Abstract
Congenital hypothyroidism remains one of the most common preventable causes of mental retardation among children. Screening for congenital hypothyroidism remains one of the most cost-effective tools to prevent mental retardation in the population. Umbilical cord blood thyroid-stimulating hormone (TSH) levels remain an attractive and a practical step for screening for congenital hypothyroidism. The aims of this study were as follows: (1) to find normative values of cord blood TSH for the study group and (2) to use cord blood TSH levels as a marker for screening of congenital hypothyroidism. Cord blood of 1824 neonates who were of term gestation, weighed >2.5 kg at birth, whose mothers were off thyroid medication were a part of the study group. Umbilical cord blood was collected at the time of delivery and TSH was estimated. All babies who had a cord blood TSH value of >20 mIU/L were called bay on day 7 of life for a full thyroid profile. Cord blood samples of 1824 neonates were tested for TSH. Male–female ratio was 979:845 = 1.15:1. The birth weights ranged between 2.5 and 4.5 kg with an average birth weight of 2.811 kg. Mean (standard deviation) TSH value was 7.725 (8.99). TSH values ranged between 1.2 and 100 mIU/ml. TSH values corresponding to the 3rd, 10th, 25th, 50th, 90th, 95th, and 97th percentile were 2.32, 4.05, 5.67, 7.5, 12, 20.63, and 30.88, respectively. Out of the 88 babies recalled for repeat testing, 80 babies only turned up; eventually one turned out to be hypothyroid on repeat testing. The incidence of congenital hypothyroidism in our study was 1 in 1824. To conclude, we can safely use a cutoff of cord blood TSH value of >20 mIU/L for the purpose of screening for congenital hypothyroidism. For logistic angles, a higher cutoff of >30 mIU/L can be used. Large population-based studies are required to establish normative values for cord blood TSH in our country.
Keywords: Cord blood, Hypothyroidism, TSH
INTRODUCTION
Congenital hypothyroidism is one of the most common preventable causes of mental retardation in the country. It has an incidence of 1 in 4000 births in various neonatal screening programs.[1] Screening for congenital hypothyroidism remains one of the most cost-effective tools in preventing mental retardation in the population. Neonatal screening programs for congenital hypothyroidism are widespread in developed countries, but unfortunately such a nationwide program is nonexistent in our country. Ideally, universal screening at 3–4 days should be done for detection of congenital hypothyroidism but with babies being discharged early, and the absence of a supportive follow-up system has lead cord blood thyroid-stimulating hormone (TSH) levels being used as a screening marker for detection of congenital hypothyroidism.[2] Various Asian countries have started using cord blood samples for screening of congenital hypothyroidism.[3,4,5,6] Very few studies on cord blood TSH values are available in the Indian literature.[7] This study was conducted to find normative values of TSH in cord blood samples and to use cord blood TSH value as a screening marker for congenital hypothyroidism.
Aim
The aims of this study were as follows:
To find normative values of cord blood TSH for the study group
To use cord blood TSH as a marker for screening of congenital hypothyroidism.
MATERIALS AND METHODS
The study was carried out from October 2013 to October 2017 in a private medical college in India. All consecutive deliveries conducted during this period were part of the study. All the deliveries were attended by either of the two authors.
Blood samples were collected in a sterile container drawn from 15 to 20 cm length of umbilical cord incised during the time of birth of a baby. The sample obtained was a mixed sample which contained blood from both umbilical artery and umbilical vein. Babies who were born premature, weighed <2.5 kg at birth, required resuscitation, whose mothers were on thyroid medications were excluded from the study.
Detailed antenatal history, parity, medical history, thyroid status, and community were recorded on a predesigned pro forma. Details of the baby were recorded on a separate pro forma. TSH was estimated within 24 h by chemiluminescence immunoassay (kit supplied by Roche E411). Cord blood samples of 1824 neonates were subjected to TSH estimation. Totally 1824 neonates formed the study group. All those neonates who had a cord blood TSH value of <20 mIu/ml were called back on day 7 of life for a full thyroid profile including TSH, T3, T4, fT3, and fT4.
RESULTS
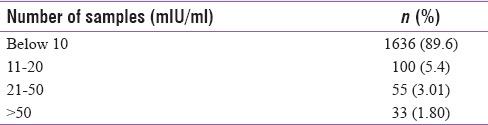
Cord blood samples of 1824 neonates were tested for TSH. Male-female ratio was 979:845 = 1.15:1. The birth weights ranged between 2.5 and 4.5 kg, with an average birth weight of 2.811 kg [Table 1]. Mean (standard deviation) TSH value was 7.725 (8.99) among the study group. Table 2 depicts the TSH values of the entire cohort. TSH values ranged between 1.2 and 100 mIU/ml. TSH values corresponding to 3rd, 10th, 25th, 50th, 90th, 95th, and 97th percentile were 2.32, 4.05, 5.67, 7.5, 12, 20.63, and 30.88, respectively. Among the 88 patients recalled for repeat sampling, eighty turned up and eight were lost to follow-up. One neonate finally proved to be hypothyroid on repeat workup. The cord blood TSH in the baby who eventually turned out to be hypothyroid was 100 mIU/ml.
Table 1.
Weight-wise distribution of the study group
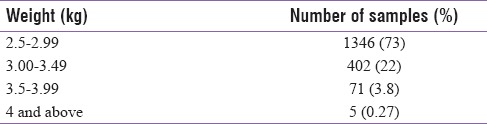
Table 2.
