Abstract
Prevalence estimates of very young children’s exposure to potentially traumatic events (PTEs) are limited. The study objective was to estimate the lifetime prevalence and correlates of noninterpersonal PTEs and violence exposure in a representative healthy birth cohort (ages 1–3 years) from an urban–suburban region of the United States (37.8% minority, 20.2% poverty). Parents completed 2 surveys approximately 1-year apart. By 24–48 months of age, the prevalence of exposure was 26.3% (14.5% noninterpersonal, 13.8% violence). Exposure was common among children living in poverty (49.0% overall, 19.7% noninterpersonal, 33.7% violence). The most consistent factors associated with exposure were poverty, parental depressive symptoms, and single parenting. Findings underscore the potential for prevention and intervention in early childhood to advance public health and reduce morbidity.
Among older youth and adults, exposure to potentially traumatic experiences (PTEs), such as serious injury, loss, natural disasters, and violence, has been linked to increased risk for an array of mental health problems (Copeland, Keeler, Angold, & Costello, 2007; Ford, Stockton, Kaltman, & Green, 2006; Kessler, Davis, & Kendler, 1997). Evidence of associations between PTEs and social, emotional, and behavioral problems and psychiatric disorders has begun to emerge even in very young children (under 6 years of age; Bogat, DeJonghe, Levendosky, Davidson, & von Eye, 2006; Briggs-Gowan et al., 2010; Meiser-Stedman, Smith, Glucksman, Yule, & Dalgleish, 2008; Scheeringa, 2009). Adverse experiences occurring in early childhood may be particularly detrimental to functioning because this period is important for brain development and differentiation (De Bellis & Van Dillen, 2005; Teicher, Tomoda, & Andersen, 2006). However, although they are essential to inform prevention and intervention efforts, limited data exist concerning the prevalence and correlates of PTEs in early childhood.
In young children, PTEs may be defined using developmentally modified diagnostic criteria for posttraumatic stress disorder (PTSD; Zero to Three, 1994) as events that “involve actual or threatened death or serious injury to the physical or psychological integrity of the child or another person.” Although closely resembling the posttraumatic stress disorder definition of traumatic events according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition-Text Revision (DSM-IV-TR; American Psychiatric Association, 2000), this definition differs because diagnostic criteria for young children do not require that the child experience intense fear, helplessness, or horror at the time of the event. Potentially traumatic experiences can further be classified as interpersonal or involving the intentional acts of other persons, such as violence toward another person or acts of war (Ford et al., 2006). Noninterpersonal PTEs, by contrast, do not involve the intentional acts of other person(s) and include experiences, such as car accidents, injuries, animal attacks, and natural disasters. The relevance of distinguishing between interpersonal and noninterpersonal events lies in evidence that interpersonal events may have particularly detrimental effects on functioning (Briggs-Gowan et al., 2010; Ford et al., 2006).
As many as 90% of adults in the United States are estimated to have experienced one or more PTE in their lifetime (Breslau et al., 1998; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Many exposures appear to occur before adulthood, as Copeland and colleagues (2007) estimated that 68% of adolescents had experienced at least one PTE in their lifetime. Exposures may begin in early childhood. However, estimates for this period are very limited. One study of 1- to 5-year-olds attending an urban primary care practice serving low-income families indicated that 10% had witnessed a knifing or shooting and 18% had witnessed at least one episode of shoving, kicking, or punching (Taylor, Zuckerman, Harik, & Groves, 1994). The prevalence of interparental violence exposure in the United States is estimated from 12 to 24% (Knickerbocker, Heyman, Slep, Jouriles, & McDonald, 2007; Slep & O’Leary, 2005). One study estimated the past-year prevalence of exposure to severe interparental violence at 24% among 3- to 7-year-olds (Slep et al., 2005); however, the generalizability of this estimate is constrained by a low response rate. To our knowledge, the prevalence of noninterpersonal PTEs in early childhood has not been reported.
Some studies have suggested sex differences in exposure, with boys at greater risk for accidents and injuries (Scheidt et al., 1995; Stoddard et al., 2006) and girls at greater risk for witnessing inter-parental violence (Bogat et al., 2006). Childhood violence exposure also has been linked to poverty (Christoffel, 1990; Cunradi, Caetano, Clark, & Schafer, 2000; Margolin & Gordis, 2000). Other factors associated with exposure, including lower parental education, single parenting, and parental mood and anxiety symptoms, are commonly associated with both poverty and poorer childhood outcomes (Appleyard, Egeland, van Dulmen, & Sroufe, 2005; Briggs-Gowan et al., 2010; Scheeringa, 2009). Disentangling the effects of poverty from those of other risk factors may clarify patterns of risk.
The present study capitalized on data from a healthy birth cohort of young children (ages 1 to 3 years) from an urban–suburban region of the northeastern United States. The first aim was to estimate the lifetime prevalence of exposure overall and by poverty status. Drawing on the limited data available for young children and estimates for adolescents and adults, the prevalence of exposure to potentially traumatic violence and noninterpersonal events was hypothesized to be approximately 20%. The second aim was to investigate possible sex differences, with boys hypothesized to be at greater risk for noninterpersonal PTEs and girls at greater risk for witnessing violence. The final aim was to identify sociodemographic and parental factors associated with lifetime exposure (reported in the first survey when children were approximately 1 and 2 years of age) and incident exposure (i.e., exposures first reported in the second survey, when children were approximately 2 or 3 years of age, among those without prior exposure). The possibility that poverty may moderate the associations between other risk factors and exposure also was examined.
