Abstract
Background
Methicillin-resistant Staphylococcus aureus (MRSA) can cause serious infections in elementary students. Therefore, we aimed to elucidate the quantitative associations of school environmental contamination with nasal carriage of MRSA by students in a dose-response manner. Phenotypic and molecular characterizations were performed to further assess the associations.
Materials and methods
A cross-sectional study was conducted from March to August 2016 in eight elementary schools in Guangzhou, China. A multistage stratified cluster sampling design was used to include Chinese students and selected classes. Nasal swabs from students and environmental swabs from the schools were collected. The dose-response relationship was examined using multivariate logistic regression modeling with cluster-correlated robust variance estimates to account for correlations of isolates between the environment and the students.
Results
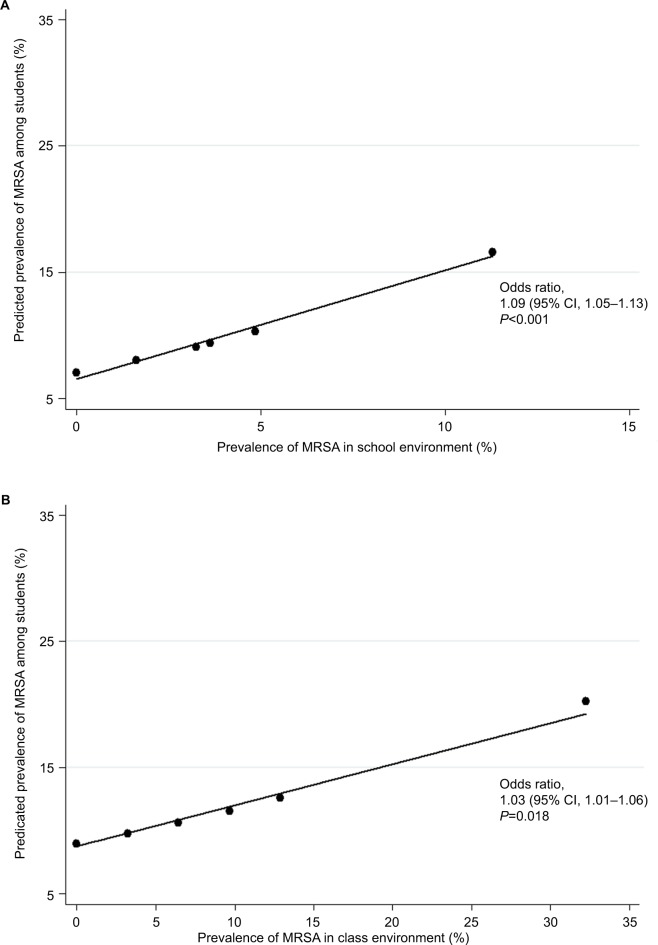
The prevalence rates of MRSA among 1705 students and 1240 environment samples were 10.15% and 3.87%, respectively. There were positive prevalence associations of school (odds ratio 1.09, 95% confidence interval [CI] 1.05–1.13) and class (odds ratio 1.03, 95% CI 1.01–1.06) environmental contamination with nasal carriage of MRSA isolates by students.
Conclusions
Comparisons of MRSA isolates between the environment and the students in terms of phenotypic and molecular characterization were mostly insignificant. School environmental contamination with MRSA was positively associated with MRSA nasal carriage by elementary students. Disinfection measures and education regarding hand hygiene should be considered to decrease the prevalence of MRSA nasal carriage among students.
Keywords: methicillin-resistant Staphylococcus aureus, school environment, contamination, elementary students, nasal carriage
Introduction
Methicillin-resistant Staphylococcus aureus (MRSA) can cause infections of the skin and soft tissue,1 endocarditis,2 sepsis,3 and other infections. Nasal carriage of MRSA has been verified to be an important risk factor for MRSA infection.4,5 Currently, the number of studies regarding community-associated MRSA (CA-MRSA) of colonization and infection is increasing,6,7 and studies have shown high proportions of MRSA nasal carriage in the student population.8,9 The majority of recent studies, however, have focused on kindergarten children,10,11 high or middle school students,9,12 and college students.13,14 Few studies have focused on elementary school students.15 Compared to other student populations, elementary school students may be easily ignored.
In addition, results of pulsed-field gel electrophoresis (PFGE) in several studies have qualitatively revealed that the environment might play an important role in the transmission of MRSA among populations. American investigators reported that a homology of MRSA strains existed between dental students and environmental surfaces in the dental school clinic.16 Mexican investigators found that there were homologous MRSA strains between students and their mobile phones.17 Portuguese investigators also found that there was possible transmission of MRSA clones between nasal carriage by passengers and contamination of public buses.18 Therefore, there were possible transmissions between humans and the environment.
As dense places, schools could also possibly create the opportunity for the spread of MRSA to some extent.19 Additionally, the environment of schools could affect the health of students. Current studies, however, are qualitative and cannot reveal the numeric associations of school environmental contamination with nasal carriage of MRSA isolates by elementary students. Therefore, with the aim of elucidating the dose-response associations of school environmental contamination with nasal carriage of MRSA isolates by students, we performed a cross-sectional study to determine the prevalence of MRSA nasal carriage among students, the prevalence of MRSA contamination in the school environment, and the associations of school environmental contamination with MRSA isolates in elementary students by prevalence and phenotypic and molecular characterization.
Materials and methods
Ethics statement
This study was approved by the Ethics Committee of Guangdong Pharmaceutical University, and it was performed in accordance with the approved guidelines of the Declaration of Helsinki. All participants were recruited voluntarily after their parents or legal representatives signed an informed consent agreement from.
