Abstract
Background
WHO’s Global Programme to Eliminate Lymphatic Filariasis (LF) uses mass drug administration (MDA) of anthelmintic medications to interrupt LF transmission in endemic areas. Recently, a single dose combination of ivermectin (IVM), diethylcarbamazine (DEC), and albendazole (ALB) was shown to be markedly more effective than the standard two-drug regimens (DEC or IVM, plus ALB) for achieving long-term clearance of microfilaremia.
Objective and methods
To provide context for the results of a large-scale, international safety trial of MDA using triple drug therapy, we searched Ovid Medline for studies published from 1985–2017 that reported adverse events (AEs) following treatment of LF with IVM, DEC, ALB, or any combination of these medications. Studies that reported AE rates by treatment group were included.
Findings
We reviewed 162 published manuscripts, 55 of which met inclusion criteria. Among these, 34 were clinic or hospital-based clinical trials, and 21 were community-based studies. Reported AE rates varied widely. The median AE rate following DEC or IVM treatment was greater than 60% among microfilaremic participants and less than 10% in persons without microfilaremia. The most common AEs reported were fever, headache, myalgia or arthralgia, fatigue, and malaise.
Interpretation
Mild to moderate systemic AEs related to death of microfilariae are common following LF treatment. Post-treatment AEs are transient and rarely severe or serious. Comparison of AE rates from different community studies is difficult due to inconsistent AE reporting, varied infection rates, and varied intensity of follow-up. A more uniform approach for assessing and reporting AEs in LF community treatment studies would be helpful.
Author summary
WHO’s Global Programme to Eliminate Lymphatic Filariais (LF) supports annual mass drug administration to over 400 million people in LF-endemic areas each year. Two drug combinations (either DEC or ivermectin, given with albendazole) have been recommended in most endemic areas. With the exception of well-described serious adverse events (AEs) occurring in patients with high level loiasis, severe AEs due to these medications are extremely rare. Mild to moderate AEs, however, are common, particularly in patients with active filarial infection. In this manuscript we synthesize published data on AEs following single-dose treatment of LF with ivermectin, DEC, or albendazole. This provides a background against which to compare the safety of triple drug therapy (ivermectin, DEC, and albendazole) recently endorsed by WHO, and provides a useful context for evaluating safety of new treatments for LF. The compiled data illustrate that transient, mild to moderate AEs following single-dose LF treatment are common in microfilaremic patients and are much less common in amicrofilaremic patients. They also show that passive surveillance for post-treatment AEs underestimates AE incidence and suggest that adherence to common reporting standards would improve the usefulness of AE reporting in filariasis studies.
Introduction
Infection with the filarial nematode parasites Wuchereria bancrofti, Brugia malayi, or Brugia timori is known as lymphatic filariasis (LF). These infections cause severe, disabling conditions including lymphedema, elephantiasis, and hydroceles in tens of millions of people in tropical and subtropical countries. Annual mass drug administration (MDA) coordinated by WHO’s Global Programme to Eliminate LF (GPELF) has significantly reduced LF transmission in many of the 78 initially endemic nations [1–3]. Yet LF remains far too common, with tens of millions infected and 850 million people at risk of acquiring the infection in 53 countries [3]. With approximately 500 million people receiving MDA for LF each year, understanding, anticipating, and preparing the targeted population for MDA-related adverse events (AEs) is important for program success.
Medications used for MDA include diethylcarbamazine (DEC), ivermectin (IVM) and albendazole (ALB). The combination of IVM plus ALB is used in areas of Africa where onchocerciasis (river blindness) is co-endemic with LF. Twice yearly ALB alone is recommended for LF-endemic areas of Africa that are co-endemic for loiasis, and DEC plus ALB is used in the rest of the world. Serious (life-threatening) AEs due to MDA are exceedingly rare [4–7]. However, when they do occur they can profoundly impact the treated community and jeopardize program success [8]. When communities are well-informed about the type and severity of AEs to be expected, they may be less likely to avoid MDA out of fear of AEs. Furthermore, the knowledgeability of community health workers (drug distributors) can be a major determinant of MDA adherence [8]. A clear understanding of the nature of expected AEs should empower program managers and community health workers to prepare their communities to anticipate and accept transient AEs, which may in turn improve compliance with MDA and facilitate LF elimination efforts.
A promising new combination therapy for LF that combines a single dose of IVM, DEC, and ALB (IDA) appears to be highly effective [9], and its safety is has been evaluated in large community-based studies in several locations (ClinicalTrials.gov Identifier: NCT02899936) [10]. This manuscript’s purpose is to provide context for understanding the safety of the new IDA treatment by reviewing published data on the rates and nature of AEs following single-dose treatment for LF with any of the IDA medications. As previously noted by many others, AE reporting in LF treatment trials is highly variable and potentially affected by multiple factors including blood microfilaria (Mf) counts, treatment regimens, filarial species, population demographics, and importantly, the thoroughness of post-treatment surveillance. We therefore sought to review AE data from published LF treatment studies to further understand the effect of these parameters on AE rates and severity. Our objective was to evaluate reports of AEs following single dose LF treatment of children and adults with IVM, DEC, or ALB (either as monotherapy or in multidrug combination regimens), published since 1985. In this report we first present a broad summary of the literature reviewed and then a quantitative synthesis of published AE rates from studies meeting our specified inclusion criteria.
Methods
The primary outcome of interest for the quantitative synthesis was the proportion of participants experiencing at least one AE (aggregate AE rate). Rates of individual AEs were a secondary outcome. We did not use a pre-specified AE definition, but rather accepted all AEs reported by the authors of the individual studies. In this manuscript we classify AEs as mild if they do not interfere with normal daily routine (work or school), as moderate if they interfere with daily routines (work or school) but not with activities of daily living, and as severe if they interfere with activities of daily living or cause temporary incapacitation. These designations correspond to Common Terminology Criteria for AEs grades 1 (mild), 2 (moderate), and 3 (severe). Serious AEs are those that are life-threatening or result in hospitalization or permanent injury (grade 4) or are fatal (grade 5) [11].
Literature search
We reviewed AE data from studies of LF treatment with single-dose regimens that were published between 1985 and 2017. We searched Ovid Medline and Embase for any articles with Medical Subject Headings (MeSH) terms “Elephantiasis, Filarial” and “Drug Therapy” plus any of the following terms: “Adverse Events”, “Poisoning”, or “Toxicity”. We limited our search to English or French language manuscripts dealing with human infections. The most recent search was conducted on 21 Aug, 2017. Two authors (PB and CH) reviewed each publication and gathered additional pertinent publications from articles referenced therein. Publications with sufficient AE data were selected for a quantitative analysis of AEs as described below. We did not pre-specify nor register a review protocol. We did not attempt to contact authors to identify additional studies.
Selection of studies for quantitative analysis
Studies published after 1985 that reported AE rates following single-dose LF treatment with IVM, DEC, or ALB (alone or in combination) were included. Studies dealing with multi-day courses (generally of DEC) were reviewed, but excluded from the quantitative analysis, as were studies that either provided inadequate information on AEs by treatment arm or did not conduct AE surveillance within one week following treatment. Complete inclusion and exclusion criteria are shown in Table 1. We followed the PRISMA Statement for Reporting Systematic Reviews and Meta-Analysis [12]; the completed PRISMA checklist is available as a supplemental file (S1 Table).
Table 1. Inclusion and exclusion criteria for quantitative analysis.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| • Treatment with DEC, IVM, or ALB • Report AE rates by study arm • AE data collected within first week after treatment • Published between 1985 and 2017 • Study arms with ≥ 10 participants |
• Studies of multi-dose treatments* • Adverse event assessments conducted long after treatment • Co-infection with Onchocerca volvulus or Loa loa • Treatment with other antifilarial medications (i.e. doxycycline) • Co-administration of other medications (such as azithromycin or praziquantel) |
Quantitative synthesis
From studies meeting inclusion criteria we extracted data including: study location (country), age range and gender of participants, intensity of surveillance, treatment regimen, Mf prevalence, geometric mean Mf counts, presence of co-infections, overall rate of AEs, and rates for any specific AEs reported. For studies that reported AEs following multiple MDA treatment rounds, we included only the AE rates that occurred after the first treatment. For studies in which one but not all treatment arms met inclusion criteria (for example, when single dose IVM or DEC was compared to 12 days of DEC), we included data only from the arm(s) meeting inclusion criteria. The number of participants reported in our analysis is the number for whom AE surveillance was conducted, which was sometimes lower than the total number treated. For example, one study conducted active post-MDA surveillance within a subset of 483 persons among 8 million people treated [18]; in our analysis, the N for this study was 483.
All extracted data were analyzed using Stata version 12.1 (College Station, TX). Because the data were not normally distributed, we report means and interquartile ranges (IQR) and use boxplots for graphical representation. Since AE reporting was insufficiently uniform among included studies, we did not attempt a formal meta-analysis of AE rates, nor did we attempt statistical analyses. Rather, we sought to present a graphical synthesis of data from these disparate studies to illustrate the range of data and an estimate of central tendency (median and interquartile range). To assess for reporting bias in individual studies, we stratified surveillance for AEs in each study as active (individual participants were contacted and asked about AEs) or passive (individuals with AEs had to seek out the study team to report). The quality of active surveillance was further categorized as “high” (at least daily contact during the first 72 hours), “moderate” (at least one contact within first 72 hours), or “low” (participants contacted after 72 hours). Although we hoped to analyze the effect of each extracted variable on reported AE rates, we found that the quality of data reported for most parameters was insufficient. We therefore limited our analysis to an ad hoc comparison of treatment regimens, Mf status, and intensity of AE surveillance.
Results
Literature review
Many informative articles that reported AEs following treatment for LF could not be included in our quantitative analysis either because they reported composite AE scores rather than rates, or because they did not report AE rates separately by treatment group. We have attempted to review some of the observations from both included and excluded publications in the following paragraphs.
LF MDA medications
Diethylcarbamazine (DEC). DEC is a piperazine derivative with microfilaricidal and partial macrofilaricidal activity [19], and the amount traditionally given for LF treatment was 72 mg/kg divided in 12 daily doses. Although some early studies suggested that weekly or monthly treatments might be equally or more effective than the 12 day treatment course [20, 21], it was not until single dose IVM was shown to drastically reduce Mf counts that single dose DEC was tested and found to be effective [16, 22–24]. A 6mg/kg DEC dose appears to have the best balance between efficacy and AEs [22]. Mf counts drop markedly in the first few days following single-dose DEC with continued slow decline for 6 or 7 months. This decline is generally followed by partial rebound of microfilaremia [16, 24–30]; the level to which Mf counts rebound may be lower with higher cumulative DEC doses [19, 31–36]. Serious AEs including loss of vision and fatal encephalopathy can occur when DEC is given to persons with active onchocerciasis or loiasis [37]. DEC is therefore not used in areas of Africa where LF is co-endemic with O. volvulus or L. loa. Direct pharmacologic AEs in persons with no filarial infections are generally limited to transient gastrointestinal upset (nausea, vomiting, diarrhea), dizziness, or lightheadedness that occur within a few hours of ingestion [19, 38].
