Abstract
A 76-year-old woman was admitted to the hospital four times from November 2007 to June 2009. In this complex case, the patient had silicosis complicated by broncholithiasis, oesophagobronchial fistulas, and relapsed tuberculosis. She had worked as a stone crusher for 3 years and was exposed to a large amount of quartz dust. Barium oesophagography, gastroesophageal endoscopy, and biopsy suggested oesophageal-related chronic inflammation and ulceration, which may have caused the repeated oesophagobronchial fistulas. Bronchoscopy revealed a free broncholithiasis in the left mainstem bronchus. The patient was admitted a fourth time because of silicotuberculosis relapse. After 9 months of antituberculosis treatment, the patient recovered and was still clinically well at the time of this writing.
Keywords: Silicosis, oesophagobronchial fistula, broncholithiasis, tuberculosis
Introduction
We herein describe a case of silicosis complicated by broncholithiasis, oesophagobronchial fistulas, and relapsed tuberculosis. This case illustrates one of the unusual and complex complications of silicosis. In contrast to the findings of similar case reports,1–4 we believe that these silicosis complications were interrelated.
Case report
A 76-year-old woman was initially admitted to the hospital on 9 November 2007 with a 2-week history of acute exacerbation of a chronic cough and dysphagia involving both solids and liquids. She had no haemoptysis, fever, chills, chest pain, or weight loss. Sixty years before presentation, the patient had worked as a stone crusher for 3 years, whereby she was exposed to a large amount of quartz dust without the use of any respiratory protective equipment. In 1969, she was diagnosed with silicosis and tuberculosis; the tuberculosis was treated and remained stable. She experienced no further exposure to dust or other toxic substances. On follow-up, she showed no change in her condition. The patient was a lifelong non-smoker and drank no alcohol. She was taking no medication.
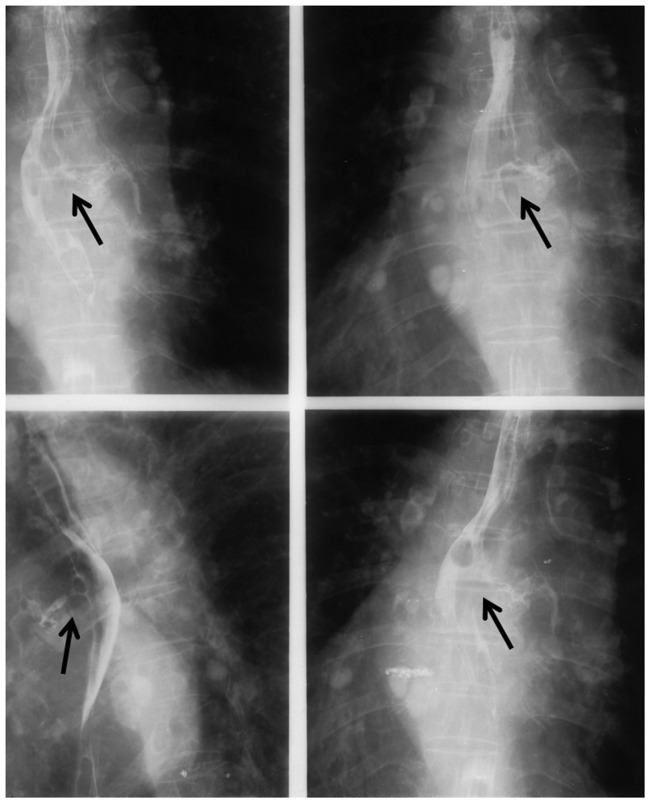
On the current admission to the hospital, the patient appeared well on physical examination and had no palpable peripheral lymph nodes. Occasional wheezing was heard in both lungs. Laboratory data, including blood tests and measurement of serum electrolytes, liver enzymes, bilirubin, and renal function, were normal. A tuberculosis skin test revealed negative results. Three sputum specimens were negative for acid-fast bacilli by staining and culture. Chest radiography and computed tomography demonstrated eggshell calcifications of the hilar and mediastinal lymph nodes in the paratracheal, subcarinal, and aorticopulmonary window regions; bilateral multiple pulmonary nodules were visible. The lower left lobe showed a dense, ground-glass shadow. Barium oesophagography revealed two fistulas between the middle oesophagus and left main bronchus, immediately tracking into the left bronchial tree (Figure 1). The patient was diagnosed with silicosis with oesophagobronchial fistulas and aspiration pneumonitis. She received antibiotics, and an oesophageal stent was placed on 14 December 2007. The patient’s symptoms improved.