Study design and population
A cross-sectional study was conducted between March 2016 and August 2016 in eight elementary schools in Guangzhou, China. A multistage, stratified, cluster sampling design was used to obtain a representative sample. In the initial phase, three administrative districts from the urban region and one administrative district from the rural region were selected using simple random sampling. In the second phase, we selected two elementary schools from each administrative district using the simple random sampling technique, and eight schools were included in all. In the third step, we chose students from grades four and five due to their better compliance and lower academic burden. The number of classes in each grade and each school were proportionally and randomly sampled. Finally, all students with consent agreements from each class were included in the study.
Selection of environmental locations
We performed environmental sampling in those classes that we selected above. Three places (classroom, restroom, and common area) in each school were selected for sampling based on previous studies and pre-surveys. Six locations (floor, light switch, door handle, desk, chair, and air) of each classroom, five locations (floor, light switch, door handle, faucet, and toilet flush handle) in the two restrooms (men’s and women’s), and three locations (handle of stairs, floor of stairs, and floor of corridor) in the common area were sampled. In total, 31 samples of each class were sampled. These locations were frequently touched by people, easily contacted by skin, and amenable to cleaning and disinfecting. With the aim of avoiding bias of sampling time, we performed sampling between 2:00 and 4:00 pm on weekdays.
Data collection and sampling
For students, we collected their demographic information (gender, age, weight, and height) through questionnaires completed by their parents. At the end of every data collection day, each questionnaire was examined for its completeness and consistency. Sterile swabs moistened with sterile saline water were used to sample both nasal vestibules of the students and surfaces of environmental locations, by trained personnel. Approximately 10×10 cm areas of floors, desks, and chairs were wiped because of their regular surfaces. The entire area of light switches, handles, and toilet faucets were wiped because of their irregular surfaces. Swabs were then inoculated in enrichment broth tubes containing 1% tryptone, 7.5% sodium chloride, 1% mannitol, and 0.25% yeast extract.
As for air sampling, we used the natural sedimentation method. We placed five mannitol salt agar plates on five desktops in each classroom during lessons (one plate in the center and four at four corners of the classroom). After 10 minutes, we closed the cover of the plates. All swabs and plates were stored below 4°C and transferred to the laboratory within 4 hours for further analyses.
Isolation and identification
After 24 hours of incubation at 37±1°C, the swabs were transferred to mannitol salt agar plates for another 24 hours of incubation. Samples, including air samples were identified as Staphylococcus aureus (S. aureus) isolates according to specific colony morphology and being positive for gram staining, the catalase reaction, hemolysis test, the DNase test, coagulase tests, and 16S rRNA and nuc genes. Those S. aureus isolates that were positive for the mecA gene and non-susceptible to cefoxitin were identified as MRSA isolates.
Antibiotic susceptibility testing
Antibiotic susceptibility testing was conducted using the Kirby-Bauer disk diffusion method, following the Clinical and Laboratory Standards Institute guidelines 2015.20 The reference MRSA strain ATCC43300 was used for quality control. All MRSA isolates underwent phenotype analysis for antibiotic susceptibility to 12 antimicrobial agents: cefoxitin, penicillin, linezolid, gentamicin, teicoplanin, erythromycin, trimethoprim-sulfamethoxazole, moxifloxacin, rifampin, chloramphenicol, tetracycline, and clindamycin. Isolates were defined as non-susceptible if they were resistant or intermediate to an antibiotic. Isolates were classified as multidrug-resistant (MDR) if they were non-susceptible to no less than three antibiotic classes (note that these isolates were already non-susceptible to all beta-lactam antibiotics).21
Molecular characterization
The DNA of all MRSA was extracted using the sodium dodecyl sulfate method22 and further tested to confirm the presence of the distinctive genes (16S rRNA, nuc, and mecA),23,24 the Panton-valentine leukocidin (Pvl) gene,25 immune evasion cluster (IEC) genes (Hlb, Scn, Chp, Sak, Sea, and Sep),26 toxin genes (Tst, Eta, and Etb),27 and resistant genes (penicillin [BlaZ], aminoglycosides [Aac(6′)-aph(2′)], tetracycline [Tet(M) and Tet(K)], macrolides [Erm(A)and Erm(C)], and chloramphenicol [Cat(A)])28 using polymerase chain reaction (PCR) assays as in previous studies.
A multiplex PCR technique was used to confirm and type the staphylococcal cassette chromosome mec (SCC-mec) gene.24 The results were reported as types I–V and those isolates that were not types I–V were deemed as non-typeable (NT).
Multilocus sequence typing (MLST) PCR assays were conducted using previously published primers and conditions.29 Allelic profiles and sequence types (STs) were assigned using the MLST database (http://www.mlst.net). Singletons or members of a clonal complex were determined using the eBURST algorithm (http://eburst.mlst.net). Dendrogram analysis was performed based on ST type to determine the clonal relatedness and potential epidemiologic origin.
