Abstract
Purpose
To report the case of a 65-year-old metalworker with no known history of ocular trauma, who suffered from intense ocular pain during magnetic resonance imaging (MRI) of the brain, due to a retained intraocular metallic foreign body (IOFB).
Case report
Meticulous ophthalmological examination was inconclusive. An IOFB was confirmed with X-ray scan, whereas its exact localization was enabled by means of ultrasonography and ultrasound biomicroscopy (UBM).
Conclusions
Despite appropriate screening protocols, MRI-related ocular complications might occur in the presence of a hidden metallic IOFB. Clinical detection of ocular foreign bodies can sometimes be challenging. Ultrasonography and UBM are valuable adjuncts for the accurate localization, especially of small or hidden particles.
Keywords: MRI, Intraocular foreign body, Ultrasonography, UBM
SOMMARIO
Scopo dello studio
Presentare il caso clinico di un operaio metallurgico, di 65 anni, con anamnesi negativa per traumi oculari, che durante un esame di Risonanza Magnetica (MRI) del capo ha avvertito intenso dolore oculare a causa di un corpo estraneo ritenuto.
Caso clinico
L’esame oftalmologico di routine è stato inconclusivo. La presenza di un corpo estraneo intraoculare è stata documentata con una radiografia (RX) delle orbite, mentre la sua esatta localizzazione e’ stata resa possibile dall’ ecografia oculare (US) e dalla biomicroscopia ad ultrasuoni (UBM).
Conclusioni
Nonostante protocolli di screening adeguati, complicazioni oculari in corso di MRI possono verificarsi in presenza di un corpo estraneo oculare non noto. L’ esatta localizzazione di un corpo estraneo intraoculare talvolta può essere laboriosa e inconclusiva. US e UBM oculare sono metodiche di ausilio per la localizzazione accurata di corpi estranei, soprattutto di piccole dimensioni.
Introduction
Magnetic resonance imaging (MRI) is contraindicated in cases with a suspected intraocular ferromagnetic foreign body, because the object can easily move in the strong magnetic field, leading to serious and potentially vision-threatening ocular adverse events [1].
To our knowledge, there are only a few case reports of complicated MRI due to retained intraocular foreign body (IOFB) in the literature. Kelly et al. reported first in 1986 the occurrence of sudden unilateral visual loss due to vitreous hemorrhage following brain MRI [2]. In a similar case, a patient complained of sudden eye pain and loss of vision immediately after MRI. Ophthalmological examination showed a small paracentral corneal scar and a 50% hyphaema without vitreous hemorrhage [3]. In both cases Computed Tomography (CT) revealed a retained IOFB. Vote et al. reported in 2001 a rapidly progressing IOFB-related traumatic cataract after MRI [4], whereas in a recent report microhyphaema was caused by dislodgement of an IOFB embedded within the iris [5].
Herein we report a case of a patient with acute ocular pain during MRI, due to retained IOFB. Meticulous ophthalmic examination could not localize any object. This was identified by means of orbital X-rays, whereas the exact localization of it was detected only by conventional ultrasonography and anterior segment ultrasound biomicroscopy (UBM), highlighting the impact of those examinations in the diagnosis and clinical management of such patients.
Case report
A 65-year-old male presented to the imaging department of our hospital for cervical and lumbar spine MRI to investigate his chronic bilateral leg tremor. According to our protocol, the patient filled out an MRI safety questionnaire prior to the examination. A previous ocular trauma was denied.
During the examination the patient complained of acute pain in his left eye. The MRI was immediately terminated and the patient was referred to our clinic for ophthalmological evaluation. The patient insisted on not having any ocular traumas in the past. Nevertheless, his occupation prior to retirement involved working for a construction company as a metalworker.
