Abstract
Introduction
Many uncommon obstetric and gynecologic problems associated with pregnancy and the early postpartum period can lead to severe abdominal pain and be life-threatening. The patient will be in urgent need of a quick and accurate decision. The means of management will depend on the ability to differentiate between these problems to achieve an optimal diagnosis.
Materials and methods
30 pregnant females attended a private obstetric ultrasound clinic with clinical picture of acute abdomen with pregnancy. All were subjected to an ultrasound exam, the results were recorded, and the final diagnosis was reached based on the postoperative results.
Results
Patients were classified according to their duration of pregnancy into cases with acute abdomen that occurred during the first trimester, during the second trimester, during the third trimester, and in the early postpartum period.
Conclusion
Ultrasonography is a valuable tool for detecting the etiology and guiding the management in cases of emergency situations faced by the obstetrician and gynecologist during pregnancy and the early postpartum period.
Keywords: Obstetric/gynecological emergencies, Ultrasound, Acute abdomen, Pregnancy
Sommario
Introduzione
Molti rari problemi ostetrici e ginecologici associati alla gravidanza e al primo periodo post-partum possono determinare severo dolore addominale e mettere a rischio la vita. Queste patologie richiedono decisioni rapide e accurate e la loro gestione dipende dalla capacità di riconoscerle.
Materiali e metodi
Lo studio ha incluso ha incluso 30 donne in gravidanza afferenti ad una clinica ostetrica privata con quadro clinico di addome acuto associato alla gravidanza. In tutte le pazienti è stata eseguita una ecografia ostetrica e i risultati dell’esame sono stati confrontati con quelli confrontati con i dati dell'esito postoperatorio.
Risultati
Le pazienti sono state classificate in base al periodo della gravidanza, in particolare come casi di addome acuto avvenuti durante il primo trimestre, il secondo trimestre, il terzo trimestre e nel periodo precoce del post-partum.
Conclusioni
L’ecografia è uno strumento prezioso nel rilevare le patologie e guidare la gestione delle pazienti con dolore addominale severo durante la gravidanza e il periodo precoce del post-partum.
Introduction
Severe abdominal pain in females during gestation can be due to obstetric/gynecologic problems or abnormalities related to the abdominal organs.
The obstetrician needs to differentiate among these conditions. In the absence of vaginal bleeding, the differentiation is hard. Most obstetricians do not have experience with abdominal ultrasound, but many can perform an obstetric ultrasound. Thus, they can look into the pregnancy’s and fetus’ condition but simply cannot identify the other conditions linked to the gynecologic or abdominal organs. So, most obstetricians refer cases of acute abdomen during pregnancy to a radiology clinic or nearby ultrasound clinic. The patient is in urgent need of a quick and accurate decision because the conditions may be life-threatening in many cases. Most radiologists and specialists in the field of ultrasound are experienced in the diagnosis of many abdominal causes of acute abdomen, such as obstructive uropathy due to ureteric stones, calcular cholecystitis, appendicitis, and pancreatitis.
The current study will evaluate other uncommon emergencies related to obstetric or gynecological problems associated with gestation.
Aim of the work
The study proposed to explain and evaluate many uncommon obstetric and gynecologic problems that can be life-threatening to the patient during the pregnancy and early postpartum period and to evaluate how to achieve an optimal diagnosis using ultrasound to make the best management decisions.
Methodology
Thirty pregnant females attended a private obstetric ultrasound clinic with clinical picture of acute abdomen associated with pregnancy from March 2013 to January 2017. All were examined with a SonoAce X 8 ultrasound machine (Medison, Korea) with either or both of a multi-frequency 4–8 MHz convex ultrasound probe and a 2–9 MHz endovaginal probe assisted by color Doppler capability according to the duration of the pregnancy. Patients with acute abdominal pain due to causes not related to obstetric or gynecological problem were excluded from the study. Their ages ranged from 20 to 36 years.
Patients were classified according to their duration of pregnancy into acute abdomen that occurred during the first trimester, acute abdomen that occurred during the second trimester, acute abdomen that occurred during the third trimester, and acute abdomen that occurred during the early post-delivery period.
For cases with clinical picture of acute abdomen that occurred during the first trimester, after she had evacuated her urinary bladder, each patient was examined with a transvaginal probe for the site of the gestational sac, the presence of the fetal node inside, viability, perisac hematoma, and the presence of associated uterine myomas. The adnexal regions were scanned for the presence of cysts or solid masses and Douglas’ pouch for the presence of free turbid fluid collections.