METHOD
Participants
Participants are from a longitudinal study of a healthy birth cohort that was randomly selected from healthy birth records at the State of Connecticut Department of Public Health for children born at Yale-New Haven Hospital and living in the 15 towns and cities that comprised the New Haven-Meriden Standard Metropolitan Statistical Area of the 1990 Census. This region has been examined in several large-scale community studies because of its mix of urban and suburban families and socioeconomic and ethnic diversity (Briggs-Gowan, Horwitz, Schwab-Stone, Leventhal, & Leaf, 2000; Lahey et al., 1996). Births from July 1995 through September 1997 were eligible. As shown in Figure 1, because the aim of the original study was to refine and validate a measure of normative development, children at high risk for serious developmental delay due to birth complications (e.g., lack of oxygen, need for resuscitation), prematurity (< 36 weeks), low birth weight (< 2,200 grams), and genetic disorders (e.g., Down syndrome), were excluded, as were those with a sibling already sampled or who were deceased or adopted. A sex- and age- (3-month age bands) stratified random sample of 1,788 was drawn from the 7,433 who where eligible after exclusions, with sample size determined by the original study aims and response rate projections.
Figure 1.
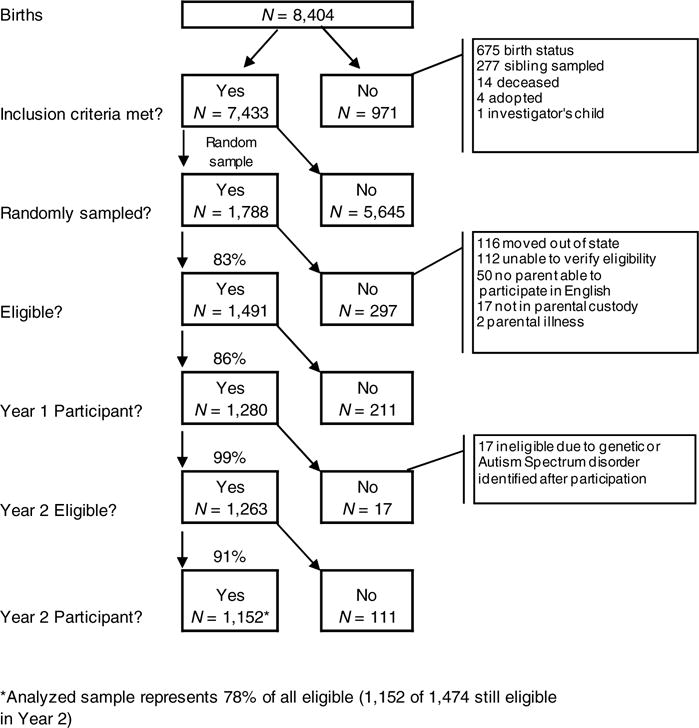
Sampling design, response, and retention.
Three eligibility criteria were applied after sampling: parent able to participate in English; child in parental custody, and continued residence in the state (if not still residing in the region sampled), resulting in a final eligible sample of 1,491. There were no differences between eligible (n = 1,491) and noneligible (n = 297) children in gestational age, paternal education, or child sex. However, eligible children tended to have higher birthweight (Meligible = 3,422, SD = 486 vs. Mnoneligible = 3,334, SD = 493 grams, respectively), t(1786) = 2.84, p =< .01, Cohen’s d= 0.18; older parents—paternal age: Meligible = 32.2, SD = 6.5 vs. Mnoneligible = 30.4, SD = 6.6 years, t(1786) = 3.77, p < .01, Cohen’s d= 0.27, and maternal age: Meligible = 29.5, SD = 6.1 vs. Mnoneligible = 27.1.4, SD = 5.7 years, t(1786) = 6.26, p < .01, Cohen’s d = 0.41; and higher maternal education (Meligible = 14.0, SD = 2.4 vs. Mnoneligible = 13.2, SD = 2.8 years), t(1786) = 4.36, p < .01, Cohen’s d = 0.31. Eligible children were less likely to be of minority ethnicity (25.7%) than noneligible children (42.4%), χ2(1, 1788) = 33.25, p < .01. However, although these differences were statistically significant, the effect sizes were in the small to moderate range (Cohen’s d of .50 is considered a medium size effect; Cohen, 1988). The sample also was similar to the target region (see below).
Analyses focused on participants in two annual surveys. In Year 1, 1,280 parents participated (86% of 1,491 eligible). Parents were invited to complete another survey approximately 1 year later (Year 2). The mean intersurvey interval was 368 days (SD = 64, median = 368). Seventeen children were deemed ineligible after participation due to serious developmental disabilities (e.g., autism, Down syndrome) identified after sampling. After these exclusions and the exclusion of one child with missing data, 1,152 children with data from both years were available for analyses, representing 78% of the 1,474 eligible children. Children in the analyzed sample (n = 1,152) were similar (p > .05) to all other eligible children whose families did not participate in one or both years (n = 322) in child sex, birth weight, paternal age, gestational age, and years at the birth address, but were significantly more likely to be Caucasian, χ2(1, 1473) = 9.78, p < .05, had slightly higher parental education—mothers: t(1394) = −3.72, p<.01, Mnonparticipant = 13.6, SD = 2.4 versus Mparticipant = 14 2, SD = 2.3, Cohen’s d = 0.24, and fathers: t(1325) = −2.49, p < .01, Mnonparticipant = 13.8, SD = 2.2 versus Mparticipant = 14.2, SD = 2.3, Cohen’s d = 0.17; and slightly older maternal age, t(1471) = −2.94, p < .01, Mnonparticipant = 28.6, SD = 6.2 versus Mparticipant = 29.7, SD = 6.1, Cohen’s d = 0.19.
