Abstract
Background and Aims:
Ultrasonography (USG)-guided transversus abdominis plane (TAP) block is an abdominal field block with high efficacy. This study was undertaken with the aim of determining the effect of the addition of dexamethasone to 0.5% ropivacaine on post-operative analgesia in USG-guided TAP block for inguinal hernia repair.
Methods:
A double-blind randomised control study was conducted on sixty patients posted for inguinal hernia repair with the American Society of Anesthesiologists physical Status I or II, who were allocated two groups of 30 each. Patients in Group RS received 0.5% ropivacaine (20 ml) and normal saline (2 ml) whereas patients in Group RD received 0.5% ropivacaine (20 ml) and dexamethasone (2 ml, i.e., 8 mg), in USG-guided TAP Block on the same side, after repair of inguinal hernia under spinal anaesthesia. Visual analogue scale (VAS) scores, time for request of first analgesia and total tramadol consumption in first 24 h were compared. Unpaired Student's t-test and Mann–Whitney U-test were performed using SPSS 23 Software.
Results:
Patients in Group RD had significantly lower VAS scores as compared to Group RS from 4th to 12th h, postoperatively. Duration of analgesia was significantly more in Group RD (547.50 [530,530] min) when compared with Group RS (387.50 [370,400] min) (P < 0.001). The demand for intravenous tramadol was significantly low in Group RD (223.33 ± 56.83 mg) as compared to Group RS (293.33 ± 25.71 mg) (P < 0.001).
Conclusion:
Addition of dexamethasone to ropivacaine in USG-guided TAP block significantly reduces post-operative pain and prolongs the duration of post-operative analgesia, thereby reducing analgesic consumption.
Key words: Dexamethasone, ropivacaine, transversus abdominis plane block, ultrasonography
INTRODUCTION
Surgical stress response occurring as a result of uncontrolled pain after surgeries severely affects various physiological functions, even leading to increased perioperative morbidity and mortality. Hence, effective post-operative analgesia is an essential component of the care of surgical patients.[1] Regional anaesthesia with local anaesthetic agents not only inhibits the stress response to surgery but also improves the post-operative outcome. Post-operative pain in inguinal hernia repair is best treated with multimodal approach combining locoregional analgesia (transversus abdominis plane [TAP] block), non-steroidal anti-inflammatory drugs and opioids.[2]
Ultrasonography-guided TAP block is an effective peripheral abdominal field block that blocks the ilioinguinal, iliohypogastric and lower intercostal (T7–T11) nerves.[3] TAP block has been utilised as a part of multimodal regime for post-operative analgesia in various surgical procedures involving lower abdominal wall incision. For regional anaesthesia, local anaesthetics alone provide good operative conditions but have shorter duration of post-operative analgesia. Hence, various adjuvants such as opioids, clonidine and ketamine are added to local anaesthetics to achieve a quick, dense and prolonged block, but their use is limited by side effects such as nausea, vomiting and pruritus.[4] Dexamethasone, a very potent and highly selective glucocorticoid has been used as an adjuvant to local anaesthetics in various nerve blocks resulting in variable effects on onset but prolonged duration of analgesia and motor block.[5]
The aim of our study was to determine the effect of dexamethasone on post-operative analgesia when added to 0.5% ropivacaine in USG-guided TAP block for inguinal hernia repair. The primary objective of the study was to compare the quality and duration of post-operative analgesia.
