Abstract
Background and Aims:
Laryngoscopy and intubation cause sympathetic stimulation and arousal reactions. We evaluated the role of dexmedetomidine and magnesium sulphate on pressor responses to laryngoscopy and intubation as compared to placebo, when depth of anaesthesia was maintained at a constant bispectral index (BIS) range 40-50 (±5).
Methods:
One hundred and twenty patients were randomised to receive either dexmedetomidine 1 μg/kg (Group DS), magnesium sulphate 30 mg/kg diluted in 100 ml saline (Group MS) or 100 ml normal saline (Group NS) 15 min before induction of anaesthesia in a double blind manner. After achieving BIS 40–50 (±5), laryngoscopy and intubation were performed. Heart rate (HR), systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded pre-drug, after drug, at intubation, at intervals of 1 min till 5 min, then every 2 min till 10 min and every 10 min for 30 min. Statistical analysis was done using Chi-square test and one way analysis of variance.
Results:
SBP, DBP and HR fell in the DS and MS groups. No significant changes in BP were seen in the NS group at induction and after intubation. HR rose in the NS group (P < 0.001) at induction from 86.35 ± 9.05 to 95.35 ± 11.60 at 2 min. Patients in DS and MS groups had significantly lower HR, SBP and DBP at laryngoscopy and intubation.
Conclusion:
At BIS levels 40-50 (±5) there was no pressor response to intubation in the NS Group. Dexmedetomidine and magnesium sulphate significantly reduced the heart rate and blood pressure from baseline.
Key words: Bi-spectral index, dexmedetomidine, laryngoscopy, magnesium sulphate, pressor response, tracheal intubation
INTRODUCTION
Laryngoscopy and intubation, being noxious stimuli, incite remarkable sympathetic activity. The pressor response, represented by an abrupt rise in the arterial blood pressure and heart rate (HR), arising 30 s after laryngoscopy and intubation, returns to baseline values steadily within 5–10 min.[1] These transitory responses usually produce no consequences in healthy individuals but may be harmful to the patients having reactive airways, hypertension, coronary artery disease, myocardial insufficiency and cerebrovascular diseases.[2]
Common factors precipitating the pressor response to laryngoscopy and intubation are light planes of anaesthesia, prolonged time for the procedure, elevation of vagally innervated posterior part of epiglottis by straight/Miller blade, anatomically difficult view, greater force used to displace the tongue and more manipulations/attempts at laryngoscopy and intubation.[3] Several drugs and manoeuvres have been used for mitigating this stress response with variable benefits and side effects.[4]
Dexmedetomidine is known to attenuate hypertensive responses associated with intubation, surgical stimulation and emergence.[5] Intravenous (IV) magnesium sulphate has also been shown to reduce the haemodynamic changes associated with laryngoscopy and intubation.[6] Both the drugs have been used by various authors for assessing their efficacy to abolish these pressor responses.[7,8]
Laryngoscopy and intubation can cause sympathetic stimulation and arousal reactions. We therefore designed this study to evaluate the attenuation of this pressor response by dexmedetomidine and magnesium sulphate as compared to placebo, when the depth of anaesthesia was maintained at bi-spectral index (BIS) range 40–50 (±5) in all the patients.
METHODS
After approval from the Institutional Ethics Committee, the present study enrolled 120 patients of American Society of Anesthesiologists (ASA physical status I and II, aged 18–60 years, of either sex, scheduled for elective surgery under general anaesthesia using induction with propofol and maintenance with vecuronium and isoflurane. The exclusion criteria were refusal of consent; hepatic, renal or cardiovascular dysfunction; uncontrolled hypertension; epilepsy; pregnancy; postural hypotension; anticipated difficult airway; anticipated major blood losses and fluid shift; patients on sedatives and drug allergies. Duration of the study was from February 2016 to July 2017. The study was registered with the Clinical Trials Registry of India (CTRI/2018/03/012744).
