Short abstract
Background
Reversible splenial lesion syndrome is a distinct entity radiologically characterized by a reversible lesion in the splenium of the corpus callosum. According to previous reports, this condition may be associated with antiepileptic drug use or withdrawal. We herein report a case of reversible splenial lesion syndrome associated with oxcarbazepine withdrawal.
Case Report
A 39-year-old man presented with an 8-year history of epileptic seizures. During the previous 3 years, he had taken oxcarbazepine irregularly. One week prior to admission, he withdrew the oxcarbazepine on his own, and the epilepsy became aggravated. Magnetic resonance imaging (MRI) revealed an isolated lesion in the splenium of the corpus callosum with slight hypointensity on T1-weighted imaging and slight hyperintensity on T2-weighted imaging. Regular oxcarbazepine was prescribed. Over a 5-month follow-up period, repeat MRI showed that the abnormal signals in the splenium of the corpus callosum had completely disappeared.
Conclusion
Reversible splenial lesion syndrome is a rare clinicoradiological disorder that can resolve spontaneously with a favorable outcome. Clinicians should be aware of this condition and that oxcarbazepine withdrawal is a possible etiological factor.
Keywords: Reversible splenial lesion syndrome, antiepileptic drug, withdrawal, case report, oxcarbazepine, magnetic resonance imaging
Introduction
Reversible splenial lesion syndrome is a distinct entity radiologically characterized by a reversible lesion in the splenium of the corpus callosum.1,2 Although this disorder has been reported in patients with a variety of conditions, its definitive pathogenesis remains unclear. Potential causes include antiepileptic drug use or withdrawal, central nervous system infection, metabolic disturbances, and demyelinating neuropathies.1–4 Previous case reports have noted that withdrawal of antiepileptic drugs, such as oxcarbazepine and carbamazepine, may significantly increase the risk of reversible splenial lesion syndrome.5,6 Some scholars have speculated that this phenomenon may be attributed to reversible demyelination or cytotoxic edema after abrupt withdrawal of antiepileptic drugs.3 Due to the scarcity of related studies, more clinical evidence is needed to elucidate the correlation between reversible splenial lesion syndrome and antiepileptic drug withdrawal.
To add more clinical evidence to the current body of literature, we herein report a case of reversible splenial lesion syndrome associated with oxcarbazepine withdrawal. The relevant pathogenesis, radiological features, and prognosis were analyzed.
Case report
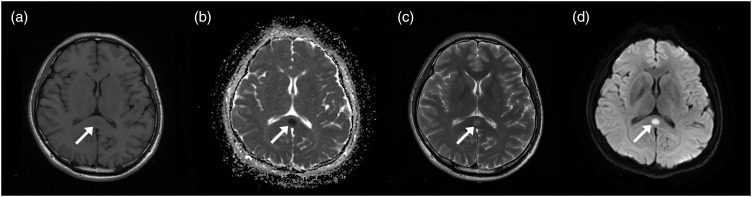
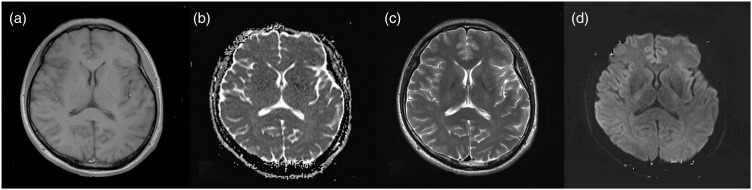
A 39-year-old man presented with an 8-year history of epileptic seizures. The seizures manifested as loss of consciousness, convulsions, limb stiffness, eye and head fixation to the left, teeth clenching, frothing at the mouth, and urinary incontinence; each episode lasted 5 to 6 minutes. The patient’s consciousness would return to normal approximately 20 to 30 minutes after the ictal episodes, at which time he would develop headache, fatigue, and somnolence. Nevertheless, the patient had no memory of the seizures. Initially, he experienced two seizures annually, and no specific treatment was administered. Three years prior to admission, he began to take oral oxcarbazepine irregularly. One week prior to admission, he withdrew the oxcarbazepine on his own, and the epilepsy became aggravated (five seizures occurred during this week). Physical examination showed no abnormality, and the patient denied any related family history. Brain magnetic resonance imaging (MRI) revealed an isolated, well-circumscribed lesion in the splenium of the corpus callosum. The lesion appeared slightly hypointense on T1-weighted imaging and apparent diffusion coefficient (ADC) imaging and slightly hyperintense on T2-weighted imaging, fluid-attenuated inversion recovery (FLAIR) imaging, and diffusion-weighted imaging (DWI); after administration of contrast medium, there was no remarkable enhancement (Figure 1). Long-term electroencephalogram monitoring demonstrated multifocal sharp and sharp-slow waves in the bilateral frontal and temporal regions during the interictal periods. Laboratory blood and cerebrospinal fluid examination findings were normal. A diagnosis of reversible splenial lesion syndrome and epilepsy (generalized tonic-clonic seizure secondary to focal impaired awareness seizures) was made. A regular regimen of oral oxcarbazepine (600 mg daily) was prescribed. The patient remained seizure-free during a 5-month follow-up period, and MRI showed that the abnormal signals in the splenium of the corpus callosum had completely disappeared (Figure 2).