METHODS
This prospective, randomised, double-blinded study was conducted after approval from Hospital's Ethical Committee over a period of 6 months. A written and informed consent was taken from the patient after explaining the procedure to the patient. Patients with the American Society of Anesthesiologists (ASA) physical Status I or II, aged 18–65 years, with body mass index <30 kg/m2 undergoing open surgery for elective inguinal hernia repair were included in the study. The exclusion criteria included patient refusal, patient with known hypersensitivity to local anaesthetics, patient with opioid addiction, bleeding diathesis, any chronic systemic illness, anatomical abnormality, infection at the regional site, peripheral neuropathy and neurological deficits. Matched pair randomisation was used for the study where patients were grouped into pairs based on having similar observable characteristics. One unit in each pair was randomly assigned to the treatment group and the other to the control group. Patients in Group RS received 20 ml 0.5% ropivacaine (Aesmira Pharmaceuticals, India) +2 ml normal saline with total volume of 22 ml whereas patients in Group RD received 20 ml 0.5% ropivacaine +2 ml dexamethasone (8 mg) (Zee Pharmaceuticals, India) with total volume of 22 ml. Sealed opaque envelopes containing group allocation were opened just before performing the TAP block. During pre-anaesthetic workup patient's detailed history, general physical examination and systemic examination was carried out. Routine investigations as per recent guidelines were also noted. The patient was explained in detail about the anaesthesia procedure, drugs and visual analogue scale (VAS) score (from 0-100).[6] On arriving inside operating room, standard ASA monitoring was attached. A large bore (18 G) intravenous (IV) cannula was inserted under local anaesthesia in a peripheral vein. The patient was pre-medicated with midazolam 0.02 mg/kg IV. Co-loading with a crystalloid solution at 10 mL/kg was done while administering spinal anaesthesia. Under aseptic precautions, spinal anaesthesia was administered using 3 ml 0.5% bupivacaine (hyperbaric) at L3–4 or L4–5 interspace with 25 gauge Quincke tip Spinal needle (B. Braun; Melsungen, Germany). Electrocardiogram and oxygen saturation with pulse oximeter (SpO2) were monitored continuously, and non-invasive blood pressure was recorded every 5 min during the intraoperative period.
After completion of the surgical procedure, the patient was administered USG-guided TAP block. First, skin was prepared with antiseptic, followed by draping with sterile cloth. The Ultrasound probe (M-turbo 11-mm broadband linear array, 6–14 MHz; Sonosite, Bothell, Washington, USA) was sheathed. After identifying the lower costal margin and iliac crest, the ultrasound probe was placed in the midaxillary line between them, in a transverse plane to the lateral abdominal wall to obtain a transverse view of the abdominal layers. A 22G needle was inserted 1 cm medial to the probe and advanced using the in-plane technique with real-time assessment using USG. The injection site was defined between aponeurosis of internal oblique and transversus abdominis muscles. After the tip of needle was correctly placed, 2 ml drug was injected to hydrodissect the tissue followed by injection of drug in 5 ml increments with gentle intermittent aspiration. During the injection, the distribution of local anaesthetic solution was observed as a hypoechoic enlargement on USG. Specific drug combinations were prepared by individual anaesthesiologist who was not part of the study. During administration of TAP block, drug injection was stopped if the needle slid into muscle (to avoid intramuscular spread and haematoma formation) or if any signs or symptoms of toxicity appeared. The patient was then transferred to post-operative ward where injection tramadol 2 mg/kg IV was given as rescue analgesic on VAS score >40 or on patient's demand, whichever first.
The primary outcome of the study was duration of analgesia which was defined as the time interval from completion of local anaesthetic administration till first demand of analgesic, and the quality of analgesia as determined by VAS score at predefined intervals at 2, 4, 6, 8, 10, 12, 18 and 24 h. The secondary outcomes included total tramadol consumption, post-operative adverse effects and complications (haemodynamic instability, respiratory depression, nausea, vomiting, transient femoral nerve palsy, haematoma at site of injection) during post-operative period up to 24 h. In addition, regression of motor block due to spinal anaesthesia was assessed using Modified Bromage Score to exclude the failed spinal anaesthesia, if any.[7]
A power analysis based on time for analgesia in a previous study carried out on TAP block by Ammar and Mahmoud[8] revealed that 30 patients in each group would be sufficient to detect difference in the duration of analgesia with a significant interval of 1 h, with α error = 0.05, β error = 0.20, power of study at 80% and confidence limit of 95%. Statistical analysis was done using SPSS 23 software (IBM SPSS, trial version, New York, USA). The Kolmogorov–Smirnov test was used to verify the normal distribution of continuous variables. Normally distributed continuous variables were compared using unpaired Student's t-test. Mann–Whitney U-test was performed for comparison of VAS scores and time for analgesia. Tramadol consumption was also compared using unpaired Student's t-test. Continuous variables were expressed as mean ± standard deviation or median with interquartile range as deemed appropriate. Categorical variables were compared using Chi-square test. All analyses were two-tailed and P < 0.05 was considered statistically significant.