Definitions of overweight and obesity
The weight of the students was measured using a digital scale designed and manufactured under the guidance of the United Nations International Children’s Emergency Fund with a precision of 100 g to measure body weight. Height measurements were taken using a locally produced United Nations International Children’s Emergency Fund measuring board with a precision of 0.1 cm. The weight and height of the students were taken twice, and variations between the two measurements of 100 g for weight and 0.1 cm for height were accepted as normal; however, repeated measurements were carried out upon significantly larger variations above 100 g in weight and 0.1 cm in height. The weight scale was calibrated before measuring the students’ weights. Repeated measurements were taken and checked by two measurers independently. Body mass index (BMI) was calculated as the weight in kilograms divided by the square of the height in meters (kg/m2). The age- and gender-specific BMI cutoff points recommended by the Working Group on Obesity in China were used to define overweight and obesity.30
Statistical analysis
The data were entered using Epidata 3.1 (EpiData Association, Odense Denmark) and exported to Stata 14.2 (College Station, Texas, USA) software for further analysis. The data were then cleaned using frequencies for logical and consistency errors. Descriptive statistics were carried out to characterize the study population using different variables. Significance of the difference between proportions was determined using Pearson’s chi-square tests for categorical variables. Univariate logistic regression and univariate logistic regression modeling with cluster-correlated robust variance estimates were used to analyze the difference of demographic characteristics among students with MRSA nasal carriage. Demographic characteristics independently associated with nasal carriage of MRSA isolates among students were identified as confounding variables in a dose-response manner with multivariate logistic regression modeling with cluster-correlated robust variance estimates to account for the correlations of isolates between the environment and students. There were two clusters in the study. One was a class cluster, and the other was a school cluster. Crude and adjusted odds ratios (ORs) with their 95% confidence interval (CI) were calculated to determine the strength and presence of an association. Moreover, we drew linear prediction plots to intuitively elucidate the dose-response association of MRSA isolates between nasal carriage among students and the environment in classes or schools. All statistical measures were estimated using survey data analysis methods. The data were analyzed using a Stata package. A two-sided P-value for statistical significance was defined as P<0.05.
Results
Prevalence of MRSA nasal carriage among students
Overall, 1705 students from 40 classes in eight elementary schools were included. The prevalence of MRSA nasal carriage among the students was 10.15% (173/1705). There were statistically significant differences of MRSA nasal carriage among students in different schools (χ2=31.211, P<0.001) and classes (χ2=94.749, P<0.001).
Prevalence of MRSA contamination in the environment
The prevalence of MRSA contamination in the school environment was 3.87% (48/1240). There were statistically significant differences of MRSA environmental contamination in different schools (χ2=15.345, P=0.018) and classes (χ2=59.011, P<0.001); however, there were no statistically significant differences of MRSA environmental contamination in different places (χ2=0.720, P=0.698) and locations (χ2=18.259, P=0.148). There were also no statistically significant differences of MRSA environmental contamination in different locations of classrooms, restrooms, or common areas. More details can be found in Table 1.
Table 1.
Distribution of MRSA isolates in the elementary school environment in Guangzhou, China, 2016
| Location | N | Positive (%) | χ2 | P-value |
|---|---|---|---|---|
| Classroom | 760 | 32 (4.21) | 1.238 | 0.457 |
| Floor | 40 | 3 (7.50) | ||
| Light switch | 80 | 6 (7.50) | ||
| Door handle | 40 | 1 (2.50) | ||
| Desk | 200 | 13 (6.50) | ||
| Chair | 200 | 5 (2.50) | ||
| Air | 200 | 4 (2.00) | ||
| Restroom | 320 | 10 (3.13) | 1.325 | 0.441 |
| Floor | 40 | 1 (2.50) | ||
| Light switch | 80 | 0 (0.00) | ||
| Door handle | 40 | 1 (2.50) | ||
| Faucet | 80 | 6 (7.50) | ||
| Toilet flush handle | 80 | 2 (2.50) | ||
| Common area | 160 | 6 (3.75) | 0.060 | 0.909 |
| Handle of stairs | 80 | 3 (3.75) | ||
| Floor of stairs | 40 | 1 (2.50) | ||
| Floor of corridor | 40 | 2 (5.00) | ||
| Total | 1240 | 48 (3.87) |
Abbreviations: MRSA, methicillin-resistant Staphylococcus aureus; N, number of isolates.
Association of prevalence between the environment and students
Grade (χ2=4.443, P=0.035) had a statistically significant effect on MRSA nasal carriage among students; however, after adjusting for school and class cluster, there was no significant difference. More details can be found in Table 2.
Table 2.
Demographic characteristics of elementary students with MRSA nasal carriage in Guangzhou, 2016
| Characteristics | N | Positive (%) | OR (95% CI) | AOR (95% CI)a | AOR (95% CI)b |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 789 | 73 (9.25) | Reference | Reference | Reference |
| Male | 916 | 100 (10.92) | 1.20 (0.87–1.65) | 1.20 (0.93–1.56) | 1.20 (0.93–1.55) |
| Age, years | |||||
| ≤10 | 1033 | 115 (11.13) | Reference | Reference | Reference |
| >10 | 672 | 58 (8.63) | 0.75 (0.54–1.05) | 0.75 (0.40–1.41) | 0.75 (0.45–1.26) |
| BMI group | |||||
| Normal weight | 1213 | 120 (9.89) | Reference | Reference | Reference |
| Overweight | 171 | 12 (7.02) | 0.69 (0.37–1.27) | 0.69 (0.51–0.93) | 0.69 (0.39–1.23) |
| Obese | 114 | 16 (14.04) | 1.49 (0.85–2.60) | 1.49 (0.86–2.58) | 1.49 (0.80–2.76) |
| Grade | |||||
| Four | 792 | 98 (12.37) | Reference | Reference | Reference |
| Five | 913 | 75 (8.21) | 0.63 (0.46–0.87) | 0.63 (0.36–1.12) | 0.63 (0.36–1.10) |
| Region | |||||
| Urban | 1399 | 139 (9.94) | Reference | Reference | Reference |
| Rural | 306 | 75 (8.21) | 1.13 (0.76–1.69) | 1.13 (0.61–2.10) | 1.13 (0.67–1.93) |
Notes:
Adjusted for school cluster;
Adjusted for class cluster.