Figure 1.
Brain magnetic resonance imaging on admission. Axial magnetic resonance imaging revealed an isolated lesion in the splenium of the corpus callosum. The lesion (arrows) appeared slightly hypointense on (a) T1-weighted imaging and (b) apparent diffusion coefficient imaging and slightly hyperintense on (c) T2-weighted imaging and (d) fluid-attenuated inversion recovery imaging.
Figure 2.
Brain magnetic resonance imaging 5 months after discharge. (a) Axial T1-weighted, (b) diffusion-weighted, (c) T2-weighted, and (d) fluid-attenuated inversion recovery imaging revealed that the abnormal signals in the splenium of the corpus callosum had completely disappeared.
This study was approved by the Institutional Review Board and Ethics Committee of the First Hospital of Jilin University. Informed consent was obtained from the parents of the patient.
Discussion
Reversible splenial lesion syndrome was originally reported by Kim et al.7 in 1999. They observed the characteristic focal, nonhemorrhagic, transient lesion in the splenium of the corpus callosum in patients who took dilantin and/or vigabatrin, and the authors considered that this syndrome might be related to the toxicity of the antiepileptic drugs. In 2011, Garcia-Monco et al.3 further described the radiological and clinical features of this condition and proposed the term reversible splenial lesion syndrome.
The etiology of reversible splenial lesion syndrome remains unclear. In recent years, it has been found to be associated with several disorders of various origins, including infection,1,8 epilepsy-related factors (epileptic seizures, antiepileptic drug use, and antiepileptic drug withdrawal),3,5,6 high-altitude brain edema, migraine, anorexia nervosa, peroneal myoatrophy, and systemic diseases (hypernatremia, dysglycemia, vitamin B12 deficiency, and systemic lupus erythematosus).9,10 The pathogenetic mechanisms of reversible splenial lesion syndrome remain obscure. However, the hyperintensity on DWI with low ADC values is consistent with restricted diffusion, suggestive of cytotoxic edema. The level of the extracellular excitatory neurotransmitter glutamic acid may increase due to inflammatory injury or epilepsy-related abnormal discharge of neurons, mediating the influx of sodium ions and thus resulting in cytotoxic edema of myelin sheath cells. Additionally, hypoglycemia may cause energy pump failure and water-sodium retention, leading to cytotoxic edema; this hypothesis can explain the reversibility of the splenial lesions. Moreover, the splenium of the corpus callosum may be sensitive to water–electrolyte imbalance or osmotic changes, making it vulnerable in various neurological or systemic disorders.11 In the current case, we considered the possible cause of the reversible splenial lesion syndrome to be oxcarbazepine withdrawal and the resultant frequent seizures. After regular administration of oxcarbazepine, the epilepsy was well controlled and the splenial lesion disappeared, supporting the above speculation.
Reversible splenial lesion syndrome has characteristic radiological features, manifesting as an isolated, round- or ovoid-shaped, well-circumscribed lesion in the central part of the splenium of the corpus callosum with hypointensity to isointensity on T1-weighted imaging and slight hyperintensity on T2-weighted and FLAIR imaging. The signal is usually homogeneous without necrosis or cystic changes, and there is no remarkable perilesional edema or space-occupying effect. After administration of contrast medium, the lesion shows no enhancement. On DWI, the lesion appears hyperintense with low ADC values. These radiological abnormalities are transient and reversible, usually disappearing after a variable lapse.12
Based on our clinical experience, the differential diagnoses of reversible splenial lesion syndrome should include a) multiple sclerosis, which usually affects middle-aged women and manifests as multifocal periventricular lesions with remarkable “open-ring” enhancement; b) Marchiafava–Bignami disease, which usually affects middle-aged and older men with a long-term history of alcoholism and manifests as abnormal signals in the body and genu of the corpus callosum with a space-occupying effect and contrast enhancement on MRI; c) acute disseminated encephalomyelitis, which manifests as asymmetric lesions in the white matter of the bilateral hemispheres and in the body and genu of the corpus callosum with significant contrast enhancement on MRI; d) neoplasms in the corpus callosum, which are usually associated with peritumoral edema, a space-occupying effect, and variable contrast enhancement; e) reversible posterior leukoencephalopathy syndrome, which usually affects patients with hypertensive encephalopathy or eclampsia; and f) local infarcts in the splenium of the corpus callosum, which are common in older patients with posterior circulation ischemia.