Pre-anaesthetic evaluation and relevant investigations were carried out in all patients. On the night before the surgery, informed written consent was obtained and tablet alprazolam 0.5 mg was given to all patients and were fasted for 6 h.
In the operating room, non-invasive blood pressure (NIBP), electrocardiogram (ECG), pulse oximeter (SpO2) and bispectral index monitor (BIS VISTA™ monitoring system, Covidien Ilc, 15 Hampshire Street, Mansfield, MA, 02048, USA) were attached and intravenous cannula was secured.
Eligible patients were randomly divided into three groups of 40 each by computer-generated random numbers, sealed in envelopes as folded slips in the OT complex. These slips were picked up by an independent observer who later prepared the drug solutions accordingly.
TP (pre-test drug) electrocardiogram (ECG), BIS value, SpO2, heart rate HR) and blood pressures, systolic (SBP) and diastolic (DBP) were recorded. This was a participant and investigator blinded study. Group DS (n = 40) was administered IV dexmedetomidine 1 μg/kg, Group MS (n = 40) received IV magnesium sulphate 30 mg/kg and Group NS (n = 40), control group, received normal saline intravenously. Blinding was done by preparation of the injectable solution using either dexmedetomidine or magnesium sulphate or 0.9% saline (control) by an independent observer not involved in this study. Infusion of the study drug was given in 100 ml normal saline over 15–20 min 15 min before induction according to the groups allotted.
TA (after test drug): SBP, DBP, HR, were recorded after 5 min of drug infusion. IV glycopyrrolate 0.01 mg/kg and butorphanol 0.02 mg/kg were given to all patients to avoid any bias.
Patients were pre-oxygenated for 3 min with 100% oxygen and then, anaesthesia was induced with propofol IV titrated to achieve BIS value in range of 40–50 (±5), and then 1.5 mg/kg succinylcholine IV was adminstered. Laryngoscopy was carried out gently in <15 s. The pressor response was evaluated at a constant BIS index of 40–50 (±5). Endotracheal tube tolerance (coughing or bucking) was noted. Patients requiring >15 s for laryngoscopy, bronchospasm or laryngospasm were added in the demographic profile but excluded from statistical analysis. Perioperative hypotension was defined as SBP <90 mmHg and bradycardia as HR <50 beats/min. Arrhythmias were defined as supraventricular or premature ventricular beats >3/min or any rhythm other than sinus. Injection atropine 0.3 mg increments and mephentermine 6 mg bolus were used to treat bradycardia and hypotension, respectively. BIS values, SpO2, HR, SBP and DBP were recorded at- T0 at intubation, at the interval of 1 min till 5 min, then 2 min till 10 min and every 10 min for 30 min.
Subsequently, the maintenance of anaesthesia was carried out with isoflurane and 66% nitrous oxide in oxygen with controlled ventilation using a closed circuit throughout. Injection vecuronium bromide 0.08 mg/kg IV was given as an initial dose for neuromuscular blockade and 0.02 mg//kg bolus IV when required. Residual neuromuscular blockade was reversed at the end of surgery using IV neostigmine 0.05 mg/kg and glycopyrrolate 0.02 mg/kg, followed by extubation.
The primary outcome of interest were changes in BP and HR from baseline, at intubation and upto 30 min after intubation.
Based on a previously published study, taking HR as the primary objective, SD obtained was 5.397 and expected difference between the means was calculated as 3.38. Assuming the power of our study 80% and an alpha error of 0.05, sample size was calculated to be 40.[9]
Statistical Package for the Social Sciences (SPSS) 17.0 software was used for the statistical analysis of the compiled data by applying Chi-square test and the One-Way Analysis of Variance (ANOVA) with post hoc Tukey HSD tests. Means and standard deviations represented the average and typical spread of values. P < 0.001 was considered a highly significant difference and P < 0.05 was significant.