Abbreviations: MRSA, methicillin-resistant Staphylococcus aureus; N, number of isolates; BMI, body mass index, weight (kg)/height (m)2; OR, odds ratio; AOR, adjusted OR; CI, confidence interval.
There were positive prevalence associations of school or class environment with MRSA isolates in students. The ORs and 95% CIs between the school or class environment and students in terms of the prevalence of MRSA isolates were 1.09 (95% CI, 1.05–1.13; P<0.001) and 1.03 (95% CI, 1.01–1.06; P=0.018), respectively. More details can be found in Figure 1.
Figure 1.
The relationship of the prevalence rates of MRSA isolates between the environment and students in Guangzhou, China, 2016.
Notes: (A) Linear prediction plot between the predicted prevalence of MRSA among students and the prevalence of MRSA isolates in the school environment. (B) Linear prediction plot between the predicted prevalence of MRSA among students and the prevalence of MRSA isolates in the class environment.
Abbreviation: MRSA, methicillin-resistant Staphylococcus aureus.
Association of phenotypic characterization between the environment and students
The most predominant non-susceptible antibiotic among elementary students was penicillin (100.00%, 173/173), followed by erythromycin (98.27%, 170/173), clindamycin (95.95%, 166/173), teicoplanin (91.91%, 159/173), tetracycline (82.66%, 143/173), rifampin (80.35%, 139/173), linezolid (72.25%, 125/173), chloramphenicol (34.68%, 60/173), trimethoprim-sulfamethoxazole (28.90%, 50/173), moxifloxacin (23.70%, 41/173), and gentamicin (10.40%, 18/173). The most predominant non-susceptible antibiotic among the school environment was penicillin (100.00%, 48/48) and erythromycin (100.00%, 48/48), followed by teicoplanin (95.83%, 46/48), tetracycline (95.83%, 46/48), rifampin (91.67%, 44/48), clindamycin (87.50%, 42/48), linezolid (85.42%, 41/48), moxifloxacin (29.17%, 14/48), chloramphenicol (25.00%, 12/48), trimethoprim-sulfamethoxazole (25.00%, 12/48), and gentamicin (14.58%, 7/48). When comparing the proportions of antibiotic non-susceptibility among students and the environment in terms of MRSA isolates, only tetracycline and clindamycin were significant. Note that the proportions of MDR MRSA were over 95% in both students and the environment. More details can be found in Table 3.
Table 3.
Antibiotic resistance and genetic characteristics of MRSA isolates from elementary students in Guangzhou, 2016 (n [%])
| Item | Student (N=173) | Environment (N=48) | χ2 | P-value |
|---|---|---|---|---|
| Antibiotic (non-susceptible) | ||||
| FOX | 151 (87.28) | 40 (83.33) | 0.500 | 0.480 |
| P | 173 (100.00) | 48 (100.00) | – | – |
| LZD | 125 (72.25) | 41 (85.42) | 3.482 | 0.062 |
| CN | 18 (10.40) | 7 (14.58) | 0.654 | 0.419 |
| TEC | 159 (91.91) | 46 (95.83) | – | 0.532 |
| E | 170 (98.27) | 48 (100.00) | – | 1.000 |
| SXT | 50 (28.90) | 12 (25.00) | 0.283 | 0.594 |
| MXF | 41 (23.70) | 14 (29.17) | 0.601 | 0.438 |
| RD | 139 (80.35) | 44 (91.67) | 3.382 | 0.066 |
| C | 60 (34.68) | 12 (25.00) | 1.604 | 0.205 |
| TE | 143 (82.66) | 46 (95.83) | 5.267 | 0.022 |
| DA | 166 (95.95) | 42 (87.50) | – | 0.039 |
| MDR | 169 (97.69) | 48 (100.00) | – | 0.579 |
| Gene (positive) | ||||
| IEC genes | ||||
| Hlb | 126 (72.83) | 33 (68.75) | 0.310 | 0.578 |
| Scn | 38 (21.97) | 6 (12.50) | 2.111 | 0.146 |
| Chp | 95 (54.91) | 27 (56.25) | 0.027 | 0.869 |
| Sak | 167 (96.53) | 46 (95.83) | 0.053 | 0.819 |
| Sea | 115 (66.47) | 38 (79.17) | 2.842 | 0.092 |
| Sep | 1 (0.58) | 0 (0.00) | – | 1.000 |
| Toxin genes | ||||
| Tst | 42 (24.28) | 9 (18.75) | 0.647 | 0.421 |
| Eta | 18 (10.40) | 2 (4.17) | – | 0.258 |
| Etb | 7 (4.05) | 7 (14.58) | – | 0.015 |
| Pvl | 10 (5.78) | 1 (2.08) | – | 0.463 |
| Resistant genes | ||||
| BlaZ | 169 (97.69) | 48 (100.00) | – | 0.579 |
| Aac(6′)-aph(2′) | 15 (8.67) | 5 (10.42) | – | 0.776 |
| Tet(M) | 113 (65.32) | 34 (70.83) | 0.513 | 0.474 |
| Tet(K) | 84 (48.55) | 31 (64.58) | 3.868 | 0.049 |
| Erm(A) | 1 (0.58) | 0 (0.00) | – | 1.000 |
| Erm(C) | 3 (1.73) | 2 (4.17) | – | 0.298 |
| Cat(A) | 0 (0.00) | 48 (100.00) | 221.000 | <0.001 |
Note: –, no estimate is provided owing to the lack of occurrence of the outcome of interest in at least one group.