Visual acuity was 20/20 in both eyes. Intraocular pressure was within normal limits (14 and 13 mmHg in the right eye and left eye, respectively). On slit-lamp examination a cystic conjuctival lesion was identified 4 mm away from the corneoscleral junction (limbus) at the inferonasal area of the left eye, probably corresponding to the IOFB entry site (Fig. 1a). Anterior Segment Optical Coherence Tomography (AS-OCT) confirmed this lesion (Fig. 1b). Apart from this finding, no other ocular pathology was seen; both eyes had no optical media opacities, there was no anterior chamber reaction, the pupils were round, isocoric, reactive to light without posterior synechiae. No relative afferent pupillary defect was detected. Gonioscopy did not reveal any IOFB or synechiae in the angle. Fundoscopy was also unremarkable with no macular pathology. Despite a thorough peripheral fundus examination with scleral depression no sign of previous trauma or IOFB was identified. B-scan ultrasonography did not show any hyper-reflective object or related shadowing. Eventually, orbital radiography confirmed the presence of a metallic IOFB in the lower third of the orbit (Fig. 2). Conventional ultrasonography and UBM provided the precise localization of the foreign body in the inferonasal pars plana (Figs. 3 and 4). On repeat fundoscopy with scleral indentation a slight elevation in the area of the inferonasal pars plana could be seen. An electrophysiological evaluation was also conducted to rule out any retinal toxicity due to the IOFB. Both eyes revealed normal electroretinograms.
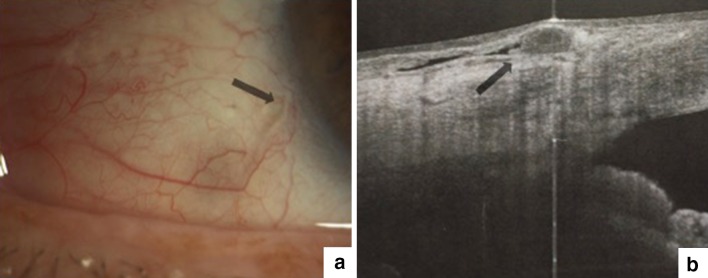
Fig. 1.
a Slit-lamp photo of the left eye. The arrow indicates a cystic conjuctival lesion at the inferonasal area, probably corresponding to foreign body entry site. b Anterior segment optical coherence tomography (AS-OCT) of the inferonasal area depicts the cystic conjuctival lesion (arrow)
Fig. 2.
Radiographs of the skull and orbits. A metallic foreign body is detected in the inferior third of the left orbit (arrows)
Fig. 3.
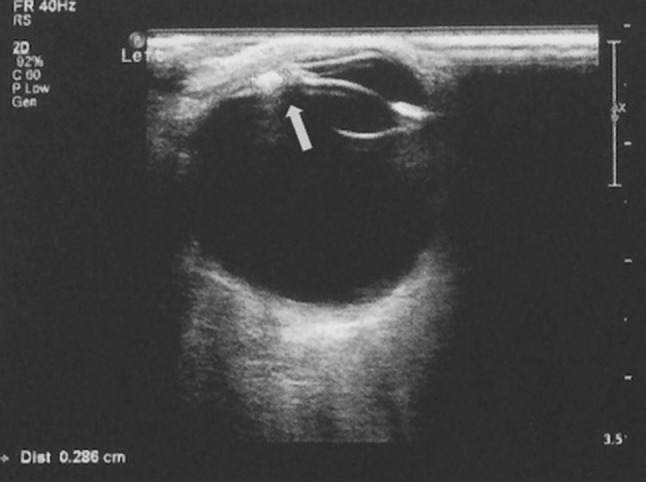
Conventional ultrasonography of the left globe shows a highly reflective foreign body with an approximate diameter of 3 mm in the pars plana with reverberation artifacts seen posteriorly (arrow)
Fig. 4.
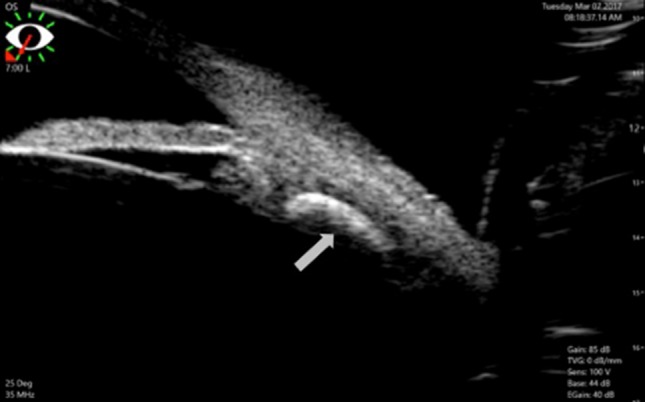
Ultrasound biomicroscopy of the left eye shows a retained foreign body in the pars plana
Taking into consideration the fact that the patient had no symptoms or any ocular complication after MRI, we decided to abstain from any intervention.
