Abstract
Background and Aims:
Fibre-optic intubation (FOI) through supraglottic airway devices (SADs) is useful in the management of the difficult airway. We compared two methods of FOI through seven SADs in a randomised crossover manikin study to assess each device's performance and discuss implications on SAD selection.
Methods:
Thirty anaesthetsiologists, 15 seniors and 15 juniors, each performed low skill FOI (LSFOI) with seven SADs using both 'direct' and 'indirect' methods. The order of method and device used were randomised. The primary end point was success rate of intubation; secondary end points were time taken for intubation, incidence of difficulties with direct and indirect LSFOI and operator device preference. Statistical analysis was with univariable analysis and comparison of proportions.
Results:
Data from six devices were analysed due to a protocol breach with one SAD. There was no difference in intubation success rate across all SADs and intubation methods. Intubation time was significantly shorter in AmbuAuragain than other SADs and shorter with the direct method of LSFOI than the indirect method (mean difference of 6.9 s, P = 0.027). Ambu Auragain had the least SAD and bronchoscope-related difficulties. Seniors had significantly shorter mean intubation times than juniors by 11.6 s (P = 0.0392). The most preferred SAD for both methods was AmbuAuragain.
Conclusion:
Low skill FOI consistently achieves a high intubation success rate regardless of experience, choice of method, or SAD used. SAD design features may significantly affect the performance of low skill FOI.
Key words: Airway management, endotracheal, intubation, laryngeal mask airway, manikin
INTRODUCTION
Fibre-optic intubation (FOI) is the gold standard in the management of various types of difficult airways but is a complex psychomotor skill with a steep learning curve. 'Low skill' FOI is FOI through a supraglottic airway device (SAD). The SAD allows ventilation during and between attempts at low skill FOI, acts as a conduit and guides the fibre-optic intubating bronchoscope (FOB) to the glottis after exiting the bowl of the SAD. The latter two functions make FOI 'low skill'. Low skill FOI has a high success rate even in difficult airways and forms part of plan B in the Difficult Airway Society (DAS) guidelines on the management of the unanticipated difficult airway.[1,2] There are two methods of low skill FOI (see methodology): direct and indirect.
SADs can be classified based on their functions [Table 1].[3] The first-generation SAD (SAD1) has a single ventilation port. Second-generation SADs (SAD2) have an additional gastric port. We further subdivided these into 'standard' SADs (sSAD1 and sSAD2) to differentiate those designed specifically for fibre-optic 'intubation' (iSAD1 and iSAD2). The iSADs also tend to have wider ventilation ports to facilitate low skill FOI and allows the use of standard width tracheal tubes. sSADs tend to be narrower due to the gastric port, therefore, needing narrow and long tracheal tubes: narrow to fit through the ventilation port and long so that the tracheal cuff, when inflated, resides distal to the vocal cords.[4] Alternatively, the Aintree intubation catheter (AIC), as part of the indirect method, can be used.
Table 1.
Characteristics of supraglottic airway devices
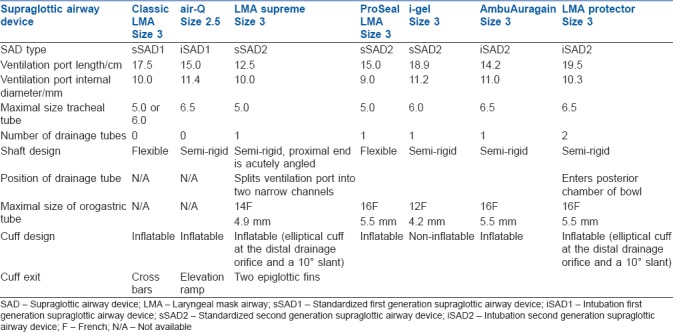
We tested the hypothesis that there is a difference in low skill FOI success rates and performance between the 'standard' and 'intubation' types of SAD1 and SAD2. The sSAD1 was the classic laryngeal mask airway (LMA)™ (IntaventOrthofix Ltd., Maidenhead, Berks, UK); the iSAD1 was the air-Q® LMA (Mercury Medical, Clearwater, FL, USA); the sSAD2 was the ProSeal™ LMA (IntaventOrthofix, Maidenhead, Berks, UK), LMA Supreme™ (IntaventOrthofix Ltd., Maidenhead, Berks, UK) and i-gel™ (Intersurgical Ltd., Wokingham, Berkshire, United Kingdom); and the iSAD2 was the Ambu® Auragain™ LMA (Ambu, Ballerup, Denmark) and the LMA Protector™ (Teleflex Medical, Co., Westmeath, Ireland).