RESULTS
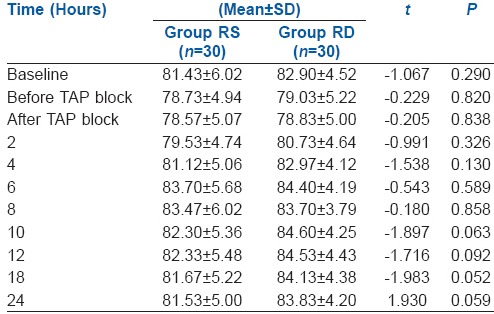
Both groups were matched for the demographic data [Table 1]. Duration of analgesia was significantly more in dexamethasone containing Group RD (547.50 (530,530) min) when compared with Group RS (387.50 (370,400) min) (P < 0.000) [Table 2]. Patients in Group RD had significantly lower VAS scores as compared to Group RS from 4th to 12th h of post-operative period [Figure 1 and Table 3]. Patients of dexamethasone containing Group RD had lower tramadol requirement ([223.33 ± 56.83 mg] vs. [293.33 ± 25.71 mg] [P < 0.001]) [Table 2] and lower incidence of nausea and vomiting as compared to Group RS [Table 4]. No statistical difference was observed between both the groups regarding patient's haemodynamic variables [Table 5a–d in online supplement]. No complications attributable to TAP block were observed.
Table 1.
Comparison between the two groups according to demographic data (n=30)
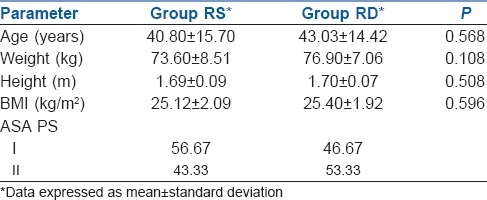
Table 2.
Comparison between the results of two groups (n=30)
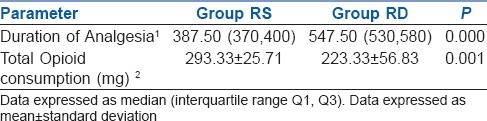
Figure 1.
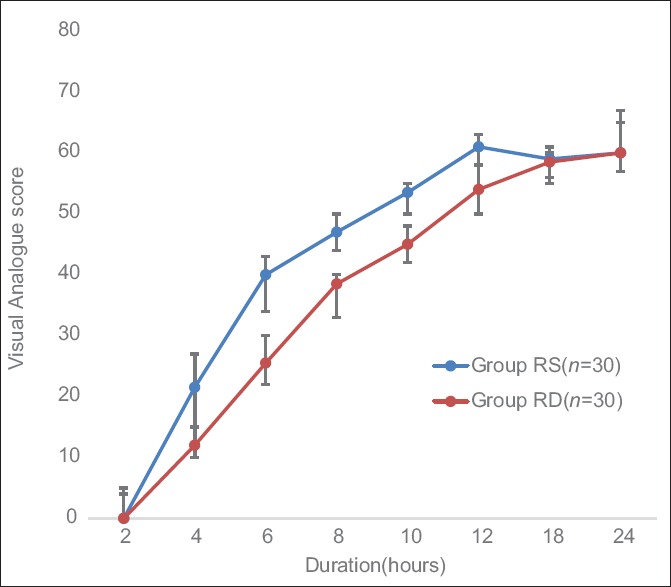
Change in visual analogue scale score
Table 3.
Comparison between the two groups according to VAS
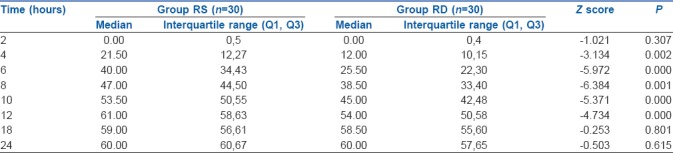
Table 4.
