Abstract
Introduction:
The benefits of treating subclinical hypothyroidism are currently under debate, prevention of adverse cardiac events purporting to be one of the main benefits. The effect of subclinical hypothyroidism on the cardiovascular health of the Indian sub-population is largely unknown. This study was designed to examine these effects and to help guide treatment of this disorder.
Methods:
A cross-sectional adult population survey was carried out in urban coastal area of central Kerala. 986 volunteers underwent complete biochemical and physical examinations, 110 were found to have subclinical hypothyroidism (8.9%). The ten-year risk of an adverse cardiac event, was calculated using the Framingham score algorithm. Eligible subclinical hypothyroid subjects (N = 110) and a randomly selected, age and gender matched control group (N = 220) were compared.
Results:
This population was found to have high baseline levels of diabetes 19.5%, hypercholesterolemia 57.2% and systolic hypertension 24.6%. No association was found between subclinical hypothyroid status or rising TSH and Framingham 10-year risk. While no difference between groups was noted with respect to lipid profile, a rising TSH was found to be significantly correlated with mild worsening of the lipid profile. A significant positive correlation was found between skinfold thickness and TSH.
Conclusions:
Subclinical hypothyroidism is not a contributing factor to elevated Framingham risk in this population, and while a mild effect was observed on the lipid profile, its effect is unlikely to be clinically relevant. We hypothesize that in this population a genetic component may be responsible for the uniquely high rates of metabolic syndrome and other endocrine diseases.
Keywords: Atherosclerosis, cardiovascular diseases, dyslipidemia, hypothyroidism, India, thyroid gland
INTRODUCTION
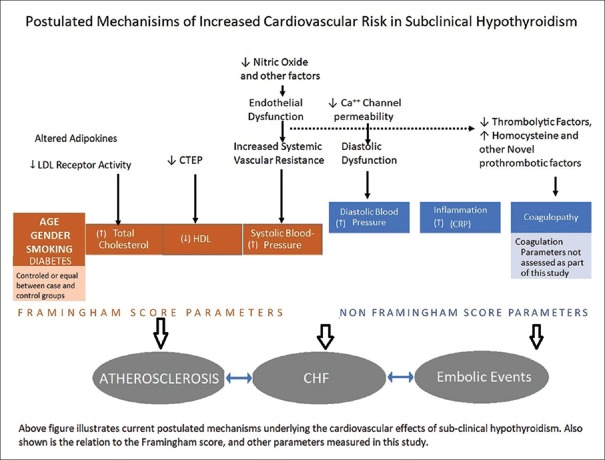
Disorders of the thyroid, both diverse and increasingly common, affect several aspects of health, including major detrimental effects on the cardiovascular system, such as the lipid profile and blood pressures. Cardiovascular disease accounts for the largest share of mortality in developed nations and increasingly in developing countries. Numerous studies have shown the negative effect of overt hypothyroidism on factors contributing to cardiac health such as, body mass index (BMI), lipid profile, blood pressures, endothelial function, and left ventricular function [Figure 1].[1] Most large studies show the prevalence of subclinical hypothyroidism at 5–10 times[2,3,4] that of overt hypothyroidism and yet less is known about this disorder of often protean manifestations, of note is the lack of consensus regarding its implications on cardiovascular health.
Figure 1.
Postulated mechanisms of cardiovascular effects of subclinical hypothyroidism and its relation to study design
The state of Kerala in Southern India has undergone rapid economic, social, and cultural development in the last 20 years. Westernization of diets and increase in sedentary work along with other lifestyle shifts are possibly responsible for its current epidemic of lifestyle diseases, the prevalence of cardiovascular disease being comparable to or exceeding Western countries.[5] Further adding to the cardiovascular burden of this population is the high prevalence of type two diabetes in this population (19.5% vs. 9.3% in the US) highlighting the effect of probable environmental and genetic factors.[6] Furthermore, in data previously published by this group, Kerala has been documented to have a much higher prevalence of thyroid conditions than elsewhere (around 10%), despite being an iodine-sufficient population,[7] population data from the United Kingdom, in the Wickham Study showed a prevalence of around 4%. High background radiation due to thorium-containing monazite sands or high intake of cyanogenic glycosides found in local tapioca crops are often proposed as explanations; however, scientific data supporting these hypotheses are scant.
