Abstract
Reports on the burden of heart failure (HF) have largely omitted HF diagnosed in outpatient settings. We quantified annual incidence rates (IR, per 1,000 person years) of HF identified in ambulatory clinics, emergency departments (EDs), and during hospital stays in a national probability sample of Medicare beneficiaries from 2008 to 2014, by age and race/ethnicity. A 20% random sample of Medicare beneficiaries ages ≥65 years with continuous Medicare Parts A, B, and D coverage was used to estimate annual IRs of HF identified using ICD-9-CM codes. Of the 681,487 beneficiaries with incident HF from 2008–2014, 283,451 (41%) presented in ambulatory clinics, 76,919 (11%) in EDs, and 321,117 (47%) in hospitals. Overall, incidence of HF in ambulatory clinics decreased from 2008 (IR=22.2, 95% CI: 22.0, 22.4) to 2014 (IR=15.0, 95% CI: 14.8, 15.1). Similarly, incidence of HF-related ED visits without an admission to the hospital decreased somewhat from 2008 (IR=5.5, 95% CI: 5.4, 5.6) to 2012 (IR=4.2, 95% CI: 4.1, 4.3) and stabilized from 2013 to 2014. Similar to previous reports, HF hospitalizations, both ICD-9-CM code 428.x in the primary and any position, decreased over the study period. Over half of all new cases of HF among Medicare beneficiaries presented in an ambulatory clinic or ED. The overall incidence of HF decreased from 2008 to 2014, regardless of health care setting. In conclusion, consideration of outpatient HF is warranted to better understand the burden of HF and its temporal trends.
Keywords: heart failure, incidence, Medicare, ambulatory care
Introduction
Heart failure (HF) is the leading hospital discharge diagnosis among Medicare beneficiaries1. To reduce morbidity and cost, the Centers for Medicare and Medicaid Services (CMS) initiated public reporting of HF hospital readmission rates in 2009 and, in 2010, established financial penalties for hospitals with high readmission rates 2. Strategies to reduce HF-related hospital admissions and readmissions have led to increased diagnosis and management of HF in ambulatory care clinics and emergency departments (EDs) 3, 4. It has been posited that policy changes in financial reimbursements may have prompted an increase in HF management in the ED in lieu of an inpatient stay 4. These questions highlight the need to assess occurrence and temporal trends of HF care in ambulatory clinics and emergency departments. Few studies have described ambulatory HF 5–8, and none have reported on HF-related ambulatory clinic visits separately from HF-related ED visits. The objective of this study was to quantify and compare annual incidence rates of HF diagnosed in the ambulatory clinic, the ED (not resulting in a hospital admission), and during hospital admissions. We hypothesized that US policy and payment changes would drive some diagnosis and treatment of HF patients to non-hospitalized settings, resulting in a modest decrease in incidence of hospitalized HF and a corresponding increase in the incidence of HF-related ambulatory clinic and ED visits.
Methods
Our source population was a 20% random sample of all CMS Medicare beneficiaries age ≥65 years with Medicare fee-for-service Parts A, B, and D coverage for ≥1 calendar month during 2007–2014. Beneficiaries were randomly selected by CMS based on the beneficiary ID number. Once a beneficiary met this selection criterion, all available fee-for-service claims and death data were included through the end of 2014, disenrollment from Medicare fee-for-service Parts A and B, or death, whichever came first.
Information concerning beneficiary enrollment in fee-for-service Parts A and B was obtained from the annual Medicare Beneficiary Summary files. Continuous enrollment periods were created to indicate uninterrupted fee-for-service coverage in Parts A and B and lack of enrollment in a Medicare Advantage (HMO) plan. Medicare Provider Annual Review (MedPAR, Part A), Carrier, and Outpatient files (Part B) were merged with denominator files containing demographic and enrollment information including race/ethnicity, date of birth, sex, and enrollment dates.
For participants with multiple enrollment periods, the first enrollment period was selected to minimize misclassification of prevalent HF as incident. To further minimize misclassification, we established a 2-year look-back period (the first 2 years of continuous fee-for-service enrollment) free of HF-related Medicare claims 9. Therefore, beneficiaries were included if they were enrolled in continuous Medicare fee-for-service Parts A and B for >2 years resulting in a cohort of Medicare beneficiaries age ≥67 years.
Outpatient HF was identified from Carrier claims with Current Procedural Terminology (CPT) Evaluation and Management service codes for new and established outpatient visits (99201–99205), consultations (99241–99245), and established preventive medicine visits (99395–99397) and from Outpatient claims as visits to Federally Qualified Healthcare Center (revenue center codes 520–521). Identified visits were matched with Carrier (Part B) claims and claims for outpatient services, respectively. Using provider specialty codes to identify provider types, we identified outpatient clinic visits, patients seen and released from the ED, and observation stays. Outpatient clinic visits were classified as ambulatory clinic visits. ED visits and observation stays that did not result in a hospitalization were classified as ED visits. Hospitalized HF was identified from annual MedPAR records.