Discussion
Retained foreign bodies following ocular injury may lead to serious complications, including inflammation or infection. According to the localization of the foreign body, a projectile injury can result in an intraorbital, a superficial (closed-globe injury) or an intraocular foreign body (IOFB) in case of perforation of the scleral wall [6].
In the herein reported case, the symptom of intense ocular pain during MRI raised the suspicion of a retained ferromagnetic foreign body. The incidence of intraorbital metallic foreign bodies in the general population has been reported at 0.27%, whereas in at-risk patients such as metalworkers or patients with a history of ocular trauma with metal at 2.5% [7]. Metallic objects under magnetic field undergo a translational and a rotational force to align with the magnetic field, thus a ferromagnetic IOFB can easily dislodge and damage adjacent tissue. Other factors contributing to the risk and type of injury are the ferromagnetic property of a metal, sharpness and exact location of the foreign body in the eye [1].
IOFBs located in the anterior segment account for 21–38% of cases and are usually diagnosed by means of slit-lamp examination and gonioscopy. In most cases IOFB are found in the posterior segment, especially in the vitreous. Less common locations are the preretinal, subretinal and suprachoroidal space. Vitreous hemorrhage and traumatic cataract are not uncommon and may prevent visualization of the IOFB [8]. Subconjuctival hemorrhage and poor patient cooperation can additionally render the detection of small foreign bodies challenging. In cases where foreign bodies are suspected imaging methods such as CT, MRI for non- ferromagnetic objects, ultrasonography and UBM should additionally be performed.
CT is the imaging method of choice in the setting of suspected metallic IOFB. Thin-section axial and coronal images at 1 mm can provide excellent visualization of metallic foreign bodies greater than 0.05 mm, as well as potential bone and soft-tissue injuries [9]. Plain X-ray films can also be usefull in the identification especially of a metallic IOFB, but are inferior to CT in precisely localizing it [10]. B-Scan ultrasound is superior to the above-mentioned imaging modalities in the localization of foreign bodies relative to the ocular structures, as well as associated ocular damage [11]. UBM is a high-frequency (50 MHz) and high-resolution imaging technique, offering cross-sectional images of the anterior segment to a depth of 4 mm [12] and particularly usefull in localizing small, nonmetallic objects [13].
In our patient clinical examination results were inconclusive. X-ray films confirmed the presence of an IOFB; however, they could not provide sufficient information regarding the exact localization of it. Conventional ultrasonography and UBM could precisely localize it, confirming their importance as a valuable adjunct in the diagnosis of retained IOFBs. Bryden et al. compared in 1990 the relative detection rates of real time ultrasonography and plain radiographs using a porcine model. With an overall detection rate of 93% ultrasonography was shown to be significantly more sensitive for the imaging of IOFB than X-rays (40%) [10]. Regarding UBM, in a case series of 12 patients with foreign-body- associated ocular trauma of the anterior segment Deramo et al. identified the foreign body with UBM in 75% of the cohort, whereas in 25% of the eyes CT and/or contact B-scan ultrasonography failed to detect it [13]. Guha et al. compared in 2006 UBM with B-scan ultrasound and CT in 18 eyes with anterior segment foreign bodies. The IOFB detection rates were 36.5% by ultrasound, 88.9% by CT scan and 94.4% by UBM, showing the high diagnostic value of this technique [14].
It is interesting that the patient could not recollect any eye injury and also that despite appropriate screening protocols MRI-related ocular complications might occur. A study by Seidenwurm et al. evaluated the cost-effectiveness of clinical versus radiographic screening for an orbital foreign body before MRI and concluded based on the findings that occupational history by itself is not sufficient to mandate radiographic orbital screening [15]. According to the guidelines published in 2013 by an expert panel on MR safety, only patients with suspected ferromagnetic foreign body or patients with a history of eye injury with foreign body, however, for which they sought medical advice are to be screened by either X-ray orbit films or by a radiologist’s review and assessment of previous CT or MRI images, if obtained after the injury [16]. The herein reported case poses the question, whether an orbital X-ray examination or at least an ophthalmologic evaluation of high-risk patients (e.g. metalworkers) before undergoing MRI can nevertheless be justified.