RESULTS
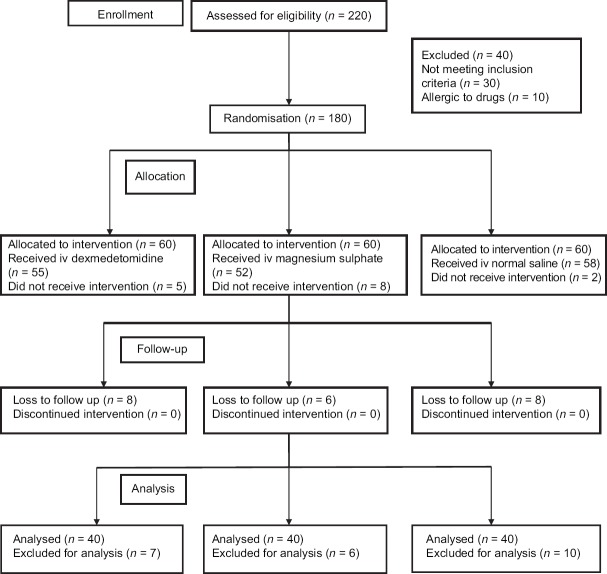
The flow of patients through the trial is described in Figure 1. Demographic data and duration of surgery between three groups were similar [Table 1].
Figure 1.
Consort Diagram
Table 1.
Demographic characteristics of patients in three groups

Baseline haemodynamic parameters were comparable among three groups. The intragroup comparison of HR in three groups compared to pre-drug values showed a statistically highly significant (P < 0.001) fall in group DS and MS up to 30 min, whereas a significant rise was seen in group NS (P < 0.001) at induction for 2 min. For another 2 min, the rise remained significant statistically. On intergroup comparison, both Group DS and MS had a highly significant (P < 0.001) fall in HR compared to NS after study drug, but Group DS showed a statistically highly significant attenuation of HR compared to MS up to 9 min. Both remained significantly lower (P < 0.001) than the control group throughout. No rise in HR above the baseline was seen in group DS and MS at any point of time during the post-intubation period [Figure 2].
Figure 2.
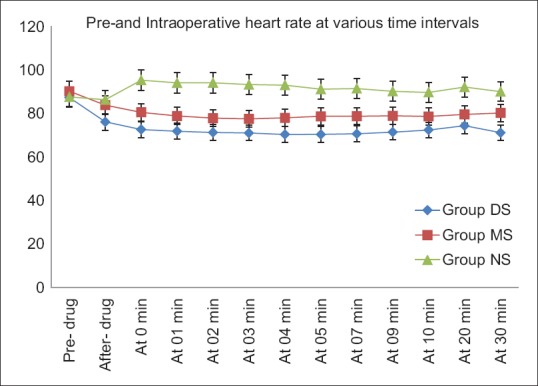
Comparison of mean heart rate among three groups
Before intubation, a significant reduction in the mean SBP values was seen after the study drug infusion in Group DS from 132.77 ± 9.70 to 117.28 ± 9.88 and MS from 131.73 ± 9.70 to 119.58 ± 9.18 (P < 0.001), but not in the NS group. In NS group, SBP increased significantly (P < 0.001) at intubation only from 123.70 ± 13.45 to 129.60 ± 15.40. However, SBP remained significantly lower in other two groups (P < 0.001) till 30 min post-intubation as compared to pre-drug values. Compared to NS group, both DS and MS groups showed a significant (P < 0.05) and highly significant (P < 0.001) decrease in SBP throughout the intra-operative period, group DS having the lowest SBP value [Figure 3].
Figure 3.