HF-related claims were identified using HF-specific International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 428.x in any position. Regarding HF hospitalizations, 428.x in the primary position, an indication that HF was the primary diagnosis for a hospitalization, is specific (99%); however, its sensitivity is low (33%) 10. With a broader ICD-9-CM code definition of 428.x in any position, the specificity decreases (86%) but the sensitivity increases substantially (83%) 10. Thus, we identified HF hospitalizations using 2 ICD-9-CM code definitions: ICD-9-CM code of 428.x in any position and ICD-9-CM code of 428.x in the primary position.
Incident HF was defined as the first HF claim, regardless of health care setting, observed after the established look-back period. If a beneficiary was hospitalized, seen in the ED, or visited an ambulatory clinic for a HF-related reason (ICD-9-CM code of 428.x) during the 2-year look-back period, they were classified as having prevalent HF. Beneficiaries with prevalent HF were excluded.
To our knowledge, there are no validation studies for outpatient HF ICD-9-CM code algorithms 10. Thus we conducted a sensitivity analysis by including a more specific definition of ambulatory clinic HF. An “ambulatory HF-related visit with confirmation” was defined as a HF-related visit to a primary care physician or cardiologist with a second HF-related visit to the ambulatory clinic, ED, or hospital within 365 days of the initial ambulatory clinic visit. The date of the first ambulatory clinic visit was considered the date of incident HF.
Demographic information on age (recorded on July 1 of enrollment year), race/ethnicity, and gender was obtained from annual Medicare beneficiary summary files. Age was categorized as 67–69 years, 70–74 years, 75–79 year, 80–84 years, and ≥85 years. Race/ethnicity was categorized as non-Hispanic white, black, Hispanic, Asian, Native American, and other. Medicare beneficiaries were excluded if they had a self-identified race of “other”. We considered hospital and outpatient claims for comorbidities prior to incident HF, including during the 2-year look-back period and during the incident visit. All claims for comorbidities in each calendar year (prior to an incident HF) were used. Diagnostic codes for comorbidities are presented in Supplemental Table 1.
Descriptive characteristics were expressed as counts and percentages. Poisson regression models were used to estimate annual crude and age-adjusted incidence rates per 1,000 person-years and corresponding 95% confidence intervals (CI). The analyses and presentation of results were stratified by age group (65–74, 75–79, 80–84, and ≥85 years) and race/ethnicity (white, black, Hispanic, Asian, and Native American). Incidence rate ratios (IRR) were estimated to determine differences in incidence between sex, age, and race/ethnic groups.
All analyses were conducted using SAS V9.3 (SAS Inc. Cary, North Carolina). This study was approved/exempted by the UNC Institutional Review Board. Individual informed consent was not required.
Results
Of the 681,487 CMS Medicare fee-for-service beneficiaries in the 20% random sample with incident HF from 2008 to 2014, 283,451 (41%) first presented in the ambulatory clinic, 76,919 (11%) in the ED, and 321,117 (47%) in the hospital. Compared with beneficiaries whose incident HF occurred in the ambulatory clinic, beneficiaries seen and released from the ED at the time of their initial HF diagnosis were more likely to be women (63% vs. 56%), age ≥85 years (26% vs. 20%), and black (11% vs. 8%, Table 1). Beneficiaries admitted to the hospital had similar demographic characteristics to those treated in the ED. Beneficiaries admitted to the hospital for their initial HF diagnosis generally had a greater proportion of comorbidities than beneficiaries whose incident HF presented in the ambulatory clinic or ED (Table 1). During the years 2008 to 2014, incidence rates of hospitalized HF (428.x in any position) were higher compared to rates of HF diagnosed in the ambulatory clinic, ED, and the hospital (with a primary diagnostic code, Figure 1). Demographic characteristics by year are presented in Supplemental Table 2.
Table 1.