For cases with acute abdomen that occurred during the second and third trimesters, an abdominal ultrasound exam was performed using a convex probe assisted by color and pulsed Doppler capabilities. We evaluated the pregnancy’s state with regard to the fetus’ viability; estimated sonographic age; fetus presentation; amount of amniotic fluid; site and grade of the placenta; umbilical cord flow parameters; presence of uterine fibroids for the site; size, texture, and vascularity; any adnexal masses or cysts; and if there was free fluid in the peritoneal cavity.
For cases in the post-delivery period, the patients were examined with a convex probe assisted by color and pulsed Doppler capabilities for the size of the uterus, the contents of the endometrial cavity, the adnexal regions, the adnexal venous plexus, the ovarian veins, and the peritoneal cavity for the presence of free fluid. As all cases, except two with right ovarian vein thrombosis who received anticoagulant therapy, were subjected to surgical intervention, they were followed for the postoperative results through direct contact with the referred clinicians or with the senior staff of the obstetric department of the Fayoum general hospital, and the final diagnosis was reached based on the surgical results and the results of follow-up.
Results
Eighteen out of 30 cases that attended the ultrasound clinic with clinical picture of acute abdomen during the first trimester of pregnancy had ultrasound exam results that showed the following.
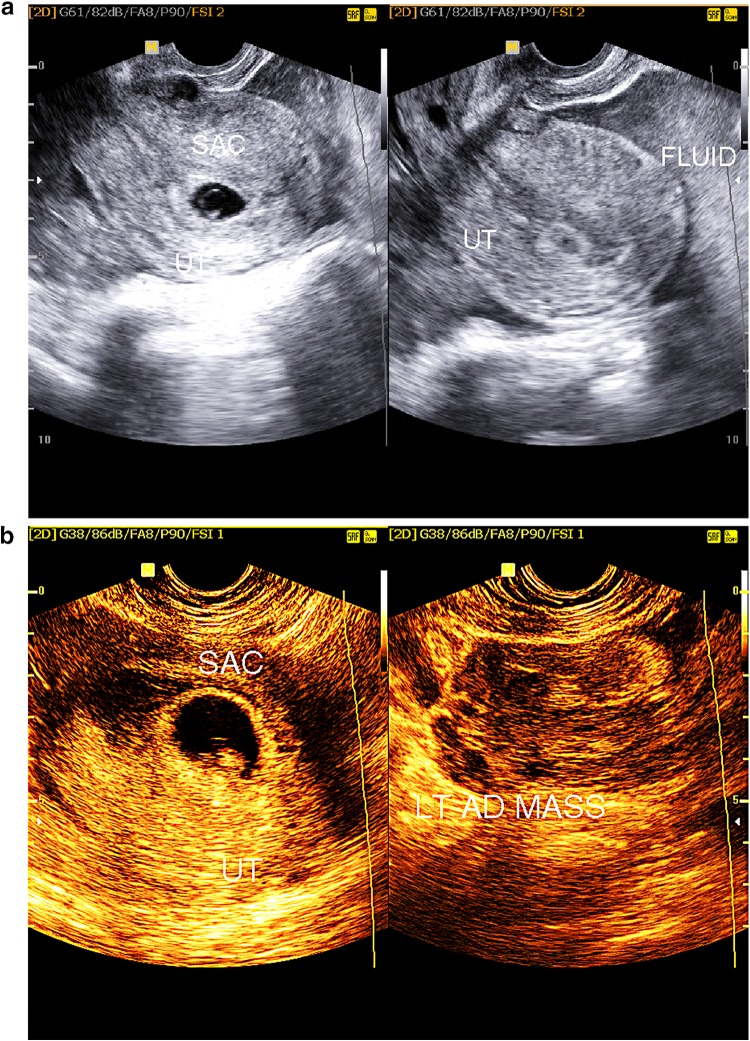
Heterotopic pregnancy (two cases) (Fig. 1a, b)
Fig. 1.
a B-mode transvaginal ultrasound showing intrauterine early pregnancy associated with free turbid peritoneal fluid subsequent to rupture tubal ectopic pregnancy. b Transvaginal ultrasound showing single intrauterine gestational sac associated with heterogeneous left adnexal mass subsequent of disturbed left tubal ectopic pregnancy
One case was diagnosed by the presence of an adnexal soft tissue-like mass of inhomogeneous texture and free turbid fluid in Douglas’ pouch or in the peritoneal cavity, in association with an intrauterine gestational sac. The other case showed an intrauterine small gestational sac associated with moderate free turbid peritoneal fluid in the presence of severe lower abdominal pain.
