Introduction
A partial molar pregnancy occurs when an egg receives two sets of chromosomes from the father. Because two sperms have fertilized the egg, there are now 69 chromosomes instead of the normal 46. Very rarely, a twin pregnancy is formed wherein one is a partial mole and other a normal fetus [1]. We present here a case of partial molar pregnancy with normal fetus, with complete placenta previa.
Case History
A 24-year-old second gravida presented to the outpatient department with pregnancy test positive. Her first pregnancy was a missed abortion which was terminated medically. Following this, she was given pre-conceptional counseling and folic acid was started.
Her basic antenatal blood test and scans (dating and nuchal translucency) were un-remarkable. Her anomaly scan revealed normal-appearing fetus with molar placenta covering the internal os completely. Other biometric parameters were normal. There was no soft tissue or bony markers.
Patient was counseled regarding the complication of molar pregnancy, complete placenta previa and chances of fetal abnormalities. With written informed consent, amniocentesis was performed.
Liquor was brownish in color. Karyotyping was normal. Blood test (beta human chorionic gonadotrophin (HCG), thyroid-stimulating hormone (TSH), complete blood count (CBC), Toxoplasma, rubella, cytomegalovirus, herpes (TORCH)) were performed. Beta HCG was 36,846 µIU/ml. TSH was 1.77 µIU/ml.
Decision was taken to continue the pregnancy. Close monitoring of the patient with beta HCG, TSH, BP and frequent scans was done. She was given steroids at 28 weeks. The growth of fetus continued to be satisfactory. Beta HCG was 74,400 µIU/ml at 33 weeks. Planned delivery was done at 34 weeks. On table, placenta was extending anteriorly. So it was cut through, and a single live preterm female baby of weight 1.84 KG was extracted by breech (transverse lie). Baby was active and cried immediately after birth. Cord was cut, and the placenta was removed in total. There was no abnormal adherence of placenta, and it was assured that uterine cavity is clear. There was no PPH. Placenta contained multiple vesicles of size ranging from 5 mm to a maximum of 2 cm. Placenta was send for histopathologic examination. Postoperative period was uneventful. Patient was discharged on the fourth day. Baby was on minimal oxygen support for the initial three days after which the recovery was fast. Baby was discharged in a week. Beta HCG after 2 weeks came down to 15 µIU/ml.
Histopathology report showed normal-appearing chorionic villi as well as edematous villi with hydropic change and scalloping of villous membranes. Morphology was consistent with partial molar pregnancy.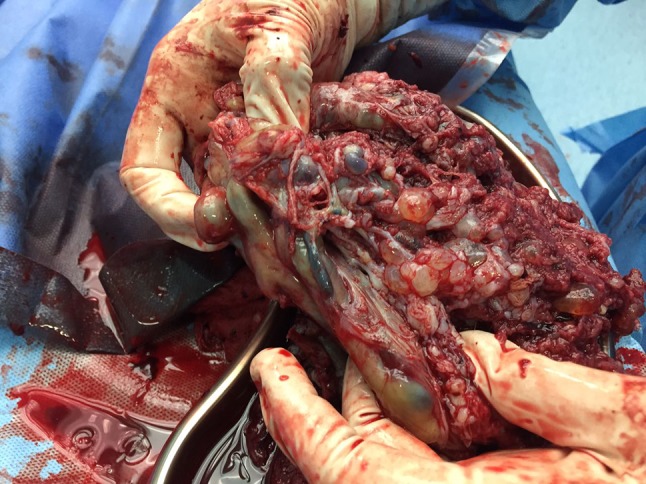
Discussion
A molar pregnancy is the result of a genetic error during the fertilization process that leads to the growth of abnormal tissue within the uterus. Gestational trophoblastic disease consists of a broad spectrum of conditions ranging from an uncomplicated partial hydatidiform molar pregnancy to choriocarcinoma. Complete molar pregnancy is formed when the sperm fertilizes an empty egg and has only placental parts. Partial mole occurs when the egg is fertilized by two sperms and contains both abnormal cells and an embryo. Usually such an embryo is associated with severe birth defects.
Incidence of partial molar pregnancy with coexisting normal fetus is 0.005–0.01% of all the pregnancies [1]. Management of molar pregnancy with normal fetus remains challenging. Molar pregnancy with coexisting fetus carries a significant risk to both the mother and the fetus. Maternal risks include abnormal bleeding, preeclampsia, eclampsia, hyperthyroidism, anemia, persistent gestational trophoblastic disease, preterm delivery and abruption. Fetal complications include abortion, congenital abnormalities, preterm birth, intrauterine growth restriction (IUGR) and intrauterine fetal demise (IUFD) [2].
Serial beta HCG monitoring and frequent scans are the tools for management of such cases.
Smitha Surendran
She is a consultant Obstetrician and Gynecologist working at Rainbow Hospital, Bangalore. She has completed her MS at JJMMC, Davanagere, and MBBS from Calicut Medical College.
Compliance with Ethical Standards
Conflict of interest
Dr. Smitha Surendran, Dr. Teena Thomas, Dr. V. S. Vishnupriya declare that they have no conflict of interest.
Human and Animal Rights Statement
The procedure performed in this case involving human participant was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from the individual participant who was included in the study.
Footnotes
Smitha Surendran is a consultant Obstetrician and Gynecologist working at Rainbow Hospital, Bangalore, India. She has completed her MS at JJMMC, Davanagere, and MBBS from Calicut Medical College; Teena Thomas is a consultant Obstetrician and Gynecologist, working at Rainbow Hospital, Bangalore, India; V. S. Vishnupriya is a consultant Obstetrician and Gynecologist and Infertility specialist working at Rainbow Hospital, Bangalore, India.
References
- 1.Rahamni M, Parviz S. A case report of partial molar pregnancy associated with a normal appearing dizygotic fetus. Asian Pacific J Reprod. 2016;5(2):171–173. doi: 10.1016/j.apjr.2016.01.015. [DOI] [Google Scholar]
- 2.Dhananjaya BS, Nanda S, Gopal N, Tejeswini KK. A term pregnancy with partial molar changes: a case report. Int J Biol Med Res. 2011;2(4):1191–1192. [Google Scholar]