Descriptive characteristics of a random 20% sample of Medicare fee-for-service beneficiaries with parts A and B for ≥2 years with incident heart failure, overall and by health care setting of incident heart failure (2008–2014)
| Health Care Setting of Heart Failure Incidence | ||||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Overall (N = 691,092) | Ambulatory Clinic (N = 287,866) | Emergency Department (N = 78,407) | Hospital (N = 324,819) | |||||
|
|
||||||||
| % Female | 410,800 | (59%) | 160,329 | (56%) | 49,508 | (63%) | 200,963 | (62%) |
| Age (years)a | ||||||||
| 67–69 | 143,289 | (21%) | 63,864 | (22%) | 16,977 | (22%) | 62,448 | (19%) |
| 70–74 | 118,058 | (17%) | 54,003 | (19%) | 12,511 | (16.0%) | 51,544 | (16%) |
| 75–79 | 128,402 | (19%) | 56,166 | (20%) | 13,438 | (17%) | 58,798 | (18%) |
| 80–84 | 133,092 | (19%) | 53,904 | (19%) | 14,623 | (19%) | 64,565 | (20%) |
| ≥85 | 162,511 | (24%) | 56,916 | (20%) | 19,960 | (26%) | 85,635 | (26%) |
| Race | ||||||||
| White | 582,774 | (84%) | 243,035 | (84%) | 66,228 | (85) | 273,511 | (84%) |
| Black | 64,254 | (9%) | 23,633 | (8.2%) | 8,229 | (11%) | 32,392 | (10%) |
| Hispanic | 11,696 | (1.7%) | 5,964 | (2.1%) | 624 | (0.8%) | 5,108 | (1.6%) |
| Asian | 14,992 | (2.2%) | 6,882 | (2.4%) | 1,277 | (1.6%) | 6,833 | (2.1%) |
| Native American | 3,259 | (0.5%) | 1,273 | (0.4%) | 499 | (0.6%) | 1,487 | (0.5%) |
| Other | 7,234 | (1.0%) | 3,567 | (1.2%) | 539 | (0.7%) | 3,128 | (1.0%) |
| Missing | 1,143 | (0.2%) | 499 | (0.2%) | 113 | (0.1%) | 531 | (0.2%) |
| Comorbidities | ||||||||
| Cardiomyopathy | 85,595 | (12%) | 27,577 | (9.6%) | 6,434 | (8.2%) | 51,584 | (16%) |
| Dyspnea and respiratory abnormalities | 30,032 | (4.3%) | 9,580 | (3.3%) | 3,122 | (4.0%) | 17,330 | (5.3%) |
| Valvular disease | 185,998 | (27%) | 75,539 | (26%) | 16,288 | (21%) | 94,171 | (29%) |
| Hypertension | 586,851 | (85%) | 239,018 | (83%) | 67,714 | (86%) | 280,119 | (86%) |
| Diabetes mellitus | 283,286 | (41%) | 110,322 | (38%) | 32,932 | (42%) | 140,032 | (43%) |
| Myocardial infarction | 78,142 | (11%) | 15,643 | (5.4%) | 5,188 | (6.6%) | 57,311 | (18%) |
| Atrial fibrillation | 248,480 | (36%) | 89,203 | (31%) | 24,951 | (32%) | 134,326 | (41%) |
| Anemia | 231,996 | (34%) | 72,597 | (25%) | 24,596 | (31%) | 134,803 | (42%) |
| Cardiac dysrhythmias | 258,822 | (38%) | 101,533 | (35%) | 27,597 | (35%) | 129,692 | (40%) |
| Conduction disorder | 126,527 | (18%) | 45,869 | (16%) | 14,376 | (18%) | 66,282 | (20%) |
| Chronic kidney disease | 175,511 | (25%) | 52,440 | (18%) | 17,959 | (23%) | 105,112 | (32%) |
| Acute kidney disease | 148,036 | (21%) | 29,901 | (10%) | 11,780 | (15%) | 106,355 | (33%) |
| COPD | 91,969 | (13%) | 24,426 | (8.5%) | 10,139 | (13%) | 57,404 | (18%) |
| Pneumonia | 172,068 | (25%) | 41,947 | (14%) | 17,380 | (22%) | 112,741 | (35%) |
| Other fluid and electrolyte disorders | 87,051 | (13%) | 18,340 | (6.4%) | 7,256 | (9.3%) | 61,455 | (19%) |
| Coronary atherosclerosis or other heart disease | 379,214 | (55%) | 152,269 | (53%) | 40,890 | (52%) | 186,055 | (57%) |
Age was recorded on July 1 of a given year
Figure 1. Crude incidence rates for heart failure by health care setting, a random 20% sample of Medicare fee-for-service beneficiaries with parts A and B for ≥2 years (2008–2014).