Abbreviations: N/n, number of isolates; FOX, cefoxitin; P, penicillin; LZD, linezolid; CN, gentamicin; TEC, teicoplanin; E, erythromycin; SXT, trimethoprim-sulfamethoxazole; MXF, moxifloxacin; RD, rifampin; C, chloramphenicol; TE, tetracycline; DA, clindamycin; MDR, multidrug resistant; IEC, immune evasion cluster.
Association of molecular characterization between the environment and students
When comparing the proportions of IEC genes in the MRSA isolates among students and the environment, there was no significant difference. Among the proportions of all toxin genes, only the Etb gene was significantly different between MRSA isolates in students and the environment. There were insignificant differences in the resistant genes between students and the environment for MRSA isolates, with the exception of the Tet(K) and Cat(A) genes. More details can be found in Table 3.
Of the MRSA isolates among the students, the most predominant SCCmec type was type IV (69.36%, 120/173), followed by NT (11.56, 20/173), type V (8.09%, 14/173), type I (5.20%, 9/173), type III (4.05%, 7/173), and type II (1.73%, 3/173). Of the MRSA isolates in the environment, the most predominant SCCmec type was type IV (58.33%, 28/48), followed by NT (12.50, 6/48), type I (8.33%, 4/48), type II (8.33%, 4/48), type III (6.25%, 3/48), and type V (6.25%, 3/48). There was a significant difference of SCCmec type II in MRSA isolates between the students and environment.
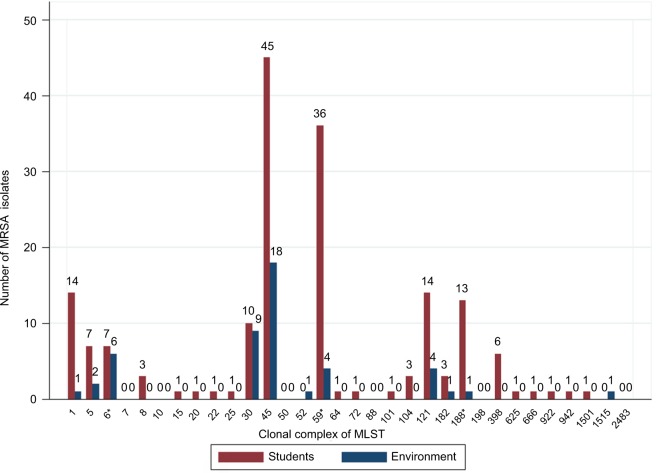
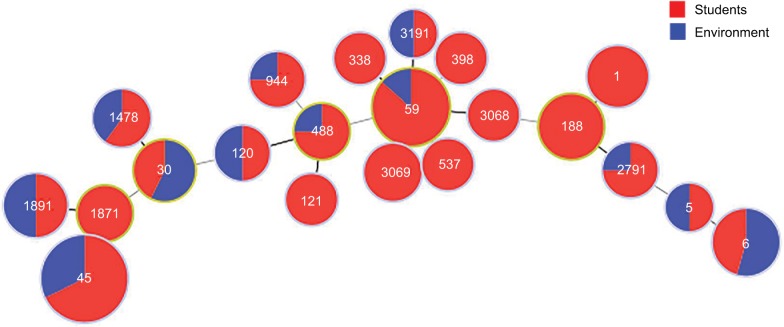
There were 26 CC types and 77 STs of MRSA isolates in this study. The five most predominant CC types of MRSA isolates among the students were CC45 (26.01%, 45/173), CC59 (20.81%, 36/173), CC1 (8.09%, 14/173), CC121 (8.09%, 14/173), and CC30 (5.78%, 10/173). The five most predominant CC types of MRSA isolates in the environment were CC45 (37.50%, 18/48), CC30 (18.75%, 9/48), CC6 (12.50%, 6/48), CC59 (8.33%, 4/48), and CC121 (8.33%, 4/48). The statistically significant CC types of MRSA isolates between the students and environment were CC6, CC59, and CC188. Note that ST5, ST6, ST30, ST45, ST59, ST120, ST488, ST944, ST1478, ST1891, ST2791, and ST3191 were found in MRSA isolates from both the students and environment. More details can be found in Figure 2 and Figure 3.
Figure 2.
Distribution of clonal complex types of MRSA isolates from students and the environment in Guangzhou, China, 2016.
Note: *There was a statistically significant difference, P<0.05.
Abbreviations: MRSA, methicillin-resistant Staphylococcus aureus; MLST, multilocus sequence typing.
Figure 3.
The sequence type relationship of MRSA isolates between the students and school environment in Guangzhou, China, 2016.
Abbreviation: MRSA, methicillin-resistant Staphylococcus aureus.
Discussion
To the authors’ knowledge, this is the first study on the dose-response prevalence associations of MRSA isolates between nasal carriage by elementary students and school environmental contamination. This study found that there were positive prevalence associations of school or class environmental contamination with nasal carriage of MRSA isolates by elementary students. The ORs of the MRSA isolates in school environments was higher than that in class environments, which may demonstrate a more severe effect of school environmental contamination on the MRSA nasal carriage by students. Therefore, these findings may suggest that school environmental contamination with MRSA plays a role in MRSA nasal colonization of students.
