Abstract
Persistent or chronic pain is the primary reason people seek medical care, yet current therapies are either inadequate for certain types of pain or cause intolerable side effects. Recently, pain neurobiologists have identified a number of cellular and molecular processes that lead to the initiation and maintenance of pain. Understanding these underlying mechanisms has given significant promise for the development of more effective, more specific pain therapies in the near future.
Persistent Pain Is a Major Public Health Problem Today
Over one-third of the world's population suffers from persistent or recurrent pain, costing the American public alone approximately $100 billion each year in health care, compensation, and litigation (1). Chronic pain is associated with conditions such as back injury, migraine headaches, arthritis, herpes zoster, diabetic neuropathy, temporomandibular joint syndrome, and cancer. Many of the currently available pain therapies are either inadequate or cause uncomfortable to deleterious side effects. Chronic pain results not just from the physical insult but also from a combination of physical, emotional, psychological, and social abnormalities. Because many pains persist after an insult is healed, the ongoing pain rather than the injury underlies the patient's disability. Untreated pain may become self-perpetuating because pain has immunosuppressive effects that leave patients susceptible to subsequent diseases. It is now clear that if we can effectively treat the pain despite the underlying cause, it will be possible for patients to regain normal functioning. The key to more successful pain treatment is to understand the mechanisms that generate and maintain chronic pain.
Why Is Pain a New Frontier of Science?
The onset of the 21st century is an incredibly exciting time in pain biology. Information from recent studies in basic pain research is virtually exploding and has revealed numerous novel targets for the advent of new pain therapies. Major advances have occurred at levels spanning from molecular studies that have identified transduction proteins in nociceptors to cortical imaging studies which reveal how pain is experienced on a cognitive level (2, 3). Two key lines of discovery have been (i) molecular/cellular transduction mechanisms and (ii) neuronal plasticity.
Molecular/Cellular Mechanisms
Elegant molecular genetic studies conducted in the past few years have now enabled us to identify specific molecules that are involved in the processes of pain transduction. A giant step forward came with the identification of proteins called vanilloid receptors, which allow us to detect noxious heat (4, 5). The VR1 protein is a heat transducer because it converts thermal energy into an electrical signal (action potentials) that is sent to the central nervous system, enabling us to detect a stimulus as painfully hot. Without the VR1 receptor, one does not effectively detect noxious heat, particularly in the setting of inflammation (6, 18). Recently, basic pain researchers have identified a number of transduction molecules that will clearly be key targets in developing pioneering pain therapies (7).
Neuronal Plasticity
Plasticity is a term used to refer to changes that occur in the established nervous system. Changes in neuronal structure; connections between neurons; and alterations in the quantity and properties of neurotransmitters, receptors, and ion channels can ultimately result in increased functional activity of neurons in the pain pathway. Conversely, plasticity can decrease the body's own pain inhibitory systems, resulting ultimately in increased pain. Injury, inflammation, and disease can all cause neuronal plasticity and increased pain by means of increased excitatory or decreased inhibitory mechanisms. Plasticity can result in short-term changes that last minutes to hours, or long-term changes which may be permanent.
Why Focus on the Primary Afferent Neuron?
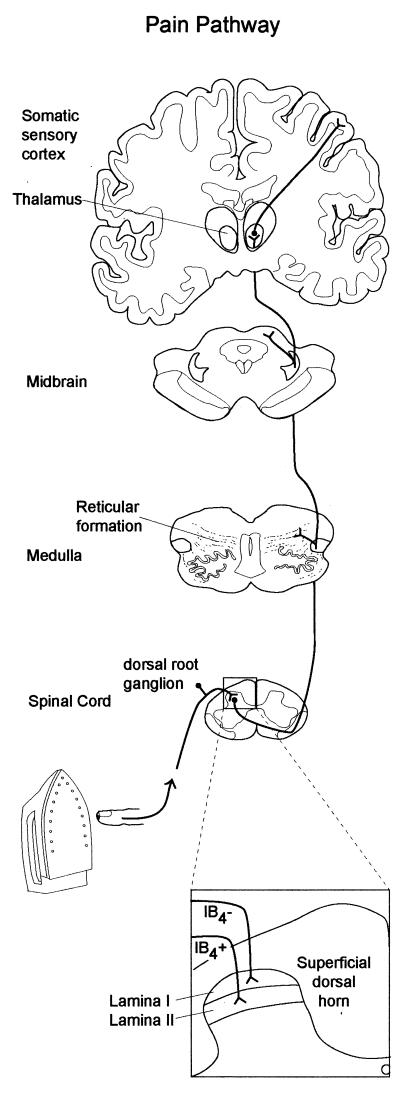
Pain transduction and perception is extensive and complex, involving fundamental biological events at multiple levels of the nervous system (Fig. 1). Our Frontiers of Science session was not intended to be a comprehensive review of the latest findings at all levels of the pain pathway. Instead, we focused on the place where sensation of pain is initiated, the primary afferent nociceptor. Nociceptors are a subpopulation of primary sensory neurons that are activated by “noxious” stimuli, i.e., stimuli that can produce tissue damage. Compelling evidence suggests that plasticity in nociceptors contributes substantially to the increased pain one feels in the presence of injury. Plasticity in nociceptors is critical for both the development and maintenance of plasticity in the central nervous system (2). That many receptors and ion channels recently identified are found specifically in nociceptors makes these proteins very good targets for eliminating pain without inducing side effects. Finally, the accessibility of the peripheral nervous system makes nociceptors a logical target for the development of novel therapeutic interventions.
