1.24 to 2.01) and less likely to have their primary residence outside of the program catchment area (OR 0.21; 95% CI 0.15 to 0.29). We also found a gradient by neighbourhood-level income quintile, and those living in the most deprived areas were half as likely to be an EPI user as those living in the least deprived areas (OR 0.51; 95% CI 0.36 to 0.73). We did not find evidence of differences by migrant status or rurality of residence.
Table 1.
Baseline sociodemographic, clinical, and service use characteristics of users and nonusers of EPI services.
| EPI user (n = 752) | EPI nonuser (n = 1853) | Standardized difference, % | |
|---|---|---|---|
| Age at index date | |||
| 16 to 20 years | 306 (40.7) | 214 (11.5) | 70 |
| 21 to 25 years | 212 (28.2) | 241 (13.0) | 38 |
| 26 to 30 years | 96 (12.8) | 227 (12.3) | 2 |
| 31 to 35 years | 64 (8.5) | 265 (14.3) | 18 |
| 36 to 40 years | 38 (5.1) | 274 (14.8) | 33 |
| 41 to 45 years | 25 (3.3) | 290 (15.7) | 43 |
| 46 to 50 years | 11 (1.5) | 342 (18.5) | 59 |
| Male gender | 558 (74.2) | 996 (53.8) | 44 |
| Rural residence | 54 (7.2) | 163 (8.8) | 6 |
| Resides outside of catchment | 92 (12.2) | 521 (28.1) | 40 |
| Income quintile | |||
| Highest (5) | 140 (18.6) | 222 (12.0) | 19 |
| 4 | 110 (14.6) | 262 (14.1) | 1 |
| 3 | 146 (19.4) | 350 (18.9) | 1 |
| 2 | 110 (14.6) | 262 (14.1) | 0 |
| Lowest (1) | 140 (18.6) | 222 (12.0) | 17 |
| Migrant status | |||
| Nonmigrant | 669 (89.0) | 1682 (90.8) | 6 |
| Immigrant | 47 (6.3) | 102 (5.5) | 3 |
| Refugee | 36 (4.8) | 69 (3.7) | 5 |
| Index diagnosis | |||
| Schizophrenia | 277 (36.8) | 768 (41.4) | 9 |
| Delusional disorder | 52 (6.9) | 163 (8.8) | 7 |
| Other psychosis | 423 (56.3) | 922 (49.8) | 13 |
| Diagnosing physician | |||
| Family physician | 30 (4.0) | 589 (31.8) | 78 |
| Psychiatrist | 616 (81.9) | 797 (43.0) | 88 |
| Family physician + psychiatrist | 58 (7.7) | 94 (5.1) | 11 |
| Other | 48 (6.4) | 373 (20.1) | 41 |
| Inpatient at index diagnosis | 271 (36.0) | 241 (13.0) | 56 |
| Prior alcohol-related disorder | 50 (6.6) | 366 (19.8) | 39 |
| Prior substance-related disorder | 107 (14.2) | 504 (27.2) | 32 |
| Primary care contact in previous 6 months | 249 (33.1) | 859 (46.4) | 27 |
| Psychiatrist contact in previous 6 months | 162 (21.5) | 600 (32.4) | 25 |
| Any ED visit in previous 6 months | 89 (11.8) | 242 (13.1) | 4 |
| Any hospitalization in previous 6 months | 25 (3.3) | 133 (7.2) | 17 |
Data are shown as n (%) unless otherwise specified. ED = emergency department; EPI = early psychosis intervention.
Table 2.