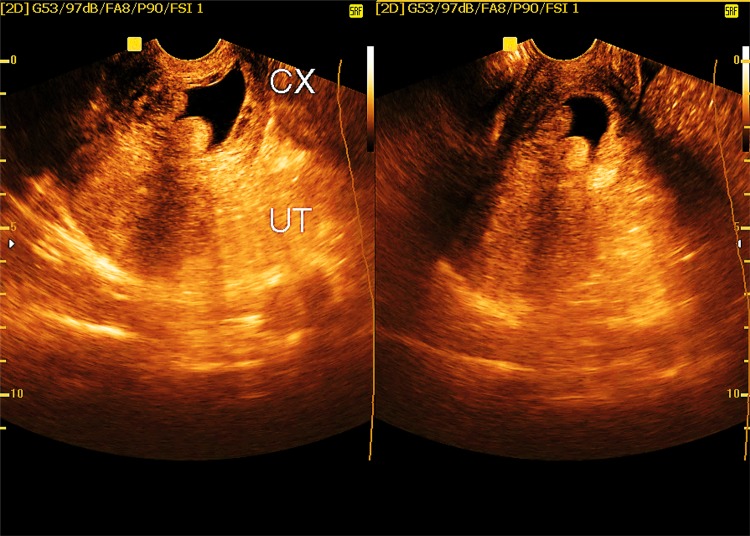
Cervical ectopic pregnancy (one case) (Fig. 2)
Fig. 2.
Transvaginal ultrasound showing irregular gestational sac within the cervical canal (cx) with closed internal os
This case was diagnosed by the presence of a gestational sac that showed a mega yolk sac inside and no fetal node within the cervical canal, with closed internal os and partially opened external os, negative sliding of the sac during vaginal probing, and prominent peri-gestational sac blood flow.
Interstitial ectopic pregnancy (one case)
The patient showed an eccentric situated gestational sac showing a yolk sac inside and a fetal node with a myometrial wall thickness less than 5 mm at its outer aspect.
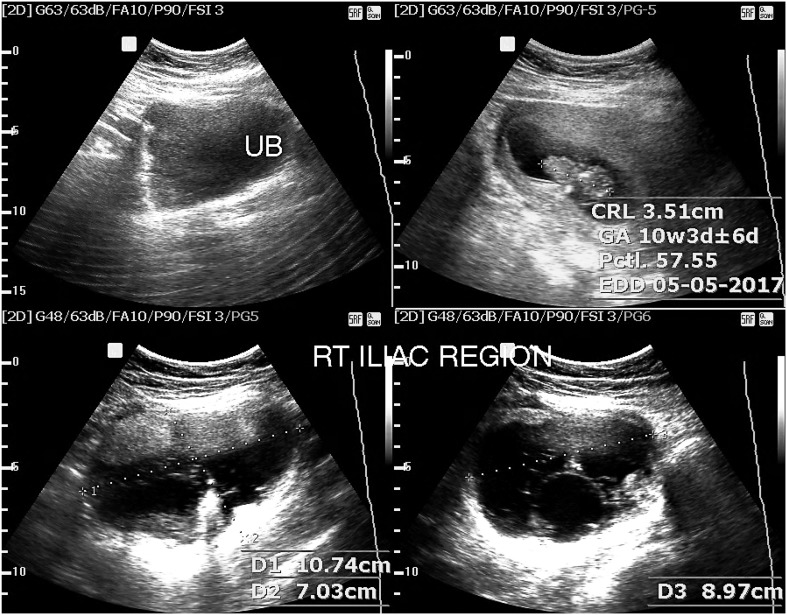
Ectopic gestation at the site of Cesarean section (CS) scar (six cases) (Fig. 3)
Fig. 3.
B-mode ultrasound exam showing ectopic gestational sac at site of uterine CS scar
These patients showed the eccentric location of the sac situated anterior to the uterine cavity within the myometrial wall on the site of the CS scar or the presence of retained parts of conception on the site of the uterine CS scar.
