Abstract
Objective
Decentered flaps are rarely reported after femtosecond laser-assisted in situ keratomileusis flap procedures. We present a patient with a decentered flap after preparation of a corneal flap using the Femto LDV technique.
Methods
The 22-year-old man required a redo operation because of a decentered corneal flap. It was performed the same day at the patient's insistence and with his consent. The new corneal flap for the redo surgery was prepared using the femtosecond laser technique and IntraLase.
Results
Uncorrected visual acuity for each eye was 1.2 during the 12-month follow-up. The results of the Femtosecond laser technique showed good predictability and repeatability regarding the preparation of corneal flaps, but it still may cause some intraoperative complications.
Conclusion
Once redo surgery is needed, the size and depth of the initially prepared flap should be determined using anterior segment optical coherence tomography to pre-set the parameters for preparation of the redo flap.
Keywords: Decentered flap, LASIK, optical coherence tomography (OCT), second flap, Femto LDV, redo surgery
Introduction
The femtosecond laser-assisted in situ keratomileusis flap (LASIK) technique is superior to microkeratome LASIK for the preparation of corneal flaps with suitable depth. It also exhibits satisfactory safety, predictability, and repeatability.1 In rare cases, however, it causes some intraoperative complications.2–5 A decentered flap is sometimes generated during microkeratome LASIK. In this case report, we present a patient with a decentered flap after preparation of a corneal flap using the Femto LDV technique. IntraLase (Abbott Medical Optics, Santa Ana, CA, USA) was used to prepare the second flap. During the 12-month follow-up, the uncorrected distance visual acuity for each eye was 1.2.
Case report
A 22-year-old man presented to our department for correction of refractive errors. The ophthalmological examination revealed uncorrected visual acuity of 0.25 and 0.3 in the right and left eyes, respectively. The central corneal thickness of the right eye was 500 µm, and that of the left right was 502 µm. Treatment with Zeimer Femto LDV-assisted laser in situ keratomileusis (LASIK; Zeimer, Port, Switzerland) was proposed. The size of the ring of negative pressure was set at 9.0 mm. The pre-set depth of the valve was 110 µm. The surgery in the right eye was successful. In the left eye, however, a small, eccentric flap with a diameter of approximately 6.5 mm was noted in proximity to the nasal side (Figure 1). The surgery was therefore aborted, and redo surgery was proposed after an interval of 3 months, at which time the corneal profile would have stabilized. The patient, however, insisted on undergoing redo surgery immediately as he wished to participate in a civil servant physical examination the next day. The patient was informed about the potential risks, and he gave written informed consent.
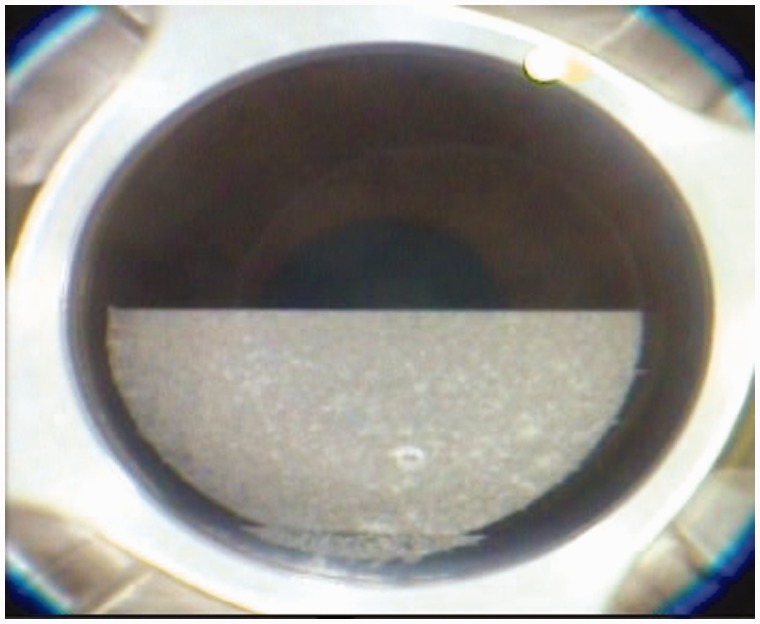
Figure 1.
A decentered flap was prepared in the left eye using the Femto LDV technique. The flap diameter was 6.5 mm.