Fully adjusted model of factors associated with admission to an EPI program relative to nonusers of EPI services.
| OR (95% CI) | |
|---|---|
| Age at index date | |
| 16 to 20 years | Reference |
| 21 to 25 years | 0.62 (0.45 to 0.84) |
| 26 to 30 years | 0.35 (0.24 to 0.50) |
| 31 to 35 years | 0.17 (0.11 to 0.24) |
| 36 to 40 years | 0.09 (0.06 to 0.14) |
| 41 to 45 years | 0.06 (0.04 to 0.10) |
| 46 to 50 years | 0.03 (0.01 to 0.05) |
| Male gender | 1.58 (1.24 to 2.01) |
| Rural residence | 1.55 (0.98 to 2.46) |
| Resides outside of catchment | 0.21 (0.15 to 0.29) |
| Income quintile | |
| Highest (5) | Reference |
| 4 | 0.66 (0.44 to 0.99) |
| 3 | 0.63 (0.43 to 0.91) |
| 2 | 0.57 (0.40 to 0.82) |
| Lowest (1) | 0.51 (0.36 to 0.73) |
| Migrant status | |
| Nonmigrant | Reference |
| Immigrant | 0.71 (0.45 to 1.12) |
| Refugee | 0.97 (0.58 to 1.65) |
| Index diagnosis | |
| Schizophrenia | Reference |
| Delusional disorder | 0.81 (0.52 to 1.24) |
| Other psychosis | 0.90 (0.71 to 1.16) |
| Index diagnosis by psychiatrist | 7.35 (5.43 to 10.00) |
| Outpatient at index diagnosis | 0.50 (0.38 to 0.65) |
| History of alcohol-related disorder | 0.42 (0.28 to 0.63) |
| History of substance-related disorder | 0.68 (0.50 to 0.93) |
| Year (1997 to 2013) | 1.00 (0.98 to 1.02) |
| Family physician visit in previous 6 months | 0.90 (0.71 to 1.14) |
| Psychiatrist visit in previous 6 months | 0.56 (0.43 to 0.73) |
| ED visit in previous 6 months | 0.96 (0.67 to 1.36) |
| Hospitalization in previous 6 months | 0.70 (0.40 to 1.21) |
CI = confidence interval; ED = emergency department; EPI = early psychosis intervention; OR = odds ratio.
EPI users were much more likely to have received their index diagnosis of a psychotic disorder from a psychiatrist (OR 7.35; 95% CI 5.43 to 10.00) relative to nonusers. This includes a diagnosis by a psychiatrist from an inpatient psychiatric admission (36%) or by a psychiatrist via an outpatient or ED visit (64%) and also includes the possibility that the index diagnosis occurred at first contact with an EPI psychiatrist (1.5% of all EPI users). EPI users were less likely to have outpatient status at the index diagnosis (OR 0.50; 95% CI 0.38 to 0.65) and were also less likely to have a history of contact with services for alcohol-related (OR 0.42; 95% CI 0.28 to 0.63) or substance-related disorders (OR 0.68; 95% CI 0.50 to 0.93). We did not observe differences by type of diagnosis or year of onset in the odds of EPI service use.
There were few differences between EPI users and nonusers in prior contacts with mental health services. Of exception, people who were receiving ongoing care from a psychiatrist for other mental health reasons in the 6-month period preceding the index diagnosis of psychosis were less likely to be an EPI user (OR 0.56; 95% CI 0.43 to 0.73).
Discussion
Much of the prior research on EPI services is predicated on the belief that nearly all patients with first-episode psychosis are represented in these services, with a notable lack of consideration of people who may be receiving care elsewhere in the health system. Contrary to our initial hypothesis, we found that nearly half of people with an incident diagnosis of nonaffective psychosis are not accessing EPI services for screening or admission. However, consistent with our second hypothesis, we found evidence of sociodemographic disparities in access to EPI services: nonusers were more likely to be female, older at first onset, and live in the most socioeconomically deprived areas of the catchment area. We also found that access varies by clinical factors, namely, acute presentation necessitating inpatient treatment, involvement of a psychiatrist at the index diagnosis of a psychotic disorder, and absence of comorbid alcohol- and substance-related disorders. Follow-up data from this cohort suggest that EPI users have better outcomes across several indicators relative to nonusers in the first 2 years after program admission. Using propensity score matching to make the groups more comparable on sociodemographic, clinical, and service use characteristics, we found that EPI users had more rapid access to psychiatric services, lower rates of ED visits for mental health reasons, and lower rates of all-cause mortality.20 Thus, reducing the observed disparities in access to EPI services could have significant impacts across the larger health system context.