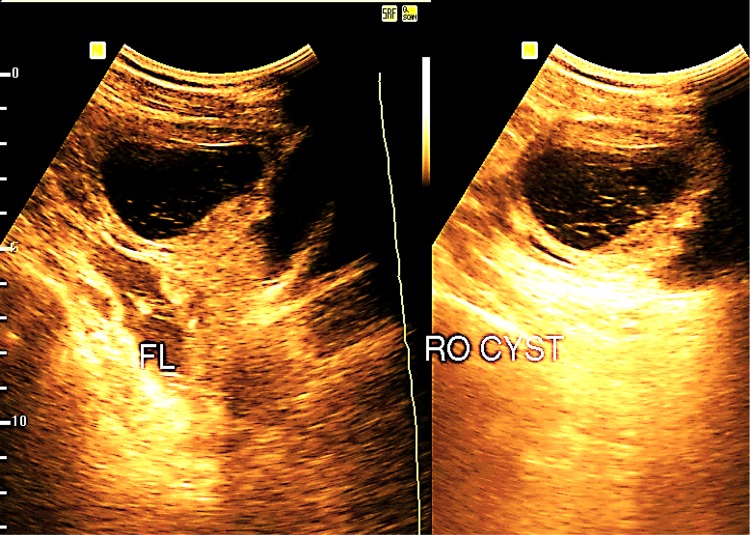
Ruptured ovarian cyst in association with intrauterine pregnancy (three cases) (Fig. 4)
Fig. 4.
B-mode ultrasound exam showing right ovarian cyst with low-level echoes and fine septa associated with mild free turbid pelvic fluid
One case showed an adnexal complex cyst with medium- and low-level echoes inside and the presence of free turbid fluid inside the peritoneal cavity and’ Douglas’ pouch. The second case showed a collapsed cyst with inhomogeneous contents. The third case attended with no cyst that could be determined and the presence of moderate free turbid peritoneal fluid in the second and third cases.
Hemorrhagic ovarian cyst in association with intrauterine pregnancy (three cases) (Fig. 5)
Fig. 5.

Transvaginal ultrasound showing complex ovarian cyst suggesting a hemorrhagic cyst
All showed a complex cyst with inhomogeneous contents showing concave borders and no flow inside, suggesting blood clots and fine septa.
Complicated dermoid cyst in association with pregnancy (two cases) (Fig. 6)
Fig. 6.
B-mode ultrasound image showing single intrauterine pregnancy associated with tender right ovarian complex cyst with moderate echogenic side wall soft tissue-like component and multiple septa suggesting a dermoid cyst
These were diagnosed with the presence of a tender adnexal cyst showing moderately echogenic contents with calcifications inside, thickened walls, and medium-level gravitating echoes. Torsion could be omitted if the walls showed venous and arterial flow signals.
Second trimester causes of acute abdomen associated with pregnancy observed in our study (6 out of 30 cases)
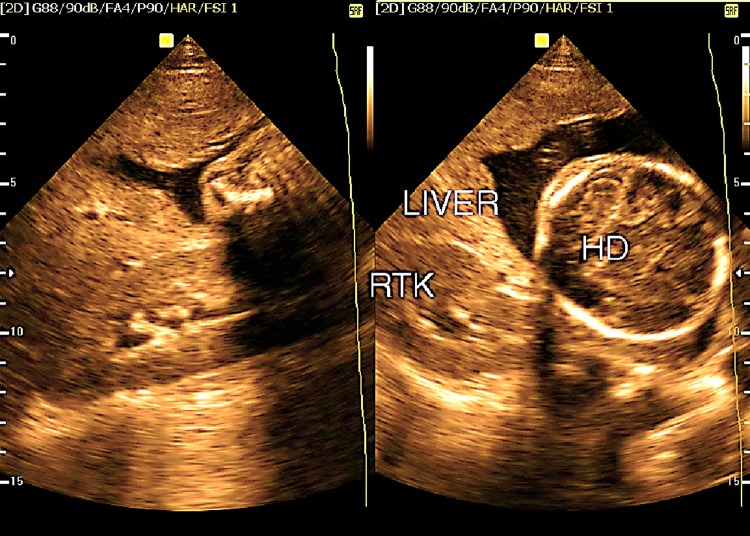
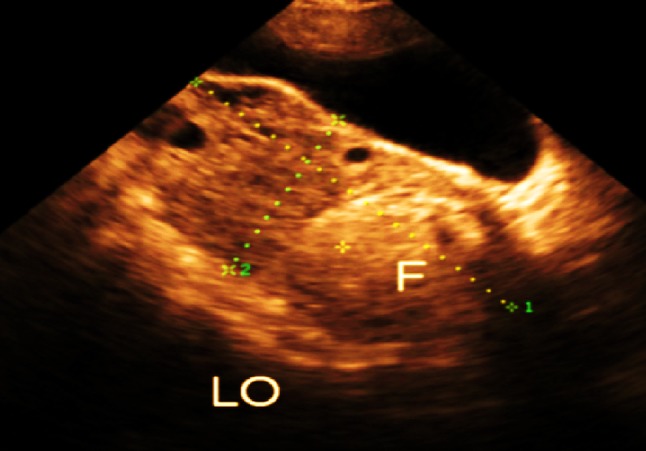
Ruptured ectopic pregnancy in rudimentary horn (two cases) (Fig. 7)
Fig. 7.