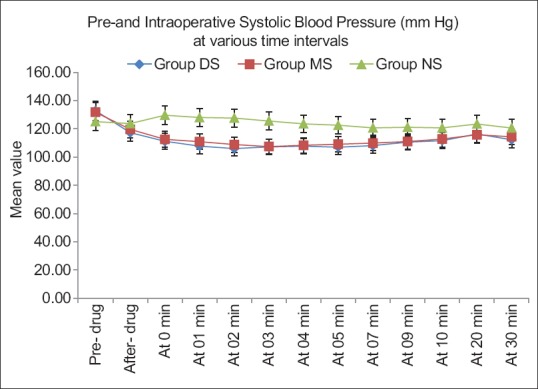
Comparison of mean systolic blood pressure among three groups
Similarly, a fall in DBP was noticed on intragroup comparison, after the study drug infusion in Group DS and MS, which remained highly significant (P < 0.001) throughout. However, no significant (P > 0.05) change in DBP was seen in NS group. The comparison of both Group DS and MS with NS was significant (P < 0.05) or highly significant (P < 0.001) at all-time intervals with no increase above the baseline in DS and MS groups [Figure 4].
Figure 4.
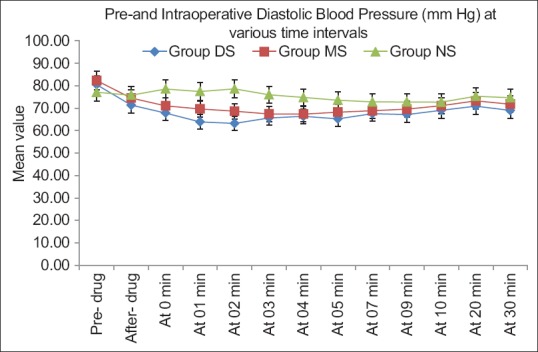
Comparison of mean diastolic blood pressure among three groups
Baseline BIS values were comparable in all the three groups. Opioid (Butorphanol) was given after the study drug in all the three groups, just before induction, so changes in BIS trend with opioid timing were not significant. BIS changes were studied in relevance to the study drug. Laryngoscopy was done after induction with propofol at a BIS of 40–50 (±5).
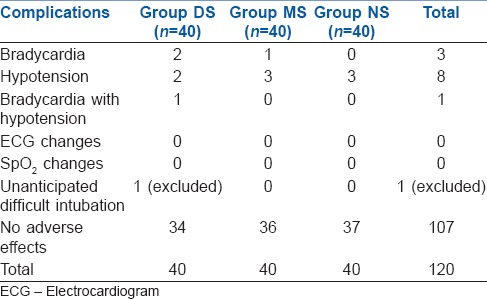
No coughing or bucking or movements were seen after intubation. Airway trauma, laryngospasm or bronchospasm and fall in SpO2 were also not seen. No changes in ECG (arrhythmias) were observed. No significant adverse effects were noted in either of the groups [Table 2]. One patient of DS group with unanticipated difficult intubation was included in demographic profile but was excluded from statistical analysis.
Table 2.
Intra-operative complications
DISCUSSION
Laryngoscopy and intubation are known to cause an increase in HR and blood pressure.[1,3,10] In the present study, the effect of dexmedetomidine and magnesium sulphate on the pressor responses was compared to normal saline group (placebo) after achieving an adequate depth of anaesthesia, that is BIS value 40–50 (±5). In our pilot study, we observed that BIS levels of 40–50 provided better conditions for laryngoscopy than BIS 40–60. Since laryngoscopy and endotracheal intubation, similar to any other peripheral noxious stimulus, might produce a reflex response in the reticular activating system of brainstem, it can lead to wakefulness, making the planes of anaesthesia lighter.[11] Hence, maintaining the BIS values at 40–50 during the induction of anaesthesia may prevent such responses.
Dexmedetomidine and magnesium sulphate appeared to best meet the characteristics of a drug to prevent these sympathetic responses.[12] Bolus dose of 1 μg/kg was selected for dexmedetomidine, as it provides better control compared to 0.5 μg/kg and less side effects than 2 μg/kg.[13,14] Magnesium sulphate in a bolus dose of 30 mg/kg was observed to attenuate the adverse haemodynamic responses without any hypotension or bradycardia.[15] Placebo group was included for comparison, so as to know the haemodynamic changes that would occur with laryngoscopy and intubation if the study drugs were not used.