Figure 1.
Barium esophagraphy of 2 fistula tracs between the esophagus and bronchus in the patient.
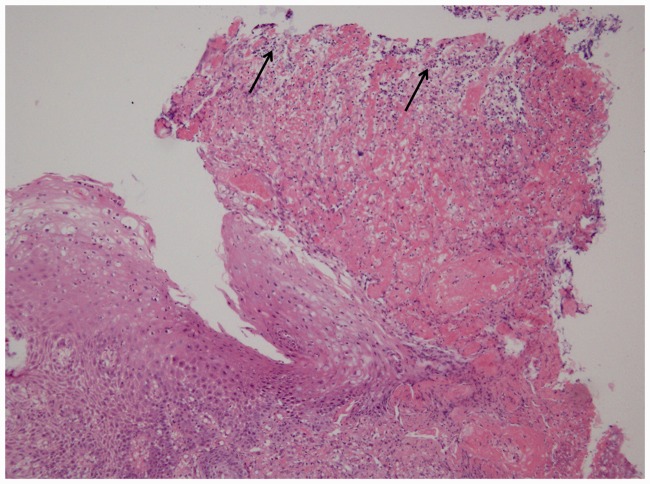
However, her symptoms recurred within 3 days, and gastroesophageal endoscopy demonstrated a small ulcerated lesion above the metallic stents, with a small diverticulum 18 cm from the upper incisor and inflamed and friable oesophageal mucosa. Examination of a biopsy specimen revealed chronic inflammation and an ulcer without granulomas, malignancy, or microorganisms (Figure 2). Another oesophageal stent was placed on 20 December 2007. The patient’s symptoms improved, and she was discharged from the hospital.
Figure 2.
Histological examination of esophagealbiopsy: moderate chronic inflammation and ulceration of esophageal squamous epithelium.
The patient was readmitted 2 months later, this time to another hospital because of a severe cough exacerbated by swallowing liquids and solid food. Gastroesophageal endoscopy revealed a new small mid-oesophageal ulcer. Other examination findings were normal, including the results of tumour marker tests. A tuberculin skin test produced negative results. During the next few days, the patient reported episodes of coughing and expectoration of small calculi with a greyish colour and stony consistency, resembling “coral,” about 5 to 10 mm in diameter. Bronchoscopic examination showed a free broncholithiasis in the left mainstem bronchus and mucosal thickening and stenosis, with no significant airway obstruction of the mainstem bronchus. The broncholithiasis was extracted with no bleeding. Biopsy of the bronchus revealed chronic inflammation with no evidence of malignant tumour cells or granulomas. Sputum and bronchoalveolar lavage analyses revealed no Mycobacterium tuberculosis, fungi, or malignant tumour cells. The patient was diagnosed with silicosis with broncholithiasis and oesophagobronchial fistulas
The patient continued to have frequent complications, and the fistulas remained persistent; this was probably related to stasis in the oesophagus. A more conservative operative approach was initiated because of the patient’s frail condition, and a gastrostomy tube was inserted.