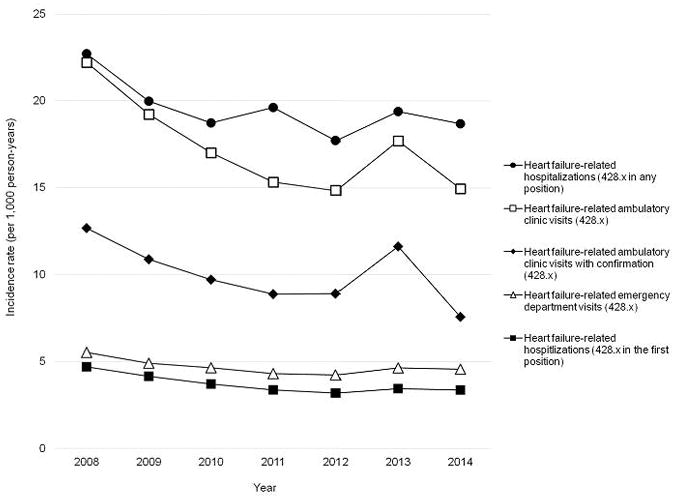
Abbreviations: International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)
Ambulatory clinic visits included visits to primary care physicians and cardiologists
Ambulatory clinic visits with confirmation are a subset of all heart failure-related ambulatory clinic visits; only those with a second heart failure-related visit in the ambulatory clinic, emergency department, or hospital within 365 days of the incident ambulatory clinic visits are included
Emergency department visits included visits to the emergency department that did not end in a hospital admission (routine discharge) and observation stays
Hospitalizations included emergency department visits with a subsequent admission to the hospital
Primary hospitalizations are a subset of all heart failure-related hospitalizations with an ICD-9-CM code of 428.x in the first position of the hospital billing record
Heart failure-related claims were identified using heart failure-specific ICD-9-CM codes 428.x in any position in the billing record
Incidence heart failure was defined as the first heart failure claim observed after the first 2 years of fee-for-service enrollment free of a heart failure claim
Age was recorded on July 1 of a given year
Incidence of HF in ambulatory clinics decreased from 22.2 per 1,000 person years (95% CI: 22.0, 22.4) in 2008 to 15.0 per 1,000 person years (95% CI: 14.8, 15.1) in 2014, with a spike in 2013 (IR=17.7, 95% CI: 17.5, 17.9, Figure 1). Incidence of HF-related ambulatory clinic visits was incrementally higher among older age groups (Figure 2, Supplemental Table 3). Trends in the incidence of HF from 2008 to 2014 did not differ by age group. Compared to white beneficiaries, Asian, Native American, and black beneficiaries had consistently higher rates of incident HF, while Hispanic beneficiaries experienced the lowest rates of HF incidence (Figure 2, Supplemental Table 3). Among all race/ethnic groups, incidence of HF-related ambulatory clinic visits declined from 2008 to 2012. Similar to the overall trend, incidence increased in 2013 among black, Native American, and white beneficiaries. Incidence continued to decrease among Hispanic and Asian beneficiaries.
Figure 2. Crude incidence rates for heart failure related ambulatory clinic and emergency department visits (ICD-9-CM code 42.8.x) by age and race, a random 20% sample of Medicare fee-for-service beneficiaries with parts A and B for ≥2 years (2008–2014).
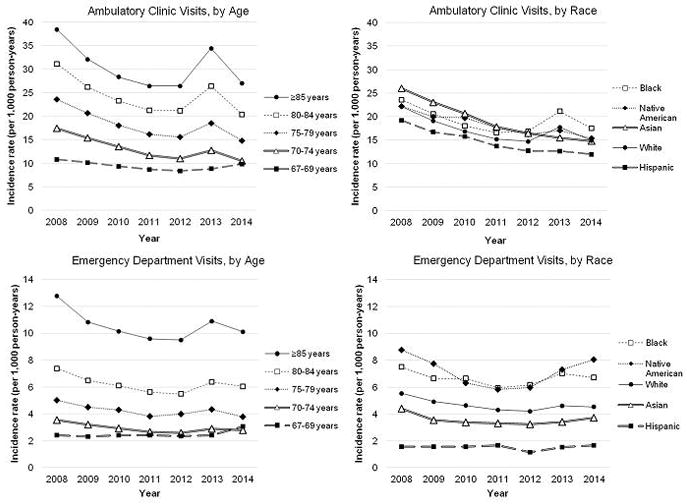
Abbreviations: International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)
Ambulatory clinic visits included visits to primary care physicians and cardiologists
Emergency department visits included visits to the emergency department that did not end in a hospital admission (routine discharge) and observation stays
Heart failure-related claims were identified using heart failure-specific ICD-9-CM codes 428.x in any position in the billing record
Incidence heart failure was defined as the first heart failure claim observed after the first 2 years of fee-for-service enrollment free of a heart failure claim
Age was recorded on July 1 of a given year
Of the 283,451 beneficiaries who presented with incident HF in ambulatory clinics, 164,625 (58%) had a subsequent HF-related visit to a clinic, ED, or hospital within 365 days of the incident visit (outpatient HF with confirmation). The trend in incident ambulatory HF-related visit with confirmation remained virtually unchanged compared to all incident ambulatory clinic visits overall and by age and race/ethnic groups (Figure 1, Supplemental Figure 1, Supplemental Table 4).