Our study contributes to the existing literature because we assessed the quantitative associations of MRSA isolates between the environment and students, which had not been done in other published studies. Moreover, the phenotypic characterization of MRSA isolates between the students and environment was statistically insignificant with the exception of two or three antibiotics, which meant that the phenotypic characterization of the isolates between the environment and students was similar. Regarding the molecular characterization of the MRSA isolates between the students and environment, differences observed in the majority of genes were insignificant, which also suggests that the molecular characterization of isolates between the environment and students was similar. From these three aspects of similar characterization, it is implied that there was transmission of MRSA between the school environment and elementary students.
The prevalence in students was 10.15% (173/1705) and this rate is higher than that observed in other studies.31–34 Likewise, the prevalence of MRSA in the environment was 3.87% (48/1240) and this rate is higher than that observed in other studies.35–37 The results of the prevalence demonstrate a higher burden of MRSA isolates among the environment and students, which should be paid greater attention.
The proportions of antibiotic non-susceptibility in MRSA isolates among students were higher than in other studies,12,38 which should be noted by clinical workers. A majority of antibiotic non-susceptibility of MRSA isolates between the environment and students was statistically insignificant, which may suggest that isolates transmit between the environment and students. Studies have revealed that isolates with the same PFGE types have similar or the same patterns of antibiotic susceptibility.36,39
IEC genes are becoming increasingly important because they can affect transmission ability40 and the epidemic characteristics of isolates.26 The proportions of IEC genes in this study were similar to other studies,41 as were the proportions of toxin genes and resistant genes.16,19,42 The main SCCmec types in this study were type IV and V, but the proportion of types I–III was over 10%, which may demonstrate that there was cross-transmission between the communities and hospitals.16,36 The distribution of CC types demonstrated the phylogenetic relatedness of isolates between the environment and students. Therefore, with regard to the molecular characterization of MRSA isolates between the environment and students, differences in the majority of genes were insignificant, which may also suggest that isolates transmit between the environment and students. Studies have revealed that isolates with the same PFGE types have similar or the same molecular characterization.16,34
Our findings suggest the importance of considering school environmental contamination when designing interventions aimed at reducing MRSA nasal carriage in elementary students. In hospitals, studies have shown that increased environmental cleaning reduces the proportions of MRSA isolates in the environment.43 Therefore, strengthening environmental cleaning in communities may also reduce the proportions of MRSA isolates. Further research is needed to determine whether effective decontamination of the school environment reduces the nasal carriage by elementary students.
This study has several limitations. First, we could not establish temporality because of the cross-sectional design. Second, because we could not collect the height and weight data on the spot, we used self-reported height and weight to calculate BMI, which could have resulted in misclassification; however, parents did not know the colonization status of their children, so any misclassification was likely non-differential. Third, we did not offer decolonization to students and whether such intervention would improve the health of the students is scientifically unproven.
Despite these limitations, the study had several strengths. First, the sample size of this study was large. Second, to our knowledge, our study was the first to elucidate the quantitative association of isolates between the environment and students. Third, we performed phenotypic and molecular characterization of the isolates to further assess the associations.
Conclusion
In conclusion, school environmental contamination with MRSA was positively associated with MRSA nasal carriage in elementary students. Environmental decontamination should be considered as a strategy to prevent MRSA nasal carriage. Therefore, disinfection measures of the school environment and education regarding hand hygiene for elementary students should be considered to decrease the prevalence of MRSA nasal carriage among students.
Availability of data and materials
Due to ethical restrictions related to protecting participant confidentiality, underlying data cannot be made publicly available. These data are available upon request from the principal investigator, Zhenjiang Yao (e-mail: zhjyao2001@yahoo.com).
Acknowledgments
Our study was supported by the Innovation Fund of Guangdong Science and Technology Planning Project (grant number 2014A020213013). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Author contributions
All authors contributed towards data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Liu X, Liang J, Jiang Y, et al. Molecular characteristics of community-acquired methicillin-resistant Staphylococcus aureus strains isolated from outpatients with skin and soft tissue infections in Wuhan, China. Pathog Dis. 2016;74(4):ftw026. doi: 10.1093/femspd/ftw026. [DOI] [PubMed] [Google Scholar]