B-mode ultrasound image showing floating fetal parts in the abdominal cavity with placenta seen beneath the under surface of the liver suggesting ruptured uterus
One case showed marked free turbid peritoneal fluid with fetal parts seen floating within the amniotic fluid and the placenta seen beneath the lower edge of the liver. The second case showed the non-viable fetus and placenta in the peritoneal cavity with marked free turbid peritoneal fluid, and the uterus in each case was normal-sized with a normal endometrial lining.
Ruptured tubo-ovarian abscess associated with pregnancy (one case)
This was observed in a patient showing an ovoid-shaped soft tissue-like mass lesion with marginal hypervascularity observed in the adnexal region and an echogenic turbid free peritoneal fluid in association with a single living intrauterine pregnancy.
Torsion in pedunculated subserous myoma (one case)
The patient showed a tender subserous fundal uterine mass lesion with an inhomogeneous echo pattern and no visible vascularity inside with color Doppler.
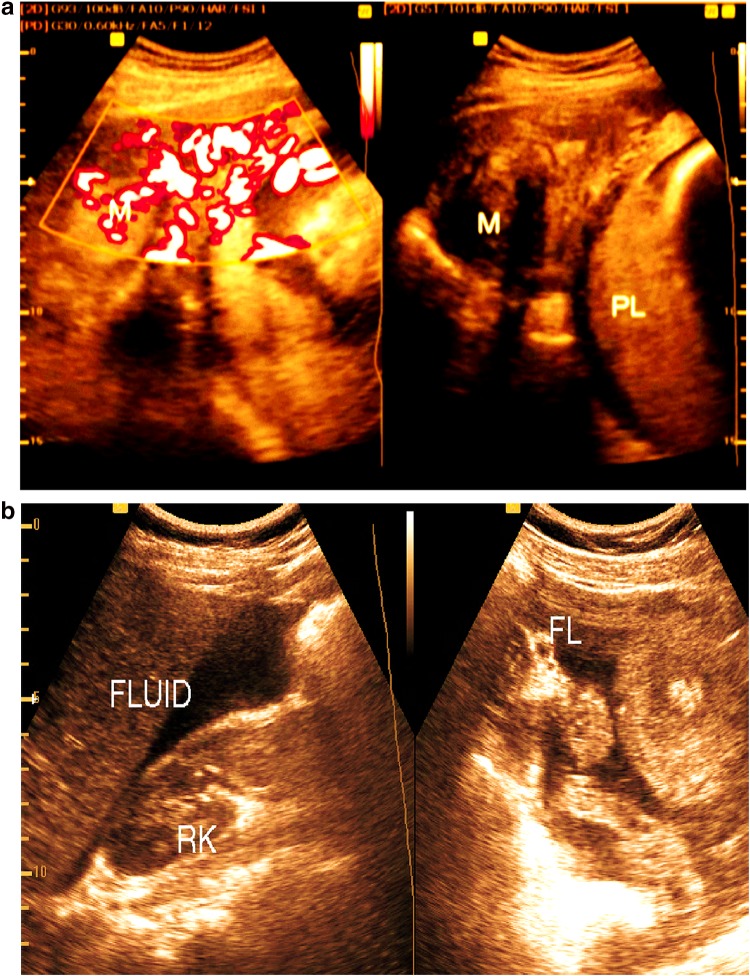
Ovarian torsion with pregnancy (two cases) (Fig. 8)
Fig. 8.
Real-time abdominal ultrasound showing enlarged left ovary with small follicles and echogenic focal lesion inside suggesting ovarian torsion with small ovarian dermoid cyst
In each case, the ovary was markedly enlarged, with multiple small follicles and a small, well-defined echogenic focal lesion inside, suggesting a dermoid cyst in one case. The ovary in each case showed no parenchymal color flow signal inside, with associated mild free turbid peritoneal fluid.
Cases with acute abdomen that occurred during the third trimester (four cases)
Ruptured surface vessels of subserous myoma (one case) (Fig. 9)
Fig. 9.
a Color duplex ultrasound image showing subserous myoma with multiple surface vessels. b The same patient with moderate free turbid peritoneal fluid
The patient attended the ultrasound exam with severe abdominal pain and she was in shock; the result of the exam showed subserous fundal fibroid rich in vascular markings with multiple venous channels around its periphery associated with moderate free turbid peritoneal fluid and a single viable intrauterine pregnancy.