Incidence of HF-related ED visits not resulting in a hospital admission decreased marginally from 2008 (IR=5.5 per 1,000 person years, 95% CI: 5.4, 5.6) to 2012 (IR=4.2 per 1,000 person years, 95% CI: 4.1, 4.3, Figure 1) and remained stable through 2014. The incidence was higher among older age groups and was stable over the study period for beneficiaries 67–69 years, 70–74 years, and 75–79 years (Figure 2, Supplemental Table 5). The incidence of HF-related ED visits of those 80 years and older decreased from 2008 to 2012 with an increase in 2013 followed by a decrease in 2014. Incidence rates for HF-related ED visits among Native American and black beneficiaries were consistently higher compared to white beneficiaries (Figure 2, Supplemental Table 5). Hispanic and Asian beneficiaries had the lowest incidence rates of ED HF during the study period. Among Native American and black beneficiaries, incidence of HF-related ED visits decreased from 2008 to 2011 with a subsequent increase in incidence through 2014. Incidence was stable among Asian and Hispanic beneficiaries and decreased nominally for white beneficiaries during the entire study period.
Incidence of hospitalized HF (ICD-9-CM code 428.x in any position) decreased from 2008 (IR=22.7 per 1,000 person years, 95% CI: 22.5, 22.9) to 2010 (IR=18.7 per 1,000 person years, 95% CI: 18.5, 18.9, Figure 1). Following the decline, the trend for incident HF hospitalizations was unstable from 2011 to 2014. Incidence of hospitalized HF was higher among older age groups (Figure 3, Supplemental Table 6). Incidence of hospitalized HF and associated trends over time differed by race/ethnicity (Figure 3, Supplemental Table 6). Black and Native American beneficiaries had the highest, and Hispanic beneficiaries had the lowest incidence of hospitalized HF over the study period compared to white and Asian beneficiaries, who had similar incidence rates. Incidence of hospitalized HF declined over the study period among black and Asian beneficiaries, remained relatively stable for Native American and white beneficiaries, and increased among Hispanic beneficiaries.
Figure 3. Crude incidence rates for heart failure related hospitalizations and primary hospitalizations (ICD-9-CM code 428.x) by age and race, a random 20% sample of Medicare fee-for-service beneficiaries with parts A and B for ≥2 years (2008–2014).
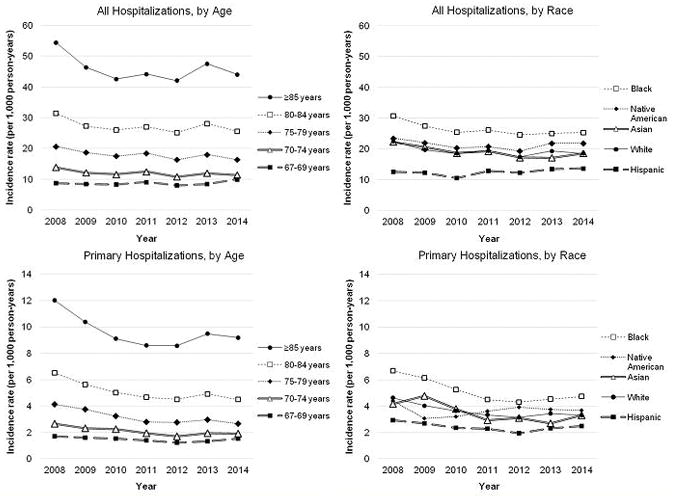
Abbreviations: International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)
Hospitalizations included emergency department visits with a subsequent admission to the hospital
Primary hospitalizations are a subset of all heart failure-related hospitalizations with an ICD-9-CM code of 428.x in the first position of the hospital billing record
Heart failure-related claims were identified using heart failure-specific ICD-9-CM codes 428.x in any position or the first position in the billing record
Incidence heart failure was defined as the first heart failure claim observed after the first 2 years of fee-for-service enrollment free of a heart failure claim
Age was recorded on July 1 of a given year
Of the 321,117 incident HF hospitalizations, 60,492 (19%) carried ICD-9-CM diagnostic code in the primary position. The incidence of HF hospitalizations with a primary diagnostic code decreased from 2008 (IR=4.7 per 1,000 person years, 95% CI: 4.6, 4.8) to 2014 (IR=3.4 per 1,000 person years, 95% CI: 3.3, 3.4). The incidence was higher among older age groups (Figure 3, Supplemental Table 7). For beneficiaries ≥85 years, an initial decline in incidence was followed by an increase in 2012 to 2013 and leveled in 2014. The incidence of HF hospitalizations with a primary diagnostic code among beneficiaries 67–69 and 70–74 years was stable during the study period. Black beneficiaries had the highest, and Hispanic beneficiaries had the lowest incidence of HF hospitalizations with a primary diagnostic code over the study period (Figure 3, Supplemental Table 7). The incidence among Native American and Asian beneficiaries did not differ from that of white beneficiaries. From 2008 to 2012, incidence of hospitalized HF decreased among black and Hispanic beneficiaries, followed by an increase from 2012 to 2014 for both groups.
Discussion
Complementing previous reports on the incidence and temporal trends of hospitalized HF 11–14, we present new information on the incidence of HF in ambulatory clinics, EDs, and hospitals from 2008 to 2014 in a sample of US Medicare beneficiaries. We observed over half of all new HF visits among CMS Medicare beneficiaries occurred in a non-hospitalized setting during the study period.