In Year 1, 96% of children were 12–36 months of age, with a median age of 24.5 months (M = 24.5, SD = 7.2, range = 11.5–42.0). In Year 2, 97% of children were 24–48 months of age, with a median age of 36.6 months (M = 36.6, SD = 7.2, range = 23.9–56.9). A small percentage of children were outside the target age range of 12–36 months in Year 1 or 24–48 months in Year 2, due to variation in the timing of mailings and the promptness of locating parents and obtaining participation. Early and late participation was associated with characteristics potentially associated with risk for exposure (minority ethnicity, lower parental education, χ2 = 6.24–8.63, df from 1,968 to 1,1151, p < .05); therefore, they were retained in analyses.
The sample was ethnically and sociodemographically diverse (Table 1) and similar to the region, according to 2006–2008 Census Bureau estimates for families with young children in New Haven County (U.S. Census Bureau, 2006–2008). Specifically, the sample and the region were similar with respect to marital status (74% vs. 72% married), minority race (76% vs. 77% Caucasian according to race reported at birth), and poverty status (17% vs. 16%); however, mothers in the analyzed sample were more likely to have attained a high school education than mothers in the region (74% vs. 66%).
Table 1.
Participant Characteristics (N = 1, 152)
| N | % | % Weighted | |
|---|---|---|---|
| Boys | 598 | 51.9 | 49.6 |
| Girls | 554 | 48.1 | 50.4 |
| Ethnicity | |||
| Caucasian | 768 | 66.7 | 62.2 |
| African American/Black | 185 | 16.1 | 19.9 |
| Hispanic | 60 | 5.2 | 5.1 |
| Multiethnic (Black and/or Hispanic) | 94 | 8.1 | 8.9 |
| Other | 45 | 3.9 | 3.9 |
| Respondent | |||
| Biological mother | 1107 | 96.1 | 96.2 |
| Biological father | 36 | 3.1 | 3.0 |
| Other | 9 | 0.8 | 0.8 |
| Maternal education | |||
| ≤High school | 295 | 25.8 | 28.4 |
| Beyond high school | 849 | 74.2 | 71.6 |
| Paternal education | |||
| ≤High school | 281 | 29.0 | 30.6 |
| Beyond high school | 688 | 71.0 | 69.4 |
| Other sociodemographic indicators | |||
| Living in poverty | 196 | 17.4 | 20.2 |
| Single-parent household | 211 | 18.3 | 21.3 |
In the summer of 1998, parents were mailed a letter describing the study, followed 1 week later by a survey, consent form, and children’s book. Surveys were mailed 2 weeks before children entered a sampling age-band. Staff subsequently telephoned parents to encourage participation. Tracking staff familiar with the communities visited family addresses to verify that addresses were current, locate new addresses, and encourage parents to participate. This procedure was repeated in 1999. Parents received $25 for completing each survey. All procedures were approved by two institutional review boards. Parental consent was obtained.
Measures
The Child Life Events Scale (Carter & Briggs-Gowan, 1998) is a checklist on which parents indicate the child’s lifetime experience of each of 14 events that “may be upsetting for young children” including PTEs and more normative events, such as birth of a sibling. Given the young age of the sample, establishing whether children perceived events as involving potential harm or death to self or other was not possible. Therefore, events analyzed were restricted to those most likely to have the potential to be perceived by young children as life threatening or involving potential harm. Three items described violence exposure: “seen violence in neighborhood,” “seen someone hit, push, or kick a family member,” and “seen someone use a weapon to threaten or hurt a family member.” Three items described potentially traumatic noninterpersonal events: “bitten by a dog,” “been in a car accident,” and “hurt seriously.” Parents also provided written descriptions of injuries. To be conservative, injuries were restricted to those involving concussion, head trauma, or burns, because the pain, disorientation, and loss of consciousness that may be associated with these types of injuries were considered more likely to be perceived as life-threatening than more minor injuries (e.g., injuries needing stitches or broken bones). These injuries were coded by independent review of the first and second authors, followed by a consensus rating of any discrepancies. Parents were asked to report the child’s age the last time the event occurred. This information was used to exclude events that happened prior to 6 months because younger infants may be in a stress hyporesponsive period in which the biological effects of PTEs might be substantially attenuated (Heim, Plotsky, & Nemeroff, 2004). Individual events and composite variables reflecting any violence exposure and any noninterpersonal PTE were used in analyses.
Sociodemographic characteristics were gathered from birth records and surveys. Poverty calculations were based on household size and income and whether income-based public assistance was received.
The Center for Epidemiologic Studies Depression Scale (Radloff, 1977) is a 20-item self-report adult depression scale. Items are rated on a 4-point scale from rarely/none to all of the time. A clinical cutpoint of 16 has been recommended (Radloff et al., 1977). Internal consistency (α = .88) and test-retest reliability (intraclass correlation coefficient [ICC] .69) were acceptable in this sample. Prior research has indicated adequate criterion-related validity (Myers & Weissman, 1980).