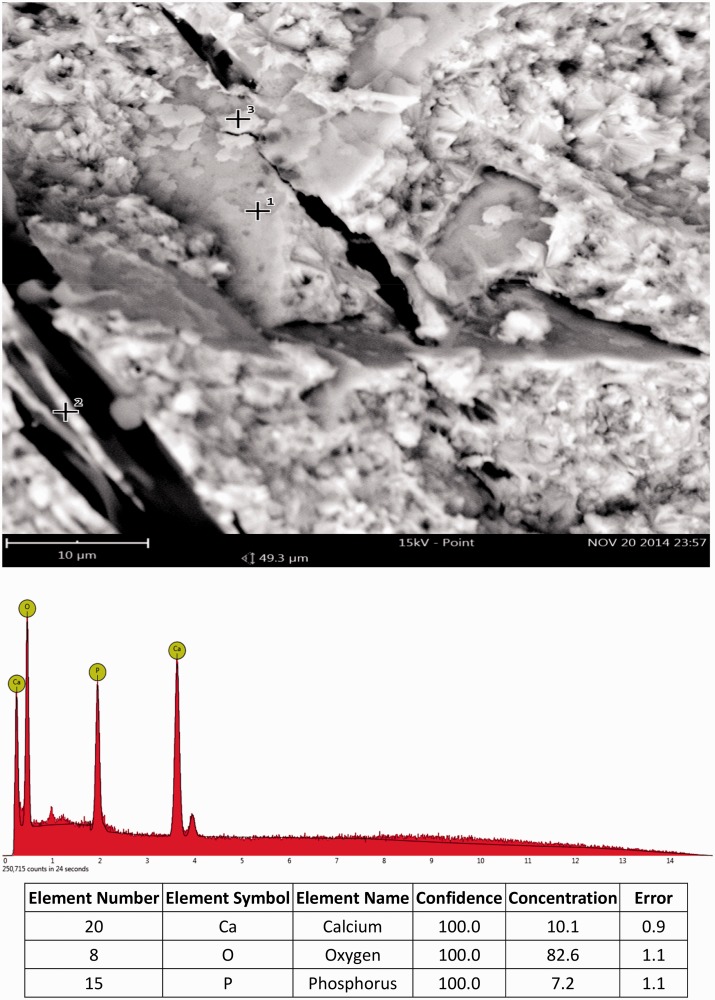
Two samples of the expectorated material were analysed by electron microscopy and energy dispersive spectrometry at 15 kV (Phenom ProX system; Phenom-World, the Netherlands). Semiquantitative chemical analyses were performed using a high-resolution silicon drift detector and a high-sensitivity energy dispersive spectrometry detector without any coating on the sample. Mineralogy analysis revealed the broncholithiasis to be composed of calcium and phosphate, with no crystals of silica or silicate (Figure 3).
Figure 3.
Electron microscopy and energy-dispersive spectrometry of broncholithiasis-sample.
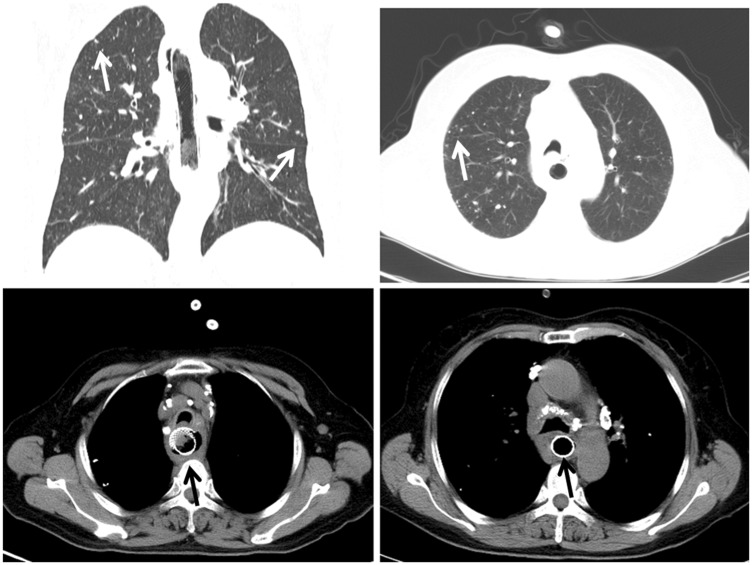
In June 2009 (16 months later), the patient was admitted to the hospital for the third time because of a 10-day history of coughing, sputum production, dyspnoea, fever, and night sweats. The admission laboratory data included a white blood cell count of 6.65 × 109/L (reference range, 4.0–10.0 × 109/L), haemoglobin level of 114 g/L (reference range, 110–150 g/L), high-sensitivity C-reactive protein level of 26.38 mg/L (reference range, 0–3 mg/L), serum albumin level of 43.20 g/L (reference range, 35–55 g/L), serum protein level of 70 g/L, and erythrocyte sedimentation rate of 34.90 mm/h (reference range, 0–20 mm/h). A skin test for purified protein derivative (5 TU) was strongly positive, with an induration of 25 mm with ulceration. The concentrated sputum test result was positive. The patient was diagnosed with silicotuberculosis relapse. Computed tomography revealed an oesophageal stent shadow, oesophageal wall thickening, multiple small nodular spots, patchy shadows, and multiple calcified lymph nodes in the mediastinal and lung windows (Figure 4). Antituberculosis treatment with rifapentine (450 mg twice a week), isoniazid (inhaled, 300 mg once a day), and pyrazinamide (750 mg once a day) was initiated. After 9 months of antituberculosis treatment, the patient regained a satisfactory state of health under continual observation (Figure 4). She was clinically well at the time of this writing.