The Framingham risk score is one of the most widely used tools in estimating cardiovascular risk. A revised score calculator has been prepared by D’Agostino et al. and is used to calculate the person's 10-year risk percentage based on the risk factors and standard physical and biochemical measurements.[8] Parameters include the patients age, gender, systolic blood pressure, total cholesterol, high-density lipoprotein (HDL) cholesterol, use of hypertensive medication, tobacco, and a diagnosis of diabetes. While studies have shown the impact of hypothyroidism on cardiovascular health, sparse data exists regarding subclinical hypothyroidism and the risk score, and consensus has been difficult to achieve regarding the implications of its overall cardiovascular effects. It is noted that while, the risk score per se is not validated in the subclinical hypothyroid population, its individual parameters are precisely those which are hypothesized to contribute the most to the excess cardiac morbidity and mortality.
Subclinical hypothyroidism is postulated to affect the Cardiovascular system in several ways [Figure 1]. Perturbation of the lipid profile is thought to be due to effects of an altered adipokine profile on low-density lipoprotein (LDL) receptor affinity and lifespan, and inadequate T3-mediated signaling leading to lower levels of cholesterol ester transfer protein which is responsible for LDL to HDL conversion.[9] Decreased nitric oxide production and sensitivity of vascular endothelial cells, along with decreased thermogenesis, are thought to be partly responsible for the elevated systemic vascular resistance seen. Those factors along with altered myocyte intracellular calcium handling leading to cardiac diastolic dysfunction are postulated to be responsible for the increased morbidity due to congestive heart failure seen.[10] Endothelial dysfunction along with altered pro/anticoagulant factors are considered most likely to be the cause of increased risk of embolic events.
Western studies such as those done by Rodondi et al.have shown a slight increase in cardiac morbidly and mortality associated with subclinical hypothyroidism;[11] however, other studies, such as those focusing on the elderly have disagreed.[12] A large majority of Western studies have shown an elevation in total cholesterol and triglycerides.[13] However, regarding Asian populations, literature is lacking, and available literature has not come to a consensus regarding the impact if any on cardiovascular health profile. Several studies, for example, Choi JK et al. in Korea[14] and several studies from the Indian subcontinent show lack and presence of[15,16,17] negative impacts on cardiac health.
Given an apparent genetic susceptibility to coronary heart disease in the South Asian population,[18] and the uniquely high rates of thyroid disease in Kerala, this begs the question, whether subclinical hypothyroidism is a significant contributing factor to the high rates of cardiovascular morbidity in this community? Could subclinical hypothyroidism represent a new modifiable risk factor for cardiac disease? The present study is conducted as part of the community-based Amrita Diabetes and Endocrine Population Survey (ADEPS). Its intent being to investigate the effect of endocrine and metabolic factors on the community health of Kerala, here particularly to evaluate the effect of subclinical hypothyroidism on the cardiovascular health this population.
MATERIALS AND METHODS
Data collection
The data used was obtained as part of the ADEPS, which was conducted in three randomly selected areas of the Ernakulam district of Kerala. Data was obtained from community-dwelling volunteers. The aim of the study is to investigate both diabetes and endocrine conditions, the ideal sample size was estimated based on an expected prevalence of 4% for endocrine conditions; thus, a sample size of 3000 was required to have a type 1 error of 0.05 and allowable error around of 20%. Wards were considered as the primary sampling focus and were sampled using cluster sampling as per the WHO methodology. Fifty clusters of 7 houses each were visited, and at the end of the first phase, 931 houses and 3069 adults had been logged.
Ultimately 32% of the population who underwent the survey participated in further workup. The demographic profile of the second phase was generally similar to those in the first phase, with a slight skew to older age. Investigations in the second phase included physical evaluation and biochemical investigations. A medical doctor verified medical history and performed physical examinations. Biochemical investigations included glucose tolerance tests, plasma glucose, thyroid function tests, lipid profile, electrolyte measurements, and blood counts, along with a host of other metabolic tests including liver function tests, urea, and creatinine estimation.
Definitions and tools
We defined subclinical hypothyroidism as a thyroid-stimulating hormone (TSH) level of ≥4.2 uIU/ml and free T4 between 1.8 ng/ml and 0.8 ng/ml. Diabetes was defined per the current WHO Criteria of fasting glucose greater than 126 mg/dl and 2 h postprandial of more than 200 mg/dl. Persons with blood sugars within normal range but on medication for diabetes were also considered as diabetic. Hypertension was defined as a sitting systolic blood pressure of ≥140 mm/Hg and/or diastolic >90 mm/Hg. Hypercholesterolemia was defined as fasting serum total cholesterol of >200 mg/dl.