A rise in HR was observed after the laryngoscopy and intubation in the placebo group, but it returned promptly towards the baseline after 2 min.[16,17] In addition, no significant change in BP was noticed, as opposed to previous studies documenting a rise in BP where BIS monitoring had not been used.[17] Throughout the study period, SBP and DBP values in the placebo group were comparable to the baseline. It can be advocated that maintaining an adequate depth of anaesthesia at BIS 40–50 (±5) was enough to prevent the sympathetic reflex mediated by laryngoscopy and intubation.
However, HR and BP were significantly lower (P < 0.001) in both dexmedetomidine and magnesium sulphate groups but dexmedetomidine accounted for even lower values comparatively because of its sympatholytic and vagomimetic effects.[7] Slow infusion of dexmedetomidine over 15 min caused a gradual fall in plasma catecholamine levels.[18] Dexmedetomidine binds to α2 receptors (α2:α1-1620:1) located on vascular pre-junctional terminals, inhibiting the release of norepinephrine through negative feedback causing a decrease in sympathetic outflow which accounted for a decrease in BP.[19] It also causes increase in vagal activity and has some peripheral ganglion blocking action.[20] Infusion of magnesium sulphate produces a fall in HR and BP by directly blocking the release of catecholamines from both adrenal gland and adrenergic nerve terminals and indirectly through negative feedback mechanism.[6] It also acts directly on the blood vessels leading to vasodilatation and decreases vasopressin-stimulated vasoconstriction.[21] The stability of intra-operative haemodynamics achieved with single 30 mg/kg dose of MgSO4 at induction ameliorated the need for continuous peri-operative infusion as opposed to previous studies.[22,23]
Significantly lower BIS values with least variability were observed with dexmedetomidine and magnesium sulphate during intubation and thereafter. This finding can be attributed to the fact that both the drugs prevented the escalation in the central catecholamine levels. However, there was a significant decrease in haemodynamic variables throughout, which may actually be desirable in certain surgeries where induced hypotension may be beneficial. BIS monitoring serves the goal of maintaining adequate depth of anaesthesia well and reducing the requirement of IV induction agents, volatile agents and analgesics.[24] Since, the BIS values increase with unpleasant stimuli, it can be utilised as an objective marker for quantifying hypnosis that proved advantageous to assess the blunting of the pressor response.[25]
The primary outcome of our study was to evaluate the effect of drugs such as dexmedetomidine and magnesium sulphate to prevent pressor responses in comparison to control group under BIS monitoring. Since there are many studies describing the use of dexmedetomidine in preventing the pressor response to laryngoscopy and intubation, but this being an expensive drug in terms of cost and delayed recovery, due to its sedative effect, a cheaper substitute is required. MgSO4 may be a good alternative for producing a similar effect. However, the results showed a different trend. There was a minimal pressor response in control group, as adequate depth of anaesthesia was maintained at BIS 40–50. Dexmedetomidine and MgSO4 produce a significant decrease in haemodynamics further rather than maintaining stability. Out of the two drugs, MgSO4 proved to be a better alternative.
BIS monitoring during laryngoscopy and intubation should be made a part of healthcare policy, since it not only produces stable condition but also reduces the cost of drugs to obtund pressor responses. The literature till now describes BIS range of 40–60 to be the indicator of adequate depth of anaesthesia, but in our pilot cases, we found BIS depth of 40–50 produced more stable conditions. Contrary to other studies, here the pressor responses have been assessed using BIS, whereas, in the past obtunding of pressor responses with various drugs was studied without confirming adequacy of depth of anaesthesia.