Factors Associated With EPI Admission
Although the upper age limit for many EPI programs in Ontario and elsewhere is 35 years,21 PEPP had an upper age limit of 50 years during the period of this study. Despite this extended age criterion, our findings suggest that people who are older at first onset are not accessing the EPI program. It has been suggested that “early intervention” has become synonymous with “intervention in youth,”21 and service providers in our study may have been under the false impression that EPI was not suitable for patients who experience a first episode later in life. Alternatively, prior research suggests that people under the age of 35 years are more likely to be hospitalized for first-episode psychosis,21 which may have increased the likelihood of being detected by the EPI program. We found that people with an inpatient admission at the index diagnosis were more likely to be an EPI user.
This age effect also functions to disproportionately exclude women; men had a nearly 50% greater odds of EPI admission. It is well established that the age of onset of a psychotic disorder is later among women,22 and it has been estimated that 1 in 3 women with first-episode psychosis, and 1 in 5 men, will be excluded from EPI services using an upper age limit of 35 years.21 Women with first-episode psychosis have been found to have better premorbid functioning22 as well as a higher level of social functioning and a greater likelihood of engagement in employment or education at 5-year follow-up.23 It is possible that women have a more benign course of illness that may be amenable to treatment in less specialized settings, thereby accounting for the large proportion of women in our nonuser group.
Finally, our findings highlight stark disparities in access to EPI services across socioeconomic strata. People living in the most deprived areas were half as likely to be admitted to EPI services relative to those in the least deprived areas. Socioeconomic status is an established risk factor for psychotic disorders,24,25 although its impact on access to care for people with first-episode psychosis has been unclear in the literature to date.14 Targeted education programs with service providers have been shown to be effective for increasing the number of EPI referrals of clients with a low socioeconomic status26 and could be one avenue for reducing these disparities in access to care.
Clinical and Research Implications
Our findings have significant implications for EPI service planning; we estimate that there are a substantial number of additional people who would meet the eligibility criteria for EPI services, and this potential demand may exceed the capacity of established programs. Indeed, reports from other jurisdictions suggest that the estimates used for service planning are far lower than the actual number of cases presenting to services.27,28 Irrespective of whether the nonusers are true cases of first-episode psychosis, a much larger proportion should be referred to the EPI program for screening, which will place additional demands on program resources. Additionally, adaptations to the EPI model of care may be warranted if the services are not seen as acceptable or relevant to particular subgroups, such as older women.
Our findings also highlight the need for EPI programs to be engaging in ongoing outreach to service providers in other sectors, particularly primary care. The EPI program had been initially engaged in a community-wide outreach program29; however, the frequency and intensity of this outreach have declined over time. A post hoc examination of the number of cases per year suggests that the proportion of nonusers has increased over time, with declining numbers of people in the EPI-screened group and stable numbers in the EPI user group (data available on request). Nearly half of our sample had a family physician involved in the index diagnosis of a psychotic disorder, a large proportion of whom were nonusers, and prior research suggests that informational campaigns are effective at improving detection and referral rates in primary care.13 Outreach to other psychiatric professionals may also be warranted. Although psychiatrist involvement at the index diagnosis drastically increases access to EPI services, those who were receiving ongoing care from a psychiatrist for other mental health reasons in the 6 months prior to the index diagnosis were less likely to access EPI services. This aligns with previous findings that ongoing psychiatric care at the onset of psychosis extends the treatment delay,30,31 which may arise from difficulties recognizing and responding to changes in symptoms or an inability to convince patients to change service providers once a therapeutic relationship has been established.30 Ongoing outreach to service providers appears to be warranted, even for well-established EPI programs. Indeed, public education is one of the government standards for EPI services in Ontario,32 and results from a survey of EPI services across the province suggest that community outreach is a struggle for many programs.33
Our findings also have implications for research in the field of first-episode psychosis. We need accurate population-based estimates of the epidemiology of psychotic disorders to allow service planners and administrators to more effectively resource EPI services and evaluate their coverage. Although not mentioned in the Ontario standards,32 the EPI standards from the National Institute for Health and Care Excellence in the United Kingom,34 as well as the First Episode Psychosis Services Fidelity Scale,35 highlight the need for accurate data on psychosis incidence to allow for an assessment of the needs of the local population and the coverage of the program. Additionally, investigators studying samples drawn from EPI programs need to consider that this may represent a select subset of people with psychotic disorders who differ on sociodemographic and clinical factors. This will impact the generalizability of research findings to the broader population of people with psychosis.