Ivermectin (IVM). IVM is a semisynthetic member of the avermectin class of antihelminthics initially isolated from fermentation products of Streptomyces avermitilis. IVM treatment for LF was first reported in the late 1980s [39–41] and 15 early safety and efficacy studies of IVM for bancroftian filariasis were reviewed in a 1997 meta analysis [42]. IVM dosing for LF MDA is based on height and roughly corresponds to 150–200 μg/kg. Single dose IVM induces a rapid clearance of circulating Mf within the first five days; rebound of microfilaremia following IVM begins as early as 30 days post-treatment with continued increases out to 6 months [16, 25, 40, 41, 43–46]. This rapid Mf clearance occurs with doses as low as 20 μg/kg [15, 39, 46], but higher doses (200 to 400 μg/kg) may have a more prolonged effect [47]. Unlike DEC, single dose IVM has little or no effect on filarial antigen levels [48–50], suggesting a lack of macrofilaricidal effect. IVM is teratogenic at repeated high doses in laboratory animals and is not given to children weighing less than 15 kg or to pregnant women during MDA for LF [2, 51]. As with DEC, IVM can precipitate severe encephalopathy and death when given to persons heavily infected with L. loa [52, 53], and is not used as MDA for LF in areas with high intensity L. loa infections.
Albendazole (ALB). ALB belongs to the benzimidazole group of anthelminthic agents and is thought to inhibit tubulin polymerization leading to immobilization and death of susceptible helminths. Two meta-analyses of ALB combination therapy for LF published in 2005 disagreed regarding ALB’s value for treating LF [6, 7], and its inclusion in LF MDA regimens is partially due to its activity against soil-transmitted helminths (STH) [6, 7, 54]. Single-dose ALB alone induces very slow declines in Mf counts and a minor decrease in filarial antigen levels, suggesting a partial macrofilaricidal effect [54–56], which may be enhanced by twice yearly treatment [57, 58]. Although high dose ALB (400 mg twice daily) for 3 weeks induced scrotal reactions in 11 of 15 men in one study (compared to zero of 13 DEC-treated men) [59], there is no evidence that adding single-dose ALB to IVM or DEC for LF MDA increases AEs [5]. In areas where LF is co-endemic with loiasis, semiannual ALB alone (together with integrated vector management) is recommended for LF MDA, because ALB can be safely given to persons with loiasis [60, 61].
AEs following treatment of LF
Transient mild to moderate adverse reactions such as fever, headache, dizziness, malaise, myalgia, fatigue, and gastrointestinal upset are common after treatment of LF and are primarily related to dying Mf [5, 6, 62]. Less commonly reported AEs include cough and dyspnea [15, 17, 23, 40] (sometimes associated with blood-tinged sputum and transient pulmonary infiltrates [63] or bronchoconstriction [40, 64]), urticaria or other rash [45, 63, 65], transient proteinuria or hematuria [9, 44, 63, 66], elevated alkaline phosphatase [63] or transaminase levels [46, 59, 65], palpebral edema (with DEC) [17], increased eosinophilia 7–14 days post-treatment [17, 40, 59, 67], and postural hypotension [16, 23, 40, 45, 68]. Systemic AEs generally occur with 24–48 hours after the first dose of microfilaricidal medications (IVM or DEC) [23, 24, 29, 30, 40, 43–45, 54, 56, 64, 67–75], including when low “clearing doses” of drugs are given before full therapeutic doses [14, 15, 24]. Most systemic AEs resolve within 48 hours of onset, although they sometimes last longer [15, 16, 24, 29, 30, 40, 44, 45, 54, 56, 64, 67, 69, 73, 75].
Localized AEs following LF treatment are much less common than systemic AEs. They include the development of subcutaneous or scrotal nodules, spermatic cord swelling, new onset or increased hydrocele, dilated and inflamed lymphatic vessels (the “string sign”) [68], arthritis, lymphadenitis (sometimes with suppuration), and new onset lymphedema [76]. Local reactions may occur within 24–48 hours after treatment, but often the onset is later (1 week or more after treatment) [15, 17, 44, 45, 55, 59, 66, 72, 77]. They are generally self-limited, resolving over the course of one to several weeks. They are thought to be caused by the death of adult filarial worms in lymphatic vessels [14, 15, 17, 19, 44, 63, 78, 79]; prior to the development of adult worm antigen assays and ultrasound visualization of adult worms [79], rates of scrotal reactions were frequently used as a surrogate measure of macrofilaricidal activity [15, 59, 77]. Biopsies of scrotal nodules confirm the presence of dead or dying adult worms and excised nodules sometimes contain both dying and healthy adult worms [79–81].
Factors potentially affecting reported AE rates
Infection intensity. Because AEs are related to the death of circulating Mf, the rates and severity of AEs following LF treatment increase with increasing Mf loads and increased microfilaricidal efficacy [14–16, 22, 30, 34, 38, 39, 43, 47, 54, 65, 78, 82–84]. Because of this, AEs are highest following the first dose of microfilaricidal drugs, and they tend to be less frequent and milder in later treatment rounds [47, 67, 74, 77, 85–89]. One notable exception was an initial dose-finding study of IVM against brugian filariasis that did not observe a correlation between AEs and pre-treatment Mf counts [67].
Gender and age. Most studies that reported gender-specific rates of directly-observed AEs did not report significantly different rates between men and women [15, 22, 30, 56, 90, 91]. However, two community MDA studies with passive AE surveillance reported higher rates in women. This may reflect gender-specific differences in reporting, rather than physiologic differences [76, 92]. In one large MDA study in Haiti, moderate AEs (those interfering with school or work) were more frequently reported by men, and these were most commonly due to scrotal pain [72]. Reported AE rates tend to be lower in children [48, 49, 54, 64, 84].
Species differences. Differences in susceptibility to treatment between brugian and bancroftian filariasis may affect AE rates among those who are Mf positive. For bancroftian filariasis, IVM appears to clear Mf more rapidly and more completely than DEC [14, 16, 17, 25, 30, 45, 93, 94], but Mf counts also rebound sooner following IVM treatment. DEC induces a slower, more sustained decline, with gradual Mf reductions out to about 6 months [25, 31, 64, 95]. Over a longer period, reductions in Mf counts are equivalent [14, 25, 71, 96, 97] or slightly better with DEC [16, 17, 24, 45]. For bancroftian filariasis, acute reactions tend to be higher with IVM and later (localized) reactions higher with DEC [17, 45].
The decline in Mf counts following IVM treatment may be somewhat slower in persons with brugian filariasis [65, 67] and AEs following IVM treatment of brugian filariasis may be less severe and occur slightly later post-treatment (day 2–3) [65]. Brugia Mf may be more sensitive to DEC-mediated killing [19, 24, 68, 82], and Brugia Mf carriers may have more AEs when treated with DEC than W. bancrofti Mf carriers [24, 73, 82]. Treatment of brugian filariasis does not result in scrotal reactions, a finding that reflects Brugia’s lack of tropism for scrotal lymphatic vessels and the lack of hydroceles in brugian filariasis [24].
Medication dose. The initial evaluation of IVM for bancroftian filariasis suggested that 25 μg/kg worked as well as higher doses, but with fewer AEs [40]. The initial study of IVM for brugian filariasis also had a trend towards lower AEs with 25 μg/kg, but this was not statistically significant [67]. In general, however, the level of microfilaremia is much more predictive of AEs than the dose of antifilarial medication [39, 84]. For example, in several studies where low “clearing doses” of medications were given prior to higher “treatment” doses, AE rates were higher with the clearing dose than with the treatment dose for both IVM [13, 15, 98] and DEC [98].
Passive vs. active surveillance. Intensity of AE surveillance following MDA can have a large effect on reported AE rates. One study directly compared AE rates reported by active surveillance (daily visits) with AE reports from subsequent coverage surveys and found 3–4 fold higher AE rates identified by active surveillance [18]. In passive surveillance studies, the rate of reported symptoms may have more to do with general health-seeking behavior than with Mf-related AEs [99].
Co-infections. Co-infections with other filarial species can have dramatic effects on AEs experienced following treatment for LF. These include the well-recognized risk of ocular damage with visual loss after treatment of onchocerciasis with DEC, and encephalopathy and death in persons with heavy loiasis infections [52, 53]. GI symptoms following MDA for LF may be partially related to the effects of treatment on intestinal helminths; extremely low rates of GI side effects were observed in one study that excluded those with a positive stool ova and parasite screen from treatment [56].
AE pathogenesis
Wolbachia. The molecular mechanisms underlying AEs following LF treatment are incompletely understood, but one leading hypothesis is that they are related to release of bacterial endotoxin-like lipoproteins from endosymbiotic Wolbachia released from dying Mf. Several lines of evidence support this hypothesis. First, B. malayi-infected adults with moderate to severe AEs were more likely to have Wolbachia DNA in post-treatment serum samples compared to those with mild or no AEs [100]. Second, a lipopolysaccharide (LPS)-like activity in B. malayi extract is a potent inducer of TNF-α, IL-1ß and nitric oxide (NO) in murine macrophages, while extracts from the rodent filarial parasite A. viteae (which do not harbor Wolbachia) do not induce these responses [101, 102]. It was surprising, therefore, when the B. malayi-associated Wolbachia genome published in 2004 did not contain genes required for the biosynthesis of lipid A, an essential component of LPS [103]. This suggested that Wolbachia does not contain LPS in its cell wall [104]. However, a peptidoglycan-associated lipoprotein (PAL) in Wolbachia may effectively mimic the activity of LPS. PAL can signal through TLR2/TLR6, induces pro-inflammatory responses in vitro (in murine and human cells) and in vivo (mice) [105], and is abundant in B. malayi, where it localizes to the Wolbachia membrane [106]. Finally, depletion of Wolbachia with a three or six week treatment course of doxycycline prior to anti-filarial treatment with ALB plus either DEC or IVM decreased the risk of acute AEs [107, 108]; whether this was due to depletion of Wolbachia or to doxycycline-related reductions in Mf counts is unclear. Concurrent treatment with doxycycline and DEC reduced inflammatory cytokines and AE severity among microfilaremic patients in another study [109], but an imbalance in the baseline Mf counts in the latter study makes that finding difficult to interpret. Another study did not demonstrate a significant reduction in AEs in persons with LF after pre-clearance of Wolbachia with doxycycline [110].
Circulating immune complexes. Circulating immune complexes may also contribute to the development of AEs following LF treatment. These are heterogeneous aggregates of antigens, antibodies and components of the complement cascade [111] that activate pro-inflammatory pathways when they circulate or accumulate in tissue. One publication reported that filarial excretory-secretory antigens and immune complex titers increased after DEC treatment of LF patients [112]. A later study showed that these changes were temporally correlated with the onset of AEs and that their magnitude was significantly greater in individuals who developed AEs after treatment [113].