We assessed the performance of seven SADs in low skill FOI by direct and indirect methods in a manikin performed by junior and senior anaesthetists. The primary outcome was success rate of low skill FOI. The secondary outcomes were time for successful low skill FOI; difficulties encountered as caused by the SAD, fibrescope and AIC; effect of experience on success rate and speed of intubation and operator preference of SAD for both methods.
METHODS
A randomised crossover manikin study was approved by SingHealth Centralised Institutional Review Board (CIRB Ref 2016/2862). Anaesthetists from our department of Anaesthesiology were voluntarily recruited with written informed consent. Seniority of the anaesthetist (with seniors being defined as accredited specialists and juniors defined as anaesthesia trainees or non-trainee rotating medical officers) and the number of years of anaesthetic experience was collected. A total of thirty anaesthesiologists were recruited, comprising 15 seniors and 15 juniors, based on previous low skill FOI studies by de Lloyd et al.[5,6]
Each participant viewed a standard video on low skill FOI demonstrating a step-by-step guide. They then performed low skill FOI twice (direct and indirect methods) in a manikin using seven SADs. The order of SAD and method were randomised using a web-based computer-generated research randomiser (https://www.randomizer.org/). Before conducting the trial, the investigators determined the sizes of the SADs that best fitted the manikin: size three for all the SADs except size 2.5 for the air-Q. The tube sizes were chosen so that they fit easily through the SAD ventilation port: 5.0 mm tube for the Proseal LMA and LMA Supreme and 6.0 mm tube for the remaining SADs. The manikin used was the Laerdal® Airway Management Trainer (Laerdal® Medical Ltd., Orpington, Kent, UK). Each SAD was inserted into the manikin by the same study investigator before the start of each low skill FOI to standardise intubating conditions. The same 4.4 mm intubating FOB (Olympus BF-MP 160F, Singapore Pte Ltd) was used for all attempts. Blinding of the participants and the study investigator collecting data was not possible as the SADs were easily identifiable.
In direct low skill FOI, the proximal part of the FOB is preloaded with a microlaryngoscopy tube. The distal part of the FOB is then inserted through the ventilation port of the SAD and glottis and into the trachea. The microlaryngoscopy tube is railroaded over the FOB and into the trachea (until the tube connector rests at the entrance of the ventilation port), and the FOB removed. In the indirect method, the FOB is preloaded with an AIC and inserted through the ventilation port of the SAD and glottis and into the trachea. The FOB is removed, leaving the AIC in the lower trachea. Then, the SAD is removed, a tracheal tube is railroaded over the AIC and into the trachea and then the AIC is removed.
Correct placement of the tracheal tube was confirmed by inflation of the manikin lungs with a self-inflating bag. No verbal cues or assistance was given to the participants.
Primary outcome was the rate of successful low skill FOI, defined as intubation resulting in correct placement of the tracheal tube demonstrated by inflation of the manikin lung. Failure was defined as oesophageal intubation, attempts requiring >3 min or the participant giving up. The following secondary outcomes were also measured: intubation time (time from picking up the FOB to delivery of a single breath), incidence of difficulties encountered related to the SAD, FOB and AIC and operator preference.
SAD-related difficulties were defined as the SAD shaft being too long, SAD curvature being too acute, suboptimal or obscured glottic view and difficulty inserting the tracheal tube into the SAD. FOB-related difficulties were defined as insertion of the FOB into the gastric port of SAD, additional manipulation of the tracheal tube over the FOB, dislodgement of the SAD when removing the FOB, difficulty removing the FOB from the SAD and entry of the FOB into the oesophagus. AIC-related difficulties were defined as: difficulty railroading the tracheal tube over the AIC, dislodgement of the AIC, AIC removed before the tracheal tube was railroaded, AIC kinked and AIC slipping over the FOB tip, thereby causing difficulty with viewing and flexing of the distal tip of the FOB.