There is no specific treatment for reversible splenial lesion syndrome, and the current mainstream therapeutic options target the primary etiological factors. The prognosis of reversible splenial lesion syndrome is usually favorable. Previous studies have shown that the clinical outcomes of patients with reversible splenial lesion syndrome are mainly associated with the potential etiologies.13 In the current case, after the antiepileptic regimen was prescribed, the patient achieved a satisfactory recovery. Clinicians should be aware of how to identify reversible splenial lesion syndrome and ensure close follow-up observation. Specific interventions do not seem warranted.
Conclusion
Reversible splenial lesion syndrome is an infrequent clinicoradiological disturbance that can resolve spontaneously, and the individual prognosis is usually favorable. Clinicians should be aware of this disorder and that anti-epilepsy drug withdrawal may be a possible etiological cause.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Li C, Wu X, Qi H, et al. Reversible splenial lesion syndrome associated with lobar pneumonia: Case report and review of literature. Medicine (Baltimore) 2016; 95: e4798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen WX, Liu HS, Yang SD, et al. Reversible splenial lesion syndrome in children: Retrospective study and summary of case series. Brain Dev 2016; 38: 915–927. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Monco JC, Cortina IE, Ferreira E, et al. Reversible splenial lesion syndrome (RESLES): what's in a name? J Neuroimaging 2011; 21: e1–e14. [DOI] [PubMed] [Google Scholar]
- 4.Kaino K, Kumagai R, Furukawa S, et al. Reversible splenial lesion syndrome with a hyperosmolar hyperglycemic state and neuroleptic malignant syndrome caused by olanzapine. J Diabetes Investig 2017; 8: 392–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cortese R, Pontrelli G, Mogavero MP, et al. Reversible splenial lesion and complex visual disturbances due to carbamazepine withdrawal. Neurol Sci 2015; 36: 1515–1516. [DOI] [PubMed] [Google Scholar]
- 6.Güven H, Delibaş S, Comoğlu SS, et al. Transient lesion in the splenium of the corpus callosum due to carbamazepine. Turk Neurosurg 2008; 18: 264–270. [PubMed] [Google Scholar]
- 7.Kim SS, Chang KH, Kim ST, et al. Focal lesion in the splenium of the corpus callosum in epileptic patients: antiepileptic drug toxicity? AJNR Am J Neuroradiol 1999; 20: 125–129. [PubMed] [Google Scholar]
- 8.Avcu G, Kilinc MA, Eraslan C, et al. Mild encephalitis/encephalopathy with reversible splenial lesion (MERS) associated with Streptococcus pneumoniae Bacteraemia. J Infect Public Health 2017; 10: 479–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin FY, Yang CY. Reversible splenial lesion of the corpus callosum in migraine with aura. Neurologist 2011; 17: 157–159. [DOI] [PubMed] [Google Scholar]
- 10.Yamashita S, Kawakita K, Hosomi N, et al. Reversible magnetic resonance imaging changes associated with hypoglycemia. Case report. Neurol Med Chir (Tokyo) 2010; 50: 651–654. [DOI] [PubMed] [Google Scholar]
- 11.Takanashi J, Barkovich AJ, Yamaguchi K, et al. Influenza-associated encephalitis/encephalopathy with a reversible lesion in the splenium of the corpus callosum: a case report and literature review. AJNR Am J Neuroradiol 2004; 25: 798–802. [PMC free article] [PubMed] [Google Scholar]
- 12.Conti M, Salis A, Urigo C, et al. Transient focal lesion in the splenium of the corpus callosum: MR imaging with an attempt to clinical-physiopathological explanation and review of the literature. Radiol Med 2007; 112: 921–935. [DOI] [PubMed] [Google Scholar]
- 13.Achalia R, Andrade C, Reversible abnormality of the splenium in a bipolar patient with neuroleptic malignant syndrome. Bipolar Disord 2014; 16: 773–775. [DOI] [PubMed] [Google Scholar]