Quantitative synthesis of published AE rates
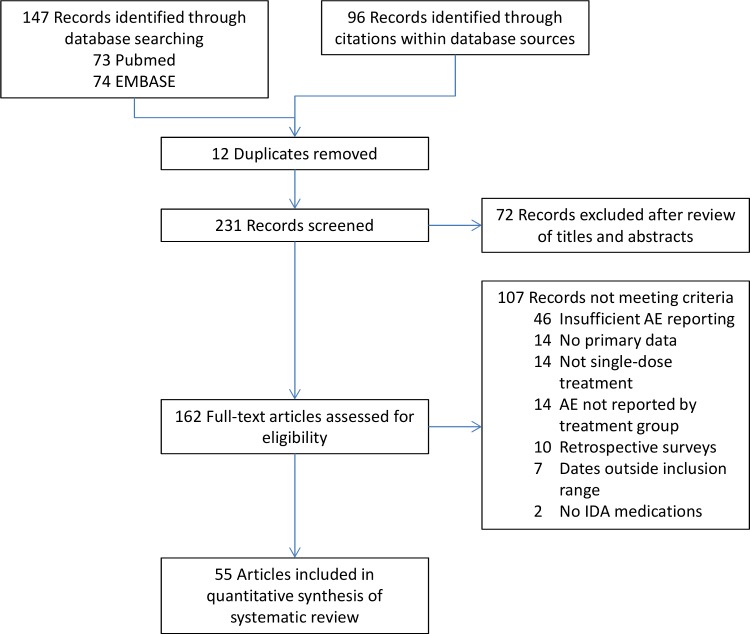
To summarize published rates of AEs following single-dose treatment of LF, and to explore how these might differ by treatment medication and AE surveillance, we compiled data from articles with adequate AE reporting into a combined analysis. Among 162 full text articles reviewed, 55 contained AE data that met criteria for inclusion (Fig 1). There was considerable heterogeneity in the way that AEs were reported in these studies; 34 reported both the aggregate incidence of AEs (i.e. the number of persons experiencing any AE) and the percentage of persons experiencing specific AEs. Seventeen studies reported an aggregate incidence but not specific events, and four reported specific events but not aggregate incidence. Methods of AE ascertainment varied widely between studies, from intensive in-hospital monitoring to passive reporting in community-based trials. For the purposes of our analyses we grouped the studies into two main types: (1) clinical trials with active AE surveillance and (2) community studies with either active or passive surveillance. The former group comprises studies in which 100% of participants were Mf positive, while community studies had varied Mf rates (Table 2).
Fig 1. PRISMA flow diagram for inclusion of articles in the quantitative synthesis.
Table 2. Articles included in the quantitative analysis by article type and study location.
| Study location | N Studies | N participants | References |
|---|---|---|---|
| Hospital or Clinic Based Studies with High Quality, Active Surveillance | |||
| Brazil | 3 | 194 | [17, 44, 64] |
| China | 1 | 60 | [71] |
| Egypt | 1 | 71 | [45] |
| French Polynesia | 7 | 314 | [69, 85, 90, 93, 94, 114, 115] |
| Haiti | 4 | 340 | [13, 15, 54, 84] |
| India | 11 | 591 | [16, 30, 40, 43, 56, 67, 68, 75, 87, 116, 117] |
| Indonesia | 1 | 15 | [23] |
| Malaysia | 1 | 40 | [65] |
| Papua New Guinea | 1 | 24 | [9] |
| Senegal | 1 | 16 | [41] |
| Sri Lanka | 2 | 77 | [14, 46] |
| Tanzania | 1 | 25 | [118] |
| Subtotal | 34 | 1,767 | |
| Community Based Studies with Active Surveillance | |||
| Brazil | 2 | 818 | [76, 119] |
| Egypt | 1 | 28 | [77] |
| French Polynesia | 2 | 4,421 | [39, 47] |
| Ghana | 2 | 1,299 | [108, 120] |
| India | 5 | 10,596 | [18, 86, 110, 121, 122] |
| Papua New Guinea | 1 | 966 | [123] |
| Samoa | 1 | 458 | [22] |
| Sri Lanka | 1 | 31 | [29] |
| Tanzania | 1 | 57 | [124] |
| Subtotal | 16 | 18,674 | |
| Community Based Studies with Passive Surveillance | |||
| Ghana | 1 | 15,020 | [125] |
| Haiti | 2 | 74,968 | [72, 99] |
| Kenya | 1 | 170 | [126] |
| Mali | 1 | 42 | [127] |
| Subtotal | 5 | 90,200 | |
| Total | 55 | 110,641 | |
AE rates by Mf status and surveillance intensity
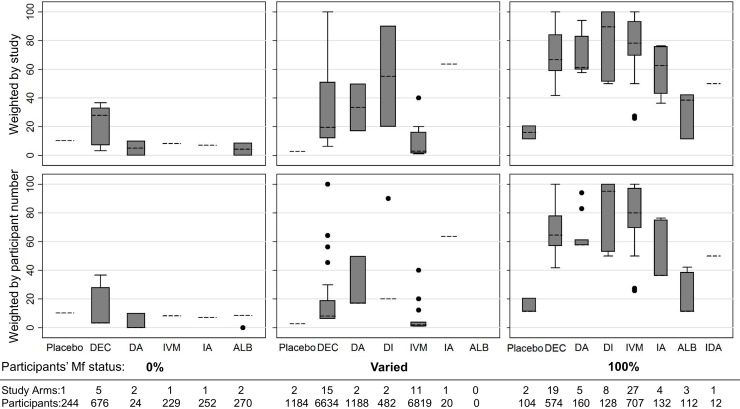
As shown in Fig 2, reported AE rates were markedly higher in study arms where 100% of participants were Mf positive. The median aggregate AE rate (proportion of participants experiencing at least one AE) among study arms where all participants were microfilaremic was 70% when each study was given equal weight and 67% when results were adjusted to consider the number of participants per study arm. Reported AE rates in non-placebo groups with no microfilaremia ranged from zero to 37% with a median of 8.3% (7.1% when adjusted for participants per study arm). As expected, studies with passive surveillance reported much lower AE rates (ranging from 0 to 24% regardless of Mf prevalence); this included two study arms from one study in which all participants were microfilaremic [127]. A complete list of the studies included with the extracted data and notes is available as a supplement (S2 Table).
Fig 2. Box plot of reported percentage of participants experiencing at least one AE among individual treatment groups (study arms), comparing active (dark boxes) and passive (light boxes) surveillance methods, excluding placebos.
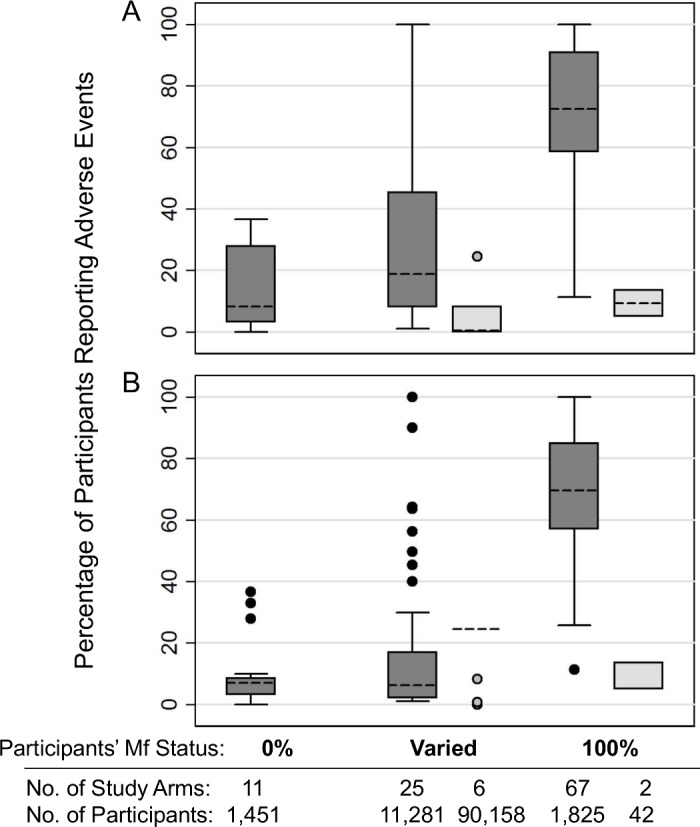
Groups where no participants (0%) or all participants (100%) were Mf positive were from hospital or clinic-based clinical trials; those with “varied” Mf status were from community studies. A) Results when each study group was considered to have equal weight. B) Results when results were adjusted to consider the number of participants in each study group. Boxes indicate the interquartile range (IQR) and dashed line the median. Whiskers indicate the upper and lower adjacent values: upper = the greatest value less than (75th percentile + (1.5 x IQR)); lower = the lowest value greater than (25th percentile–(1.5 x IQR)).
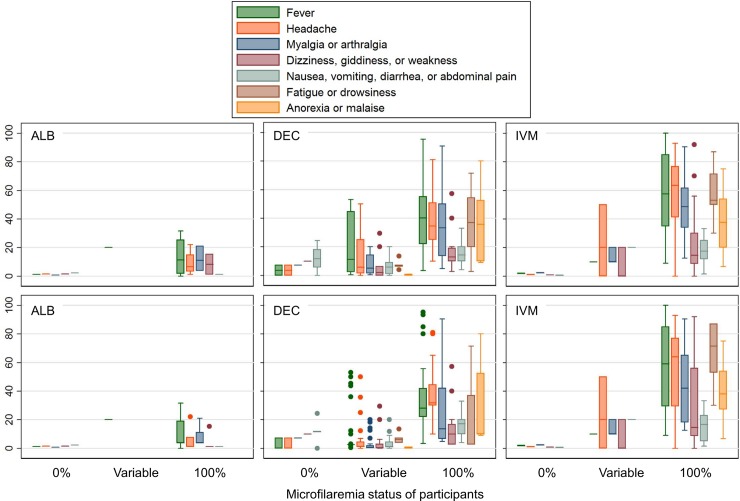
AE rates by treatment
Aggregated AE rates by treatment regimen from studies with active surveillance are shown in Fig 3. AE rates in amicrofilaremic groups were less than or equal to 10% in all groups except among persons treated with DEC only. Among the five included amicrofilaremic treatment groups receiving DEC, three were from a single study that compared different DEC doses (4, 6, or 8 mg/kg) and reported AE rates >25% with all three DEC doses [22]. It is difficult to explain the unusually high AE rates reported from that study.
Fig 3. Percentage of participants experiencing at least one AE in studies with active surveillance, according to the microfilaremia (Mf) status of participants.
Groups where no participants (0%) or all participants (100%) were Mf positive were from hospital or clinic-based clinical trials; those with “varied” Mf status were from community studies. The top panels show equal weighting for each study, regardless of participant number; results in the bottom panels are weighted by participant number. Boxes indicate the interquartile range (IQR) and dashed line the median. Whiskers indicate the upper and lower adjacent values: upper = the greatest value less than (75th percentile + (1.5 x IQR)); lower = the lowest value greater than (25th percentile–(1.5 x IQR). Abbreviations: ALB = Albendazole, DA = DEC + Albendazole, DI = DEC + Ivermectin, IA = Ivermectin + Albendazole, IDA = Ivermectin + DEC + Albendazole, IVM = Ivermectin.