The 2011 Framingham cardiovascular risk scoring system as set out by D’Agostino et al. was used for analyzing the cardiovascular risk in persons between 30 and 75 years of age. The 10-year risk score of the patient was received as the outcome from the algorithm.
Methodology
Our case group consisted of 110 eligible subclinical hypothyroid patients, who satisfied our definition of biochemical evidence of subclinical hypothyroidism. Exclusion criteria included treatment for hypothyroidism, history of previous thyroid conditions, and pregnancy. An age and gender-matched control group (n = 220) was created from randomly selected patients with normal thyroid function tests. Framingham score was calculated from persons who had all data points required.
Statistical analysis of the data was done using SPSS version 16 (IBM analytics, Armonk, New York, USA). Students t- test was used to compare means between the case and control groups. Correlation analysis was performed to determine the “r” values of the association between rising TSH on the parameters of cardiac health. The analysis was repeated on several subgroups, including our nondiabetic cases and matched controls, and men and women separately. P < 0.05 was taken as statistically significant.
RESULTS
Overview of study group
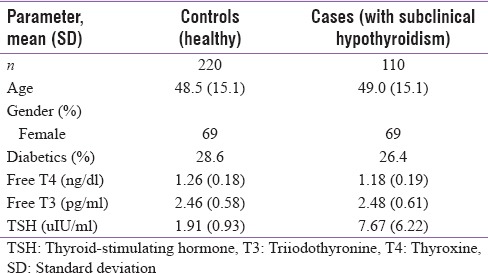
As shown in Table 1, our study group contained 110 subclinical hypothyroid with a TSH range from 4.2 uIU/L to 35.10 uIU/. Our randomly selected euthyroid control group consisted of 220 persons with a TSH range from 0.28 to 4.16 uIU/L. Our case group consisted of 13 persons with “severe subclinical hypothyroidism,” i.e., a TSH ≥10 uIU/ml. Our case group had a 26.4% prevalence of Type 2 diabetes and our controls had a 28.6%, the mean fasting blood sugar being 85.89 mg/dl (standard deviation [SD] 14.0) in our cases and 86.5 mg/dl (SD 11.7) in our controls. The percentage of self-reported current smokers was nearly the same in both case and controls groups at 4.5% and 4.1%, respectively. An analysis of our total population sample (N = 986) revealed the prevalence of cardiovascular risk factors as follows: diabetes 19.5%, hypercholesterolemia 57.2%, and hypertension 24.6%.
Table 1.
Overview of study groups
Intergroup analysis
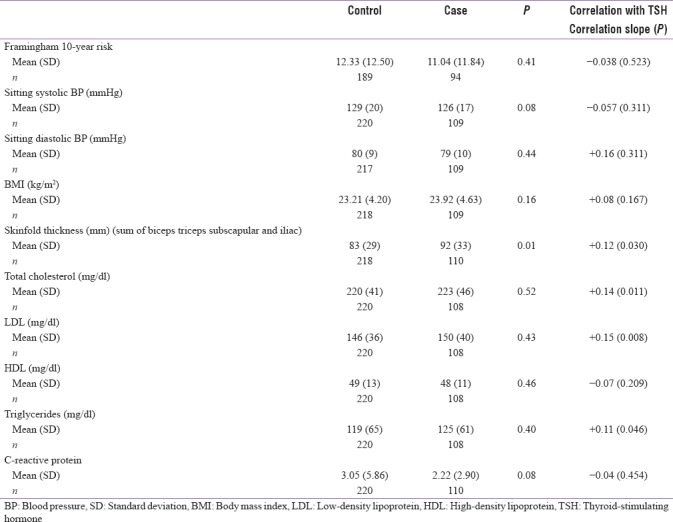
No statistically significant difference was found in the Framingham scores between the two groups [Table 2]. However, a statistical difference was found in the skinfold thickness, the cases having nearly 10 mm higher sum of skinfold thickness. Contrary to our expectations, our group of subclinical hypothyroid patients had lower systolic blood pressure and lower CRP although these last two observations are only approaching statistical significance.