Figure 4.
CT scan of esophageal stent shadow, esophageal wall thickening, multiple small nodules, patch shadows, and mediastinal and lung door multiple calcified lymph nodes.
Discussion
Most oesophagobronchial fistulas in adults result from a locally advanced oesophageal or bronchogenic malignancy. Benign oesophagobronchial fistulas are acquired through traumatic or prolonged intubation of the trachea or oesophagus5 and result from mediastinal inflammation. Silicosis-related lymphadenopathy in the posterior mediastinum with calcification induces the development of a tiny traction diverticulum of the oesophagus. We considered that the pressure from the lymph node had caused the oesophageal torus lesion while obstruction of the bloodstream had caused the ulcer. Ingestion of sharp silica fragments may cause local repeated injuries during their passage down the oesophagus and become buried in the mucosa, stimulating proliferation by providing anchorage.6 According to the findings of barium oesophagography, gastroesophageal endoscopy examination, and biopsy, the patient may have developed oesophageal-related chronic inflammation, diverticulitis, and ulceration that may have led to repeated oesophagobronchial fistulas. The frequent complications and persistent fistulas were probably related to stasis in the oesophagus.
Silicosis is frequently complicated by tuberculosis.7 Several studies have revealed that mediastinal granulomatous inflammation caused by tuberculosis could account for 14% to 67% of benign oesophagobronchial fistulas based on the prevalence of tuberculosis in the study population.8 An oesophagobronchial fistula is an unusual manifestation of tuberculosis, and its correct diagnosis may sometimes be difficult because of its insidious and non-specific clinical course. Although the tuberculosis-related examination failed to find indications of tuberculosis in the present case, tuberculosis could not be ruled out. More than 1 year later, the patient showed symptoms of tuberculosis; thus, the diagnosis was eventually established and successfully treated by antituberculosis chemotherapy. We therefore believe that initial tuberculosis should not be excluded.
Traditionally, the treatment of oesophagobronchial fistulas has relied on surgical repair. In recent years, medical management with antituberculosis therapy for patients with tuberculous oesophagobronchial fistulas has been successful.9 Other treatments include placement of self-expanding metallic stents, percutaneous gastrostomy, or silicon oesophageal prostheses.10 Metallic stents are superior to other methods.11 In our patient, two oesophageal stents were placed for management of the fistulas but failed to prevent repeated fistulas related to oesophageal inflammation. The patient had undergone one percutaneous gastrostomy at the time of this writing. The treatment of an oesophagobronchial fistula depends on the severity of symptoms, location of the fistula, and general condition of the patient.