Aggregate AE rates after treatment of microfilaremic persons with regimens that included DEC or IVM ranged between 40 and 100%, with two exceptions: Dunyo reported AE rates of 25.8% and 36.3% among those treated with IVM alone or IVM plus ALB, respectively [120], and Mak reported a rate of 27.5% among those receiving IVM alone [65]. Among the three included studies reporting aggregate AE rates after ALB only treatment, AEs were reported in 11% of 80 participants (tactile fever, myalgia, headache, weakness, abdominal pain, itching) [120], 38% of 12 participants (itching, palpitation, or fever) [118], and 42% of 19 participants (predominantly fever and myalgia) [56].
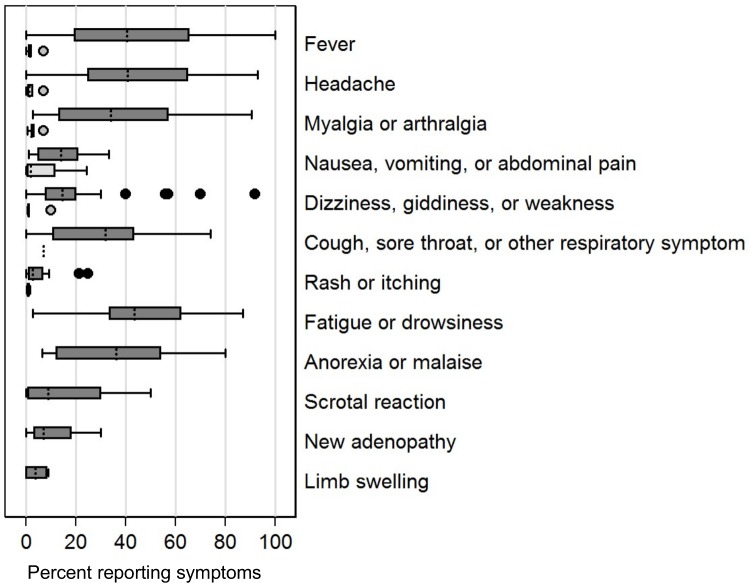
Rate of specific AEs
Results varied widely in studies with active surveillance that reported specific AEs after treatment of Mf positive persons. Rates of fever were 100% in some studies, and other systemic symptoms including myalgia/arthralgia, dizziness, giddiness, weakness, fatigue, and malaise were also very common. Rates of systemic events in amicrofilaremic individuals were much lower (Fig 4). The rates and patterns of AEs did not clearly differ between DEC and IVM, but AEs were much less common after ALB, and they were low with any medication in amicrofilaremic participants (Fig 5).
Fig 4. Reported percentages of specific AEs in treatment arms with 100% microfilaremia rates (shaded bars) or no microfilaremia (open bars).
Only studies with active AE reporting are included and each study arm is given equal weight (not weighted by participant number). Boxes indicate the interquartile range (IQR) and dashed line the median. Whiskers indicate the upper and lower adjacent values: upper = the greatest value less than (75th percentile + (1.5 x IQR)); lower = the lowest value greater than (25th percentile–(1.5 x IQR)).
Fig 5. Percentage of participants experiencing common systemic AEs by treatment group, according to the microfilaremia status of participants.
DEC and IVM data include all study arms where the indicated drug was given alone or in combination (with or without ALB). For clarity, the ALB panel shows only study arms in which ALB alone was given. The upper panels assign each study are equal weight; the lower panels are weighted according to number of participants per study arm. Boxes indicate the interquartile range (IQR) and horizontal line the median. Whiskers indicate the upper and lower adjacent values: upper = the greatest value less than (75th percentile + (1.5 x IQR)); lower = the lowest value greater than (25th percentile–(1.5 x IQR)).
Discussion
In this review we initially sought to quantify the effects of various factors on AE rates that occur following MDA for LF. We quickly realized that the heterogeneity in the way AEs have been reported in the literature would not allow a meaningful quantitative multivariate analysis. We nevertheless felt a compilation of reported AE rates would be beneficial. Despite the limitations of combining data from methodologically disparate studies, we believe the compiled data illustrate the following main points: 1) AEs are very common in microfilaremic patients after single-dose treatment of LF with drugs (IVM and DEC) that rapidly reduce Mf counts. 2) AEs are much less common in amicrofilaremic participants, regardless of treatment regimen. 3) Passive surveillance tends to underestimate the occurrence of AEs, and 4) Heterogeneity in the stringency of AE surveillance and format of AE reporting makes comparisons between studies difficult.
The relationship between AE rates and the prevalence of microfilaremia is illustrated by the striking differences between study arms with 100% microfilaremia and those with no microfilaremia. It would have been interesting to compare Mf prevalence to AE rates among the community studies with varied Mf prevalence; this was not attempted because of the variability in AE reporting for these studies and because uncertainty regarding true Mf rates would have made this comparison unreliable.
It is clear that community proclivities for reporting AEs vary from place to place and study to study. This is perhaps most evident in reported AE rates after placebo treatment. Studies with highly active AE surveillance in Haiti and Tahiti reported high AE rates after placebo treatment [54, 84, 93], but AE rates were low after placebo treatment in Ghana and India [86, 120]. This place-to-place AE reporting variability is also evident in the wide range of AE rates reported among different studies with the same treatment regimens (see Figs 3 and 5). Potential reasons for this might include the prevalence of STH or other helminth infections, differing intensities of LF infection, and varying cultural norms. In addition, where populations have been sensitized to expect AEs following MDA, more AEs may be perceived [18].
Nearly all the studies cited in this review reported AE rates in some manner, but we were only able to include 55 in the quantitative synthesis. The primary reason for excluding studies was that they did not present AE data in a way that linked AE rates to treatment regimens. For example, many studies reported AE severity scores rather than rates. Others reported that AE rates did not differ significantly between treatment groups, but did not report the numbers for each group. When AE rates were reported by treatment group, comparisons were often hampered by non-standardized AE reporting procedures. Some authors did not report the timeframe over which AE surveillance was conducted, making it difficult to surmise whether early or late AEs may have been missed. Although most studies included in our analysis described whether AE surveillance was active or passive, many contained insufficient detail to determine how sensitive the study procedures were for detecting AEs. For example, ascertainment rates (the proportion of participants in community-based studies who were actually visited and queried about AEs) were almost never reported.
This review has several strengths and weaknesses. The primary strength is that it compiles data from 30 years of published studies. It also illustrates how variable AE reporting can be, and it provides a context for interpreting AE rates observed in future LF treatment studies. One weakness was our inability to include data from many high quality studies that did not report AEs by treatment arm. In addition, because we restricted our analysis to studies of single-dose therapy, many rich and highly informative studies that used multi-dose treatment regimens were excluded. In general, the pattern of AEs reported in such studies was similar to single dose studies. That is to say, the rate and severity of AEs increased with increasing Mf counts and most AEs occurred during the first 48 hours after the initial treatment dose [38, 82].
The heterogeneity in AE reporting among the reviewed studies highlights the need for a more structured approach to AE reporting in LF treatment studies. Although this problem is not unique to filariasis [128], it can be compounded by the nature of community-based studies. We therefore suggest the following measures for improving AE reporting in community based treatment trials for LF and other neglected tropical diseases (Box 1). 1) Clearly specify the methods for ascertaining AEs. Indicate whether an attempt was made to contact each participant (active surveillance) or whether participants were required to seek out study staff to report AEs (passive surveillance). Indicate when and how often participants were contacted. Avoid ambiguous language such as “followed closely”, or “closely monitored”. Rather, describe what was actually done. For example, “treated individuals were visited daily in their homes for five days after treatment”. 2) If surveillance was active, report the ascertainment rate; that is, the proportion of participants sought during surveillance that was actually found. Knowing what proportion of participants actually contributed to the reported AE rates will help the reader assess the reported findings. For example, one study reported, “All subjects [were] asked to come to the study site on day 2 and day 5….In addition, team members also went door to door.” The door to door contacting was presumably meant to ascertain AEs in subjects not reporting at the study site, since subjects may choose not to present for follow-up either because they feel well and see no need, or because they feel ill and don’t wish to leave their homes. The higher the proportion of participants for whom actual AE status is not ascertained, the greater the uncertainty regarding the reported AE rates. Unfortunately, the study cited—and most other community studies we reviewed—did not report ascertainment rates. 3) Report numerators and denominators. When severity scores are used (for example, 1 = mild, 2 = moderate, 3 = severe) to compare AEs between study groups, the actual number of persons experiencing AEs should also be reported so that rates can be calculated. The difference between one person with a severe AE and three people with one mild AE each is important, and the reporting of AE data should allow the reader to distinguish the difference. In addition to clearly specifying the number of persons experiencing AEs (the numerator), the denominator should be clearly defined. In active studies, we suggest reporting AE rates as the proportion of those experiencing AEs over the number actually assessed. For example, five persons experiencing AEs among 20 patients treated should be reported as 50% (not 25%) if only 10 of those treated were actually assessed. 4) Use standardized grading criteria for reporting AE severity. Examples include the National Cancer Institute’s Common Terminology Criteria for Adverse Events (available at https://evs.nci.nih.gov/ftp1/CTCAE/About.html) or the Division of AIDS Table for Grading the Severity of Adult and Pediatric Adverse Events (available at http://rsc.tech-res.com/clinical-research-sites/safety-reporting/daids-grading-tables). 5) Follow CONSORT guidelines for better reporting of harms in clinical trials [129].
Box 1. Recommendation for AE reporting in filariasis studies.
- Clearly specify the method for ascertaining AEs.
-
○Was an attempt made to contact each participant to assess for AEs?
-
○When and how often were AEs assessed?
-
○
Report the ascertainment rate (the percentage of participants assessed for AEs).
- Report numerators and denominators.
-
○How many adverse events occurred among how many participants?
-
○Report the actual numbers, even if severity scores are used, to allow readers to calculate rates.
-
○
Use standardized grading for reporting AE severity.
Follow CONSORT guidelines for reporting harms.
In conclusion, this review has shown that AEs following single dose treatment of LF are common and should be expected in microfilaremic patients. This information provides a useful context for understanding AEs observed with new treatments for LF. Clear and detailed reporting of AEs in community treatment studies is essential to accurately inform elimination program workers and their communities, and to set appropriate expectations. The fear of MDA-associated AEs is often out of proportion to the actual risk, because most post-treatment AEs are mild and transient. A frank explanation of AEs as a marker for treatment efficacy by program managers and community health workers may improve compliance with MDA and facilitate LF elimination efforts.