Table 2.
Group and correlation analysis of cardiac risk factors
The same test was repeated individually with males only, females only, and nondiabetics only. In the females-only analysis, largely similar results were obtained, the only statistically significant finding being a difference in the skinfold thickness (P = 0.039). In the males-only analysis, no statistical significance was found between the groups. The P value of the association between skinfold thickness and group was 0.125. In the nondiabetic subgroup, the effect on both skinfold thickness was marginal with a P = 0.068; however, the effect on the C-reactive protein (CRP) levels became more significant with P = 0.018. We would have liked to repeat analysis on cases with TSH >10; however, our numbers were too small to make this statistically feasible.
Correlation of parameters with thyroid-stimulating hormone
In Table 2, we have analyzed the effect of a rising TSH on the parameters with correlation analysis. Again, no effect was seen on the overall Framingham 10-year risk score. However, further analysis on the lipid profile reveals a statistically significant correlation between rising TSH with LDL cholesterol, total cholesterol, and triglyceride levels. Correlation between TSH and skinfold thickness was also positive. No effect was seen with the blood pressures, BMI, or serological markers such as CRP or uric acid.
Thyroid-stimulating hormone stratified analysis of lipid profile data
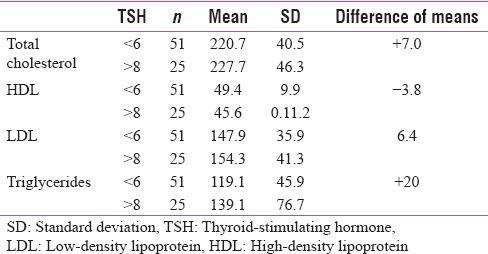
We further subdivided our subclinical hypothyroid cases based on its TSH into two groups TSH <6 and TSH >8 [Table 3], the groups while being largely demographically similar showed the same trends as were seen in the continuous TSH analysis; however, we draw highlight to the magnitude of the difference between the parameters at the upper and lower levels of TSH here.
Table 3.
Thyroid-stimulating hormone stratified analysis
DISCUSSION
Cardiovascular diseases account for the largest single share of morbidity among developed nations, and many developing nations including India. By combating modifiable risk factors through primary prevention, the burden of cardiovascular disease can be reduced. South Asians are known to be at increased risk for atherosclerosis even with comparable risk factor profile to Western counterparts.[19] Our population perhaps as a manifestation of these presumed genetic factors has an elevated baseline risk profile with high rates of diabetes, hypercholesterolemia, and hypertension. Our data fails to show any significant Framingham 10-year risk difference between our subclinical hypothyroid population and our controls. Existing data from the Indian subcontinent have generally shown a trend toward increased risk in the form of deranged lipid profile, elevated diastolic blood pressure, and elevated CRP.[15,16,17] The current American Academy of Clinical Endocrinology consensus statements propose that only a TSH greater than 10 uIU/ml is an indication for treatment in view of possible elevated cardiovascular risk and higher risk of progression to overt hypothyroidism.[20] Given our results, we feel that this consensus holds true in this population also.
Other contrasting results include lack of elevation in the diastolic blood pressure in subclinical hypothyroid cases which is contrary to Sharma et al.'s findings. Interestingly, we have also found a mild negative correlation between the CRP and TSH, notably this association was strongest in our nondiabetic population who had lower baseline CRP. This was surprising, as most studies show elevated inflammatory markers in hypothyroidism,[21,22] and as far as we are aware this is the first such documentation of lower CRP in a subclinical versus a normal group.
Our data does highlight a significant difference in skinfold thickness between the populations, and a positive effect of rising TSH on skinfold thickness; however, no effect on the BMI or on the waist circumference has been noted. Other studies on the Asian population such as Sridevi et al. have controlled for BMI between their groups or have found no significant effect between groups.[15,16,17] Statistically significant positive correlations were noted between TSH and LDL cholesterol, total cholesterol, and triglycerides. Similar results have been reported in various other studies. However, the difference of the means of LDL, and triglycerides between individuals in the lower and upper ranges of TSH was negligible [Table 3]. While a trend with rising TSH was observed, it is interesting to note the lack of any significance when comparing between our two groups. This is likely due to the weak effect, and small effective range of TSH in the population. Hence, we presume that these effects may not be clinically relevant in this population with deranged baseline lipid profile.