The second flap was made using the IntraLase technique. Prior to the redo surgery, anterior optical coherence tomography was performed, which revealed that the depth of the first flap was 119 µm (Figure 2). The corneal depth for the present surgery was then pre-set at 140 µm, and the diameter of the flap was 8.6 mm (Figure 3). Following the redo surgery, the patient was required to wear a bandage contact lens. The uncorrected visual acuity for both eyes was 0.5 at 2 h postoperatively. The corneal flap location was satisfactory, with a slit lamp revealing only slight edema (Figure 4). The margins of the flap had healed completely at 2 days postoperatively (Figure 5). The uncorrected visual acuity for each eye was 1.2 at 5 days after surgery, and the profile of the cornea was more regular than previously (Figure 6). The patient was followed up for more than 12 months, with a satisfactory prognosis regarding vision and refraction.
Figure 2.
Optical coherence tomography shows that the depth of the decentered flap was 119 µm. The corresponding matrix bridge was 439 µm.
Figure 3.
The flap was successfully prepared using IntraLase. The margin of the flap is clearly seen.
Figure 4.
The para position of the corneal flap in the left eye is satisfactory 2 h postoperatively, with only slight edema.
Figure 5.
The epithelium of the flap had healed 2 days postoperatively.
Figure 6.
Corneal profiles at postoperative day 2 (a) and postoperative day 5 (b).
Discussion
Femtosecond laser—including IntraLase, Femto LDV, VisuMax, WaveLight FS200—has been commonly used to correct corneal refraction. Among these laser types, IntraLase was the first to be used in clinical practice. Its advantages included preparing corneal flaps with a uniform gauge as well as good predictability and repeatability. It did not require taking the corneal curvature into consideration, and it was not associated with any unexpected events, including freeing or cracking of the flaps.6,7 It did, however, cause some postoperative complications, such as diffuse lamellar keratitis,8 anterior chamber gas bubbles,9 subepithelial gas,5 and transient light sensitivity.3
Recently, Femto LDV has been reported useful for preparing high-quality corneal flaps with unified texture and as good predictability as obtained using the IntraLase technique. Previously reports indicated that the depth and diameter of the flaps prepared using Femto LDV were determined based on the corneal depth and the keratometric value. These flaps had some complications, however, such as loss of epithelium, becoming decentered, and developing adhesions, an irregular margin, and/or crimping.
In the patient presented here, a decentered flap was generated in the left eye after creating the flap using the Femto LDV technique. As the patient demanded that the second surgery be done urgently, it was performed on the same day. If the same depth were set for flaps created for the redo surgery, they might have a broken matrix and/or matrix bridge. Therefore, the depth of the flaps created for the redo surgery were thicker (about 20 µm) than the one that had been originally designed to raise the flap. Individual designs of the flap are not possible using the Femto LDV as the parameters are fixed in advance. Moreover, a flatter keratometric value of 39.5 D was determined, indicating a potential risk of small flap formation during the redo surgery if Femto LDV was used. For this reason, the flap was created using IntraLase FS60 for the redo surgery, and it showed no direct association with the flatter keratometric value. The final corneal flap depth was 143 µm, which was 24 µm more than the pre-set depth.
The time interval between the initial surgery and the second surgery is still controversial. Studies have proposed that the interval for preparing the flap using microkeratome LASIK should be 3–6 months to allow the corneal profile to stabilize.10 In contrast, others deemed that a duration of more than a week was acceptable in clinical practice, so long as the corneal flap had healed.11 For the femtosecond laser technique, loss of negative pressure may be induced during flap creation. Generally, the same parameter could be used for the subsequent flap creation as the corneal flap was not detached from the matrix completely during the flap creation using IntraLase. Hence, the subsequent flap creation prior to flap elevation had no effect on the shifting of the corneal flap and the matrix. In fact, few matrix bridges are formed during flap creation using the Femto LDV method. Therefore, the flaps could be easily detached. In our previous experience, patients whose flaps became decentered during the surgery were scheduled to undergo the second surgery after an interval of ≥7 days. In this report, the patient demanded urgent second surgery, so it was performed on the same day.
Postoperative complications during the creation of corneal flaps are generally associated with deficiency or loss of negative pressure; a low, flat keratometric value; and false vacuum aspiration.12,13 The optimal method to prevent these complications is to expose the eyeball to guarantee vacuum aspiration. For those with low or large, flat keratometric values, IntraLase is recommended for corneal flap creation.