Broncholithiasis arises most commonly from erosion and extrusion of chronically inflamed calcified contiguous mediastinal or intrapulmonary lymph nodes in the tracheobronchial tree. Previous tuberculosis and histoplasmosis accounts for most cases of broncholith formation, but silicosis is the most well-known non-infectious cause. Silicotic lymph nodes with eggshell calcification can erode a bronchial wall. Sartorelli12 was the first to describe broncholithiasis in patients with silicosis in 1957, after which a few cases with silicosis were reported.2 Mineralogy analysis of our patient revealed that the expelled substance was composed of calcium and phosphorus but contained no crystals of silica or silicate. Energy dispersive microanalysis of the nodal tissue revealed a sharp peak for silicon.13 The broncholithiasis was thus perhaps associated with the previous tuberculosis. This case was complicated by the relapse of tuberculosis despite the silicosis. Studies have shown that treatment of broncholithiasis is restricted to clinical follow-up. Some invasive procedures may be necessary, depending on the location and size of the lesions and associated complications. In general, the prognosis is favourable.
In our case, the patient’s occupational history and radiologic features helped with the diagnosis of silicosis, but the complications of silicosis are incompletely understood. Considering all aspects of the present case, we conclude that the silicosis of the mediastinal lymph nodes was initially caused by oesophagobronchial fistula formation and broncholithiasis. As the disease progressed, relapse of the silicotuberculosis developed, highlighting another important complication. The complications of silicosis should not be ignored by clinicians.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Shukuya T, Naka G, Kawana A, et al. Pneumoconiosis associated with an esophageal ulcer and uptake revealed in FDGPET. Intern Med 2006; 45: 293–296. [DOI] [PubMed] [Google Scholar]
- 2.Antão VC, Pinheiro GA, Jansen JM. Broncholithiasis and lithoptysis associated with silicosis. Eur Respir J 2002; 20: 1057–1059. [DOI] [PubMed] [Google Scholar]
- 3.Mulliez P, Darras A, Dabouz R, et al. Broncholithiasis in a case of silicotuberculosis. Rev Pneumol Clin 1990; 46: 85–87. [in French, English Abstract]. [PubMed] [Google Scholar]
- 4.Carasso B, Couropmitree C, Heredia R. Egg-shell silicotic calcification causing bronchoesophageal fistula. Am Rev Respir Dis 1973; 108: 1384–1387. [DOI] [PubMed] [Google Scholar]
- 5.Hilgenberg AD, Grillo HC. Acquired nonmalignant tracheoesophageal fistula. J Thorac Cardiovasc Surg 1983; 85: 492–498. [PubMed] [Google Scholar]
- 6.O’Neill C, Pan Q, Clarke G, et al. Silica fragments from millet bran in mucosa surrounding oesophageal tumours in patients in northern China. Lancet 1982; 1: 1202–1206. [DOI] [PubMed] [Google Scholar]
- 7.Snider DE., Jr The relationship between tuberculosis and silicosis. Am Rev Respir Dis 1978; 118: 455–460. [DOI] [PubMed] [Google Scholar]
- 8.Sasaki M, Mochizuki H, Takahashi H. A bronchoesophageal fistula that developed shortly after the initiation of antituberculous chemotherapy. Intern Med 2013; 52: 795–799. [DOI] [PubMed] [Google Scholar]
- 9.Porter JC, Friedland JS, Freedman AR. Tuberculous bronchoesophageal fistulae in patients infected with the human immunodeficiency virus: three case reports and review. Clin Infect Dis 1994; 19: 954–957. [DOI] [PubMed] [Google Scholar]
- 10.Argüder E, Aykun G, Karalezli A, et al. Bronchoesophageal fistula. J Bronchology Interv Pulmonol 2012; 19: 47–49. [DOI] [PubMed] [Google Scholar]
- 11.Shin JH, Kim JH, Song HY. Interventional management of esophagorespiratory fistula. Korean J Radiol 2010; 11: 133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sartorelli E. Letter: Broncholithiasis in silicosis. Am Rev Respir Dis 1974; 109: 687–687. [DOI] [PubMed] [Google Scholar]
- 13.Case records of the Massachusetts general hospital. Weekly clinicopathological exercises. Case 46-1991. A 64-year-old man with recurrent hemoptysis, a bronchoesophageal fistula, and broncholithiasis. N Engl J Med 1991; 325: 1429–1436. [DOI] [PubMed] [Google Scholar]