Figure 1.
Painful stimuli such as intense heat activate the peripheral terminals of nociceptors. Action potentials are transmitted along the afferent axons to the spinal cord. The central terminals of IB4-negative unmyelinated nociceptors synapse in lamina I and outer lamina II, whereas IB4-positive unmyelinated nociceptors terminate in inner lamina II. By means of chemical transmission, nociceptors activate spinal neurons that send axons across the spinal cord and up fiber tracts and terminate in the medulla, midbrain, and thalamus. Thalamic neurons project to regions of the cortex including the somatosensory cortex.
Do Specific Types of Nociceptors Mediate Different Types of Pain?
Nociceptors are extremely heterogeneous, differing in the neurotransmitters they contain, the receptors and ion channels they express, their speed of conduction, their response properties to noxious stimuli, and their capacity to be sensitized during inflammation, injury, and disease. Significant progress toward alleviating pain will occur if we are able to achieve the following goals: (i) determine the function of these different subpopulations of nociceptors, (ii) determine whether specific subpopulations mediate distinct types of pain, and (iii) identify what cellular and molecular targets are altered on specific populations of nociceptors during different types of pain. Ultimately, these aims will allow the development of novel pain therapies that target specific mechanisms on identified populations of nociceptors.
Nociceptors can be divided into two general types. A-fiber nociceptors have lightly myelinated axons, conduct action potentials rapidly, and have medium- to large-diameter cell bodies. A-fibers mediate the fast, pricking quality of pain. C-fibers have unmyelinated axons, conduct action potentials slowly, and have small-diameter cell bodies. C-fibers mediate the slower, burning quality of pain. C-fibers comprise around 70% of all nociceptors. Two classes of C-fibers have been identified. One class contains a variety of neuropeptides, including substance P and calcitonin gene-related peptide, and expresses trkA receptors, the high-affinity receptor for nerve growth factor (8). These neurons project to the outermost region of the spinal dorsal horn (lamina I and outer lamina II) and terminate largely on spinal neurons that project to higher-order pain centers in the brain (Fig. 1). The other class contains few neuropeptides but expresses a surface carbohydrate group that selectively binds to a plant lectin called isolectin B4 (IB4). This subpopulation of neurons is supported by glial-derived neurotrophic factor during early postnatal development (9, 10). The IB4-binding neurons project to a different region of the spinal dorsal horn (inner lamina II) that contains primarily local spinal interneurons. Important questions are whether these two types of nociceptors have different functional responses to painful stimuli and whether they have distinct roles in specific types of pain.
We use isolated sensory neurons to examine the response properties of nociceptors to painful stimuli. By using patch-clamp-recording techniques, we found that IB4-positive nociceptors have larger magnitude voltage-gated sodium currents. In contrast, IB4-negative nociceptors had larger noxious heat-induced ion currents, suggesting that IB4-negative nociceptors are the nociceptors that respond intensely to noxious heat (11). In addition, IB4-negative nociceptors are much more responsive to noxious chemicals that are elevated during inflammation, including low pH and serotonin (C.L.S., unpublished data). One hypothesis, which remains to be tested, is that IB4-positive nociceptors mediate neuropathic pain, whereas IB4-negative nociceptors mediate inflammatory pain (12).
Why Is Morphine Ineffective in Treating Nerve Injury Pain?
Opioid analgesics such as morphine are universally regarded as the most powerful pain-relieving drugs. Morphine acts through the μ-opioid receptor to inhibit signals that transmit pain (13). Pain that follows direct injury to a peripheral nerve is called neuropathic pain. Unfortunately, it is still not known what mechanisms underlie this prevalent pain syndrome. Neuropathic pain is an anomaly because it is insensitive to morphine as well as other opioid drugs and is currently best managed with antidepressants and antiepileptics (14). Neuropathic pain may be insensitive to morphine because damage of primary afferent nerves results in decreased expression of μ-opioid receptors on nociceptors and spinal neurons in the pain pathway, thus reducing the efficacy of morphine (15). In addition, other substances may modulate the efficacy of morphine. For example, when the neuropeptide cholecystokinin (CCK) is applied to the spinal cord, it reduces the inhibitory effects of morphine (16). At the cellular level, μ-receptors and CCK receptors are expressed in the same spinal neurons, suggesting that CCK may directly inhibit actions of morphine by means of signaling mechanisms within a given neuron (17). Furthermore, activation of μ-receptors increases release of CCK neuropeptide, which then reduces the effectiveness of morphine in a feedback manner (17). Thus, multiple mechanisms, including decreased μ-receptors and increased CCK-induced inhibition of morphine, make opioids ineffective in treating neuropathic pain.