Supporting information
(DOC)
(XLSX)
(DOC)
Acknowledgments
We would like to thank Kim Lipsey, Medical Librarian at the Bernard Becker Medical Library, for her assistance with developing the initial literature search strategy and conducting the literature searches.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
PJB is supported by NIH/NIAID grant K08AI121422 and by an award from the NIH Loan Repayment Programs (NIAID). PJB and GJW are supported in part by grant GH5342 from the Bill & Melinda Gates Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Ichimori K, King JD, Engels D, Yajima A, Mikhailov A, Lammie P, et al. Global programme to eliminate lymphatic filariasis: the processes underlying programme success. PLoS neglected tropical diseases. 2014;8(12):e3328 Epub 2014/12/17. doi: 10.1371/journal.pntd.0003328 ; PubMed Central PMCID: PMCPmc4263400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. Preventive chemotherapy in human helminthiasis: coordinated use of anthelminthic drugs in control interventions: a manual for health professionals and programme managers Geneva, Switzerland: WHO Press; 2006. [Google Scholar]
- 3.Summary of global update on preventive chemotherapy implementation in 2016: crossing the billion. Wkly Epidemiol Rec. 2017;92(40):589–93. . [PubMed] [Google Scholar]
- 4.Tisch DJ, Michael E, Kazura JW. Mass chemotherapy options to control lymphatic filariasis: a systematic review. Lancet Infectious Diseases. 2005;5(8):514–23. doi: 10.1016/S1473-3099(05)70192-4. WOS:000231033200020. [DOI] [PubMed] [Google Scholar]
- 5.Horton J, Witt C, Ottesen EA, Lazdins JK, Addiss DG, Awadzi K, et al. An analysis of the safety of the single dose, two drug regimens used in programmes to eliminate lymphatic filariasis. Parasitology. 2000;121 Suppl:S147–60. Epub 2001/06/02. . [DOI] [PubMed] [Google Scholar]
- 6.Critchley J, Addiss D, Gamble C, Garner P, Gelband H, Ejere H. Albendazole for lymphatic filariasis. The Cochrane database of systematic reviews. 2005;(4):Cd003753.. Epub 2005/10/20. doi: 10.1002/14651858.CD003753.pub3 . [DOI] [PubMed] [Google Scholar]
- 7.Gyapong JO, Kumaraswami V, Biswas G, Ottesen EA. Treatment strategies underpinning the global programme to eliminate lymphatic filariasis. Expert Opin Pharmacother. 2005;6(2):179–200. doi: 10.1517/14656566.6.2.179 . [DOI] [PubMed] [Google Scholar]
- 8.Krentel A, Fischer PU, Weil GJ. A review of factors that influence individual compliance with mass drug administration for elimination of lymphatic filariasis. PLoS neglected tropical diseases. 2013;7(11):e2447 Epub 2013/11/28. doi: 10.1371/journal.pntd.0002447 ; PubMed Central PMCID: PMCPmc3836848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomsen EK, Sanuku N, Baea M, Satofan S, Maki E, Lombore B, et al. Efficacy, Safety, and Pharmacokinetics of Coadministered Diethylcarbamazine, Albendazole, and Ivermectin for Treatment of Bancroftian Filariasis. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2016;62(3):334–41. Epub 2015/10/22. doi: 10.1093/cid/civ882 . [DOI] [PubMed] [Google Scholar]
- 10.WHO. Guideline: alternative mass drug administration regimens to eliminate lymphatic filariasis. King JD, editor: WHO/Department of control of neglected tropical diseases; 2017. [PubMed]
- 11.Common terminology criteria for adverse events (CTCAE): National Cancer Institute; [cited 2018 3-21-18]. Available from: https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm.
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Medicine. 2009;6(7):e1000097 doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Addiss DG, Eberhard ML, Lammie PJ, Hitch WL, Spencer HC. Tolerance of single high-dose ivermectin for treatment of lymphatic filariasis. Trans R Soc Trop Med Hyg. 1991;85(2):265–6. . [DOI] [PubMed] [Google Scholar]
- 14.Ismail MM, Weil GJ, Jayasinghe KS, Premaratne UN, Abeyewickreme W, Rajaratnam HN, et al. Prolonged clearance of microfilaraemia in patients with bancroftian filariasis after multiple high doses of ivermectin or diethylcarbamazine. Trans R Soc Trop Med Hyg. 1996;90(6):684–8. Epub 1996/11/01. . [DOI] [PubMed] [Google Scholar]
- 15.Richards FO Jr., Eberhard ML, Bryan RT, McNeeley DF, Lammie PJ, McNeeley MB, et al. Comparison of high dose ivermectin and diethylcarbamazine for activity against bancroftian filariasis in Haiti. Am J Trop Med Hyg. 1991;44(1):3–10. . [DOI] [PubMed] [Google Scholar]
- 16.Ottesen EA, Vijayasekaran V, Kumaraswami V, Perumal Pillai SV, Sadanandam A, Frederick S, et al. A controlled trial of ivermectin and diethylcarbamazine in lymphatic filariasis. N Engl J Med. 1990;322(16):1113–7. doi: 10.1056/NEJM199004193221604 . [DOI] [PubMed] [Google Scholar]
- 17.Dreyer G, Coutinho A, Miranda D, Noroes J, Rizzo JA, Galdino E, et al. Treatment of bancroftian filariasis in Recife, Brazil: a two-year comparative study of the efficacy of single treatments with ivermectin or diethylcarbamazine. Trans R Soc Trop Med Hyg. 1995;89(1):98–102. . [DOI] [PubMed] [Google Scholar]
- 18.Babu BV, Rath K, Kerketta AS, Swain BK, Mishra S, Kar SK. Adverse reactions following mass drug administration during the Programme to Eliminate Lymphatic Filariasis in Orissa State, India. Trans R Soc Trop Med Hyg. 2006;100(5):464–9. doi: 10.1016/j.trstmh.2005.07.016 . [DOI] [PubMed] [Google Scholar]
- 19.Ottesen EA. Efficacy of diethylcarbamazine in eradicating infection with lymphatic-dwelling filariae in humans. Rev Infect Dis. 1985;7(3):341–56. . [DOI] [PubMed] [Google Scholar]
- 20.Nathan MB, Hamilton PJ, Monteil S, Tikasingh ES. Bancroftian filariasis in coastal north Trinidad: the effects of mass chemotherapy using spaced doses of diethylcarbamazine citrate on human microfilaraemias and vector infection rates. Trans R Soc Trop Med Hyg. 1987;81(4):663–8. . [DOI] [PubMed] [Google Scholar]
- 21.Eberhard ML, Lammie PJ, Roberts JM, Lowrie RC Jr., Effectiveness of spaced doses of diethylcarbamazine citrate for the control of bancroftian filariasis. Trop Med Parasitol. 1989;40(2):111–3. . [PubMed] [Google Scholar]
- 22.Kimura E, Penaia L, Spears GF. The efficacy of annual single-dose treatment with diethylcarbamazine citrate against diurnally subperiodic bancroftian filariasis in Samoa. Bull World Health Organ. 1985;63(6):1097–106. ; PubMed Central PMCID: PMCPMC2536478. [PMC free article] [PubMed] [Google Scholar]
- 23.Sutanto I, Boreham PF, Munawar M, Purnomo, Partono F. Adverse reactions to a single dose of diethylcarbamazine in patients with Brugia malayi infection in Riau Province, West Indonesia. Southeast Asian J Trop Med Public Health. 1985;16(3):395–400. . [PubMed] [Google Scholar]
- 24.Shenoy RK, Kumaraswami V, Rajan K, Thankom S, Jalajakumari. A comparative study of the efficacy and tolerability of single and split doses of ivermectin and diethylcarbamazine in periodic brugian filariasis. Ann Trop Med Parasitol. 1993;87(5):459–67. . [DOI] [PubMed] [Google Scholar]
- 25.Kazura J, Greenberg J, Perry R, Weil G, Day K, Alpers M. Comparison of single-dose diethylcarbamazine and ivermectin for treatment of bancroftian filariasis in Papua New Guinea. Am J Trop Med Hyg. 1993;49(6):804–11. . [DOI] [PubMed] [Google Scholar]
- 26.Meyrowitsch DW, Simonsen PE, Makunde WH. Mass DEC chemotherapy for control of bancroftian filariasis: comparative efficacy of four strategies two years after start of treatment. Trans R Soc Trop Med Hyg. 1996;90(4):423–8. . [DOI] [PubMed] [Google Scholar]
- 27.Moulia-Pelat JP, Glaziou P, Weil GJ, Nguyen LN, Gaxotte P, Nicolas L. Combination ivermectin plus diethylcarbamazine, a new effective tool for control of lymphatic filariasis. Trop Med Parasitol. 1995;46(1):9–12. Epub 1995/03/01. 7631132. [PubMed] [Google Scholar]
- 28.Moulia-Pelat JP, Nguyen LN, Glaziou P, Chanteau S, Ottesen EA, Cardines R, et al. Ivermectin plus diethylcarbamazine: an additive effect on early microfilarial clearance. Am J Trop Med Hyg. 1994;50(2):206–9. . [DOI] [PubMed] [Google Scholar]
- 29.Weerasooriya MV, Kimura E, Dayaratna DA, Weerasooriya TR, Samarawickrema WA. Efficacy of a single dose treatment of Wuchereria bancrofti microfilaria carriers with diethylcarbamazine in Matara, Sri Lanka. Ceylon Med J. 1998;43(3):151–5. . [PubMed] [Google Scholar]
- 30.Subramanyam Reddy G, Vengatesvarlou N, Das PK, Vanamail P, Vijayan AP, Kala S, et al. Tolerability and efficacy of single-dose diethyl carbamazine (DEC) or ivermectin in the clearance of Wuchereria bancrofti microfilaraemia in Pondicherry, south India. Tropical medicine & international health: TM & IH. 2000;5(11):779–85. Epub 2000/12/21. . [DOI] [PubMed] [Google Scholar]
- 31.Hakim SL, Vythilingam I, Marzukhi MI, Mak JW. Single-dose diethylcarbamazine in the control of periodic brugian filariasis in Peninsular Malaysia. Trans R Soc Trop Med Hyg. 1995;89(6):686–9. . [DOI] [PubMed] [Google Scholar]
- 32.Bockarie MJ, Alexander ND, Hyun P, Dimber Z, Bockarie F, Ibam E, et al. Randomised community-based trial of annual single-dose diethylcarbamazine with or without ivermectin against Wuchereria bancrofti infection in human beings and mosquitoes. Lancet. 1998;351(9097):162–8. doi: 10.1016/S0140-6736(97)07081-5 . [DOI] [PubMed] [Google Scholar]
- 33.Nicolas L, Plichart C, Nguyen LN, Moulia-Pelat JP. Reduction of Wuchereria bancrofti adult worm circulating antigen after annual treatments of diethylcarbamazine combined with ivermectin in French Polynesia. J Infect Dis. 1997;175(2):489–92. . [DOI] [PubMed] [Google Scholar]
