Abstract
Despite the recognition that behavioral and medical health conditions are frequently intertwined, the existing health care system divides management for these issues into separate settings. This separation results in increased barriers to receipt of care and contributes to problems of under-detection, inappropriate diagnosis, and lack of treatment engagement. Adolescents and young adults with mental health conditions have some of the lowest rates of treatment for their conditions of all age groups. Integration of behavioral health into primary care settings has the potential to address these barriers and improve outcomes for adolescents and young adults. In this paper, we review the current research literature for behavioral health integration in the adolescent and young adult population and make recommendations for needed research to move the field forward.
Introduction
In the United States, approximately 20% of adolescents and young adults have a mental health or substance misuse disorder,1–3 and these disorders account for a significant portion of the burden of disability for individuals in this age group.4 These behavioral disorders are associated with other areas of risk including higher rates of suicide,5 injury,6 risky sexual activity and unwanted pregnancy,7,8 and low educational or work achievement.9 Despite the recognition of the significant short and long-term impacts of behavioral health disorders on development, and the availability of effective treatments, only about one-third of adolescents with a diagnosable behavioral disorder receive appropriate care.10 Rates of mental health treatment decrease further as adolescents transition into young adulthood.11 Of particular concern, only half of adolescents who meet criteria for “severe” impairment from a mental health disorder report having received care10 and only 40% of 18–25 year olds with a serious mental illness that impairs functioning report receiving treatment.12 On average, 10 years pass from the initial onset of a mental health disorder and seeking treatment, with younger age at onset associated with longer delays in treatment.13
One approach to reducing delay in treatment and improving treatment delivery is the development of models aimed at improving recognition and treatment for behavioral health disorders in primary care settings through the integration of behavioral health services into medical settings.14–16 In the United States, it is estimated that 84% of adolescents have an outpatient visit and 66% have a well check-up annually17 and 70% of young adults report having a source of primary care.18 Among adolescents who are seen in primary care settings, 14–38% have been found to meet criteria for a mental health disorder.19–21 Several studies have also shown high rates of mental health comorbidity among individuals with chronic medical illnesses commonly seen in primary care,22,23 which when present, is associated with higher levels of medical symptom burden,24–26 health care costs,24 and worse medical outcomes.27 A recent meta-analysis of integrated behavioral health trials across pediatric age groups found that they had a small to moderate effect improving the outcomes of mental health and substance use disorders (d=042; 95% CI, 0.29–0.55, p<0.001).28 Thus, the integration of care has the potential to improve outcomes for both behavioral and physical health. In this article, we aim to specifically review research regarding models of integrated behavioral health in primary care settings among adolescent and young adult populations with the aim of describing needed areas of research.
Review of the Literature
To assess the current state of the literature, we conducted a systematic review of the literature using MEDLINE and PsycINFO to identify research studies examining integrated behavioral health interventions for the treatment of mental health and substance use disorders among adolescent and young adult populations in primary care settings. Literature searches contained four categories of search terms, all of which were joined by “and” conditions:
Age group designation: "adolescent", “young adult”, or “college”
Variations of integration and/or setting: “primary care”, “school”, “collaborative care”, “integrated care”, or “coordinated care”
Variations of “mental health care”, “psychotherapy”, “behavioral health”, or “mental health”
Variations of diagnosis: “depression”, “anxiety”, “disruptive behavior”, “eating disorder” or “substance”
To be included, studies had to be focused on older adolescents and/or young adults (study population predominantly within the age range of 13–25 years), examine patient outcomes, have a comparison group, offer a an integrated or health care provider-led intervention for a behavioral health condition in primary care, be published in English, and be conducted in 2004 or later. Studies of adult populations that did not specifically examine young adults separate from the older adult population were not included. For the purposes of this review, we considered school-based health clinics and college health clinics to be primary care settings. We excluded studies that recruited from the primary care setting but did not have evidence of collaboration or care delivered in that setting, as well as those conducted in the broader school setting such as classroom or campus-wide interventions. We only included those focused on treatment or secondary prevention in at-risk individuals. As the intent was to look at alcohol and illicit drug misuse, tobacco use interventions were not included.