HF first recognized as an outpatient encounter has been largely omitted from the characterization of incidence of this condition and its temporal trends 3, 11, 14–16. Recent studies suggest a significant proportion of initial diagnoses of HF present in outpatient settings, including the ambulatory clinic and ED 5, 6. HF incidence among CMS Medicare beneficiaries were similar to published incidence rates from Ontario, Canada, where almost half of incident HF visits during the years 1997–2007 occurred in the outpatient setting 5, 6. By contrast, a recent Danish study found no differences in estimated IRs for their temporal trends when outpatient diagnoses were included with hospitalized HF 17.
The incidence of HF among all CMS Medicare beneficiaries decreased from 2008 to 2014, regardless of health care setting, with more substantial declines among older beneficiaries. Our results substantiate studies that reported a decrease in the incidence of hospitalized HF in recent years 1, 5, 6, 12, 13, 18, 19. We postulated that the observed decreases in hospitalized HF would be accompanied by an increase in incident HF in ambulatory care clinics and/or in the ED without a subsequent hospital admission. To the contrary, the incidence of ambulatory clinic and ED visits also decreased from 2008 to 2014, suggesting that ambulatory clinics are not substituting for hospitalized HF care. While 92% of hospitalizations with a primary ICD-9-CM 428.x HF code were validated as acute, decompensated HF by a panel of expert reviewers 20, 21, little is known about the validity of HF codes in the ambulatory setting. When we required confirmation of the initial visit with a subsequent HF-related visit, the proportion of beneficiaries with an ambulatory clinic HF diagnosis decreased from 40% to 24%. Lack of a follow-up visit may be unusual for a patient newly diagnosed with HF. Yet, an initial diagnosis in an ambulatory clinic may be capturing individuals much earlier in their disease progression. Moreover, ambulatory clinicians may not code HF during follow-up visits, which may address common comorbidities such as hypertension or obesity or other acute medical problems.
Increasingly greater access to diagnostic tests in ambulatory care clinics, primarily echocardiograms and biomarkers that improve diagnostic accuracy and reduce rule-out diagnoses provide a potential explanation for the modest decrease in the incidence of HF in ambulatory care from 2008 to 2014. Research that considers temporal trends of various cardiorespiratory syndromes including HF and lung diseases would provide additional information. Also to be considered are the temporal trends in precursor conditions and risk factors of HF. Favorable trends in the detection and control of high blood pressure 22, paired with reductions in cardiovascular diseases antecedent to HF 22 may have contributed to the observed decrease in the incidence of HF. In contrast, other risk factors for HF such as diabetes, obesity, and physical inactivity have worsened over time 22.
The transient increase in the incidence of HF in ambulatory care settings observed in 2013 is noteworthy, possibly explained by the implementation of various CMS policies, such as the CMS Hospital Readmissions Reduction Program which were finalized in 2012 and 2013 (cms.gov). Also in 2013, CMS implemented reimbursements for telemonitoring of weight in the management of HF in the ambulatory clinic setting. While one or more of these policy changes, possibly paired with higher ambulatory care reimbursements, may have translated into a temporary increase in the number of HF-related visits, this administrative claims-based study was unable to determine the effect of such policies.
Similar to a recent study 11, we observed that black and Native American beneficiaries had the highest incidence of hospitalized HF, whereas Hispanic beneficiaries had the lowest incidence of hospitalized HF. The observed incidence of HF among Hispanic beneficiaries, which was the lowest in comparison with all other race/ethnic groups, regardless of healthcare setting is in contrast to other published studies including reports from the Multi-Ethnic Study of Atherosclerosis (MESA) 23, 24. Our results apply to insured, Medicare beneficiaries whereas MESA participants were younger and without requirements for health insurance. Observed relative differences between black/Native American and white beneficiaries did not narrow over the study period. Our data also show incidence of HF-related ED visits may also be increasing among Native American and black beneficiaries, starting in 2011. The observed higher rates of ED and hospitalized HF among black and Native Americans suggest that these groups may increasingly seek medical care in non-ambulatory settings. Significant disparities are known to exist in health care based on race/ethnicity, 25 and poverty rates among black and Native Americans are more than twice that of whites 26. Further, many Native Americans in the US reside in rural areas with limited access to primary care. Because of this limited access to care, beneficiaries may wait until a condition is more serious and seek care in an emergency or inpatient setting.
Replication of our results in other populations is warranted, such as in an all-payer cohort. Because our study sample only included Medicare beneficiaries enrolled in fee-for-service Parts A, B, and D, we were not able to consider HF encounters among individuals enrolled in Medicare Advantage, or in Medicare fee-for-service Parts A and B only. It has been reported that few differences exist between Medicare beneficiaries enrolled in fee-for-service parts A, B, and D compared to those not enrolled in part D and those enrolled in Medicare Advantage 27. However, part D enrollees have, on average, lower incomes than non-part D enrollees (ResDAC.com) and Medicare Advantage beneficiaries are less likely to reside in urban areas and are 30% less likely to use emergency room services 27.