- 34.Prasad GB, Ramaprasad P, Rao VS, Bharati MS, Harinath BC. Efficacy of two different DEC regimens in the treatment of human filarial infection. Indian J Med Res. 1990;91:133–7. . [PubMed] [Google Scholar]
- 35.Simonsen PE, Meyrowitsch DW, Makunde WH, Magnussen P. Selective diethylcarbamazine chemotherapy for control of Bancroftian filariasis in two communities of Tanzania: compared efficacy of a standard dose treatment and two semi-annual single dose treatments. Am J Trop Med Hyg. 1995;53(3):267–72. Epub 1995/09/01. . [DOI] [PubMed] [Google Scholar]
- 36.Meyrowitsch DW, Simonsen PE, Makunde WH. Mass diethylcarbamazine chemotherapy for control of bancroftian filariasis: comparative efficacy of standard treatment and two semi-annual single-dose treatments. Trans R Soc Trop Med Hyg. 1996;90(1):69–73. . [DOI] [PubMed] [Google Scholar]
- 37.Ltd EC. Patient information leaflet; diethylcarbamazine citrate tablets 100 mg USP Hertfordshire, UK: Eisai Europe Ltd; 2013. [Google Scholar]
- 38.Haarbrink M, Terhell AJ, Abadi GK, Mitsui Y, Yazdanbakhsh M. Adverse reactions following diethylcarbamazine (DEC) intake in 'endemic normals', microfilaraemics and elephantiasis patients. Trans R Soc Trop Med Hyg. 1999;93(1):91–6. . [DOI] [PubMed] [Google Scholar]
- 39.Roux J, Perolat P, Cartel JL, Boutin JP, Sechan Y, Lariviere M, et al. [A study of ivermectin in the treatment of lymphatic filariasis due to Wuchereria bancrofti var. pacifica in French Polynesia]. Bull Soc Pathol Exot Filiales. 1989;82(1):72–81. . [PubMed] [Google Scholar]
- 40.Kumaraswami V, Ottesen EA, Vijayasekaran V, Devi U, Swaminathan M, Aziz MA, et al. Ivermectin for the treatment of Wuchereria bancrofti filariasis. Efficacy and adverse reactions. JAMA. 1988;259(21):3150–3. . [PubMed] [Google Scholar]
- 41.Diallo S, Aziz MA, Ndir O, Badiane S, Bah IB, Gaye O. Dose-ranging study of ivermectin in treatment of filariasis due to Wuchereria bancrofti. Lancet. 1987;1(8540):1030 . [DOI] [PubMed] [Google Scholar]
- 42.Cao WC, Van der Ploeg CP, Plaisier AP, van der Sluijs IJ, Habbema JD. Ivermectin for the chemotherapy of bancroftian filariasis: a meta-analysis of the effect of single treatment. Tropical medicine & international health: TM & IH. 1997;2(4):393–403. . [DOI] [PubMed] [Google Scholar]
- 43.Kar SK, Patnaik S, Mania J, Kumaraswami V. Ivermectin in the treatment of bancroftian filarial infection in Orissa, India. Southeast Asian J Trop Med Public Health. 1993;24(1):80–6. . [PubMed] [Google Scholar]
- 44.Coutinho AD, Dreyer G, Medeiros Z, Lopes E, Machado G, Galdino E, et al. Ivermectin treatment of bancroftian filariasis in Recife, Brazil. Am J Trop Med Hyg. 1994;50(3):339–48. . [DOI] [PubMed] [Google Scholar]
- 45.Sabry M, Gamal H, el-Masry N, Kilpatrick ME. A placebo-controlled double-blind trial for the treatment of bancroftian filariasis with ivermectin or diethylcarbamazine. Trans R Soc Trop Med Hyg. 1991;85(5):640–3. . [DOI] [PubMed] [Google Scholar]
- 46.Ismail MM, Premaratne UN, Abeywickreme W. Treatment of bancroftian filariais with ivermectin in Sri Lanka: evaluation of efficacy and adverse reactions. Tropical Biomedicine. 1991;8:71–5. [Google Scholar]
- 47.Nguyen NL, Moulia-Pelat JP, Glaziou P, Martin PM, Cartel JL. Advantages of ivermectin at a single dose of 400 micrograms/kg compared with 100 micrograms/kg for community treatment of lymphatic filariasis in Polynesia. Trans R Soc Trop Med Hyg. 1994;88(4):461–4. . [DOI] [PubMed] [Google Scholar]
- 48.Dunyo SK, Nkrumah FK, Simonsen PE. Single-dose treatment of Wuchereria bancrofti infections with ivermectin and albendazole alone or in combination: evaluation of the potential for control at 12 months after treatment. Trans R Soc Trop Med Hyg. 2000;94(4):437–43. . [DOI] [PubMed] [Google Scholar]
- 49.Simonsen PE, Magesa SM, Dunyo SK, Malecela-Lazaro MN, Michael E. The effect of single dose ivermectin alone or in combination with albendazole on Wuchereria bancrofti infection in primary school children in Tanzania. Trans R Soc Trop Med Hyg. 2004;98(8):462–72. doi: 10.1016/j.trstmh.2003.12.005 . [DOI] [PubMed] [Google Scholar]
- 50.Weil GJ, Lammie PJ, Richards FO Jr., Eberhard ML. Changes in circulating parasite antigen levels after treatment of bancroftian filariasis with diethylcarbamazine and ivermectin. J Infect Dis. 1991;164(4):814–6. Epub 1991/10/11. . [DOI] [PubMed] [Google Scholar]
- 51.Inc. MC. Stromectol (Ivermectin). Prescribing Information. Haarlem, Netherlands: Merck & Co., Inc.; 2010. [Google Scholar]
- 52.Boussinesq M, Gardon J, Gardon-Wendel N, Kamgno J, Ngoumou P, Chippaux JP. Three probable cases of Loa loa encephalopathy following ivermectin treatment for onchocerciasis. Am J Trop Med Hyg. 1998;58(4):461–9. Epub 1998/05/09. . [DOI] [PubMed] [Google Scholar]
- 53.Gardon J, Gardon-Wendel N, Demanga N, Kamgno J, Chippaux JP, Boussinesq M. Serious reactions after mass treatment of onchocerciasis with ivermectin in an area endemic for Loa loa infection. Lancet. 1997;350(9070):18–22. Epub 1997/07/05. doi: 10.1016/S0140-6736(96)11094-1 . [DOI] [PubMed] [Google Scholar]
- 54.Fox LM, Furness BW, Haser JK, Desire D, Brissau JM, Milord MD, et al. Tolerance and efficacy of combined diethylcarbamazine and albendazole for treatment of Wuchereria bancrofti and intestinal helminth infections in Haitian children. Am J Trop Med Hyg. 2005;73(1):115–21. . [PubMed] [Google Scholar]
- 55.Ismail MM, Jayakody RL, Weil GJ, Nirmalan N, Jayasinghe KS, Abeyewickrema W, et al. Efficacy of single dose combinations of albendazole, ivermectin and diethylcarbamazine for the treatment of bancroftian filariasis. Trans R Soc Trop Med Hyg. 1998;92(1):94–7. Epub 1998/08/06. . [DOI] [PubMed] [Google Scholar]
- 56.Pani S, Subramanyam Reddy G, Das L, Vanamail P, Hoti S, Ramesh J, et al. Tolerability and efficacy of single dose albendazole, diethylcarbamazine citrate (DEC) or co-administration of albendazole with DEC in the clearance of Wuchereria bancrofti in asymptomatic microfilaraemic volunteers in Pondicherry, South India: a hospital-based study. Filaria J. 2002;1(1):1 doi: 10.1186/1475-2883-1-1 ; PubMed Central PMCID: PMCPMC139957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pion SD, Chesnais CB, Bopda J, Louya F, Fischer PU, Majewski AC, et al. The impact of two semiannual treatments with albendazole alone on lymphatic filariasis and soil-transmitted helminth infections: a community-based study in the Republic of Congo. Am J Trop Med Hyg. 2015;92(5):959–66. doi: 10.4269/ajtmh.14-0661 ; PubMed Central PMCID: PMCPMC4426585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pion SDS, Chesnais CB, Weil GJ, Fischer PU, Missamou F, Boussinesq M. Effect of 3 years of biannual mass drug administration with albendazole on lymphatic filariasis and soil-transmitted helminth infections: a community-based study in Republic of the Congo. Lancet Infect Dis. 2017;17(7):763–9. doi: 10.1016/S1473-3099(17)30175-5 . [DOI] [PubMed] [Google Scholar]
- 59.Jayakody RL, de Silva CSS, Weerasooriya WMT . Treatment of bancroftian filariasis with albendazole: evaluation of efficacy and adverse reactions. Tropical Biomedicine. 1993;10:19–24. [Google Scholar]
- 60.Kamgno J, Boussinesq M. Effect of a single dose (600 mg) of albendazole on Loa loa microfilaraemia. Parasite. 2002;9(1):59–63. Epub 2002/04/10. doi: 10.1051/parasite/200209159 . [DOI] [PubMed] [Google Scholar]
- 61.Kamgno J, Nguipdop-Djomo P, Gounoue R, Tejiokem M, Kuesel AC. Effect of Two or Six Doses 800 mg of Albendazole Every Two Months on Loa loa Microfilaraemia: A Double Blind, Randomized, Placebo-Controlled Trial. PLoS neglected tropical diseases. 2016;10(3):e0004492 Epub 2016/03/12. doi: 10.1371/journal.pntd.0004492 ; PubMed Central PMCID: PMCPMC4788450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ottesen EA. Lymphatic filariasis: Treatment, control and elimination. Advances in parasitology. 2006;61:395–441. Epub 2006/06/01. doi: 10.1016/S0065-308X(05)61010-X . [DOI] [PubMed] [Google Scholar]
- 63.Kar SK, Patnaik S, Kumaraswami V, Murty RS. Side reactions following ivermectin therapy in high density bancroftian microfilaraemics. Acta Trop. 1993;55(1–2):21–31. . [DOI] [PubMed] [Google Scholar]
- 64.Rizzo JA, Belo C, Lins R, Dreyer G. Children and adolescents infected with Wuchereria bancrofti in Greater Recife, Brazil: a randomized, year-long clinical trial of single treatments with diethylcarbamazine or diethylcarbamazine-albendazole. Ann Trop Med Parasitol. 2007;101(5):423–33. doi: 10.1179/136485907X176517 . [DOI] [PubMed] [Google Scholar]
- 65.Mak JW, Navaratnam V, Grewel JS, Mansor SM, Ambu S. Treatment of subperiodic Brugia malayi infection with a single dose of ivermectin. Am J Trop Med Hyg. 1993;48(4):591–6. . [DOI] [PubMed] [Google Scholar]
- 66.Dreyer G, Ottesen EA, Galdino E, Andrade L, Rocha A, Medeiros Z, et al. Renal abnormalities in microfilaremic patients with Bancroftian filariasis. Am J Trop Med Hyg. 1992;46(6):745–51. . [DOI] [PubMed] [Google Scholar]
- 67.Shenoy RK, Kumaraswami V, Rajan K, Thankom S, Jalajakumari. Ivermectin for the treatment of periodic malayan filariasis: a study of efficacy and side effects following a single oral dose and retreatment at six months. Ann Trop Med Parasitol. 1992;86(3):271–8. . [DOI] [PubMed] [Google Scholar]