Complete rupture of CS scar associated with third-trimester pregnancy (one case)
The patient was hypotensive with marked pallor, showing severe abdominal pain, with a history of cesarean section, and showed a single viable intrauterine pregnancy with oligohydramnios and marked free turbid peritoneal fluid.
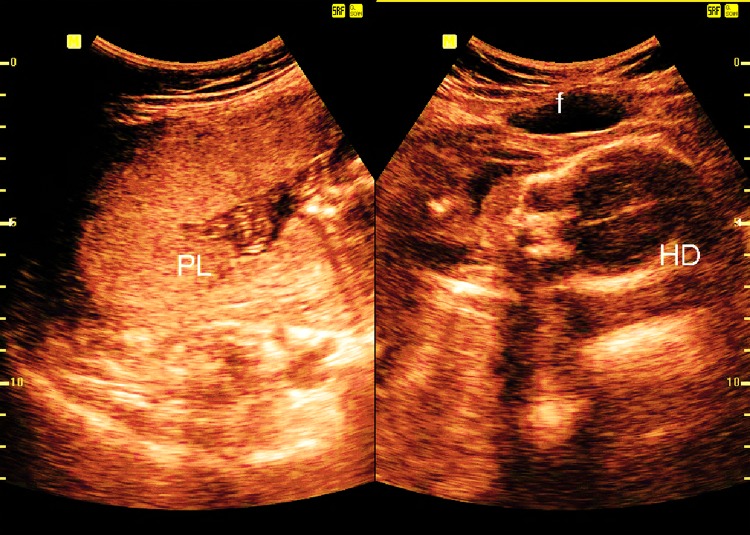
Incomplete rupture of CS scar (one case) (Fig. 10)
Fig. 10.
B-mode ultrasound image of single intrauterine pregnancy showing small encysted fluid collection anterior to the myometrium wall (incomplete uterine rupture)
This was observed during the third trimester of a viable intrauterine single pregnancy; adequate amniotic fluid and small encysted clear-content fluid was seen overlying the lower anterior uterine wall beneath the uterine serosa and the anterior abdominal wall.
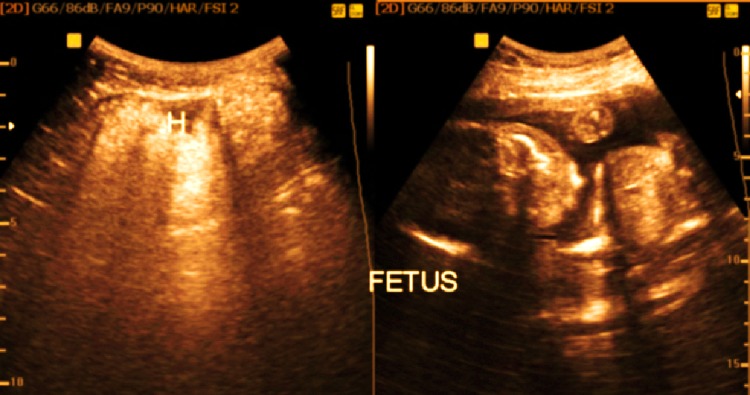
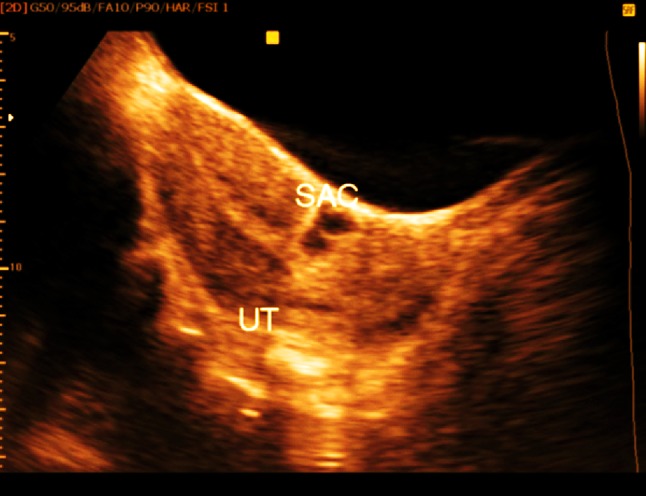
Incarcerated incisional hernia at site of abdominal wall previous CS scar (one case) (Fig. 11)
Fig. 11.