In conclusion, we observed that half of all new cases of HF among Medicare beneficiaries first presented in the ambulatory clinic and ED settings. Incidence of non-hospitalized, as well as hospitalized, HF among CMS Medicare beneficiaries decreased during the years 2008–2014 across race/ethnic and age groups. Future research on HF incidence and temporal trends in the burden of HF should consider encounters in the ambulatory setting.
Supplementary Material
Acknowledgments
Sources of Funding
R. Camplain was supported by the National Heart, Lung, and Blood Institute GRS Diversity Supplement (HHSN268201100007C), Chapel Hill, NC.
The database infrastructure used for this project was funded by the Pharmacoepidemiology Gillings Innovation Lab (PEGIL) for the Population-Based Evaluation of Drug Benefits and Harms in Older US Adults (GIL 200811.0010), the Center for Pharmacoepidemiology, Department of Epidemiology, UNC Gillings School of Global Public Health; the CER Strategic Initiative of UNC’s Clinical & Translational Science Award (UL1TR001111); the Cecil G. Sheps Center for Health Services Research, UNC; and the UNC School of Medicine.
The authors would like to acknowledge Til Stürmer for his help in accessing the data and Virginia Pate for programming assistance.
Footnotes
Disclosures, Declaration of Interest
Dr. Layton is a current employee of RTI International, an independent, nonprofit research organization that does work for government agencies and pharmaceutical companies. Dr. Layton was formerly an employee of the University of North Carolina where he received unrestricted salary support from the Center for Pharmacoepidemiology in the Department of Epidemiology; current member companies include GSK, Merck, and UCB.
All other authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, Jacobsen SJ. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004;292:344–350. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 2.Desai AS, Stevenson LW. Rehospitalization for heart failure: predict or prevent? Circulation. 2012;126:501–506. doi: 10.1161/CIRCULATIONAHA.112.125435. [DOI] [PubMed] [Google Scholar]
- 3.Howlett JG. Acute heart failure: lessons learned so far. Can J Cardiol. 2011;27:284–95. doi: 10.1016/j.cjca.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Collins SP, Pang PS, Fonarow GC, Yancy CW, Bonow RO, Gheorghiade M. Is hospital admission for heart failure really necessary?: the role of the emergency department and observation unit in preventing hospitalization and rehospitalization. J Am Coll Cardiol. 2013;61:121–126. doi: 10.1016/j.jacc.2012.08.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ezekowitz JA, Kaul P, Bakal JA, Quan H, McAlister FA. Trends in heart failure care: has the incident diagnosis of heart failure shifted from the hospital to the emergency department and outpatient clinics? Eur J Heart Fail. 2011;13:142–147. doi: 10.1093/eurjhf/hfq185. [DOI] [PubMed] [Google Scholar]
- 6.Yeung DF, Boom NK, Guo H, Lee DS, Schultz SE, Tu JV. Trends in the incidence and outcomes of heart failure in Ontario, Canada: 1997 to 2007. CMAJ. 2012;184:E765–73. doi: 10.1503/cmaj.111958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blecker S, Paul M, Taksler G, Ogedegbe G, Katz S. Heart failure-associated hospitalizations in the United States. J Am Coll Cardiol. 2013;61:1259–1267. doi: 10.1016/j.jacc.2012.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gerber Y, Weston SA, Redfield MM, Chamberlain AM, Manemann SM, Jiang R, Killian JM, Roger VL. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern Med. 2015;175:996–1004. doi: 10.1001/jamainternmed.2015.0924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Camplain R, Kucharska-Newton A, Cuthbertson CC, Wright JD, Alonso A, Heiss G. Misclassification of incident hospitalized and outpatient heart failure in administrative claims data: the Atherosclerosis Risk in Communities (ARIC) study. Pharmacoepidemiol Drug Saf. 2017 doi: 10.1002/pds.4162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saczynski JS, Andrade SE, Harrold LR, Tjia J, Cutrona SL, Dodd KS, Goldberg RJ, Gurwitz JH. A systematic review of validated methods for identifying heart failure using administrative data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):129–140. doi: 10.1002/pds.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ziaeian B, Kominski GF, Ong MK, Mays VM, Brook RH, Fonarow GC. National Differences in Trends for Heart Failure Hospitalizations by Sex and Race/Ethnicity. Circ Cardiovasc Qual Outcomes. 2017:10. doi: 10.1161/CIRCOUTCOMES.116.003552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Curtis LH, Whellan DJ, Hammill BG, Hernandez AF, Anstrom KJ, Shea AM, Schulman KA. Incidence and prevalence of heart failure in elderly persons, 1994–2003. Arch Intern Med. 2008;168:418–424. doi: 10.1001/archinternmed.2007.80. [DOI] [PubMed] [Google Scholar]