- 68.Shenoy RK, George LM, John A, Suma TK, Kumaraswami V. Treatment of microfilaraemia in asymptomatic brugian filariasis: the efficacy and safety of the combination of single doses of ivermectin and diethylcarbamazine. Ann Trop Med Parasitol. 1998;92(5):579–85. . [DOI] [PubMed] [Google Scholar]
- 69.Cartel JL, Sechan Y, Boutin JP, Celerier P, Plichart R, Roux JF. Ivermectin for treatment of bancroftian filariasis in French Polynesia: efficacy in man, effect on transmission by vector Aedes polynesiensis. Trop Med Parasitol. 1990;41(3):241–4. . [PubMed] [Google Scholar]
- 70.Dreyer G, de Andrade L. Inappropriateness of the association of diphenhydramine with diethylcarbamazine for the treatment of lymphatic filariasis. J Trop Med Hyg. 1989;92(1):32–4. . [PubMed] [Google Scholar]
- 71.Zheng HJ, Piessens WF, Tao ZH, Cheng WF, Wang SH, Cheng SH, et al. Efficacy of ivermectin for control of microfilaremia recurring after treatment with diethylcarbamazine. I. Clinical and parasitologic observations. Am J Trop Med Hyg. 1991;45(2):168–74. . [PubMed] [Google Scholar]
- 72.McLaughlin SI, Radday J, Michel MC, Addiss DG, Beach MJ, Lammie PJ, et al. Frequency, severity, and costs of adverse reactions following mass treatment for lymphatic filariasis using diethylcarbamazine and albendazole in Leogane, Haiti, 2000. Am J Trop Med Hyg. 2003;68(5):568–73. . [DOI] [PubMed] [Google Scholar]
- 73.Supali T, Ismid IS, Ruckert P, Fischer P. Treatment of Brugia timori and Wuchereria bancrofti infections in Indonesia using DEC or a combination of DEC and albendazole: adverse reactions and short-term effects on microfilariae. Tropical medicine & international health: TM & IH. 2002;7(10):894–901. . [DOI] [PubMed] [Google Scholar]
- 74.Ciferri F, Siliga N, Long G, Kessel JF. A filariasis-control program in American Samoa. Am J Trop Med Hyg. 1969;18(3):369–78. . [DOI] [PubMed] [Google Scholar]
- 75.Shenoy RK, Dalia S, John A, Suma TK, Kumaraswami V. Treatment of the microfilaraemia of asymptomatic brugian filariasis with single doses of ivermectin, diethylcarbamazine or albendazole, in various combinations. Ann Trop Med Parasitol. 1999;93(6):643–51. . [DOI] [PubMed] [Google Scholar]
- 76.Lima AW, Medeiros Z, Santos ZC, Costa GM, Braga C. Adverse reactions following mass drug administration with diethylcarbamazine in lymphatic filariasis endemic areas in the Northeast of Brazil. Rev Soc Bras Med Trop. 2012;45(6):745–50. . [DOI] [PubMed] [Google Scholar]
- 77.El Setouhy M, Ramzy RM, Ahmed ES, Kandil AM, Hussain O, Farid HA, et al. A randomized clinical trial comparing single- and multi-dose combination therapy with diethylcarbamazine and albendazole for treatment of bancroftian filariasis. Am J Trop Med Hyg. 2004;70(2):191–6. Epub 2004/03/03. . [PubMed] [Google Scholar]
- 78.Ismail MM, Jayakody RL, Weil GJ, Fernando D, De Silva MS, De Silva GA, et al. Long-term efficacy of single-dose combinations of albendazole, ivermectin and diethylcarbamazine for the treatment of bancroftian filariasis. Trans R Soc Trop Med Hyg. 2001;95(3):332–5. Epub 2001/08/09. . [DOI] [PubMed] [Google Scholar]
- 79.Noroes J, Dreyer G, Santos A, Mendes VG, Medeiros Z, Addiss D. Assessment of the efficacy of diethylcarbamazine on adult Wuchereria bancrofti in vivo. Trans R Soc Trop Med Hyg. 1997;91(1):78–81. . [DOI] [PubMed] [Google Scholar]
- 80.Dreyer G, Addiss D, Santos A, Figueredo-Silva J, Noroes J. Direct assessment in vivo of the efficacy of combined single-dose ivermectin and diethylcarbamazine against adult Wuchereria bancrofti. Trans R Soc Trop Med Hyg. 1998;92(2):219–22. . [DOI] [PubMed] [Google Scholar]
- 81.Figueredo-Silva J, Jungmann P, Noroes J, Piessens WF, Coutinho A, Brito C, et al. Histological evidence for adulticidal effect of low doses of diethylcarbamazine in bancroftian filariasis. Trans R Soc Trop Med Hyg. 1996;90(2):192–4. . [DOI] [PubMed] [Google Scholar]
- 82.Fan PC. Diethylcarbamazine treatment of bancroftian and malayan filariasis with emphasis on side effects. Ann Trop Med Parasitol. 1992;86(4):399–405. . [DOI] [PubMed] [Google Scholar]
- 83.Glaziou P, Moulia-Pelat JP, Nguyen LN, Chanteau S, Martin PM, Cartel JL. Double-blind controlled trial of a single dose of the combination ivermectin 400 micrograms/kg plus diethylcarbamazine 6 mg/kg for the treatment of bancroftian filariasis: results at six months. Trans R Soc Trop Med Hyg. 1994;88(6):707–8. . [DOI] [PubMed] [Google Scholar]
- 84.Addiss DG, Beach MJ, Streit TG, Lutwick S, LeConte FH, Lafontant JG, et al. Randomised placebo-controlled comparison of ivermectin and albendazole alone and in combination for Wuchereria bancrofti microfilaraemia in Haitian children. Lancet. 1997;350(9076):480–4. doi: 10.1016/S0140-6736(97)02231-9 . [DOI] [PubMed] [Google Scholar]
- 85.Cartel JL, Spiegel A, Nguyen Ngnoc L, Cardines R, Plichart R, Martin PM, et al. Single versus repeated doses of ivermectin and diethylcarbamazine for the treatment of Wuchereria bancrofti var. pacifica microfilaremia. Results at 12 months of a double-blind study. Trop Med Parasitol. 1991;42(4):335–8. . [PubMed] [Google Scholar]
- 86.Das PK, Ramaiah KD, Vanamail P, Pani SP, Yuvaraj J, Balarajan K, et al. Placebo-controlled community trial of four cycles of single-dose diethylcarbamazine or ivermectin against Wuchereria bancrofti infection and transmission in India. Trans R Soc Trop Med Hyg. 2001;95(3):336–41. . [DOI] [PubMed] [Google Scholar]
- 87.Kar SK, Dwibedi B, Kerketa AS, Maharana A, Panda SS, Mohanty PC, et al. A randomized controlled trial of increased dose and frequency of albendazole with standard dose DEC for treatment of Wuchereria bancrofti microfilaremics in Odisha, India. PLoS neglected tropical diseases. 2015;9(3):e0003583 Epub 2015/03/18. doi: 10.1371/journal.pntd.0003583 ; PubMed Central PMCID: PMCPmc4363665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Partono F, Purnomo, Soewarta A, Oemijati S. Low dosage diethylcarbamazine administered by villagers for the control of timorian filariasis. Trans R Soc Trop Med Hyg. 1984;78(3):370–2. . [DOI] [PubMed] [Google Scholar]
- 89.Kshirsagar NA, Gogtay NJ, Garg BS, Deshmukh PR, Rajgor DD, Kadam VS, et al. Efficacy and tolerability of treatment with single doses of diethylcarbamazine (DEC) and DEC plus albendazole (ABZ) for three consecutive years in lymphatic filariasis: a field study in India. Parasitol Res. 2017. doi: 10.1007/s00436-017-5577-9 . [DOI] [PubMed] [Google Scholar]
- 90.Cartel JL, Moulia-Pelat JP, Glaziou P, Nguyen LN, Chanteau S, Roux JF. Results of a safety trial on single-dose treatments with 400 mcg/kg of ivermectin in bancroftian filariasis. Trop Med Parasitol. 1992;43(4):263–6. . [PubMed] [Google Scholar]
- 91.Yongyuth P, Koyadun S, Jaturabundit N, Jariyahuttakij W, Bhumiratana A. Adverse reactions of 300 MG diethylcarbamazine, and in a combination of 400 MG albendazole, for a mass annual single dose treatment, in migrant workers in Phang Nga province. J Med Assoc Thai. 2007;90(3):552–63. . [PubMed] [Google Scholar]
- 92.Gunawardena S, Sri Ranganathan S, Fernandopulle R. Pharmacovigilance through consumer feedback (reporting) in the mass treatment of lymphatic filariasis using diethylcarbamazine and albendazole in two districts of Sri Lanka. Tropical medicine & international health: TM & IH. 2008;13(9):1153–8. doi: 10.1111/j.1365-3156.2008.02120.x . [DOI] [PubMed] [Google Scholar]
- 93.Cartel JL, Spiegel A, Nguyen L, Genelle B, Roux JF. Double blind study on efficacy and safety of single doses of ivermectin and diethylcarbamazine for treatment of Polynesian Wuchereria bancrofti carriers. Results at six months. Trop Med Parasitol. 1991;42(1):38–40. . [PubMed] [Google Scholar]
- 94.Moulia-Pelat JP, Nguyen LN, Glaziou P, Chanteau S, Gay VM, Martin PM, et al. Safety trial of single-dose treatments with a combination of ivermectin and diethylcarbamazine in bancroftian filariasis. Trop Med Parasitol. 1993;44(2):79–82. . [PubMed] [Google Scholar]
- 95.Andrade LD, Medeiros Z, Pires ML, Pimentel A, Rocha A, Figueredo-Silva J, et al. Comparative efficacy of three different diethylcarbamazine regimens in lymphatic filariasis. Trans R Soc Trop Med Hyg. 1995;89(3):319–21. . [DOI] [PubMed] [Google Scholar]
- 96.Cartel JL, Spiegel A, Nguyen L, Plichart R, Martin PM, Roux JF. The treatment of microfilaremia due to Wuchereria bancrofti var. pacifica: ivermectin versus diethylcarbamazine. Ann Soc Belg Med Trop. 1991;71(3):229–36. . [PubMed] [Google Scholar]
- 97.Eberhard ML, Hightower AW, McNeeley DF, Lammie PJ. Long-term suppression of microfilaraemia following ivermectin treatment. Trans R Soc Trop Med Hyg. 1992;86(3):287–8. . [DOI] [PubMed] [Google Scholar]
- 98.Addiss DG, Eberhard ML, Lammie PJ, McNeeley MB, Lee SH, McNeeley DF, et al. Comparative efficacy of clearing-dose and single high-dose ivermectin and diethylcarbamazine against Wuchereria bancrofti microfilaremia. Am J Trop Med Hyg. 1993;48(2):178–85. . [DOI] [PubMed] [Google Scholar]
- 99.Hochberg N, Michel MC, Lammie PJ, Mathieu E, Direny AN, De Rochars MB, et al. Symptoms reported after mass drug administration for lymphatic filariasis in Leogane, Haiti. Am J Trop Med Hyg. 2006;75(5):928–32. . [PubMed] [Google Scholar]