Data from Supreme LMA were excluded as different tracheal tubes' sizes were inadvertently used, breaching methodology. Statistical analysis was performed using R, version 3.3.2 software (R Foundation for Statistical Computing, Vienna, Austria) and P < 0.05 was considered statistically significant. Univariable mixed model was used to analyse effects of SAD group and type, method and operator experience level on intubation success rate, and effect size is presented as odds ratio. Univariable linear mixed model was used to analyse effects SAD group and type, method and operator experience on intubation time and effect size presented as mean difference. Comparison of proportions was used to analyse effect of SAD group and type on incidence of SAD-, FOB- and AIC-related difficulties. Mean (standard deviation) was presented for intubation time. Intubation success rates and incidence of SAD, FOB and AIC-related difficulties are presented as frequency in percentages. Our sample size was based on previous low skill FOI studies by de Lloyd et al.,[5,6] with standard deviation of intubation time as 10s, clinically significant time difference as at least 10 s for P < 0.01 and power of 99% to determine a sample size of 30.
RESULTS
The median (interquartile range [range]) number of years of anaesthetic experience for seniors was 17 (12 [7–25]) and for juniors was 1.5 (3.5 [0.17–6]).
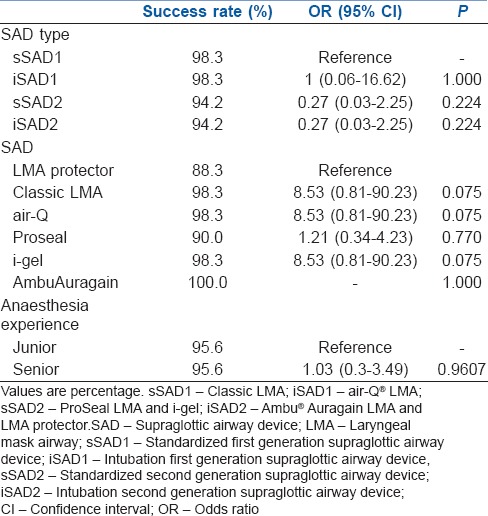
We found no significant difference in intubation success rates across all groups (iSAD1, sSAD1, iSAD2 and sSAD2) and types of SAD, whether using the direct or indirect method [Table 2].
Table 2.
Composite (direct and indirect methods) intubation success rates by supraglottic airway device type, supraglottic airway device and experience
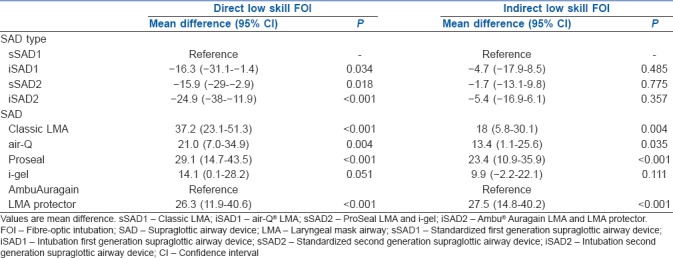
Intubation time was significantly shorter in AmbuAuragain than all other SADs overall by 12.0–27.4 s (mean difference). Comparing SAD groups, intubation time was significantly shorter in iSAD2 than sSAD1. Of clinical significance, sSAD1 had the longest intubation time of all the SAD groups, being slower than other SAD types by 8.6–15.3 s. Intubation times in the sSAD1 were significantly longer than all other groups with direct low skill FOI. There was no significant difference in intubation time for all groups with indirect low skill FOI. The direct method of low skill FOI has a significantly shorter intubation time than the indirect method by a mean of 6.9 s [Tables 3 and 4].
Table 3.
Overall intubation time mean difference by supraglottic airway device type, supraglottic airway device, experience and method
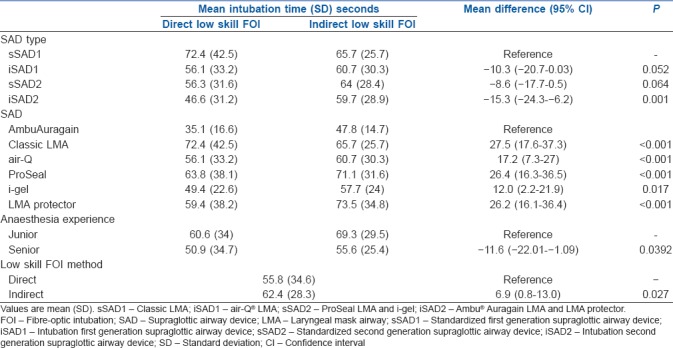
Table 4.