In summary, femtosecond laser showed good predictability and repeatability for the preparation of corneal flaps, but it still may cause some postoperative complications. Once redo surgery is needed, the size and depth of the initially prepared flap should be determined using anterior-segment optical coherence tomography to pre-set the parameters for the redo flap. In our clinical practice, the size of this flap is larger than the first one to prevent a damaged matrix and matrix bridge. In addition, special care should be taken to prevent folding and shifting the flaps.
Declaration of conflicting interests
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Durrie DS, Kezirian GM. Femtosecond laser versus mechanical keratome flaps in wavefront-guided laser in situ keratomileusis: prospective contralateral eye study. J Cataract Refract Surg 2005; 31: 120–126. DOI: 10.1016/j.jcrs.2004.09.046. [DOI] [PubMed] [Google Scholar]
- 2.Nordan LT, Slade SG, Baker RN, et al. Femtosecond laser flap creation for laser in situ keratomileusis: six-month follow-up of initial U.S. clinical series. J Refract Surg 2003; 19: 8–14. [DOI] [PubMed] [Google Scholar]
- 3.Muñoz G, Albarrán-Diego C, Sakla HF, et al. Transient light-sensitivity syndrome after laser in situ keratomileusis with the femtosecond laser incidence and prevention. J Cataract Refract Surg 2006; 32: 2075–2079. DOI: 10.1016/j.jcrs.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 4.Lifshitz T, Levy J, Klemperer I, et al. Anterior chamber gas bubbles after corneal flap creation with a femtosecond laser. J Cataract Refract Surg 2005; 31: 2227–2229. DOI: 10.1016/j.jcrs.2004.12.069. [DOI] [PubMed] [Google Scholar]
- 5.Srinivasan S, Herzig S. Sub-epithelial gas breakthrough during femtosecond laser flap creation for LASIK. Br J Ophthalmol 2007; 91: 1373–1373. 2007/09/27. DOI: 10.1136/bjo.2007.129213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yao P, Xu Y, Zhou X. Comparison of the predictability, uniformity and stability of a laser in situ keratomileusis corneal flap created with a VisuMax femtosecond laser or a Moria microkeratome. The J Int Med Res 2011; 39: 748–758. DOI: 10.1177/147323001103900306. [DOI] [PubMed] [Google Scholar]
- 7.Mrochen M, Wüllner C, Krause J, et al. Technical aspects of the WaveLight FS200 femtosecond laser. J Refract Surg 2010; 26: S833–S840. DOI: 10.3928/1081597x-20100921-12. [DOI] [PubMed] [Google Scholar]
- 8.de Paula FH, Khairallah CG, Niziol LM, et al. Diffuse lamellar keratitis after laser in situ keratomileusis with femtosecond laser flap creation. J Cataract Refract Surg 2012; 38: 1014–1019. DOI: 10.1016/j.jcrs.2011.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Srinivasan S, Rootman DS. Anterior chamber gas bubble formation during femtosecond laser flap creation for LASIK. J Refract Surg 2007; 23: 828–830. [DOI] [PubMed] [Google Scholar]
- 10.Romero-Diaz-de-Leon L, Serna-Ojeda JC, Navas A, et al. Intraoperative flap complications in LASIK surgery performed by ophthalmology residents. J Ophthalmic Vis Res 2016; 11: 263–267. DOI: 10.4103/2008-322x.188393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klein SR, Epstein RJ, Randleman JB, et al. Corneal ectasia after laser in situ keratomileusis in patients without apparent preoperative risk factors. Cornea 2006; 25: 388–403. DOI: 10.1097/01.ico.0000222479.68242.77. [DOI] [PubMed] [Google Scholar]
- 12.Tran DB, Sarayba MA, Bor Z, et al. Randomized prospective clinical study comparing induced aberrations with IntraLase and Hansatome flap creation in fellow eyes: potential impact on wavefront-guided laser in situ keratomileusis. J Cataract Refract Surg 2005; 31: 97–105. DOI: 10.1016/j.jcrs.2004.10.037. [DOI] [PubMed] [Google Scholar]
- 13.Chen S, Feng Y, Stojanovic A, et al. IntraLase femtosecond laser vs mechanical microkeratomes in LASIK for myopia: a systematic review and meta-analysis. J Refract Surg 2012; 28: 15–24. DOI: 10.3928/1081597x-20111228-02. [DOI] [PubMed] [Google Scholar]