Strengths and Limitations
To our knowledge, our study is the first to examine disparities in access to EPI services. Our findings are strengthened by a population-based database with linkage of primary data from a well-established and long-standing EPI program.
The most notable limitation to our findings is that we do not have information on the reasons behind the nonuse of EPI services, which is an essential avenue for future research to better inform service planning and outreach strategies. Studies employing qualitative or mixed-method designs would be particularly informative for understanding the trends that we observed. We are limited by the availability of data in the administrative data holdings and therefore are likely missing information on other factors that may influence access to EPI services. Potential examples include ethnicity, symptom severity, level of functioning, and family involvement in help-seeking. We did not find evidence of differences by migrant status; however, only a small proportion of our sample were first-generation migrants (11%), and further research with more diverse samples is warranted. Finally, our sample was limited to people with nonaffective psychosis, and our findings may not be generalizable to affective psychotic disorder.
Conclusions
We need a greater consideration of patients with first-episode psychosis who are not accessing EPI services. Our findings highlight gaps in the provision of these services that vary along sociodemographic and clinical lines. Nonpsychiatric health professionals could be targeted with interventions aimed at increasing detection and referral rates to ensure that all people with first-episode psychosis have the opportunity to benefit from early intervention.
Supplemental Material
Online_Supplement_#1 for Disparities in Access to Early Psychosis Intervention Services: Comparison of Service Users and Nonusers in Health Administrative Data by Kelly K. Anderson, Ross Norman, Arlene G. MacDougall, Jordan Edwards, Lena Palaniyappan, Cindy Lau, and Paul Kurdyak in The Canadian Journal of Psychiatry
Supplemental Material
Online_Supplement_#2 for Disparities in Access to Early Psychosis Intervention Services: Comparison of Service Users and Nonusers in Health Administrative Data by Kelly K. Anderson, Ross Norman, Arlene G. MacDougall, Jordan Edwards, Lena Palaniyappan, Cindy Lau, and Paul Kurdyak in The Canadian Journal of Psychiatry
Acknowledgments
This study was conducted at the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by the ICES or the MOHLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors and not necessarily those of the CIHI.
Footnotes
Data Access: The data set from this study is held securely in coded form at the ICES, and the ICES analyst (C.L.) had full access to study data. While data-sharing agreements prohibit the ICES from making the data set publicly available, access can be granted to those who meet prespecified criteria for confidential access, available at www.ices.on.ca/DAS. The full data-set creation plan is available from the authors upon request.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by a New Investigator Fellowship from the Ontario Mental Health Foundation (K.K.A.).
ORCID iD: Kelly K. Anderson, PhD  http://orcid.org/0000-0001-9843-404X
http://orcid.org/0000-0001-9843-404X
Supplemental Material: Supplementary material for this article is available online.