Funding
This study received no funding.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Kim SJ, Kim KA. Safety issues and updates under MR environments. Eur J Radiol. 2017;89:7–13. doi: 10.1016/j.ejrad.2017.01.010. [DOI] [PubMed] [Google Scholar]
- 2.Kelly WM, Paglen PG, Pearson JA, San Diego AG, Soloman MA. Ferromagnetism of intraocular foreign body causes unilateral blindness after MR study. AJNR Am J Neuroradiol. 1986;7:243–245. [PMC free article] [PubMed] [Google Scholar]
- 3.Ta CN, Bowman RW. Hyphema caused by a metallic intraocular foreign body during magnetic resonance imaging. Am J Ophthalmol. 2000;129:533–534. doi: 10.1016/S0002-9394(99)00435-3. [DOI] [PubMed] [Google Scholar]
- 4.Vote BJ, Simpson AJ. X-ray turns a blind eye to ferrous metal. Clin Exp Ophthalmol. 2001;29:262–264. doi: 10.1046/j.1442-9071.2001.00420.x. [DOI] [PubMed] [Google Scholar]
- 5.Lawrence DA, Lipman AT, Gupta SK, Nacey NC. Undetected intraocular metallic foreign body causing hyphema in a patient undergoing MRI: a rare occurrence demonstrating the limitations of pre-MRI safety screening. Magn Reson Imaging. 2015;33:358–361. doi: 10.1016/j.mri.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Ophthalmology. 1996;103:240–243. doi: 10.1016/S0161-6420(96)30710-0. [DOI] [PubMed] [Google Scholar]
- 7.Williamson MR, Espinosa MC, Boutin RD, Orrison WW, Hart BL, Jr, Kelsey CA. Metallic foreign bodies in the orbits of patients undergoing MR imaging: prevalence and value of radiography and CT before MR. Am J Roentgenol. 1994;162:981–983. doi: 10.2214/ajr.162.4.8141030. [DOI] [PubMed] [Google Scholar]
- 8.Parke DW, 3rd, Flynn HW, Jr, Fisher YL. Management of intraocular foreign bodies: a clinical flight plan. Can J Ophthalmol. 2013;48:8–12. doi: 10.1016/j.jcjo.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 9.Chacko JG, Figueroa RE, Johnson MH, Marcus DM, Brooks SE. Detection and localization of steel intraocular foreign bodies using computed tomography. Ophthalmology. 1997;104:319–323. doi: 10.1016/S0161-6420(97)30317-0. [DOI] [PubMed] [Google Scholar]
- 10.Bryden FM, Pyott AA, Bailey M, McGhee CN. Real time ultrasound in the assessment of intraocular foreign bodies. Eye. 1990;4:727–731. doi: 10.1038/eye.1990.103. [DOI] [PubMed] [Google Scholar]
- 11.McNicholas MMJ, Brophy DP, Power WJ, Griffin JF. Ocular trauma: evaluation with US. Radiology. 1995;195:423–427. doi: 10.1148/radiology.195.2.7724761. [DOI] [PubMed] [Google Scholar]
- 12.Pavlin CJ, Harasiewicz K, Sherar MD, Foster FS. Clinical use of ultrasound biomicroscopy. Ophthalmology. 1991;98:287–295. doi: 10.1016/S0161-6420(91)32298-X. [DOI] [PubMed] [Google Scholar]
- 13.Deramo VA, Shah GK, Baumal CR, et al. Ultrasound biomicroscopy as a tool for detecting and localizing occult foreign bodies after ocular trauma. Ophthalmology. 1999;106:301–305. doi: 10.1016/S0161-6420(99)90056-8. [DOI] [PubMed] [Google Scholar]
- 14.Guha S, Bhende M, Baskaran M, Sharma T. Role of ultrasound biomicroscopy in the detection and localization of anterior segment foreign bodies. Ann Acad Med Singapore. 2006;35:536–540. [PubMed] [Google Scholar]
- 15.Seidenwurm DJ, McDonnell CH, 3rd, Raghavan N, Breslau J. Cost utility analysis of radiographic screening for an orbital foreign body before MR imaging. AJNR Am J Neuroradiol. 2000;21:426–433. [PMC free article] [PubMed] [Google Scholar]
- 16.Expert Panel on MR Safet. Kanal E, Barkovich AJ, Bell C, et al. ACR guidance document on MR safe practices: 2013. J Magn Reson Imaging. 2013;37:501–530. doi: 10.1002/jmri.24011. [DOI] [PubMed] [Google Scholar]