Umbilical cord blood thyroid-stimulating hormone values (n=1824)
DISCUSSION
Screening for congenital hypothyroidism is the need of the hour.[8] Unfortunately, it has not been implemented in India on a nationwide basis due to lack of available facilities, lack of awareness among treating physicians, cost, and early discharge of neonates due to overburden in the government setups. The use of cord blood TSH as a screening tool for congenital hypothyroidism remains a practical option due to its ease of availability, simplicity, and accessibility. Studies across the world have shown that cord blood remains a good sampling technique for screening of congenital hypothyroidism. Our results show that 10% samples had a cord blood TSH value >10 mIu/ml, which is slightly higher as compared to that reported by Mekennon et al. and Manglik et al.[2,9] Our mean TSH value was 7.725 mIU/L, which is quite comparable to other studies. Our recall rate for repeat testing was 4.8% which is somewhat higher as compared to 2.27% reported by Wu et al., who had a large cohort of 11,000 neonates.[6] There is wide variation in the normal cord blood TSH values which can vary from 1 to 38.9 mIU/L.[9] We have used a cutoff of 20 mIU/L, which has also been used in studies across the world. Had we used a cutoff of 30 mIU/L, our recall rate would have fallen to 3%, and on further increasing the cutoff value to 40 mIU/L, the recall rate would have fallen to 2%. Considering our annual birth rate of 20 million babies and a recall rate of 4.8%, almost 960,000 babies would need to be called back for a repeat thyroid profile. It would be a herculean task in our country. Higher cutoff values of TSH for recall would lead to lesser babies being called for repeat testing, thereby decreasing the economic and logistic burden on the existing health-care facilities.
We had one baby with congenital hypothyroidism in a cohort of 1824 giving us an incidence of 1 in 1824. Various studies from across India have reported the incidence of congenital hypothyroidism as varied as between 1 in 248 and 1 in 1700.[10,11] Geographic, ethnic differences are responsible for this wide variation in incidence, and a cohort size of 1824 samples is too less to assess incidence.
Our figures have shown a comparable trend with the normative data for cord blood TSH values as reported by various workers across the globe.
The biggest drawback of our study is the small sample size. Large population-based studies are required to gauge and calculate the incidence of congenital hypothyroidism in our country.
CONCLUSION
We can safely use a cutoff of cord blood TSH value of >20 mIU/L for the purpose of screening for congenital hypothyroidism. For logistic angles, a higher cutoff of >30 mIU/L can be used. Large population-based studies are required to establish normative values for cord blood TSH in our country.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors are grateful to Dr. Onjal Tayade, Asst. Professor, Department of Biochemistry, Pacific Medical College, for his help in bringing out this manuscript.
REFERENCES
- 1.Lafranchi S. Hypothyroidism. In: Behrman RE, Kleigman RM, Jenson HB, editors. Nelson Textbook of Pediatrics. 17th ed. Philadelphia: Saunders; 2004. pp. 1872–9. [Google Scholar]
- 2.Manglik AK, Chatterjee N, Ghosh G. Umbilical cord blood TSH levels in term neonates: A screening tool for congenital hypothyroidism. Indian Pediatr. 2005;42:1029–32. [PubMed] [Google Scholar]
- 3.Fagela-Domingo C, Padilla CD, Cutiongco EM. Screening for congenital hypothyroidism (CH) among Filipino newborn infants. Philippine newborn screening study group. Southeast Asian J Trop Med Public Health. 1999;30(Suppl 2):20–2. [PubMed] [Google Scholar]
- 4.Azizi F, Oladi B, Nafarabadi M, Hajipur R. Screening for congenital hypothyroidism in Tehran; The effect of iodine deficiency on transient elevation of TSH in neonates. J Fac Med SBUMS. 1993;18:34–8. [Google Scholar]
- 5.Ordookhani A, Mirmiran P, Najafi R, Hedayati M, Azizi F. Congenital hypothyroidism in Iran. Indian J Pediatr. 2003;70:625–8. doi: 10.1007/BF02724251. [DOI] [PubMed] [Google Scholar]
- 6.Wu LL, Sazali BS, Adeeb N, Khalid BA. Congenital hypothyroid screening using cord blood TSH. Singapore Med J. 1999;40:23–6. [PubMed] [Google Scholar]
- 7.Desai MP, Colaco MP, Ajgaonkar AR, Mahadik CV, Vas FE, Rege C, et al. Neonatal screening for congenital hypothyroidism in a developing country: Problems and strategies. Indian J Pediatr. 1987;54:571–81. doi: 10.1007/BF02749056. [DOI] [PubMed] [Google Scholar]
- 8.Behrman RE, Kleigman RM, Jenson HB, editors. Nelson Textbook of Pediatrics. 17th ed. Philadelphia: Saunders; 2004. p. 2412. [Google Scholar]
- 9.Mekennon Y, Gizachew WH, Chamiso B, Raue F. Thyroid stimulating hormone values in cord blood in neonates. Ethiop J Health Dev. 2003;17:125–30. [Google Scholar]
- 10.Khadilkar V, Khadilkar A, Cowasji H. Neonatal thyroid screening program using filter paper method. Cape News. 2002;6:1. [Google Scholar]
- 11.Rama Devi AR, Naushad SM. Newborn screening in India. Indian J Pediatr. 2004;71:157–60. doi: 10.1007/BF02723099. [DOI] [PubMed] [Google Scholar]