- 100.Cross HF, Haarbrink M, Egerton G, Yazdanbakhsh M, Taylor MJ. Severe reactions to filarial chemotherapy and release of Wolbachia endosymbionts into blood. Lancet. 2001;358(9296):1873–5. doi: 10.1016/S0140-6736(01)06899-4 . [DOI] [PubMed] [Google Scholar]
- 101.Taylor MJ, Cross HF, Bilo K. Inflammatory responses induced by the filarial nematode Brugia malayi are mediated by lipopolysaccharide-like activity from endosymbiotic Wolbachia bacteria. J Exp Med. 2000;191(8):1429–36. ; PubMed Central PMCID: PMC2193140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Taylor MJ, Cross HF, Ford L, Makunde WH, Prasad GB, Bilo K. Wolbachia bacteria in filarial immunity and disease. Parasite Immunol. 2001;23(7):401–9. . [DOI] [PubMed] [Google Scholar]
- 103.Foster JM, Kumar S, Ganatra MB, Kamal IH, Ware J, Ingram J, et al. Construction of bacterial artificial chromosome libraries from the parasitic nematode Brugia malayi and physical mapping of the genome of its Wolbachia endosymbiont. Int J Parasitol. 2004;34(6):733–46. doi: 10.1016/j.ijpara.2004.02.001 . [DOI] [PubMed] [Google Scholar]
- 104.Foster J, Ganatra M, Kamal I, Ware J, Makarova K, Ivanova N, et al. The Wolbachia genome of Brugia malayi: endosymbiont evolution within a human pathogenic nematode. PLoS Biol. 2005;3(4):e121 doi: 10.1371/journal.pbio.0030121 ; PubMed Central PMCID: PMC1069646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Turner JD, Langley RS, Johnston KL, Gentil K, Ford L, Wu B, et al. Wolbachia lipoprotein stimulates innate and adaptive immunity through Toll-like receptors 2 and 6 to induce disease manifestations of filariasis. J Biol Chem. 2009;284(33):22364–78. doi: 10.1074/jbc.M901528200 ; PubMed Central PMCID: PMC2755959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Voronin D, Guimaraes AF, Molyneux GR, Johnston KL, Ford L, Taylor MJ. Wolbachia lipoproteins: abundance, localisation and serology of Wolbachia peptidoglycan associated lipoprotein and the Type IV Secretion System component, VirB6 from Brugia malayi and Aedes albopictus. Parasit Vectors. 2014;7:462 doi: 10.1186/s13071-014-0462-1 ; PubMed Central PMCID: PMC4197220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Supali T, Djuardi Y, Pfarr KM, Wibowo H, Taylor MJ, Hoerauf A, et al. Doxycycline treatment of Brugia malayi-infected persons reduces microfilaremia and adverse reactions after diethylcarbamazine and albendazole treatment. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2008;46(9):1385–93. doi: 10.1086/586753 . [DOI] [PubMed] [Google Scholar]
- 108.Turner JD, Mand S, Debrah AY, Muehlfeld J, Pfarr K, McGarry HF, et al. A randomized, double-blind clinical trial of a 3-week course of doxycycline plus albendazole and ivermectin for the treatment of Wuchereria bancrofti infection. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2006;42(8):1081–9. doi: 10.1086/501351 . [DOI] [PubMed] [Google Scholar]
- 109.Sanprasert V, Sujariyakul A, Nuchprayoon S. A single dose of doxycycline in combination with diethylcarbamazine for treatment of bancroftian filariasis. Southeast Asian J Trop Med Public Health. 2010;41(4):800–12. . [PubMed] [Google Scholar]
- 110.Mand S, Pfarr K, Sahoo PK, Satapathy AK, Specht S, Klarmann U, et al. Macrofilaricidal activity and amelioration of lymphatic pathology in bancroftian filariasis after 3 weeks of doxycycline followed by single-dose diethylcarbamazine. Am J Trop Med Hyg. 2009;81(4):702–11. doi: 10.4269/ajtmh.2009.09-0155 . [DOI] [PubMed] [Google Scholar]
- 111.Stanilova SA, Slavov ES. Comparative study of circulating immune complexes quantity detection by three assays—CIF-ELISA, C1q-ELISA and anti-C3 ELISA. J Immunol Methods. 2001;253(1–2):13–21. . [DOI] [PubMed] [Google Scholar]
- 112.Ramaprasad P, Prasad GB, Harinath BC. Microfilaraemia, filarial antibody, antigen and immune complex levels in human filariasis before, during and after DEC therapy. A two-year follow-up. Acta Trop. 1988;45(3):245–55. . [PubMed] [Google Scholar]
- 113.Zheng HJ, Tao ZH, Cheng WF, Wang SH, Cheng SH, Ye YM, et al. Efficacy of ivermectin for control of microfilaremia recurring after treatment with diethylcarbamazine. II. Immunologic changes following treatment. Am J Trop Med Hyg. 1991;45(2):175–81. . [PubMed] [Google Scholar]
- 114.Cartel JL, Celerier P, Spiegel A, Burucoa C, Roux JF. A single diethylcarbamazine dose for treatment of Wuchereria bancrofti carriers in French Polynesia: efficacy and side effects. Southeast Asian J Trop Med Public Health. 1990;21(3):465–70. . [PubMed] [Google Scholar]
- 115.Cartel JL, Spiegel A, Nguyen L, Moulia-Pelat JP, Martin PM, Roux JF. [Comparative efficacy of annual and semi-annual doses of ivermectin or diethylcarbamazine for the prevention of lymphatic filariasis]. Rev Epidemiol Sante Publique. 1992;40(5):307–12. . [PubMed] [Google Scholar]
- 116.Pani SP, Reddy GS, Vanamail P, Venkatesvarlou N, Das LK, Vijayan AP. Tolerability and efficacy of single dose diethylcarbamazine (DEC) alone or co-administration with Ivermectin in the clearance of Wuchereria bancrofti microfilaraemia in Pondicherry, South India. The Journal of communicable diseases. 2004;36(4):240–50. Epub 2006/03/02. . [PubMed] [Google Scholar]
- 117.Shenoy RK, Suma TK, John A, Arun SR, Kumaraswami V, Fleckenstein LL, et al. The pharmacokinetics, safety and tolerability of the co-administration of diethylcarbamazine and albendazole. Ann Trop Med Parasitol. 2002;96(6):603–14. doi: 10.1179/000349802125001663 . [DOI] [PubMed] [Google Scholar]
- 118.Makunde WH, Kamugisha LM, Massaga JJ, Makunde RW, Savael ZX, Akida J, et al. Treatment of co-infection with bancroftian filariasis and onchocerciasis: a safety and efficacy study of albendazole with ivermectin compared to treatment of single infection with bancroftian filariasis. Filaria J. 2003;2(1):15 doi: 10.1186/1475-2883-2-15 ; PubMed Central PMCID: PMCPMC293471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Dreyer G, Noroes J, Amaral F, Nen A, Medeiros Z, Coutinho A, et al. Direct assessment of the adulticidal efficacy of a single dose of ivermectin in bancroftian filariasis. Trans R Soc Trop Med Hyg. 1995;89(4):441–3. . [DOI] [PubMed] [Google Scholar]
- 120.Dunyo SK, Nkrumah FK, Simonsen PE. A randomized double-blind placebo-controlled field trial of ivermectin and albendazole alone and in combination for the treatment of lymphatic filariasis in Ghana. Trans R Soc Trop Med Hyg. 2000;94(2):205–11. . [DOI] [PubMed] [Google Scholar]
- 121.Kshirsagar NA, Gogtay NJ, Garg BS, Deshmukh PR, Rajgor DD, Kadam VS, et al. Safety, tolerability, efficacy and plasma concentrations of diethylcarbamazine and albendazole co-administration in a field study in an area endemic for lymphatic filariasis in India. Trans R Soc Trop Med Hyg. 2004;98(4):205–17. . [DOI] [PubMed] [Google Scholar]
- 122.Panicker KN, Krishnamoorthy K, Sabesan S, Prathiba J, Abidha. Comparison of effects of mass annual and biannual single dose therapy with diethylcarbamazine for the control of Malayan filariasis. Southeast Asian J Trop Med Public Health. 1991;22(3):402–11. . [PubMed] [Google Scholar]
- 123.Bockarie MJ, Tisch DJ, Kastens W, Alexander ND, Dimber Z, Bockarie F, et al. Mass treatment to eliminate filariasis in Papua New Guinea. N Engl J Med. 2002;347(23):1841–8. doi: 10.1056/NEJMoa021309 . [DOI] [PubMed] [Google Scholar]
- 124.Makunde WH, Kamugisha LM, Makunde RA, Malecela MN, Kitua AY. Hospital-based safety and tolerability study to assess efficacy of oral doxycycline in the treatment of Wuchereria bancrofti infection in north-eastern Tanzania. Tanzania health research bulletin. 2006;8(3):128–33. Epub 2008/02/08. . [DOI] [PubMed] [Google Scholar]
- 125.Anto F, Asoala V, Anyorigiya T, Oduro A, Adjuik M, Akweongo P, et al. Simultaneous administration of praziquantel, ivermectin and albendazole, in a community in rural northern Ghana endemic for schistosomiasis, onchocerciasis and lymphatic filariasis. Tropical medicine & international health: TM & IH. 2011;16(9):1112–9. doi: 10.1111/j.1365-3156.2011.02814.x . [DOI] [PubMed] [Google Scholar]
- 126.Wamae CN, Njenga SM, Ngugi BM, Mbui J, Njaanake HK. Evaluation of effectiveness of diethylcarbamazine/albendazole combination in reduction of Wuchereria bancrofti infection using multiple infection parameters. Acta Trop. 2011;120 Suppl 1:S33–8. doi: 10.1016/j.actatropica.2010.09.009 . [DOI] [PubMed] [Google Scholar]
- 127.Dembele B, Coulibaly YI, Dolo H, Konate S, Coulibaly SY, Sanogo D, et al. Use of high-dose, twice-yearly albendazole and ivermectin to suppress Wuchereria bancrofti microfilarial levels. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2010;51(11):1229–35. doi: 10.1086/657063 ; PubMed Central PMCID: PMCPMC3106228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lineberry N, Berlin JA, Mansi B, Glasser S, Berkwits M, Klem C, et al. Recommendations to improve adverse event reporting in clinical trial publications: a joint pharmaceutical industry/journal editor perspective. BMJ (Clinical research ed). 2016;355:i5078 Epub 2016/10/05. doi: 10.1136/bmj.i5078 . [DOI] [PubMed] [Google Scholar]
- 129.Ioannidis JA, Evans SW, Gøtzsche PC, et al. Better reporting of harms in randomized trials: An extension of the consort statement. Annals of Internal Medicine. 2004;141(10):781–8. doi: 10.7326/0003-4819-141-10-200411160-00009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(XLSX)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.