Single intrauterine pregnancy with associated strangulated hernia sac (H) at site of abdominal wall CS scar
The patient attended with severe lower abdominal pain and a palpable swelling; the ultrasound exam showed an incarcerated, irreducible hernia sac showing omentum and intestinal loops inside overlying a defect at the lateral aspect of the abdominal wall CS scar with a viable intrauterine third-trimester pregnancy.
Cases with acute abdomen that occurred in the early post-delivery period (two cases)
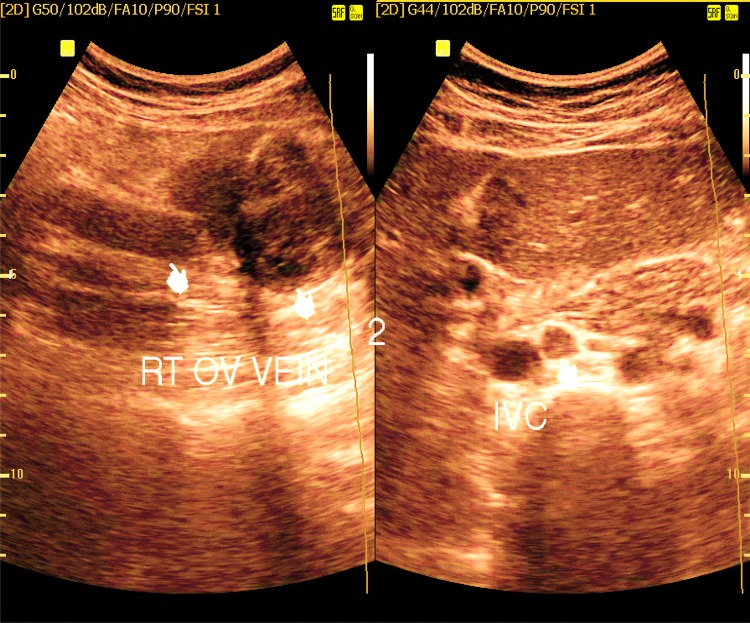
Right ovarian vein thrombosis (two cases) (Fig. 12)
Fig. 12.
Dilated right ovarian vein (indicator) till it reaches the IVC with hypoechoic contents suggesting recent thrombotic occlusion
The patients attended with severe right iliac fossa pain and clinical picture suggesting appendicitis, and on ultrasound exam, the right ovarian veins were detected with diffuse thrombotic occlusion and ectatic dilation showing no color flow signal inside, with the thrombus edge seen protruding into the inferior vena cava in one case. The patients were subjected to conservative management with anticoagulant therapy and the veins recanalized on follow-up.
Discussion
The current study evaluated cases with severe abdominal pain associated with gestation due to uncommon obstetric or gynecologic causes, which can be classified according to the duration of pregnancy into causes occurring during the first trimester, including heterotopic pregnancy, interstitial ectopic pregnancy, ectopic pregnancy at site of CS scar, and cervical ectopic pregnancy; causes occurring during the second trimester, including ruptured ectopic pregnancy in rudimentary horn and torsion of pedunculated subserous myoma; causes occurring during the third trimester, including ruptured CS scar; and causes occurring in the early postpartum period like ovarian vein thrombosis.
The most important ultrasound sign that suggests an emergency situation is the presence of free turbid peritoneal fluid in a patient with acute abdomen in association with pregnancy.
The nature of turbidity can be due to either pus or blood in most cases. Ultrasound differentiation based on the echo characteristics of the fluid is difficult, yet the presence of floating hypoechoic concave border sheet-like structures suggests blood clots. The clinical picture also may aid in the distinction. Simple diagnostic ultrasound-guided aspiration of the fluid can confirm its nature, whether blood or pus.
Pus in the presence of adnexal mass can lead to the diagnosis of ruptured tubo-ovarian abscess, but in the absence of adnexal mass, the possibility of other causes related to the gastrointestinal tract, such as perforated appendicitis and ruptured peri-diverticular abscess, are to be considered.
Bloody contents of the peritoneal fluid in association with first-trimester intrauterine pregnancy can be seen in the presence of inhomogeneous adnexal mass or adnexal thick wall ring structure or viable extra-uterine pregnancy and suggest disturbed heterotopic pregnancy [1] but in the presence of a complex ovarian cyst will lead to the diagnosis of a ruptured ovarian cyst, and if associated with an enlarged ovary with hypertrophied parenchyma showing either a simple cyst or a dermoid cyst inside and demonstrating absent blood flow by color Doppler study within the ovarian parenchyma, will lead to the diagnosis of ovarian torsion [2]. Interstitial ectopic pregnancy, cervical ectopic pregnancy, and CS scar ectopic pregnancy, which are emergency conditions that can be diagnosed during the first trimester, are usually not associated with free turbid peritoneal fluid but are usually associated with acute lower abdominal pain and vaginal bleeding [3, 4].