Comparing mean difference of intubation times for supraglottic airway device type and individual supraglottic airway devices by method
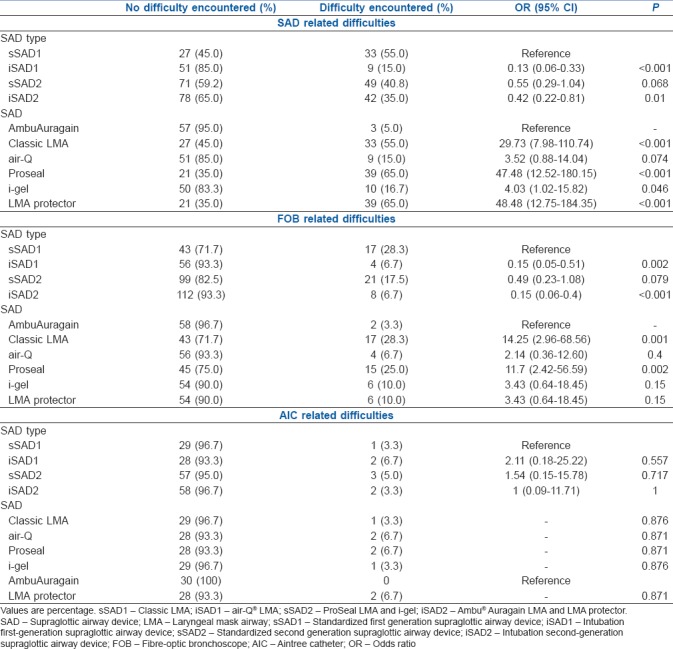
The AmbuAuragain had the least SAD-related difficulties, which was statistically significant compared to the Classic LMA, Proseal, i-gel and LMA Protector. Although there was no statistical significance between the AmbuAuragain and air-Q, we found clinical significance wherein the air-Q had three times the incidence of SAD-related difficult than the AmbuAuragain (15% vs. 5%, respectively). The sSAD1 had the highest incidences of FOB- and SAD-related difficulties, which was statistically significant when compared with the intubation SADs (iSAD1 and iSAD2). There was no statistical significance in incidences of FOB- and SAD-related difficulties between the sSAD1 and sSAD2 groups. The AmbuAuragain had the least FOB-related difficulties, which was statistically significant when compared to Classic LMA and Proseal. There was no significant difference in the incidence of AIC-related difficulties amongst all the SADs [Table 5].
Table 5.
Comparing difficulties with low skill fibre-optic intubation related to supraglottic airway device, Aintree catheter and fibre-optic bronchoscope in supraglottic airway device type and individual supraglottic airway devices
There was no significant difference in success rate of intubation between seniors and juniors. Seniors had a significantly shorter intubation time than juniors by 11.6 s (mean difference) [Tables 2 and 3].
The most preferred SAD for both direct and indirect low skill FOI was the AmbuAuragain followed by the i-gel.
DISCUSSION
Low skill FOI is considered core skill[7] and features in international difficult airway algorithms[1,8,9] for anticipated and unanticipated difficult airways.[10,11] Performance of low skill FOI may be affected by the type of SAD used. This is the first manikin study evaluating direct and indirect low skill FOI between 'standard' and 'intubation' versions of first and second-generation SADs. The key findings in this study are that all six SADs, and either method of low-skill fibreoptic intubation (LSFOI) perform equally well in terms of intubation success rate, but intubation time differs with SAD and method of LSFOI used and seniority of the anaesthetist. SADs also had differential performances in SAD- and bronchoscope-related technical difficulties.