Understanding the molecular and cellular mechanisms that underlie the initiation of pain and the development and maintenance of plasticity in primary afferent and spinal neurons will undoubtedly reveal novel targets for the discovery of more effective, more specific pain therapies.
Acknowledgments
This work was supported by National Institutes of Health Grants NS40538-01 (to C.L.S.) and NS36929 (to M.S.G.), and by Nature Science Foundation of China Grant 39840160 (to X.Z.).
Abbreviations
- IB4
isolectin B4
- CCK
cholecystokinin
Footnotes
This paper is a summary of a session presented at the third annual Chinese–American Frontiers of Science symposium, held October 20–22, 2000, at the Arnold and Mabel Beckman Center of the National Academies of Science and Engineering in Irvine, CA.
References
- 1.Loeser J D, Butler S H, Chapman C R, Turk K C, editors. Bonica's Management of Pain. Philadelphia: Lippincott; 2001. [Google Scholar]
- 2.Woolf C J, Salter M W. Science. 2000;288:1765–1768. doi: 10.1126/science.288.5472.1765. [DOI] [PubMed] [Google Scholar]
- 3.Hunt S P, Mantyh P W. Nat Rev Neurosci. 2001;2:83–91. doi: 10.1038/35053509. [DOI] [PubMed] [Google Scholar]
- 4.Caterina M J, Schumacher M A, Tominaga M, Rosen T A, Levine J D, Julius D. Nature (London) 1997;389:816–824. doi: 10.1038/39807. [DOI] [PubMed] [Google Scholar]
- 5.Caterina M J, Rosen T A, Tominaga M, Brake A J, Julius D. Nature (London) 1999;398:441–446. doi: 10.1038/18906. [DOI] [PubMed] [Google Scholar]
- 6.Caterina M J, Leffler A, Malmberg A B, Martin W J, Trafton J, Petersen-Zeitz K R, Koltzenburg M, Basbaum A I, Julius D. Science. 2000;288:306–313. doi: 10.1126/science.288.5464.306. [DOI] [PubMed] [Google Scholar]
- 7.McCleskey E W, Gold M S. Annu Rev Physiol. 1999;61:835–856. doi: 10.1146/annurev.physiol.61.1.835. [DOI] [PubMed] [Google Scholar]
- 8.Averill S, McMahon S B, Clary D O, Reichardt L F, Priestley J V. Eur J Neurosci. 1995;7:1484–1494. doi: 10.1111/j.1460-9568.1995.tb01143.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Molliver D C, Wright D E, Leitner M L, Parsadanian A S, Doster K, Wen D, Yan Q, Snider W D. Neuron. 1997;19:849–861. doi: 10.1016/s0896-6273(00)80966-6. [DOI] [PubMed] [Google Scholar]
- 10.Bennett D L, Michael G J, Ramachandran N, Munson J B, Averill S, Yan Q, McMahon S B, Priestley J V. J Neurosci. 1998;18:3059–3072. doi: 10.1523/JNEUROSCI.18-08-03059.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stucky C L, Lewin G R. J Neurosci. 1999;19:6497–6505. doi: 10.1523/JNEUROSCI.19-15-06497.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Snider W D, McMahon S B. Neuron. 1998;20:629–632. doi: 10.1016/s0896-6273(00)81003-x. [DOI] [PubMed] [Google Scholar]
- 13.Matthes H W, Maldonado R, Simonin F, Valverde O, Slowe S, Kitchen I, Befort K, Dierich A, Le Meur M, Dolle P, et al. Nature (London) 1996;383:819–823. doi: 10.1038/383819a0. [DOI] [PubMed] [Google Scholar]
- 14.Watson C P. Clin J Pain. 2000;16,Suppl.:S49–S55. doi: 10.1097/00002508-200006001-00009. [DOI] [PubMed] [Google Scholar]
- 15.Zhang X, Bao L, Shi T J, Ju G, Elde R, Hokfelt T. Neuroscience. 1998;82:223–240. doi: 10.1016/s0306-4522(97)00240-6. [DOI] [PubMed] [Google Scholar]
- 16.Kellstein D E, Price D D, Mayer D J. Brain Res. 1991;540:302–306. doi: 10.1016/0006-8993(91)90524-y. [DOI] [PubMed] [Google Scholar]
- 17.Zhang X, de Araujo, Lucas G, Elde R, Wiesenfeld-Hallin Z, Hokfelt T. Neuroscience. 2000;95:197–207. doi: 10.1016/s0306-4522(99)00419-4. [DOI] [PubMed] [Google Scholar]
- 18.Davis J B, Gray J, Gunthorpe M J, Hatcher J P, Davey P T, Overend P, Harries M H, Latcham J, Clapham C, Atkinson K, et al. Nature (London) 2000;405:183–187. doi: 10.1038/35012076. [DOI] [PubMed] [Google Scholar]