Incidence of post-operative side effects
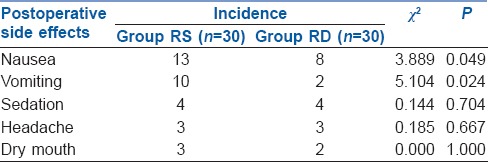
Table 5a.
Change in heart rate
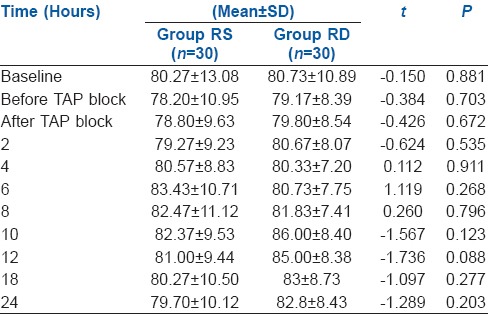
Table 5d.
Change in mean arterial pressure in mmHg
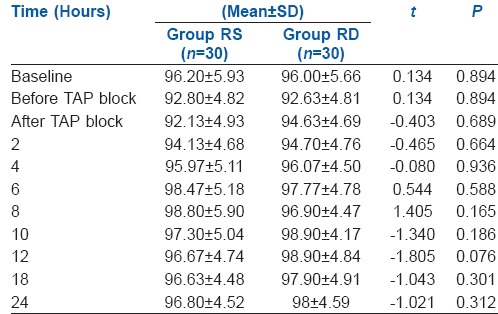
Table 5b.
Change in systolic blood pressure in mmHg
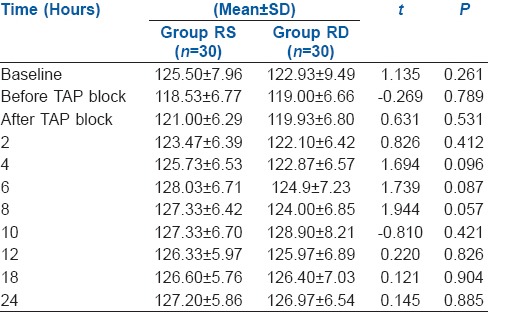
Table 5c.
Change in diastolic blood pressure in mmHg
DISCUSSION
The current study discusses the effects of addition of dexamethasone to ropivacaine in USG-guided TAP block for inguinal hernia repair. Following inguinal hernia repair, multi-modal pain therapy (balanced analgesia) is the recommended technique for treatment of post-operative pain.[9,10] The use of regional anaesthesia along with conventional oral and IV analgesics have resulted in improved outcomes. 0.5% ropivacaine was used in this study instead of 0.25% as it provides denser analgesia as observed in various previous studies.[11,12]
Addition of dexamethasone to local anaesthetics as an adjuvant increased the duration of TAP block (RD vs. RS; 547.50 (530,530) min vs. RS 387.50 (370,400) min, respectively). The increase in the duration was similar to the previous studies.[13] Dexamethasone exerts it is analgesic action by inhibiting transmission and neural discharge in nociceptive C-fibres. Hence, the duration of anaesthesia is prolonged due to dexamethasone additive action.[14] Steroids prolongs analgesia when administered as adjuvant in regional blocks but the results have been variable depending on the dosage of dexamethasone, local anaesthetic and it's concentration and site of block. Duration of prolongation of analgesia with dexamethasone is highly variable with few studies suggesting analgesia up to 20–24 h while others suggest only up to 12–16 h as observed in this study.[8,15,16] Furthermore, it has also been found that dexamethasone at doses more than 0.1 mg/kg is an effective adjunct in multimodal strategies to reduce post-operative pain and opioid consumption after surgery.[17,18] Considering the fact that doses <0.1 mg/kg failed to produce any opioid-sparing effect when administered IV, combined with the result of the study conducted by Desmet et al.[19] claiming that IV and perineural dexamethasone are equivalent in increasing the analgesic duration of regional anaesthesia, 8 mg dexamethasone was used as an adjuvant with ropivacaine.