In future, research can be planned on evaluating the pressor responses with or without BIS monitoring. Further, the impact of BIS on haemodynamic variability during laryngoscopy and intubation can be compared between different BIS ranges of 40–50 and 50–60. Plasma catecholamine levels at different BIS values could be studied to know the correlation with BIS.
CONCLUSION
It may be concluded that by maintaining a suitable anaesthetic depth using BIS index of 40–50 as a guide, the pressor response to laryngoscopy and intubation can be adequately obtunded.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Reid LC, Brace DE. Irritation of respiratory tract and its reflex effect on heart. Surg Gynecol Obstet. 1940;70:157. [Google Scholar]
- 2.Kovac AL. Controlling the hemodynamic response to laryngoscopy and endotracheal intubation. J Clin Anesth. 1996;8:63–79. doi: 10.1016/0952-8180(95)00147-6. [DOI] [PubMed] [Google Scholar]
- 3.Joffe AM, Deem SA. Physiologic and pathophysiologic responses to intubation. In: Benumof J, Hagberg CA, editors. Benumof and Hagberg's Airway Management. 3rd ed. Philadelphia: Elsevier Saunders; 2012. pp. 184–95. [Google Scholar]
- 4.Charuluxananan S, Kyokong O, Somboonviboon W, Balmongkon B, Chaisomboonpan S. Nicardipine versus lidocaine for attenuating the cardiovascular response to endotracheal intubation. J Anesth. 2000;14:77–81. doi: 10.1007/s005400050071. [DOI] [PubMed] [Google Scholar]
- 5.Tanskanen PE, Kyttä JV, Randell TT, Aantaa RE. Dexmedetomidine as an anaesthetic adjuvant in patients undergoing intracranial tumour surgery: A double-blind, randomized and placebo-controlled study. Br J Anaesth. 2006;97:658–65. doi: 10.1093/bja/ael220. [DOI] [PubMed] [Google Scholar]
- 6.James MF, Beer RE, Esser JD. Intravenous magnesium sulfate inhibits catecholamine release associated with tracheal intubation. Anesth Analg. 1989;68:772–6. [PubMed] [Google Scholar]
- 7.Keniya VM, Ladi S, Naphade R. Dexmedetomidine attenuates sympathoadrenal response to tracheal intubation and reduces perioperative anaesthetic requirement. Indian J Anaesth. 2011;55:352–7. doi: 10.4103/0019-5049.84846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montazeri K, Fallah MA. Dose response study of magnesium sulphate in suppressing cardiovascular responses to laryngoscopy and endotracheal intubation. J Res Med Sci. 2005;10:82–6. [Google Scholar]
- 9.Hazarika A, Deori AK, Bora J, Deori J, Tiwari PK. Attenuation of haemodynamic responses to laryngoscopy and intubation: A clinical study of dexmedetomidine. Int J Contemp Med Res. 2016;3:3536–8. [Google Scholar]
- 10.Mi WD, Sakai T, Takahashi S, Matsuki A. Haemodynamic and electroencephalograph responses to intubation during induction with propofol or propofol/fentanyl. Can J Anaesth. 1998;45:19–22. doi: 10.1007/BF03011986. [DOI] [PubMed] [Google Scholar]
- 11.Kanaya N, Nakayama M, Fujita S, Namiki A. Haemodynamic and EEG changes during rapid-sequence induction of anaesthesia. Can J Anaesth. 1994;41:699–702. doi: 10.1007/BF03015624. [DOI] [PubMed] [Google Scholar]
- 12.Bachofen M. Suppression of blood pressure increases during intubation: Lidocaine or fentanyl? Anaesthesist. 1988;37:156–61. [PubMed] [Google Scholar]