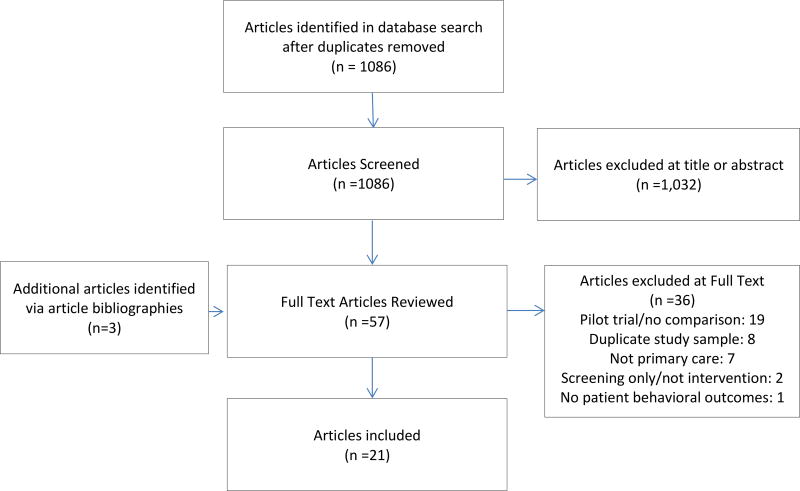
In total, when duplicates were excluded, the systematic searches identified 1,086 potential articles of which 1,032 did not meet inclusion criteria based on review of the title or abstract (Figure 1). We conducted full text article reviews for the remaining 54 articles plus an additional 3 articles identified via bibliographies of identified literature for a total of 57. Of these 57, 36 articles were excluded. The reasons for exclusion included: pilot or feasibility trial with no comparison group (19 studies), repeat use of a study sample without the presentation of new patient outcomes (8 studies), intervention not in a primary care setting (7 studies), not intervention trial (2), and no behavioral outcomes provided (1). Based on full text review, 21 trials were identified for inclusion. As detailed in Table 2, studies meeting inclusion criteria were conducted in multiple countries including the U.S. (N=10), Australia (N=3), New Zealand (N=3), South Africa (N=1), and multiple countries (N=2, US and Canada, and US and Czech Republic). All included studies were reviewed for quality by two independent reviewers using the US Preventive Services Task Force Quality Rating Criteria for Randomized Controlled Trials and Cohort Study Criteria (accessed in Appendix C by Goy et al.29). Differences in scores were subsequently reconciled via discussion between reviewers.
Figure 1.
Literature Review Flowchart
Table 2.
Collaborative Care Categorization Overview
| Coordinated | Co-Located | Integrated |
|---|---|---|
|
| ||
|
|
|
To promote accurate comparison, studies identified in our review were organized into three groups with increasing levels of integration. Groups were determined a priori based on the framework outlined in the 2010 report on Evolving Models of Behavioral Health Integration in Primary Care: “coordinated care”, “co-located care”, and “integrated care” (briefly described below and as outlined in Table 1).30,31 In “coordinated care models”, primary care providers work with community-based behavioral health specialists to provide care. The behavioral health specialist may serve as an advisor to the primary care provider without seeing the patient or can provide direct care with a coordinated exchange of information. Educational interventions that aim to enhance primary care provider skills with support and oversight by mental health providers also fit into this category. In “co-located care models”, primary care and behavioral health providers are located in the same setting to simplify the referral process, enhance communication between providers, and remove patient barriers to care. “Integrated care” refers to models of care with a shared treatment plan between providers with both behavioral and health elements. These models often involve a multidisciplinary team working together using a pre-defined protocol and a “population-based approach” to tracking outcomes in order to assure improvement for the entire patient panel.
Table 2.
Summary of Articles Included in Literature Review (Organized by condition treated and level of evidence)
| Study (Country) |
N | Youth Age Range |
Intervention Target |
Intervention Description |
Comparison condition |
Follow- Up |
Main Outcomes | Quality Rating |
|---|---|---|---|---|---|---|---|---|
| Coordinated Care Models | ||||||||
| Wissow et al., 200832 (US) | 418 | 5–16 years | Behavioral and mood problems | Primary care provider training in mental health communication skills in order to use skills at child wellness or other visits | Usual care | 6 months | Intervention associated with greater reductions in impairment among minority but not white youth. No changes noted in youth symptoms but intervention was associated with a decrease in parent symptoms. | Good |
| Werch et al., 2007 (US)38 | 155 | College Students (mean age 19 years) | Health behaviors and beliefs | Three comparison conditions:
|
Comparison between three arms, no no-treatment cohort | 1 month | Groups receiving consultation reported increased rates of physical activity, nutrition, and sleep as well as reductions in drinking and driving behaviors. | Fair |
| Borowsky et al., 2004 (US)39 | 224 | 7–15 years | Violence | Screening with physician feedback. Optional telephone-based parenting program delivered by parent-educator | Usual care | 9 months | Intervention associated with reductions in aggressive and delinquent behaviors and attention problems. Parents also reported less child bullying and physical fighting. | Good |
| Walton et al., 2013 (US)43 | 328 | 12–18 years | Cannabis use | Computerized brief intervention based on motivational interviewing with or without therapist facilitation | Usual care plus informational brochure and websites | 3, 6 & 12 months | Intervention associated with reduced cannabis-related problems and reduced other drug use (3 & 6 months) but not with reductions in cannabis or alcohol use. | Good |
| Kypri et al., 2004 (New Zealand)41 | 104 | 17–26 years | Alcohol Use | Web-based assessment and personalized feedback on alcohol use | Information pamphlet | 6 weeks & 6 months | Intervention associated with reduced total alcohol consumption at 6 weeks but not 6 months, as well as reduced personal problems and academic problems (6 months only) | Good |