Addition of dexamethasone to ropivacaine in TAP block resulted in significant reduction of tramadol consumption (RD vs. RS; [223.33 ± 56.83 mg] vs. [293.33 ± 25.71 mg], respectively). This was found to be associated with decreased side effects. Similar results have been reiterated by various previous studies.[20] Decreased nausea and vomiting associated with dexamethasone can be explained due to various reasons such as anti-inflammatory effect, direct central action at the solitary tract nucleus, interaction with the neurotransmitter serotonin, and receptor proteins tachykinin NK1 and NK2 and alpha-adrenaline maintaining the normal physiological functions of organs and systems, regulation of the hypothalamic–pituitary–adrenal axis, reducing pain and the concomitant use of opioids, which in turn reduces opioid-related nausea and vomiting.[21]
One limitation of the current study is use of spinal anaesthesia for conduction of surgery. As TAP block was administered before wearing off of spinal anaesthesia, potentiation of TAP block by spinal anaesthesia cannot be denied but as difference in VAS scores starts from 4th h onwards, when motor block has almost worn off, there seems to be no effect on adjuvant action of dexamethasone. Furthermore, lower doses of dexamethasone can be considered as an adjuvant in regional anaesthesia in future practice as more and more researches find no significant difference between different doses of dexamethasone being used in regional anaesthetic blocks.[22]
CONCLUSION
The addition of dexamethasone to ropivacaine in USG-guided TAP block significantly prolongs the duration of post-operative analgesia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would like to acknowledge Dr. Dilip Singh Chouhan, Senior Professor and Head of Department, Department of Anaesthesiology and Critical Care.
REFERENCES
- 1.Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Br J Anaesth. 2001;87:62–72. doi: 10.1093/bja/87.1.62. [DOI] [PubMed] [Google Scholar]
- 2.Demirci A, Efe EM, Türker G, Gurbet A, Kaya FN, Anil A, et al. Iliohypogastric/ilioinguinal nerve block in inguinal hernia repair for postoperative pain management: Comparison of the anatomical landmark and ultrasound guided techniques. Braz J Anesthesiol. 2014;64:350–6. doi: 10.1016/j.bjan.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 3.Wang Y, Wu T, Terry MJ, Eldrige JS, Tong Q, Erwin PJ, et al. Improved perioperative analgesia with ultrasound-guided ilioinguinal/iliohypogastric nerve or transversus abdominis plane block for open inguinal surgery: A systematic review and meta-analysis of randomized controlled trials. Phys Med Rehabil Int. 2015;2:1055–9. doi: 10.1589/jpts.28.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karakaya D, Büyükgöz F, Bariş S, Güldoǧuş F, Tür A. Addition of fentanyl to bupivacaine prolongs anesthesia and analgesia in axillary brachial plexus block. Reg Anesth Pain Med. 2001;26:434–8. doi: 10.1053/rapm.2001.24675. [DOI] [PubMed] [Google Scholar]
- 5.Cummings KC, 3rd, Napierkowski DE, Parra-Sanchez I, Kurz A, Dalton JE, Brems JJ, et al. Effect of dexamethasone on the duration of interscalene nerve blocks with ropivacaine or bupivacaine. Br J Anaesth. 2011;107:446–53. doi: 10.1093/bja/aer159. [DOI] [PubMed] [Google Scholar]
- 6.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS pain), Numeric Rating Scale for Pain (NRS pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP) Arthritis Care Res (Hoboken) 2011;63(Suppl 11):S240–52. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 7.Breen TW, Shapiro T, Glass B, Foster-Payne D, Oriol NE. Epidural anesthesia for labor in an ambulatory patient. Anesth Analg. 1993;77:919–24. doi: 10.1213/00000539-199311000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Ammar AS, Mahmoud KM. Effect of adding dexamethasone to bupivacaine on transversus abdominis plane block for abdominal hysterectomy: A prospective randomized controlled trial. Saudi J Anaesth. 2012;6:229–33. doi: 10.4103/1658-354X.101213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joshi GP. Multimodal analgesia techniques and postoperative rehabilitation. Anesthesiol Clin North America. 2005;23:185–202. doi: 10.1016/j.atc.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Kehlet H, Dahl JB. The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg. 1993;77:1048–56. doi: 10.1213/00000539-199311000-00030. [DOI] [PubMed] [Google Scholar]