- 2.Moing Le V, Alla F, Doco-Lecompte T, et al. Staphylococcus aureus bloodstream infection and endocarditis—a prospective cohort study. PLoS One. 2015;10(5):e0127385. doi: 10.1371/journal.pone.0127385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chantratita N, Wikraiphat C, Tandhavanant S, et al. Comparison of community-onset Staphylococcus argenteus and Staphylococcus aureus sepsis in Thailand: a prospective multicentre observational study. Clin Microbiol Infect. 2016;22(5):458 e11–19. doi: 10.1016/j.cmi.2016.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cadena J, Richardson AM, Frei CR. Risk factors for methicillin-resistant Staphylococcus aureus skin and soft tissue infection in MRSA-colonized patients discharged from a Veterans Affairs hospital. Epidemiol Infect. 2016;144(3):647–651. doi: 10.1017/S0950268815001132. [DOI] [PubMed] [Google Scholar]
- 5.Kao KC, Chen CB, Hu HC, Chang HC, Huang CC, Huang YC. Risk factors of methicillin-resistant Staphylococcus aureus infection and correlation with nasal colonization based on molecular genotyping in medical intensive care units: a prospective observational study. Medicine (Baltimore) 2015;94(28):e1100. doi: 10.1097/MD.0000000000001100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baker P, Cohen B, Liu J, Larson E. Incidence and risk factors for community-associated methicillin-resistant Staphylococcus aureus in New York City, 2006-2012. Epidemiol Infect. 2016;144(5):1014–1017. doi: 10.1017/S095026881500196X. [DOI] [PubMed] [Google Scholar]
- 7.Tong SY, Varrone L, Chatfield MD, Beaman M, Giffard PM. Progressive increase in community-associated methicillin-resistant Staphylococcus aureus in indigenous populations in northern Australia from 1993 to 2012. Epidemiol Infect. 2015;143(7):1519–1523. doi: 10.1017/S0950268814002611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ansari S, Gautam R, Shrestha S, Ansari SR, Subedi SN, Chhetri MR. Risk factors assessment for nasal colonization of Staphylococcus aureus and its methicillin resistant strains among pre-clinical medical students of Nepal. BMC Res Notes. 2016;9:214. doi: 10.1186/s13104-016-2021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lear A, McCord G, Peiffer J, Watkins RR, Parikh A, Warrington S. Incidence of Staphylococcus aureus nasal colonization and soft tissue infection among high school football players. J Am Board Fam Med. 2011;24(4):429–435. doi: 10.3122/jabfm.2011.04.100286. [DOI] [PubMed] [Google Scholar]
- 10.Oguzkaya-Artan M, Baykan Z, Artan C. Nasal carriage of Staphylococcus aureus in healthy preschool children. Jpn J Infect Dis. 2008;61(1):70–72. [PubMed] [Google Scholar]
- 11.Chen CJ, Hsu KH, Lin TY, Hwang KP, Chen PY, Huang YC. Factors associated with nasal colonization of methicillin-resistant Staphylococcus aureus among healthy children in Taiwan. J Clin Microbiol. 2011;49(1):131–137. doi: 10.1128/JCM.01774-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hussein NR, Basharat Z, Muhammed AH, Al-Dabbagh SA. Comparative evaluation of MRSA nasal colonization epidemiology in the urban and rural secondary school community of Kurdistan, Iraq. PLoS One. 2015;10(5):e0124920. doi: 10.1371/journal.pone.0124920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Champion AE, Goodwin TA, Brolinson PG, Werre SR, Prater MR, Inzana TJ. Prevalence and characterization of methicillin-resistant Staphylococcus aureus isolates from healthy university student athletes. Ann Clin Microbiol Antimicrob. 2014;13:33. doi: 10.1186/s12941-014-0033-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mat Azis N, Pung HP, Abdul Rachman AR, et al. A persistent antimicrobial resistance pattern and limited methicillin-resistance-associated genotype in a short-term Staphylococcus aureus carriage isolated from a student population. J Infect Public Health. 2017;10(2):156–164. doi: 10.1016/j.jiph.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 15.Kejela T, Bacha K. Prevalence and antibiotic susceptibility pattern of methicillin-resistant Staphylococcus aureus (MRSA) among primary school children and prisoners in Jimma Town, Southwest Ethiopia. Ann Clin Microbiol Antimicrob. 2013;12:11. doi: 10.1186/1476-0711-12-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roberts MC, Soge OO, Horst JA, Ly KA, Milgrom P. Methicillin-resistant Staphylococcus aureus from dental school clinic surfaces and students. Am J Infect Control. 2011;39(8):628–632. doi: 10.1016/j.ajic.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 17.Martinez-Ruíz FJ, Carrillo-Espíndola TY, Bustos-Martínez J, Hamdan-Partida A, Sánchez-Pérez L, Acosta-Gío AE. Higher prevalence of meticillin-resistant Staphylococcus aureus among dental students. J Hosp Infect. 2014;86(3):216–218. doi: 10.1016/j.jhin.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Conceição T, Diamantino F, Coelho C, de Lencastre H, Aires-de-Sousa M. Contamination of public buses with MRSA in Lisbon, Portugal: a possible transmission route of major MRSA clones within the community. PLoS One. 2013;8(11):e77812. doi: 10.1371/journal.pone.0077812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roberts MC, Soge OO, No D. Comparison of multi-drug resistant environmental methicillin-resistant Staphylococcus aureus isolated from recreational beaches and high touch surfaces in built environments. Front Microbiol. 2013;4:74. doi: 10.3389/fmicb.2013.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.CLSI . Performance standards for antimicrobial susceptibility testing; twenty-fifth informational supplement. Wayne, PA: 2015. (CLSI document M100-S25 CLSI). [Google Scholar]
- 21.Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 22.Li Ting Su JL, Guo Xiao Jian, Feng Fei. Comparison of methods for DNA extraction in Staphylococcus aureus. J Zhongkai University of Agriculture and Engineering. 2011;24(1):15–19. [Google Scholar]