The Beck Anxiety Inventory (Beck, Epstein, Brown, & Steer, 1988) is a 21-item self-report scale for assessing adult anxiety symptoms. Items are rated on a 4-point scale from not at all to severely bothered. A clinical cut of 16 was used (Beck et al., 1988). Internal consistency (α = .86) and test-retest reliability (ICC = .59) were adequate.
Social support was measured with a 12-item measure of instrumental and emotional support from the Medical Outcomes Study (Sherbourne & Stewart, 1991). Items are rated on a 5-point scale from none of the time to all of the time. Internal consistency was acceptable (α = .96). Low social support was indicated by scores ≤ 1.5 SD below the sample mean.
The total score of the Parenting Stress Index Short Form (Abidin, 1990) was used to assess parenting stress related to raising a child who the parent perceives as difficult to manage, general parenting role distress, and raising a child who does not meet parental expectations and reinforce the parent. The total Parenting Stress Index score had acceptable internal consistency (α = .94) and has demonstrated acceptable test-retest reliability (r =.68–.85) and validity in previous research (Abidin, 1990). The recommended cutpoint of 90 was used to indicate clinical levels of stress (Abidin, 1990).
Data Analysis
Weights were applied in all analyses to adjust for unequal probabilities of selection and retention. These weights adjusted for the probability of selection and adjusted for differential nonresponse and attrition on the basis of background characteristics such as gestational age, birth weight, mother’s and father’s age, and mother’s education, which were available from birth records. Because parents reported about children’s exposure in their “whole life,” prevalence estimates represent lifetime exposure. Year 2 estimates are calculated cumulatively, meaning they incorporate exposures reported in Year 1. Incident exposure refers to events reported as occurring between the Year 1 and Year 2 surveys among children with no exposure history reported in Year 1; instances when the age of occurrence predated the Year 1 survey were excluded.
Prevalence and standard error estimates were generated in SAS Version 9.1 Surveyfreq procedure, which is appropriate for calculating prevalence estimates with weighted data. Bivariate analyses examining significance of associations between risk factors and exposure variables were examined with the Rao-Scott chi-square statistic (in SAS Surveyfreq) and odds ratios (OR) with 95% confidence intervals (CIs; in SAS Surveylogistic). These relationships were further examined with multivariate logistic regression models (in SAS Surveylogistic). Variables with significant bivariate associations with the dependent variable were individually added to a model and retained if (a) they were significantly associated with the outcome, or (b) their inclusion significantly improved model fit, as indicated by significant change in model fit assessed with the G2 statistic (−2 log likelihood ratio), which is distributed as χ2, and/or changed the parameter estimate of another variable by 10% or more, suggesting shared variance. The first variable entered had the largest bivariate association with the exposure variable. The second variable retained had the largest effect on the model and/or on the parameter estimate of the first variable, and so on. Father education data was not included due to missing data for single-parent families. Given anticipated moderation by poverty of the effects of other risk factors, interactions with poverty also were examined.
RESULTS
Prevalence estimates of lifetime exposure to one or more PTE include lifetime exposure reported at the time of the first survey (Year 1), when children were approximately 12–36 months of age, and cumulatively at the time of the second survey (Year 2), when children were approximately 24–48 months of age (Table 2). Poverty was associated with increased likelihood of exposure to any violence, individual types of violence, and car accidents at both study points, and with any noninterpersonal PTE reported by Year 2. There was no significant relationship between exposure to violence and noninterpersonal PTEs in either year, χ2(1, 1137) = 1.47, ns, and χ2(1, 1148) = 1.77, ns.
Table 2.
Lifetime Prevalence of Potentially Traumatic Interpersonal and Noninterpersonal Events (N = 1152)
| Lifetime exposure (Year 1)
|
Lifetime exposure (Year 2)
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Full sample
|
Nonpoor
|
Poor
|
Full sample
|
Nonpoor
|
Poor
|
|||||||||
| N | % | SE | % | SE | % | SE | N | % | SE | % | SE | % | SE | |
| Any event | 192 | 16.9 | (1.3) | 13.9a | (1.3) | 29.2b | (3.5) | 303 | 26.3 | (1.4) | 20.5a | (1.5) | 49.0b | (3.7) |
| Noninterpersonal | 105 | 9.3 | (1.0) | 8.4a | (1.1) | 12.9a | (2.6) | 167 | 14.5 | (1.2) | 13.2a | (1.2) | 19.7b | (3.0) |
| Major injury/burn | 12 | 1.1 | (0.3) | 1.1a | (0.3) | 1.0a | (0.7) | 23 | 2.0 | (0.5) | 1.8a | (0.4) | 2.6a | (1.7) |
| Dog bite | 18 | 1.6 | (0.3) | 1.7a | (0.4) | 1.2a | (0.7) | 42 | 3.7 | (0.5) | 3.7a | (0.6) | 3.5a | (1.4) |
| Car accident | 92 | 8.1 | (1.0) | 6.7a | (1.0) | 13.8b | (2.7) | 119 | 10.3 | (1.0) | 8.6a | (1.1) | 16.7b | (2.9) |
| Violence | 96 | 8.5 | (0.9) | 5.9a | (0.9) | 18.6b | (3.0) | 159 | 13.8 | (1.2) | 8.7a | (1.0) | 33.7b | (3.6) |
| Neighborhood | 16 | 1.4 | (0.5) | 0.5a | (0.2) | 4.8b | (2.0) | 24 | 2.1 | (0.5) | 0.8a | (0.3) | 7.5b | (2.2) |
| Weapon family | 6 | 0.6 | (0.2) | 0.3a | (0.2) | 1.6b | (0.9) | 14 | 1.3 | (0.3) | 0.6a | (0.2) | 3.7b | (1.3) |
| Hit, push, kick family | 88 | 7.7 | (0.9) | 5.9a | (0.9) | 15.0b | (2.6) | 141 | 12.3 | (1.1) | 8.2a | (1.0) | 28.3b | (3.4) |
Note. Within each year, weighted prevalence estimates with different superscript letters differ significantly (p < .05) between poor and nonpoor families. SE = Standard error of the prevalence estimate.