We found a high intubation success rate regardless of degree of anaesthesia experience, choice of method or SAD used: 90.0%–100% for direct low skill FOI and 86.7%–100% for indirect low skill FOI. Patient studies showed similar high success rates of 95%–100%[12] and successful use in patients with predicted and actual difficult airways including failed intubation.[13,14,15] One reason for its high success rate and its 'low skill' is visualisation of the glottis in 74%–100% of cases once the FOB exits the SAD bowl.[16,17] In studies of simulated difficult airways, a full view of the glottis was seen 67% in patients.[17,18]
In our study, intubation times were shorter for the direct than indirect method except for the classic LMA. Shorter intubation times can be expected with the direct method as it has fewer steps and is confirmed in other manikin and cadaver studies.[5,19] Possible explanations why direct FOI times may be longer for the classic LMA are the cross-bars may make railroading difficult; railroading a tracheal tube over the FOB may take more time compared with the AIC due to inadvertent withdrawal of the FOB with subsequent oesophageal intubation;[5] looping of the FOB and impingement during railroading. Looping of the FOB occurs as it is more pliable than the AIC. Impingement during railroading is related to the relatively large gap between the FOB and the tracheal tube. With an AIC fitted over the FOB, this gap (and the risk of subsequent impingement) is decreased.[20] One manikin study on direct low skill FOI showed that, when an AIC is also preloaded onto the FOB, it significantly decreased the number of collisions with the glottis.[21]
The direct method has advantages over the indirect method: there are fewer steps; the AIC is not used, thus avoiding its associated problems (below) and the SAD does not have to be removed, thus maintaining the airway and minimising interruptions in ventilation.[19] The main disadvantage is that the SAD dictates what type of tracheal tube can be used. For example, the Proseal and Supreme LMAs fit a smaller endotracheal tube than other SADs [Table 1]. Another disadvantage is that the SAD gets in the way of surgery and needs to be removed; in cases where the tracheal tube is tight fitting within the ventilation port, removal of the SAD may be unsafe or impossible.
Advantages of the indirect method include the following:[19,22] first, the narrow AIC can be inserted into adult sizes of SAD1 and SAD2. Second, the FOB/AIC unit can be inserted through a self-sealing bronchoscopy catheter mount, allowing continued ventilation during the intubation process. Third, railroading over the AIC allows the use of larger sized tracheal tubes (≥7.0 mm), whereas in the direct method, the size of tracheal tube is limited by the diameter of the ventilation port [Table 1].
The indirect method relies on the use of the AIC, acting as a bougie over which the tracheal tube is railroaded and is associated with high success rates in both elective and emergency cases.[14,17,23] Our study demonstrated no significant differences in AIC-related problems between the various SADs, possibly suggesting that these difficulties are not surmountable regardless the design of the currently available SADs. We observed that the AIC can get dislodged and hence sheathe the tip of the FOB, preventing manipulation of the distal tip of the FOB. This makes subsequent intubation difficult or impossible. In addition, when SADs are inserted into the manikin's oropharynx, the acute angle between the vertical standing shaft and the horizontal lying bowl leads to resistance to the passage of the relatively stiff AIC through the ventilation port (24%–28% of cases).[16] Use of the AIC has also been associated with inadvertent withdrawal of the FOB out of the trachea resulting in oesophageal intubation.[5]
The decision on whether to use the direct or indirect method is based collectively on the balance of the advantages and disadvantages between both methods, the availability of SADs and AIC.[19] The size of the tracheal tube required for the clinical scenario will also be a consideration in choosing the method for low skill FOI.
Our study demonstrated that intubating SADs performed better in low skill FOI with faster intubation times and significantly less SAD- and FOB-related difficulties than the standard SAD1. The iSAD2 group showed statistically significant shorter intubation times (mean difference 15.3 s, P = 0.001), and the iSAD1 group also showed shorter intubation times which we considered to be clinically significant (mean difference 10.3 s faster, P = 0.052). Although the AmbuAuragain (an iSAD2) performed well, other SAD characteristics are also important for successful low skill FOI, as the i-gel™ (a sSAD2) performed better than LMA Protector, the other iSAD2. The AmbuAuragain had the shortest intubation times for both methods, followed by i-gel and air-Q. This is due, in part, to the lower incidences of SAD-related difficulties which, in turn, may be related to design features.
The best performing SADs in our study have design features to facilitate low skill FOI. The AmbuAuragain has a soft, rounded, anatomical curvature designed for quick and accurate placement. The i-gel is made of a medical grade thermoplastic elastomer and has a snug fitting non-inflatable cuff and a buccal cavity stabiliser.[24] It has an epiglottic rest that prevents downfolding of the epiglottis (seen in only 7% of cases) and an epiglottic ridge for stabilisation.[18,25] Both devices have a semi-rigid shaft to prevent kinking, and the widest ventilation ports amongst all the devices evaluated [internal diameter between 11 mm and 11.4 mm, Table 1].