- 13.Saǧıroǧlu AE, Celik M, Orhon Z, Yüzer S, Sen B. Dıfferent doses of dexmedetomidine on controlling haemodynamic responses to tracheal intubation. Internet J Anesthesiol. 2010;27:2. [Google Scholar]
- 14.Lawrence CJ, De Lange S. Effects of a single pre-operative dexmedetomidine dose on isoflurane requirements and peri-operative haemodynamic stability. Anaesthesia. 1997;52:736–44. doi: 10.1111/j.1365-2044.1997.169-az0303.x. [DOI] [PubMed] [Google Scholar]
- 15.Paul S, Biswas P, Bhattacharjee DP, Sengupta J. Effects of magnesium sulfate on hemodynamic response to carbon dioxide pneumoperitoneum in patients undergoing laparoscopic cholecystectomy. Anesth Essays Res. 2013;7:228–31. doi: 10.4103/0259-1162.118970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Derbyshire DR, Chmielewski A, Fell D, Vater M, Achola K, Smith G, et al. Plasma catecholamine responses to tracheal intubation. Br J Anaesth. 1983;55:855–60. doi: 10.1093/bja/55.9.855. [DOI] [PubMed] [Google Scholar]
- 17.Shribman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation. Br J Anaesth. 1987;59:295–9. doi: 10.1093/bja/59.3.295. [DOI] [PubMed] [Google Scholar]
- 18.Shin HW, Yoo HN, Kim DH, Lee H, Shin HJ, Lee HW, et al. Preanesthetic dexmedetomidine 1 μg/kg single infusion is a simple, easy, and economic adjuvant for general anesthesia. Korean J Anesthesiol. 2013;65:114–20. doi: 10.4097/kjae.2013.65.2.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Menda F, Köner O, Sayin M, Türe H, Imer P, Aykaç B, et al. Dexmedetomidine as an adjunct to anesthetic induction to attenuate hemodynamic response to endotracheal intubation in patients undergoing fast-track CABG. Ann Card Anaesth. 2010;13:16–21. doi: 10.4103/0971-9784.58829. [DOI] [PubMed] [Google Scholar]
- 20.Yildiz M, Tavlan A, Tuncer S, Reisli R, Yosunkaya A, Otelcioglu S, et al. Effect of dexmedetomidine on haemodynamic responses to laryngoscopy and intubation: Perioperative haemodynamics and anaesthetic requirements. Drugs R D. 2006;7:43–52. doi: 10.2165/00126839-200607010-00004. [DOI] [PubMed] [Google Scholar]
- 21.Altura BM, Altura BT. Magnesium and vascular tone and reactivity. Blood Vessels. 1978;15:5–16. doi: 10.1159/000158148. [DOI] [PubMed] [Google Scholar]
- 22.Ryu JH, Kang MH, Park KS, Do SH. Effects of magnesium sulphate on intraoperative anaesthetic requirements and postoperative analgesia in gynaecology patients receiving total intravenous anaesthesia. Br J Anaesth. 2008;100:397–403. doi: 10.1093/bja/aem407. [DOI] [PubMed] [Google Scholar]
- 23.Srivastava VK, Mishra A, Agrawal S, Kumar S, Sharma S, Kumar R, et al. Comparative evaluation of dexmedetomidine and magnesium sulphate on propofol consumption, haemodynamics and postoperative recovery in Spine surgery: A Prospective, randomized, placebo controlled, double-blind study. Adv Pharm Bull. 2016;6:75–81. doi: 10.15171/apb.2016.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song D, Joshi GP, White PF. Titration of volatile anesthetics using bispectral index facilitates recovery after ambulatory anesthesia. Anesthesiology. 1997;87:842–8. doi: 10.1097/00000542-199710000-00018. [DOI] [PubMed] [Google Scholar]
- 25.Ekman A, Lindholm ML, Lennmarken C, Sandin R. Reduction in the incidence of awareness using BIS monitoring. Acta Anaesthesiol Scand. 2004;48:20–6. doi: 10.1111/j.1399-6576.2004.00260.x. [DOI] [PubMed] [Google Scholar]