Poverty, minority ethnicity, marital status, parental education, and high parental depressive symptoms were significantly inter-correlated (ϕ = .07 to 53, all p < .05). However, parental anxiety correlated significantly only with poverty (ϕ = .13, p < .001) and depressive symptoms (ϕ = .26, p < .001). (Data available upon request).
Results of bivariate analyses indicated that lifetime exposure to noninterpersonal PTEs (reported in Year 1) was significantly associated only with high parental depressive symptoms (Table 3). There were no significant interactions with poverty.
Table 3.
Bivariate Tests for Association Between Potential Risk Factors and Exposure to Noninterpersonal Events
| Lifetime exposure(reported in Year 1)
|
Incident exposure
|
|||||
|---|---|---|---|---|---|---|
| Risk absent % | Risk present % | OR | 95% CI | OR | 95% CI | |
| Child sex (male) | 10.9 | 7.7 | 0.7 | 0.4–1.1 | 1.1 | 0.6–2.0 |
| Older children | 7.4 | 11.0 | 1.5 | 0.9–2.5 | 1.1 | 0.6–2.1 |
| Poverty | 8.4 | 13.0 | 1.6 | 0.9–2.8 | 1.2 | 0.5–2.6 |
| Minority ethnicity | 9.1 | 9.7 | 1.1 | 0.6–1.8 | 1.0 | 0.5–2.0 |
| Single parent | 8.4 | 12.5 | 1.6 | 0.9–2.7 | 0.9 | 0.4–2.1 |
| Maternal education ≤ high school | 10.2 | 6.8 | 0.6 | 0.4–1.1 | 1.6 | 0.8–3.1 |
| Paternal education ≤ high school | 8.2 | 9.3 | 1.1 | 0.6–2.1 | 0.6 | 0.3–1.4 |
| Parent depressive symptoms | 8.3 | 14.3 | 1.8* | 1.0–3.3 | 0.9 | 0.4–2.3 |
| Parent anxiety symptoms | 9.3 | 9.8 | 1.1 | 0.4–2.6 | 3.6** | 1.3–10.3 |
| Low social support | 9.8 | 5.2 | 0.5 | 0.2–1.2 | 0.8 | 0.2–2.6 |
| Parenting stress | 9.4 | 7.5 | 0.8 | 0.2–3.6 | 3.1** | 1.2–7.5 |
Note. Incident exposure = First-time potentially traumatic event reported in Year 2 among those with no history of exposure; OR = odds ratio, 95% CI = confidence interval for OR.
p < .05.
p < .01.
Results of additional bivariate tests revealed that incident exposure to noninterpersonal PTEs (i.e., events reported as occurring in Year 2 among children without prior history of exposure) was associated with high parenting stress and parental anxiety (Table 3). The results of a multivariate model for incident noninterpersonal PTEs, G2(2, 984) = 338.30, p < .05, indicated that although both anxiety and parenting stress met criteria for entry in the model (entry order: anxiety, parenting stress) only parenting stress was uniquely associated with incident noninterpersonal exposure (OR = 2.6, 95% CI = 1.1–6.2, p < .05). Anxiety was not uniquely associated with exposure once parenting stress was added to the model (OR = 2.6, 95% CI = 0.9–7.1, p < .10), suggesting shared variance with parenting stress. Incident exposure to noninterpersonal PTEs was too rare among children in poverty (n< 10) to test poverty interactions.
In bivariate analyses, lifetime exposure to violence was associated with several risk factors (Table 4). The multivariate model for lifetime violence exposure included (in order of entry) anxiety, depression, poverty, and marital status, G2 (4, 1094) = 584.84, p < .001. Violence exposure was uniquely associated with poverty (OR = 2.3, 95% CI = 1.0–5.1, p < .05) and depressive symptoms (OR = 2.0, 95% CI = 1.1–3.6, p < .05). Single parenting and anxiety symptoms met model inclusion criteria, but were not uniquely associated with exposure, p > .10. Finally, a significant poverty by single-parent interaction, χ2(4, 1094) = 4.62, p < .05, significantly improved model fit, G2 change = 7.14, p < .05. This interaction reflected greater risk for violence in children (a) not living in poverty from single-parent homes compared with two-parent homes (OR = 3.2, 95% CI = 1.3–8.2, p < .01), (b) from two-parent homes with poverty compared to without poverty (OR = 4.2, 95% CI = 2.0–9.0, p < .01), and (c) living in poor single-parent homes versus nonpoor two-parent homes (OR = 3.5, 95% CI = 1.9–6.2, p < .01).