Experience does not affect success in low skill FOI, which we similarly found as did previous patient and cadaver studies.[19,26] This supports the technique's description of being 'low skill'.
The AmbuAuragain and the i-gel came first and second, respectively, in both direct and indirect low skill FOI as preferred devices, which corresponded to objective performance profiles.
LMA Supreme results were disregarded due to a breach of the study protocol when different size tracheal tubes were inadvertently used. Regardless, we find the exclusion reasonable in light of the Difficult Airway Society describing indirect low skill FOI with LMA Supreme 'unreliable and cannot be recommended'.[1] Passage of both the FOB and AIC through the LMA Supreme is made difficult due to the acute angle between the entrance and main shaft of the ventilation port, the bulging gastric port, the shaft's semi-rigid curvature, the gastric port divides the ventilatory port into two lateral channels in the bowl making the passage narrow[27] and two epiglottic fins in the bowl may trap the FOB and AIC.[28]
It is not possible to completely eliminate the 'carry over' effect whereby the participant's competence in low skill FOI improves over several intubation attempts, as we know the learning curve to be approximately 4–6 intubations.[29] We standardised intubating conditions and performed randomisation of the sequence of SAD and method used to minimise this bias in our study results.
This study was conducted with a manikin, with attendant concessions to reality and extrapolation to actual clinical practice in patients. Success rate of intubation in clinical practice may be lower than that found in a manikin study, as seen in a study by Parikh et al.[30] evaluating performance of LSFOI through AmbuAuragain in paralysed patients whose airways were not anticipated to be difficult. They found that 5 out of 100 patients could not be intubated, while our manikin study had a 100% intubation success rate with AmbuAuragain. We appreciate that low skill FOI is most important in patients with difficult airways, especially when time to oxygenate is limited by physiological factors, and the manikin does not simulate this clinical scenario to reflect ease of SAD placement and reliability of oxygenation in a difficult airway. However, strengths in conducting a manikin study are low expense, quick recruitment and set up, avoiding ethical pitfalls and standardisation of clinical conditions.
We wish to highlight that our results are derived from low skill FOI attempts with pre-placed SADs, pre-selected SAD sizes and tracheal tube type and size. In a real emergency, optimal results in performing low skill FOI require training, frequent practice and comprehensive knowledge of the indications, practicalities and limitations of the technique.
CONCLUSION
This study demonstrated that low skill FOI consistently achieves a high intubation success rate regardless of degree of anaesthesia experience, choice of method or SAD used. Specific design features of each SAD can significantly affect the performance of low skill FOI in terms of time taken for intubation and technical difficulties encountered during the intubation process. The best performing SADs for low skill FOI in a manikin out of 6 SADs tested in our study were found to be AmbuAuragain and i-gel LMA.
Financial support and sponsorship
We are grateful for the loan of equipment used in this study: fibre-optic endoscope from Olympus Singapore Pte Ltd., air-Q from Kenda (Singapore) Pte Ltd., AmbuAuragain from Ambu Australia Pte Ltd., i-gel from T. E. Medicare Pte Ltd., Singapore and, the classic LMA, LMA Supreme, ProSeal LMA and LMA Protector from Teleflex Medical Asia Pte Ltd.
Conflicts of interest
All authors have no conflict of interest to declare.
Acknowledgments
We thank all participants and are grateful for support from the Singapore General Hospital Department of Anaesthesiology to perform the study.