References
- 1. Harrison G. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry. 2001;178(6):506–517. [DOI] [PubMed] [Google Scholar]
- 2. Marshall M, Lewis S, Lockwood A, et al. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry. 2005;62(9):975–983. [DOI] [PubMed] [Google Scholar]
- 3. Perkins DO, Gu H, Boteva K, et al. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry. 2005;162(10):1785–1804. [DOI] [PubMed] [Google Scholar]
- 4. Norman RMG, Lewis SW, Marshall M. Duration of untreated psychosis and its relationship to clinical outcome. Br J Psychiatry. 2005;48:S19–S23. [DOI] [PubMed] [Google Scholar]
- 5. McGorry PD, Killackey E, Yung AR. Early intervention in psychotic disorders: detection and treatment of the first episode and the critical early stages. Med J Aust. 2007;187(Suppl 7):S8–S10. [DOI] [PubMed] [Google Scholar]
- 6. Bird V, Premkumar P, Kendall T, et al. Early intervention services, cognitive-behavioural therapy and family intervention in early psychosis: systematic review. Br J Psychiatry. 2010;197(5):350–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Harvey P, Lepage M, Malla A. Benefits of enriched intervention compared with standard care for patients with recent-onset psychosis: a metaanalytic approach. Can J Psychiatry. 2007;52(7):464–472. [DOI] [PubMed] [Google Scholar]
- 8. Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database Syst Rev. 2011;(6):CD004718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hastrup LH, Kronborg C, Bertelsen M, et al. Cost-effectiveness of early intervention in first-episode psychosis: economic evaluation of a randomised controlled trial (the OPUS study). Br J Psychiatry. 2013;202(1):35–41. [DOI] [PubMed] [Google Scholar]
- 10. Mihalopoulos C, Harris M, Henry L, et al. Is early intervention in psychosis cost-effective over the long term? Schizophr Bull. 2009;35(5):909–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liffick E, Mehdiyoun NF, Vohs JL, et al. Utilization and cost of health care services during the first episode of psychosis. Psychiatr Serv. 2017;68(2):131–136. [DOI] [PubMed] [Google Scholar]
- 12. Tsiachristas A, Thomas T, Leal J, et al. Economic impact of early intervention in psychosis services: results from a longitudinal retrospective controlled study in England. BMJ Open. 2016;6(10):e012611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Joa I, Johannessen JO, Auestad B, et al. The key to reducing duration of untreated first psychosis: information campaigns. Schizophr Bull. 2008;34(3):466–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Anderson KK, Fuhrer R, Malla AK. The pathways to mental health care of first-episode psychosis patients: a systematic review. Psychol Med. 2010;40(10):1585–1597. [DOI] [PubMed] [Google Scholar]
- 15. Anderson KK, Flora N, Archie S, et al. A meta-analysis of ethnic differences in pathways to care at the first episode of psychosis. Acta Psychiatr Scand. 2014;130(4):257–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Singh SP, Grange T. Measuring pathways to care in first-episode psychosis: a systematic review. Schizophr Res. 2006;81(1):75–82. [DOI] [PubMed] [Google Scholar]
- 17. Norman RMG, Manchanda R. Prevention and Early Intervention Program for Psychoses (PEPP). Healthc Q. 2016;18 Spec No:37–41. [DOI] [PubMed] [Google Scholar]
- 18. Kurdyak P, Lin E, Green D, et al. Validation of a population-based algorithm to detect chronic psychotic illness. Can J Psychiatry. 2015;60(8):362–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38(6):1228–1234. [Google Scholar]
- 20. Anderson KK, Norman R, MacDougall A, et al. The “real world” effectiveness of early psychosis intervention services: a comparison of service users and non-users in population-based health administrative data. Am J Psychiatry. In press. [Google Scholar]