Table 4.
Bivariate Tests for Association Between Potential Risk Factors and Exposure to Violence
| Lifetime exposure (reported in Year 1)
|
Incident exposure
|
|||||
|---|---|---|---|---|---|---|
| Risk absent % | Risk present % | OR | 95% CI | OR | 95% CI | |
| Child sex (male) | 9.4 | 7.6 | 0.8 | 0.5–1.3 | 1.0 | 0.5–2.1 |
| Older children | 7.6 | 9.3 | 1.1 | 0.7–1.7 | 0.5* | 0.3–0.9 |
| Poverty | 5.9 | 18.6 | 3.7*** | 2.2–6.0 | 6.3*** | 3.2–12.6 |
| Minority ethnicity | 6.6 | 11.7 | 1.9** | 1.2–3.0 | 2.6** | 1.3–5.0 |
| Single parent | 6.3 | 16.5 | 2.9*** | 1.8–4.9 | 2.6* | 1.2–5.6 |
| Maternal education ≤ high school | 8.0 | 9.7 | 1.2 | 0.7–2.0 | 1.5 | 0.7–3.0 |
| Paternal education ≤ high school | 5.3 | 9.9 | 2.0* | 1.1–3.4 | 2.4* | 1.1–5.1 |
| Parent depressive symptoms | 6.6 | 16.7 | 2.8*** | 1.6–4.8 | 2.9** | 1.3–6.4 |
| Parent anxiety symptoms | 7.7 | 24.5 | 3.9*** | 1.8–8.6 | 1.8 | 0.5–6.3 |
| Low social support | 7.8 | 13.9 | 1.9 | 0.9–3.8 | 1.8 | 0.7–4.8 |
| Parenting stress | 8.1 | 13.5 | 1.8 | 0.8–3.8 | 1.4 | 0.5–4.4 |
Note. OR = odds ratio; 95% CI = confidence interval for OR.
p < .05.
p < .01.
p < .001.
Incident violence exposure also was related to several risk factors (Table 4). The final multivariate model for incident violence exposure included poverty and depressive symptoms, G2(2, 1012) = 368.25, p < .05. Incident exposure was uniquely associated with poverty (OR = 5.6, 95% CI = 2.8–11.3, p < .01), but not depressive symptoms (OR = 2.1, 95% CI = 0.9–4.7, ns); however, including depressive symptoms improved model fit (G2 change = 5.67, p < .05). A single-parent by poverty interaction also improved model fit (G2 change = 4.52, p < .05). This interaction reflected greater risk among poor children in single-parent homes relative to nonpoor children in two-parent homes (OR = 5.2, 95% CI = 2.3–11.6, p < .05).
DISCUSSION
Approximately one quarter of the children in this representative healthy birth cohort from an urban and suburban region in the northeastern United States had experienced one or more potentially traumatic event by 2 to 3 years of age. These experiences, which included witnessing violence in the family or neighborhood, being involved in a car accident, bitten by a dog, or seriously injured, were particularly common among children living in poverty (49%), but also were apparent in children not living in poverty (21%). Additionally, exposure to PTEs was significantly associated with contextual risks in children’s lives, such as living in a single-parent home, high parenting stress, and clinical levels of parental mood and anxiety symptoms. Although these findings certainly require replication in samples that include children with birth complications (in addition to those born healthy as studied here), and in samples from other geographic locales (e.g., rural areas), they do suggest that a substantial proportion of very young children are exposed to potentially traumatic events. These patterns underscore the need for rigorous research to clarify the effects of early life exposure, identify characteristics of children and their families that are associated with vulnerability, and delineate mechanisms through which harm is manifest.
Findings also suggest that parental symptoms and stress may be important foci for prevention and intervention. In the case of noninterpersonal PTEs, problems in parental functioning were associated with lifetime and incident exposure. Children who had experienced a serious injury, car accident, or dog bite prior to the first survey tended to have parents who reported clinical levels of depressive symptoms. However, causation cannot be assumed because the timing of when the depressive symptoms onset relative to the exposure could not be established. Parenting stress also was uniquely associated with incident noninterpersonal PTEs, and, although not uniquely related to these PTEs, parental anxiety had a significant bivariate relationship that appeared to share variance with parenting stress. These findings suggest that depressed or stressed and anxious parents may benefit from interventions or support aimed at helping them to anticipate or prevent accidental threats to their young children’s safety.
The 17–26% estimated prevalence of violence exposure in this early childhood sample was in keeping with prevalence estimates (15–24%) of childhood exposure to domestic violence (Knickerbocker et al., 2007). Consistent with prior research (Christoffel, 1990; Cunradi et al., 2000; Margolin & Gordis, 2000) exposure was 2 to 5 times more likely among children living in poverty compared to other children. Furthermore, although seeing someone hit, push, or kick a family member was the most common form of violence witnessed, up to 7% of children living in poverty had witnessed neighborhood violence and nearly 4% had seen someone use a weapon to threaten or hurt a family member. Indeed, poverty was consistently uniquely associated with increased risk for violence exposure, with associations observed for both lifetime and incident exposure. Further, single parenting was associated with increased likelihood of lifetime violence exposure, particularly among children not living in poverty. Notably, although minority ethnicity and maternal education were individually linked to violence exposure, these associations were not significant once poverty was taken into consideration. Violence exposure also was associated with parental depressive symptoms, consistent with the pattern observed for noninterpersonal PTEs. The timing of the onset of parental depressive symptoms relative to the child’s violence exposure could not be established. However, because young children are frequently in the care of their parents and because parents of young children are most likely to be aware of violence that occurred in their presence, this association may reflect parental victimization or, at least, shared witnessing of the violence. Whatever the direction of effect, these young children appear to have experienced not only violence, but also other risk factors commonly associated with social–emotional problems in young children (Zeanah, 2000).