- 13.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. JAMA. 2011;306:1669–1678. doi: 10.1001/jama.2011.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agarwal SK, Wruck L, Quibrera M, Matsushita K, Loehr LR, Chang PP, Rosamond WD, Wright J, Heiss G, Coresh J. Temporal Trends in Hospitalization for Acute Decompensated Heart Failure in the United States, 1998–2011. Am J Epidemiol. 2016;183:462–470. doi: 10.1093/aje/kwv455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blecker S, Bhatia RS, You JJ, Lee DS, Alter DA, Wang JT, Wong HJ, Tu JV. Temporal trends in the utilization of echocardiography in Ontario, 2001 to 2009. JACC Cardiovasc Imaging. 2013;6:515–522. doi: 10.1016/j.jcmg.2012.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collins S, Storrow AB, Albert NM, Butler J, Ezekowitz J, Felker GM, Fermann GJ, Fonarow GC, Givertz MM, Hiestand B, Hollander JE, Lanfear DE, Levy PD, Pang PS, Peacock WF, Sawyer DB, Teerlink JR, Lenihan DJ Group SHAHFW. Early management of patients with acute heart failure: state of the art and future directions. A consensus document from the society for academic emergency medicine/heart failure society of America acute heart failure working group. J Card Fail. 2015;21:27–43. doi: 10.1016/j.cardfail.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christiansen MN, Kober L, Weeke P, Vasan RS, Jeppesen JL, Smith JG, Gislason GH, Torp-Pedersen C, Andersson C. Age-Specific Trends in Incidence, Mortality, and Comorbidities of Heart Failure in Denmark, 1995 to 2012. Circulation. 2017;135:1214–1223. doi: 10.1161/CIRCULATIONAHA.116.025941. [DOI] [PubMed] [Google Scholar]
- 18.Gabet A, Juilliere Y, Lamarche-Vadel A, Vernay M, Olie V. National trends in rate of patients hospitalized for heart failure and heart failure mortality in France, 2000–2012. Eur J Heart Fail. 2015;17:583–590. doi: 10.1002/ejhf.284. [DOI] [PubMed] [Google Scholar]
- 19.Sugrue A, Smyth Y, Hennessy S, Crowley J. Temporal Trends in Hospitalisations for Heart Failure. Ir Med J. 2015;108:207–209. [PubMed] [Google Scholar]
- 20.Kucharska-Newton AM, Heiss G, Ni H, Stearns SC, Puccinelli-Ortega N, Wruck LM, Chambless L. Identification of Heart Failure Events in Medicare Claims: The Atherosclerosis Risk in Communities (ARIC) Study. J Card Fail. 2016;22:48–55. doi: 10.1016/j.cardfail.2015.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosamond WD, Chang PP, Baggett C, Johnson A, Bertoni AG, Shahar E, Deswal A, Heiss G, Chambless LE. Classification of heart failure in the atherosclerosis risk in communities (ARIC) study: a comparison of diagnostic criteria. Circ Heart Fail. 2012;5:152–159. doi: 10.1161/CIRCHEARTFAILURE.111.963199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres J, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB. Heart Disease and Stroke Statistics-2015 Update: A Report From the American Heart Association. Circulation. 2014 doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 23.Silverman MG, Patel B, Blankstein R, Lima JA, Blumenthal RS, Nasir K, Blaha MJ. Impact of race, ethnicity, and multimodality biomarkers on the incidence of new-onset heart failure with preserved ejection fraction (from the Multi-Ethnic Study of Atherosclerosis) Am J Cardiol. 2016;117:1474–1481. doi: 10.1016/j.amjcard.2016.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bansal N, Katz R, Robinson-Cohen C, Odden MC, Dalrymple L, Shlipak MG, Sarnak MJ, Siscovick DS, Zelnick L, Psaty BM. Absolute rates of heart failure, coronary heart disease, and stroke in chronic kidney disease: an analysis of 3 community-based cohort studies. JAMA cardiol. 2017;2:314–318. doi: 10.1001/jamacardio.2016.4652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blanchard JC, Haywood YC, Scott C. Racial and ethnic disparities in health: an emergency medicine perspective. Acad Emerg Med. 2003;10:1289–1293. doi: 10.1111/j.1553-2712.2003.tb00615.x. [DOI] [PubMed] [Google Scholar]
- 26.Williams SM. Poverty in the US: trends, issues, and measurements. Hauppauge, NY: Nova Science Publishers; 2011. [Google Scholar]
- 27.Landon BE, Zaslavsky AM, Saunders RC, Pawlson LG, Newhouse JP, Ayanian JZ. Analysis Of Medicare Advantage HMOs compared with traditional Medicare shows lower use of many services during 2003–09. Health Aff. 2012;31:2609–2617. doi: 10.1377/hlthaff.2012.0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