REFERENCES
- 1.Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, et al. Difficult airway society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115:827–48. doi: 10.1093/bja/aev371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Myatra SN, Shah A, Kundra P, Patwa A, Ramkumar V, Divatia JV, et al. All India Difficult Airway Association 2016 guidelines for the management of unanticipated difficult tracheal intubation in adults. Indian J Anaesth. 2016;60:885–98. doi: 10.4103/0019-5049.195481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cook TM. Third generation supraglottic airway devices: An undefined concept and misused term. Time for an updated classification of supraglottic airway devices. Br J Anaesth. 2015;115:633–4. doi: 10.1093/bja/aev309. [DOI] [PubMed] [Google Scholar]
- 4.Asai T, Latto IP, Vaughan RS. The distance between the grille of the laryngeal mask airway and the vocal cords. Is conventional intubation through the laryngeal mask safe? Anaesthesia. 1993;48:667–9. doi: 10.1111/j.1365-2044.1993.tb07175.x. [DOI] [PubMed] [Google Scholar]
- 5.de Lloyd L, Hodzovic I, Voisey S, Wilkes AR, Latto IP. Comparison of fibrescope guided intubation via the classic laryngeal mask airway and i-gel in a manikin. Anaesthesia. 2010;65:36–43. doi: 10.1111/j.1365-2044.2009.06155.x. [DOI] [PubMed] [Google Scholar]
- 6.de Lloyd LJ, Subash F, Wilkes AR, Hodzovic I. A comparison of fibreoptic-guided tracheal intubation through the Ambu ® Aura-i™, the intubating laryngeal mask airway and the i-gel™: A manikin study. Anaesthesia. 2015;70:591–7. doi: 10.1111/anae.12988. [DOI] [PubMed] [Google Scholar]
- 7.Royal College of Anaesthetists. Royal College of Anaesthestists c2018. 4th National Audit Project (NAP4): Major Complications of airway Management in the United Kingdom. [Last accessed on 2018 Apr 08]. Available from: https://www.rcoa.ac.uk/system/files/CSQ-NAP4-Section3.pdf .
- 8.Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118:251–70. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 9.Frova G, Sorbello M. Algorithms for difficult airway management: A review. Minerva Anestesiol. 2009;75:201–9. [PubMed] [Google Scholar]
- 10.Joffe AM, Liew EC, Galgon RE, Viernes D, Treggiari MM. The second-generation air-Q intubating laryngeal mask for airway maintenance during anaesthesia in adults: A report of the first 70 uses. Anaesth Intensive Care. 2011;39:40–5. doi: 10.1177/0310057X1103900106. [DOI] [PubMed] [Google Scholar]
- 11.Theiler L, Gutzmann M, Kleine-Brueggeney M, Urwyler N, Kaempfen B, Greif R, et al. I-gel™ supraglottic airway in clinical practice: A prospective observational multicentre study. Br J Anaesth. 2012;109:990–5. doi: 10.1093/bja/aes309. [DOI] [PubMed] [Google Scholar]
- 12.Pandit JJ, MacLachlan K, Dravid RM, Popat MT. Comparison of times to achieve tracheal intubation with three techniques using the laryngeal or intubating laryngeal mask airway. Anaesthesia. 2002;57:128–32. doi: 10.1046/j.0003-2409.2001.02401.x. [DOI] [PubMed] [Google Scholar]
- 13.Higgs A, Clark E, Premraj K. Low-skill fibreoptic intubation: Use of the aintree catheter with the classic LMA. Anaesthesia. 2005;60:915–20. doi: 10.1111/j.1365-2044.2005.04226.x. [DOI] [PubMed] [Google Scholar]
- 14.Cook TM, Silsby J, Simpson TP. Airway rescue in acute upper airway obstruction using a ProSeal Laryngeal mask airway and an Aintree Catheter: A review of the ProSeal Laryngeal mask airway in the management of the difficult airway. Anaesthesia. 2005;60:1129–36. doi: 10.1111/j.1365-2044.2005.04370.x. [DOI] [PubMed] [Google Scholar]
- 15.Kleine-Brueggeney M, Theiler L, Urwyler N, Vogt A, Greif R. Randomized trial comparing the i-gel™ and Magill tracheal tube with the single-use ILMA™ and ILMA™ tracheal tube for fibreoptic-guided intubation in anaesthetized patients with a predicted difficult airway. Br J Anaesth. 2011;107:251–7. doi: 10.1093/bja/aer103. [DOI] [PubMed] [Google Scholar]