While differences in lifestyle and diet may explain the differences between our population and other Indian populations, they would fail to explain the differences seen between populations of the United States and Europe with our sample group. The unique endocrine environment here consists of some of the world's highest rates of hypothyroidism (despite being iodine sufficient) and diabetes. Hormone-receptor polymorphisms and polymorphisms in subcellular receptors have been associated with population-wide increased risk for disease. For example, polymorphisms of the glucocorticoid receptor are associated with obesity and metabolic syndrome.[23] Polymorphisms in the TSHα receptor have been associated with obesity and elevated cholesterol in certain lineages while polymorphisms in the TSHβ receptor have been associated with elevations in TSH due to impaired negative feedback.[24,25] Further research into genetic mechanisms behind the poor cardiovascular profile and the increased incidence of diabetes and thyroid disorders would be beneficial in this population.
CONCLUSION
We conclude with the inference that, in this population with elevated baseline cardiac risk and unique environmental and perhaps genetic factors, subclinical hypothyroidism, particularly with TSH <10 uIU/ml, does not significantly contribute to cardiovascular risk. Negative effects on the lipid profile and skinfold thickness were observed; however, the relationships while statistically significant were weak. Given our somewhat population specific findings, especially regarding lower CRP levels in our cases versus controls, we feel further investigation of the endocrine milieu would uncover novel insights into the pathogenesis of this disputed subject.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Authors would like to thank Allison Gilchrist, Research Nurse for her help in data collection, and database consolidation.
REFERENCES
- 1.Biondi B, Klein I. Hypothyroidism as a risk factor for cardiovascular disease. Endocrine. 2004;24:1–3. doi: 10.1385/ENDO:24:1:001. [DOI] [PubMed] [Google Scholar]
- 2.Hennessey JV, Espaillat R. Subclinical hypothyroidism: A historical view and shifting prevalence. Int J Clin Pract. 2015;69:771–82. doi: 10.1111/ijcp.12619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Razvi S, Weaver JU, Vanderpump MP, Pearce SH. The incidence of ischemic heart disease and mortality in people with subclinical hypothyroidism: Reanalysis of the Whickham survey cohort. J Clin Endocrinol Metab. 2010;95:1734–40. doi: 10.1210/jc.2009-1749. [DOI] [PubMed] [Google Scholar]
- 4.Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000;160:526–34. doi: 10.1001/archinte.160.4.526. [DOI] [PubMed] [Google Scholar]
- 5.Soman CR, Kutty VR, Safraj S, Vijayakumar K, Rajamohanan K, Ajayan K, et al. All-cause mortality and cardiovascular mortality in Kerala state of India: Results from a 5-year follow-up of 161,942 rural community dwelling adults. Asia Pac J Public Health. 2011;23:896–903. doi: 10.1177/1010539510365100. [DOI] [PubMed] [Google Scholar]
- 6.Menon VU, Kumar KV, Gilchrist A, Sugathan TN, Sundaram KR, Nair V, et al. Prevalence of known and undetected diabetes and associated risk factors in central Kerala – ADEPS. Diabetes Res Clin Pract. 2006;74:289–94. doi: 10.1016/j.diabres.2006.03.025. [DOI] [PubMed] [Google Scholar]
- 7.Usha Menon V, Sundaram KR, Unnikrishnan AG, Jayakumar RV, Nair V, Kumar H, et al. High prevalence of undetected thyroid disorders in an iodine sufficient adult South Indian population. J Indian Med Assoc. 2009;107:72–7. [PubMed] [Google Scholar]
- 8.D’Agostino RB, Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: The Framingham heart study. Circulation. 2008;117:743–53. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 9.Rizos CV, Elisaf MS, Liberopoulos EN. Effects of thyroid dysfunction on lipid profile. Open Cardiovasc Med J. 2011;5:76–84. doi: 10.2174/1874192401105010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Biondi B, Cooper DS. The clinical significance of subclinical thyroid dysfunction. Endocr Rev. 2008;29:76–131. doi: 10.1210/er.2006-0043. [DOI] [PubMed] [Google Scholar]