- 21. Lappin JM, Heslin M, Jones PB, et al. Outcomes following first-episode psychosis: why we should intervene early in all ages, not only in youth. Aust N Z J Psychiatry. 2016;50(11):1055–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ochoa S, Usall J, Cobo J, et al. Gender differences in schizophrenia and first-episode psychosis: a comprehensive literature review. Schizophr Res Treatment. 2012;2012:916198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Thorup A, Albert N, Bertelsen M, et al. Gender differences in first-episode psychosis at 5-year follow-up-two different courses of disease? Results from the OPUS study at 5-year follow-up. Eur Psychiatry. 2014;29(1):44–51. [DOI] [PubMed] [Google Scholar]
- 24. Anderson KK, Fuhrer R, Abrahamowicz M, et al. The incidence of first-episode schizophrenia-spectrum psychosis in adolescents and young adults in Montreal: an estimate from an administrative claims database. Can J Psychiatry. 2012;57(10):626–633. [DOI] [PubMed] [Google Scholar]
- 25. Kirkbride JB, Hameed Y, Ankireddypalli G, et al. The epidemiology of first-episode psychosis in early intervention in psychosis services: findings from the Social Epidemiology of Psychoses in East Anglia [SEPEA] study. Am J Psychiatry. 2017;174(2):143–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Malla A, Jordan G, Joober R, et al. A controlled evaluation of a targeted early case detection intervention for reducing delay in treatment of first episode psychosis. Soc Psychiatry Psychiatr Epidemiol. 2014;49(11):1711–1718. [DOI] [PubMed] [Google Scholar]
- 27. Cheng F, Kirkbride JB, Lennox BR, et al. Administrative incidence of psychosis assessed in an early intervention service in England: first epidemiological evidence from a diverse, rural and urban setting. Psychol Med. 2011;41(5):949–958. [DOI] [PubMed] [Google Scholar]
- 28. Simon GE, Coleman KJ, Yarborough BJH, et al. First presentation with psychotic symptoms in a population-based sample. Psychiatr Serv. 2017;68(5):456–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Malla A, Norman R, Scholten D, et al. A community intervention for early identification of first episode psychosis: impact on duration of untreated psychosis (DUP) and patient characteristics. Soc Psychiatry Psychiatr Epidemiol. 2005;40(5):337–344. [DOI] [PubMed] [Google Scholar]
- 30. Norman RMG, Malla AK, Verdi MB, et al. Understanding delay in treatment for first-episode psychosis. Psychol Med. 2004;34(2):255–266. [DOI] [PubMed] [Google Scholar]
- 31. Boonstra N, Sterk B, Wunderink L, et al. Association of treatment delay, migration and urbanicity in psychosis. Eur Psychiatry. 2012;27(7):500–505. [DOI] [PubMed] [Google Scholar]
- 32. Ontario Ministry of Health and Long-Term Care. Early psychosis intervention program standards. Toronto: Ontario Ministry of Health and Long-Term Care; 2011. [Google Scholar]
- 33. Durbin J, Selick A, Hierlihy D, et al. A first step in system improvement: a survey of early psychosis intervention programmes in Ontario. Early Interv Psychiatry. 2016;10(6):485–493. [DOI] [PubMed] [Google Scholar]
- 34. National Institute for Health and Care Excellence. Implementing the early intervention in psychosis access and waiting time standard: guidance. London: National Institute for Health and Care Excellence; 2016. [Google Scholar]
- 35. Addington DE, Norman R, Bond GR, et al. Development and testing of the first-episode psychosis services fidelity scale. Psychiatr Serv. 2016;67(9):1023–1025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online_Supplement_#1 for Disparities in Access to Early Psychosis Intervention Services: Comparison of Service Users and Nonusers in Health Administrative Data by Kelly K. Anderson, Ross Norman, Arlene G. MacDougall, Jordan Edwards, Lena Palaniyappan, Cindy Lau, and Paul Kurdyak in The Canadian Journal of Psychiatry
Online_Supplement_#2 for Disparities in Access to Early Psychosis Intervention Services: Comparison of Service Users and Nonusers in Health Administrative Data by Kelly K. Anderson, Ross Norman, Arlene G. MacDougall, Jordan Edwards, Lena Palaniyappan, Cindy Lau, and Paul Kurdyak in The Canadian Journal of Psychiatry