- 23.Zhang K, Sparling J, Chow BL, et al. New quadriplex PCR assay for detection of methicillin and mupirocin resistance and simultaneous discrimination of Staphylococcus aureus from coagulase-negative staphylococci. J Clin Microbiol. 2004;42(11):4947–4955. doi: 10.1128/JCM.42.11.4947-4955.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang K, McClure JA, Elsayed S, Louie T, Conly JM. Novel multiplex PCR assay for characterization and concomitant subtyping of staphylococcal cassette chromosome mec types I to V in methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2005;43(10):5026–5033. doi: 10.1128/JCM.43.10.5026-5033.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McClure JA, Conly JM, Lau V, et al. Novel multiplex PCR assay for detection of the staphylococcal virulence marker Panton-Valentine leukocidin genes and simultaneous discrimination of methicillin-susceptible from -resistant staphylococci. J Clin Microbiol. 2006;44(3):1141–1144. doi: 10.1128/JCM.44.3.1141-1144.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Wamel WJ, Rooijakkers SH, Ruyken M, van Kessel KP, van Strijp JA. The innate immune modulators staphylococcal complement inhibitor and chemotaxis inhibitory protein of Staphylococcus aureus are located on beta-hemolysin-converting bacteriophages. J Bacteriol. 2006;188(4):1310–1315. doi: 10.1128/JB.188.4.1310-1315.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jarraud S, Mougiel C, Thioulouse J, et al. Relationships between Staphylococcus aureus genetic background, virulence factors, agr groups (alleles), and human disease. Infect Immun. 2002;70(2):631–641. doi: 10.1128/IAI.70.2.631-641.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guran HS, Kahya S. Species diversity and pheno- and genotypic antibiotic resistance patterns of staphylococci isolated from retail ground meats. J Food Sci. 2015;80(6):M1291–1298. doi: 10.1111/1750-3841.12893. [DOI] [PubMed] [Google Scholar]
- 29.Enright MC, Day NP, Davies CE, Peacock SJ, Spratt BG. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J Clin Microbiol. 2000;38(3):1008–1015. doi: 10.1128/jcm.38.3.1008-1015.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Group of China Obesity Task F Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents. Zhonghua Liu Xing Bing Xue Za Zhi. 2004;25(2):97–102. Chinese. [PubMed] [Google Scholar]
- 31.Demirel G, Findik D, Dagi HT, Arslan U. Community-acquired methicillin-resistant Staphylococcus aureus and genotypes among university students in Turkey. Southeast Asian J Trop Med Public Health. 2014;45(6):1401–1409. [PubMed] [Google Scholar]
- 32.Rohde RE, Denham R, Brannon A. Methicillin resistant Staphylococcus aureus: carriage rates and characterization of students in a Texas university. Clin Lab Sci. 2009;22(3):176–184. [PubMed] [Google Scholar]
- 33.Lum T, Picardo K, Westbay T, Barnello A, Fine L, Lavigne J. Student self-screening for methicillin-resistant Staphylococcus aureus (MRSA) nasal colonization in hand hygiene education. Am J Pharm Educ. 2014;78(7):138. doi: 10.5688/ajpe787138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mendes A, Martins da Costa P, Rego D, et al. Contamination of public transports by Staphylococcus aureus and its carriage by biomedical students: point-prevalence, related risk factors and molecular characterization of methicillin-resistant strains. Public Health. 2015;129(8):1125–1131. doi: 10.1016/j.puhe.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 35.Dhagat PV, Gibbs KA, Rohde RE. Prevalence of Staphylococcus, including methicillin-resistant Staphylococcus aureus, in a physical therapy education facility. J Allied Health. 2015;44(4):215–218. [PubMed] [Google Scholar]
- 36.Roberts MC, Soge OO, No D, Helgeson SE, Meschke JS. Characterization of methicillin-resistant Staphylococcus aureus isolated from public surfaces on a university campus, student homes and local community. J Appl Microbiol. 2011;110(6):1531–1537. doi: 10.1111/j.1365-2672.2011.05017.x. [DOI] [PubMed] [Google Scholar]
- 37.Mbogori C, Muigai A, Kariuki S. Detection and characterization of methicillin resistant Staphylococcus aureus from toilet and classroom door handles in selected secondary schools in Nairobi County. Open J Med Microbiol. 2013;03(04):248–252. [Google Scholar]
- 38.Kejela T, Bacha K. Prevalence and antibiotic susceptibility pattern of methicillin-resistant Staphylococcus aureus (MRSA) among primary school children and prisoners in Jimma Town, Southwest Ethiopia. Ann Clin Microbiol Antimicrob. 2013;12:1–11. doi: 10.1186/1476-0711-12-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Furuhata K, Ishizaki N, Sogawa K, et al. Isolation, identification and antibacterial susceptibility of Staphylococcus spp. associated with the mobile phones of university students. Biocontrol Sci. 2016;21(2):91–98. doi: 10.4265/bio.21.91. [DOI] [PubMed] [Google Scholar]
- 40.McCarthy AJ, Lindsay JA. Staphylococcus aureus innate immune evasion is lineage-specific: a bioinformatics study. Infect Genet Evol. 2013;19:7–14. doi: 10.1016/j.meegid.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 41.Verkaik NJ, Benard M, Boelens HA, et al. Immune evasion cluster-positive bacteriophages are highly prevalent among human Staphylococcus aureus strains, but they are not essential in the first stages of nasal colonization. Clin Microbiol Infect. 2011;17(3):343–348. doi: 10.1111/j.1469-0691.2010.03227.x. [DOI] [PubMed] [Google Scholar]
- 42.Krishnamurthy V, Saha A, Renushri BV, Nagaraj ER. Methicillin resistant Staphylococcus aureus carriage, antibiotic resistance and molecular pathogenicity among healthy individuals exposed and not exposed to hospital environment. J Clin Diagn Res. 2014;8(7):Dc04–08. doi: 10.7860/JCDR/2014/8409.4638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dancer SJ. Importance of the environment in meticillin-resistant Staphylococcus aureus acquisition: the case for hospital cleaning. Lancet Infect Dis. 2008;8(2):101–113. doi: 10.1016/S1473-3099(07)70241-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to ethical restrictions related to protecting participant confidentiality, underlying data cannot be made publicly available. These data are available upon request from the principal investigator, Zhenjiang Yao (e-mail: zhjyao2001@yahoo.com).