- 11.Rodondi N, den Elzen WP, Bauer DC, Cappola AR, Razvi S, Walsh JP, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA. 2010;304:1365–74. doi: 10.1001/jama.2010.1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atzmon G, Barzilai N, Surks MI, Gabriely I. Genetic predisposition to elevated serum thyrotropin is associated with exceptional longevity. J Clin Endocrinol Metab. 2009;94:4768–75. doi: 10.1210/jc.2009-0808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kvetny J, Heldgaard PE, Bladbjerg EM, Gram J. Subclinical hypothyroidism is associated with a low-grade inflammation, increased triglyceride levels and predicts cardiovascular disease in males below 50 years. Clin Endocrinol (Oxf) 2004;61:232–8. doi: 10.1111/j.1365-2265.2004.02088.x. [DOI] [PubMed] [Google Scholar]
- 14.Choi JK, Kim JS, Hwang CH, Kim DH, Hwang SW, Cho B, et al. Subclinical hypothyroidism and coronary risk factors in women above 55 years. J Korean Acad Fam Med. 2002;23:96–103. [Google Scholar]
- 15.Rajendra K, Khatiwada S, Deo Mehta K, Pandey P, Lamsal M, Majhi S, et al. Cardiovascular risk factors in subclinical hypothyroidism: A case control study in Nepalese population. J Thyroid Res 2015. 2015 doi: 10.1155/2015/305241. 305241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sridevi A, Vivekanand B, Giridhar G, Mythili A, Subrahmanyan KA. Insulin resistance and lipid alterations in subclinical hypothyroidism. Indian J Endocrinol Metab. 2012;16:S345–6. doi: 10.4103/2230-8210.104085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharma R, Sharma TK, Kaushik GG, Sharma S, Vardey SK, Sinha M, et al. Subclinical hypothyroidism and its association with cardiovascular risk factors. Clin Lab. 2011;57:719–24. [PubMed] [Google Scholar]
- 18.Bhalodkar NC, Blum S, Rana T, Kitchappa R, Bhalodkar AN, Enas EA, et al. Comparison of high-density and low-density lipoprotein cholesterol subclasses and sizes in Asian Indian women with Caucasian women from the Framingham offspring study. Clin Cardiol. 2005;28:247–51. doi: 10.1002/clc.4960280510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anand SS, Yusuf S, Vuksan V, Devanesen S, Teo KK, Montague PA, et al. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: The Study of Health Assessment and Risk in Ethnic Groups (SHARE) Lancet. 2000;356:279–84. doi: 10.1016/s0140-6736(00)02502-2. [DOI] [PubMed] [Google Scholar]
- 20.Garber J, Cobin R, Gharib H, Hennessey J, Klein I, Mechanick J. 10- Clinical Practice Guidelines for Hypothyroidism in Adults: Cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. The American Association of Clinical Endocrinologists. 2012. [Last accessed on 2017 Mar 23]. Available from: https://www.aace.com/files/final-file-hypo-guidelines.pdf . [DOI] [PubMed]
- 21.Tuzcu A, Bahceci M, Gokalp D, Tuzun Y, Gunes K. Subclinical hypothyroidism may be associated with elevated high-sensitive c-reactive protein (low grade inflammation) and fasting hyperinsulinemia. Endocr J. 2005;52:89–94. doi: 10.1507/endocrj.52.89. [DOI] [PubMed] [Google Scholar]
- 22.Gupta G, Sharma P, Kumar P, Itagappa M. Study on subclinical hypothyroidism and its association with various inflammatory markers. J Clin Diagn Res. 2015;9:BC04–6. doi: 10.7860/JCDR/2015/14640.6806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chrousos GP. The role of stress and the hypothalamic-pituitary-adrenal axis in the pathogenesis of the metabolic syndrome: Neuro-endocrine and target tissue-related causes. Int J Obes Relat Metab Disord. 2000;24(Suppl 2):S50–5. doi: 10.1038/sj.ijo.0801278. [DOI] [PubMed] [Google Scholar]
- 24.Shin DJ, Osborne TF. Thyroid hormone regulation and cholesterol metabolism are connected through sterol regulatory element-binding protein-2 (SREBP-2) J Biol Chem. 2003;278:34114–8. doi: 10.1074/jbc.M305417200. [DOI] [PubMed] [Google Scholar]
- 25.Mullur R, Liu YY, Brent GA. Thyroid hormone regulation of metabolism. Physiol Rev. 2014;94:355–82. doi: 10.1152/physrev.00030.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]