The commonest complication of subserous myoma with pregnancy that causes abdominal pain is red degeneration; rare complications include torsion in pedunculated subserous myoma, which can be diagnosed when the texture of the myoma becomes heterogeneous in the absence of blood flow signal inside, with marked tenderness on probing [5]. Rupture of the surface vessel of a hypervascular subserous myoma, which could be an artery or surface vein, can occur due to rising intraabdominal pressure during pregnancy. If the bleeding vessel is an artery, the bleeding will be catastrophic, and the blood accumulates rapidly within the abdominal cavity [6]. The differentiation between torsion in a pedunculated myoma and ruptured surface vessels depends on the amount of blood in the abdominal cavity and the vascularity of the myoma.
Complete rupture of the uterus during pregnancy involves all layers of the uterine wall, including the serous covering; leads to severe bleeding from the edges at the site of the rupture and escape of amniotic fluid, fetal parts, and placenta tissue into the abdominal cavity; and is associated with fetal and maternal stress. On the other hand, incomplete rupture does not involve the serous covering of the uterus, and amniotic fluid is seen enclosed within the amniotic membrane overlying the uterine myometrium; it is not associated with fetal or maternal stress [7]. Ruptured ectopic pregnancy in a rudimentary horn usually occurs during the second trimester and has similar ultrasound diagnostic features to the complete rupture of the uterus [8]. The presence of a normal-sized uterus associated with free turbid fluid and non-viable fetus in the abdominal cavity are the key findings for the diagnosis. In the early postpartum period, severe right iliac fossa pain can be due to ovarian vein thrombosis; the condition cannot be differentiated clinically from appendicitis; and, if there is no clinical suspicion, may lead to negative laparotomy. The thrombus in the ovarian vein can propagate to reach the inferior vena cava and may detach to cause a pulmonary embolism, so early diagnosis and adequate management is extremely commended [9].
Conclusion
Ultrasonography is a valuable tool for detecting the etiology and guiding the management in cases of emergency situations faced by the obstetrician and gynecologist during pregnancy and the early postpartum period.
Funding
Not present.
Compliance with ethical standards
Conflict of interest
The author reports that he has no conflict of interest.
Ethical statements
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Informed consent
Informed consent was obtained from all patients for being included in the study.
References
- 1.Govindarajan MJ, Rajan R. Heterotopic pregnancy in natural conception. J Hum Reprod Sci. 2008;1:37–38. doi: 10.4103/0974-1208.39595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown Douglas L, Dudiak Kika M, Laing Faye C. Adnexal masses: US characterization and reporting. Radiology. 2010;254(2):342–354. doi: 10.1148/radiol.09090552. [DOI] [PubMed] [Google Scholar]
- 3.Samal SK, Rathod S. Cervical ectopic pregnancy. J Nat Sci Biol Med. 2015;6:257–260. doi: 10.4103/0976-9668.149221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Youssef AT. Endosonography of benign myometrium cysts and cyst-like lesions. J Ultrasound. 2015;18:213–222. doi: 10.1007/s40477-014-0142-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta S, Manyonda IT. Acute complications of fibroids. Best Pract Res Clin Obstet Gynaecol. 2009;23(5):609–617. doi: 10.1016/j.bpobgyn.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 6.Tajima S, Yonezawa I, Waki M, et al. Massive hemoperitoneum following spontaneous rupture of an arterial aneurysm overlying a uterine myoma. Int J Clin Exp Med. 2015;8:3002–3005. [PMC free article] [PubMed] [Google Scholar]
- 7.Kim YR, Cho DH. Uterine rupture in subsequent third trimester pregnancy diagnosed preoperatively by ultrasound: a case report. OA Case Rep. 2014;22(3):72. [Google Scholar]
- 8.Tufail A, Hashmi HA. Ruptured ectopic pregnancy in rudimentary horn of the uterus. J Coll Phys Surg Pak. 2007;17:105–106. [PubMed] [Google Scholar]
- 9.Harris K, Mehta S, Iskhakov E, et al. Ovarian vein thrombosis in the nonpregnant woman: an overlooked diagnosis. Ther Adv Hematol. 2012;3:325–328. doi: 10.1177/2040620712450887. [DOI] [PMC free article] [PubMed] [Google Scholar]