In contrast with earlier evidence that boys may be at greater risk for accidents and injuries (Scheidt et al., 1995; Stoddard et al., 2006) and girls may be at greater risk for witnessing interparental violence (Bogat et al., 2006), no sex differences were observed. This inconsistency may be related to sampling differences, selection biases, or referral patterns, as prior samples were not sampled within a representative framework. Alternatively, sex differences may be associated with features of exposure that were not assessed in this study, such as severity or chronicity of exposure.
Although a representative healthy birth cohort from a suburban and urban region was studied with a strong initial response rate and retention, children with birth complications were excluded from the sample and mothers in the sample were somewhat more educated than mothers in the region. Exposure was assessed with two annual surveys, enhancing the likelihood that events were recalled and reducing the effect of selective memory on parental reports relative to retrospective reports over longer periods. However, the study relied on a single informant and some important PTEs were not assessed, including child abuse and neglect (due to concern about asking about these sensitive topics in a mailed questionnaire), natural disasters, and acts of war and terrorism. Parents also may have defensively underreported some events due to concern about stigma or institutional responses (e.g., child protection investigation), lack of knowledge about events, or not considering events sufficiently adverse to warrant reporting (Daviss et al., 2000; Ford et al., 2000). Additionally, because the severity of dog bites and car accidents was not established, estimates may include some experiences that would not be considered “potentially traumatic.” Similarly, some injuries related to abuse or neglect may have been inappropriately classified as noninterpersonal. Subjective distress at the time of the event was not assessed. Although this criterion of PTSD is not considered developmentally appropriate for young children (Scheeringa et al., 2003), that it was not assessed constrains comparisons with other studies (e.g., Copeland et al., 2007). Finally, the assessment did not allow examination of the total number of distinct events or repeated events experienced.
The high prevalence of early childhood exposure observed, combined with mounting evidence from other studies that has linked these types of exposures with symptoms and disorders in young children, highlights the need for systematic research about how these experiences affect young children. Furthermore, as PTEs adversely affect some children but not others (Bonanno & Mancini, 2008), research is needed to identify the sequelae and mechanisms involved in response to trauma. Moreover, awareness of the high prevalence of these PTEs, many of which may be preventable, should inform efforts to establish preventive programs. Given the risk of long-term morbidity associated with trauma and the importance of early childhood for brain development and establishing emotional and behavioral regulation, empirically based prevention and intervention approaches in this developmental period have the potential to significantly advance public health.
Acknowledgments
This study was supported by National Institute of Mental Health Grant #R01MH55278 (A. Carter, PI). We also are grateful to our study families; without them this study would not have been possible.
Footnotes
The authors have no conflict of interest to disclose.
Contributor Information
Margaret J. Briggs-Gowan, Department of Psychiatry, University of Connecticut Health Center, Farmington
Julian D. Ford, Department of Psychiatry, University of Connecticut Health Center, Farmington
Lisa Fraleigh, Department of Psychiatry, University of Connecticut Health Center, Farmington.
Kimberly McCarthy, Department of Psychiatry, University of Connecticut Health Center, Farmington.