- 11.Sharma N, Mehta N, Sharma S. An evaluation of (0.25%) bupivacaine vs. (0.5%) ropivacaine for postoperative analgesia using ultrasound guided transversus abdominis plane block for abdominal surgeries: A comparative study. Indian J Clin Anaesth. 2016;3:635–9. [Google Scholar]
- 12.Su Y, Zhang Z, Zhang Y, Li H, Shi W. Efficacy of ropivacaine by the concentration of 0.25%, 0.5%, and 0.75% on surgical performance, postoperative analgesia, and patient’s satisfaction in inguinal hernioplasty: A randomized controlled trial. Patient Prefer Adherence. 2015;9:1375–9. doi: 10.2147/PPA.S93276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rasmussen SB, Saied NN, Bowens C, Jr, Mercaldo ND, Schildcrout JS, Malchow RJ, et al. Duration of upper and lower extremity peripheral nerve blockade is prolonged with dexamethasone when added to ropivacaine: A retrospective database analysis. Pain Med. 2013;14:1239–47. doi: 10.1111/pme.12150. [DOI] [PubMed] [Google Scholar]
- 14.De la Fuente N, Altermatt FR. Adding dexamethasone to peripheral nerve blocks can give better postoperative analgesia. Br J Anaesth. 2012;108:161. doi: 10.1093/bja/aer426. [DOI] [PubMed] [Google Scholar]
- 15.Fouad HA, Mohammed A, Ahmed S, Mohammed Y, Osman M, Mohammed G, et al. Efficacy of preemptive dexamethasone added to bupivacaine in ultrasound guided transversus abdominus plain block for postoperative analgesia after inguinal herniorrhaphy. Am J Res Commun. 2016;4:27–42. [Google Scholar]
- 16.Kartalov A, Jankulovski N, Kuzmanovska B, Zdravkovska M, Shosholcheva M, Spirovska T, et al. Effect of adding dexamethasone as a ropivacaine adjuvant in ultrasound-guided transversus abdominis plane block for inguinal hernia repair. Pril (Makedon Akad Nauk Umet Odd Med Nauki) 2015;36:35–41. doi: 10.1515/prilozi-2015-0076. [DOI] [PubMed] [Google Scholar]
- 17.Knezevic NN, Anantamongkol U, Candido KD. Perineural dexamethasone added to local anesthesia for brachial plexus block improves pain but delays block onset and motor blockade recovery. Pain Physician. 2015;18:1–4. [PubMed] [Google Scholar]
- 18.De Oliveira GS, Jr, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: A meta-analysis of randomized controlled trials. Anesthesiology. 2011;115:575–88. doi: 10.1097/ALN.0b013e31822a24c2. [DOI] [PubMed] [Google Scholar]
- 19.Desmet M, Braems H, Reynvoet M, Plasschaert S, Van Cauwelaert J, Pottel H, et al. And perineural dexamethasone are equivalent in increasing the analgesic duration of a single-shot interscalene block with ropivacaine for shoulder surgery: A prospective, randomized, placebo-controlled study. Br J Anaesth. 2013;111:445–52. doi: 10.1093/bja/aet109. [DOI] [PubMed] [Google Scholar]
- 20.Abdalla W. Ultrasound-guided transversus abdominis plane block for radical cystectomy with and without dexamethasone: A prospective, double-blinded controlled trial. Ain Shams J Anaesthesiol. 2014;7:539–44. [Google Scholar]
- 21.Chu CC, Hsing CH, Shieh JP, Chien CC, Ho CM, Wang JJ, et al. The cellular mechanisms of the antiemetic action of dexamethasone and related glucocorticoids against vomiting. Eur J Pharmacol. 2014;722:48–54. doi: 10.1016/j.ejphar.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 22.Tandoc MN, Fan L, Kolesnikov S, Kruglov A, Nader ND. Adjuvant dexamethasone with bupivacaine prolongs the duration of interscalene block: A prospective randomized trial. J Anesth. 2011;25:704–9. doi: 10.1007/s00540-011-1180-x. [DOI] [PubMed] [Google Scholar]