- 16.Cook TM, Lee G, Nolan JP. The proSeal laryngeal mask airway: A review of the literature. Can J Anaesth. 2005;52:739–60. doi: 10.1007/BF03016565. [DOI] [PubMed] [Google Scholar]
- 17.Blair EJ, Mihai R, Cook TM. Tracheal intubation via the Classic and Proseal laryngeal mask airways: A manikin study using the Aintree Intubating Catheter. Anaesthesia. 2007;62:385–7. doi: 10.1111/j.1365-2044.2007.04994.x. [DOI] [PubMed] [Google Scholar]
- 18.Theiler LG, Kleine-Brueggeney M, Kaiser D, Urwyler N, Luyet C, Vogt A, et al. Crossover comparison of the laryngeal mask supreme and the i-gel in simulated difficult airway scenario in anesthetized patients. Anesthesiology. 2009;111:55–62. doi: 10.1097/ALN.0b013e3181a4c6b9. [DOI] [PubMed] [Google Scholar]
- 19.Olesnicky BL, Rehak A, Bestic WB, Brock JT, Watterson L. A cadaver study comparing three fibreoptic-assisted techniques for converting a supraglottic airway to a cuffed tracheal tube. Anaesthesia. 2017;72:223–9. doi: 10.1111/anae.13733. [DOI] [PubMed] [Google Scholar]
- 20.Asai T, Shingu K. Difficulty in advancing a tracheal tube over a fibreoptic bronchoscope: Incidence, causes and solutions. Br J Anaesth. 2004;92:870–81. doi: 10.1093/bja/aeh136. [DOI] [PubMed] [Google Scholar]
- 21.Ueki R, Komasawa N, Nishimoto K, Sugi T, Hirose M, Kaminoh Y, et al. Utility of the aintree intubation catheter in fiberoptic tracheal intubation through the three types of intubating supraglottic airways: A manikin simulation study. J Anesth. 2014;28:363–7. doi: 10.1007/s00540-013-1724-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cook TM, Seller C, Gupta K, Thornton M, O'Sullivan E. Non-conventional uses of the Aintree Intubating Catheter in management of the difficult airway. Anaesthesia. 2007;62:169–74. doi: 10.1111/j.1365-2044.2006.04909.x. [DOI] [PubMed] [Google Scholar]
- 23.Wong DT, Yang JJ, Mak HY, Jagannathan N. Use of intubation introducers through a supraglottic airway to facilitate tracheal intubation: A brief review. Can J Anaesth. 2012;59:704–15. doi: 10.1007/s12630-012-9714-8. [DOI] [PubMed] [Google Scholar]
- 24.Intersurgical Complete Respiratory Systems. Intersurgical Ltd. i-gel User Guide-Intersurgical. c2018. [Last accessed on 2018 Apr 08]. Available from: http://www.intersurgical.com/content/files/80023/1103318462 .
- 25.Levitan RM, Kinkle WC. Initial anatomic investigations of the I-gel airway: A novel supraglottic airway without inflatable cuff. Anaesthesia. 2005;60:1022–6. doi: 10.1111/j.1365-2044.2005.04258.x. [DOI] [PubMed] [Google Scholar]
- 26.Hodzovic I, Janakiraman C, Sudhir G, Goodwin N, Wilkes AR, Latto IP, et al. Fibreoptic intubation through the laryngeal mask airway: Effect of operator experience. Anaesthesia. 2009;64:1066–71. doi: 10.1111/j.1365-2044.2009.06030.x. [DOI] [PubMed] [Google Scholar]
- 27.Cook TM, Gatward JJ, Handel J, Hardy R, Thompson C, Srivastava R, et al. Evaluation of the LMA supreme in 100 non-paralysed patients. Anaesthesia. 2009;64:555–62. doi: 10.1111/j.1365-2044.2008.05824.x. [DOI] [PubMed] [Google Scholar]
- 28.Greenland KB, Tan H, Edwards M. Intubation via a laryngeal mask airway with an Aintree catheter – Not all laryngeal masks are the same. Anaesthesia. 2007;62:966–7. doi: 10.1111/j.1365-2044.2007.05235.x. [DOI] [PubMed] [Google Scholar]
- 29.Atherton DP, O'Sullivan E, Lowe D, Charters P. A ventilation-exchange bougie for fibreoptic intubations with the laryngeal mask airway. Anaesthesia. 1996;51:1123–6. doi: 10.1111/j.1365-2044.1996.tb15047.x. [DOI] [PubMed] [Google Scholar]
- 30.Parikh DA, Jain RA, Lele SS, Tendolkar BA. A cohort evaluation of clinical use and performance characteristics of Ambu(®) AuraGain™: A prospective observational study. Indian J Anaesth. 2017;61:636–42. doi: 10.4103/ija.IJA_285_17. [DOI] [PMC free article] [PubMed] [Google Scholar]