Alice S. Carter, Department of Psychology, University of Massachusetts-Boston
References
- Abidin RR. Parenting Stress Index Short Form-Test manual. Charlottesville, VA: Pediatric Psychology Press; 1990. [Google Scholar]
- Appleyard K, Egeland B, van Dulmen MH, Sroufe LA. When more is not better: The role of cumulative risk in child behavior outcomes. Journal of Child Psychology and Psychiatry. 2005;46:235–245. doi: 10.1111/j.1469-7610.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting & Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Bogat GA, DeJonghe E, Levendosky AA, Davidson WS, von Eye A. Trauma symptoms among infants exposed to intimate partner violence. Child Abuse and Neglect. 2006;30:109–125. doi: 10.1016/j.chiabu.2005.09.002. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Mancini AD. The human capacity to thrive in the face of potential trauma. Pediatrics. 2008;121:369–375. doi: 10.1542/peds.2007-1648. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Clark R, Augustyn M, McCarthy KJ, Ford J. Exposure to potentially traumatic events in early childhood: Differential links to emergent psychopathology. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2010;51:1132–1140. doi: 10.1111/j.1469-7610.2010.02256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Horwitz SM, Schwab-Stone ME, Leventhal JM, Leaf PJ. Mental health in pediatric settings: Distribution of disorders and factors related to service use. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:841–849. doi: 10.1097/00004583-200007000-00012. [DOI] [PubMed] [Google Scholar]
- Carter AS, Briggs-Gowan MJ. Child Life Events Screener. New Haven, CT: 1998. Unpublished manuscript. [Google Scholar]
- Christoffel KK. Violent death and injury in US children and adolescents. American Journal of Diseases of Children. 1990;144:697–706. doi: 10.1001/archpedi.1990.02150300095025. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64:577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Cunradi CB, Caetano R, Clark C, Schafer J. Neighborhood poverty as a predictor of intimate partner violence among White, Black, and Hispanic couples in the United States: A multilevel analysis. Annals of Epidemiology. 2000;10:297–308. doi: 10.1016/s1047-2797(00)00052-1. [DOI] [PubMed] [Google Scholar]
- Daviss WB, Mooney D, Racusin R, Ford JD, Fleischer A, McHugo GJ. Predicting posttraumatic stress after hospitalization for pediatric injury. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:576–583. doi: 10.1097/00004583-200005000-00011. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Van Dillen T. Childhood post-traumatic stress disorder: An overview. Child and Adolescent Psychiatric Clinics of North America. 2005;14:745–772. doi: 10.1016/j.chc.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Ford JD, Racusin R, Ellis C, Daviss WB, Reiser J, Fleischer ATJ. Child maltreatment, other trauma exposure, and posttraumatic symptomatology among children with oppositional defiant and attention deficit hyperactivity disorders. Child Maltreatment. 2000;5:205–217. doi: 10.1177/1077559500005003001. [DOI] [PubMed] [Google Scholar]
- Ford JD, Stockton P, Kaltman S, Green BL. Disorders of extreme stress (DESNOS) symptoms are associated with type and severity of interpersonal trauma exposure in a sample of healthy young women. Journal of Interpersonal Violence. 2006;21:1399–1416. doi: 10.1177/0886260506292992. [DOI] [PubMed] [Google Scholar]
- Heim C, Plotsky PM, Nemeroff CB. Importance of studying the contributions of early adverse experience to neurobiological findings in depression. Neuropsychopharmacology. 2004;29:641–648. doi: 10.1038/sj.npp.1300397. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Knickerbocker L, Heyman RE, Slep AM, Jouriles EN, McDonald R. Co-occurrence of child and partner maltreatment: Definitions, prevalence, theory, and implications for assessment. European Psychologist. 2007;12:36–44. [Google Scholar]
- Lahey BB, Flagg EW, Bird HR, Schwab-Stone ME, Canino G, Dulcan MK, et al. The NIMH Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) Study: Background and methodology. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:855–864. doi: 10.1097/00004583-199607000-00011. [DOI] [PubMed] [Google Scholar]
- Margolin G, Gordis EB. The effects of family and community violence on children. Annual Review of Psychology. 2000;51:445–479. doi: 10.1146/annurev.psych.51.1.445. [DOI] [PubMed] [Google Scholar]
- Meiser-Stedman R, Smith P, Glucksman E, Yule W, Dalgleish T. The posttraumatic stress disorder diagnosis in preschool- and elementary school-age children exposed to motor vehicle accidents. American Journal of Psychiatry. 2008;165:1326–1337. doi: 10.1176/appi.ajp.2008.07081282. [DOI] [PubMed] [Google Scholar]
- Myers JK, Weissman MM. Use of a self-report symptom scale to detect depression in a community sample. American Journal of Psychiatry. 1980;137:1081–1084. doi: 10.1176/ajp.137.9.1081. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general popuation. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Scheeringa MS. Posttraumatic stress disorder. In: Zeanah CH, editor. Handbook of infant mental health. 3rd. New York: Guilford Press; 2009. pp. 345–361. [Google Scholar]
- Scheidt PC, Harel Y, Trumble AC, Jones DH, Overpeck MD, Bijur PE. The epidemiology of nonfatal injuries among US children and youth. American Journal of Public Health. 1995;85:932–938. doi: 10.2105/ajph.85.7.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS Social support survey. Social Science & Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Slep AM, O’Leary SG. Parent and partner violence in families with young children: Rates, patterns, and connections. Journal of Consulting and Clinical Psychology. 2005;73:435–444. doi: 10.1037/0022-006X.73.3.435. [DOI] [PubMed] [Google Scholar]
- Stoddard FJ, Ronfeldt H, Kagan J, Drake JE, Snidman N, Murphy JM, et al. Young burned children: The course of acute stress and physiological and behavioral responses. American Journal of Psychiatry. 2006;163:1084–1090. doi: 10.1176/ajp.2006.163.6.1084. [DOI] [PubMed] [Google Scholar]
- Taylor L, Zuckerman B, Harik V, Groves BM. Witnessing violence by young children and their mothers. Journal of Developmental and Behavioral Pediatrics. 1994;15:120–123. [PubMed] [Google Scholar]
- Teicher MH, Tomoda A, Andersen SL. Neurobiological consequences of early stress and childhood maltreatment: Are results from human and animal studies comparable? Annals of the New York Academy of Sciences. 2006;1071:313–323. doi: 10.1196/annals.1364.024. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. American Community Survey. 2006–2008 Retrieved Febraury 23, 2010, from http://factfinder.census.gov.
- Zeanah CH, editor. Handbook of infant mental health. 2nd. New York: Guilford Press; 2000. [Google Scholar]
- Zero to Three, National Center for Infants, Toddlers, and Families. Diagnostic classification: 0-3. Diagnostic classification of mental health and developmental disorders in infancy and early childhood. Washington, DC: Zero to Three Press; 1994. [Google Scholar]