| Kypri et al., 2008 (New Zealand)42 | 576 | 17–29 years | Alcohol use | Web-based motivational intervention in:
|
Information pamphlet | 6 & 12 months | Single dose intervention associated with reduced total alcohol consumption and academic problems. Similar results for three dose intervention. | Good |
| Mertens et al., 2014 (South Africa)36 | 403 | 18–24 years | Substance use | Single session brief motivational interviewing with a nurse practitioner plus referral resources | Usual care plus list of referral resources | 3 months | Intervention youth had significant reductions in alcohol use scores but not at-risk use of alcohol or marijuana. | Good |
| Fleming et al., 2010 (US & Canada)37 | 986 | College students ≥18 years | Substance use | Brief motivational interviewing - two 15-minute sessions with a physician and two follow-up calls | Booklet on general health issues | 12 months | Intervention associated with reduced 28-day alcohol use and alcohol problem index. No reduction in binge drinking, health care utilization, injuries, drunk driving, depression or tobacco use. | Good |
| Mason et al., 2011 (US)34 | 28 | 14–18 years, all female | Substance use | Single 20-minute session including brief motivational interviewing and social network counseling | No treatment | 1 month | Intervention associated with reduced use of substances prior to sex and reported trouble due to alcohol use | Good |
| Hides et al., 2013 (Australia)35 | 61 | 16–25 years | Substance use in youth receiving care for anxiety or depression | Brief Motivational interviewing - two to three 1-hour sessions | One-time assessment with feedback session | 6 months | Intervention associated with significantly reduced alcohol use, cannabis use, and psychological distress | Fair |
| Harris et al., 2012 (US & Czech Republic)40 | 2106 (US) 589 (CZ) | 12–18 years | Substance use | Computer-facilitated screening and feedback for youth, plus provider led brief advice based on results | Usual care (asynchronous) | 12 months | Intervention associated with significantly reduced alcohol use (US sample only) and marijuana use (Czech sample only) | Fair |
| D’Amico et al., 2008 (US)33 | 42 | 12–18 years | Reduction in substance use among high risk youth | Brief motivational interviewing intervention during a primary care visit, with telephone follow-up | Usual Care | 3 months | Intervention associated with significant reductions in marijuana use and non-significant reductions in alcohol use | Poor |
| Reid et al., 2011 (Australia)44 Reid et al., 2013 (Australia)45 | 118 | 14–24 years | Depression | Use of a phone app to collect data on mood, stress, coping, activities, eating, sleeping, exercise, and substance use for physician review during follow-up | Attention control | 6 weeks & 6 months | Intervention associated with increased provider understanding of mental health and patient emotional self awareness and decreased overall mental health symptoms. No significant reductions in depressive or other mental health disorders. | Fair |
| Merry et al., 2012 (New Zealand)46 | 187 | 12–19 years | Depression | Internet-based cognitive behavioral therapy intervention designed as a fantasy game | Usual care (89% received treatment with psychotherapy or medications) | 2 & 3 months | Intervention associated with reductions in depressive symptoms similar to usual care group and higher rates of depression remission. | Good |
| Van Vorhees et al., 2008 (US)47 Van Vorhees et al., 2009 (US)48 | 84 | 14–21 years | Secondary depression prevention among adolescents with sub-threshold symptoms | Brief motivational interviewing with provider followed by participation in an internet preventive intervention (14 modules) | Brief advice (2–3 minutes) + internet preventive intervention (14 modules) | 4–8, 12 weeks | Both groups experienced declines in depressive symptoms, increases in social support by peers, and reductions in depression-related impairment at school. The motivational interviewing group was significantly less likely to experience a depressive episode or report hopelessness by 12 weeks. | Fair |
| Banasiak et al., 2005 (Australia)49 | 109 | 18 years and older (mean age 29.5 yrs) | Bulimia Nervosa | Modified cognitive behavioral therapy self-help manual guided by brief sessions with a specialist or non-specialist health professional. | Delayed treatment control | 6 months | Intervention associated with significant improvements in psychological and bulimic symptom scales, reduced frequency of mean binge eating episodes, and greater remission of eating disordered behaviors. | Fair |
| Walsh et al., 2004 (US)50 | 91 | 18–60 years (mean age 30.6 years) | Bulimia Nervosa | Fluoxetine alone, Fluoxetine plus guided cognitive behavioral therapy self-help book, or Placebo plus guided cognitive behavioral therapy self-help book | Placebo alone | 3–4 months | Participants receiving fluoxetine had reduced binge eating and vomiting episodes and a greater improvement in psychological symptoms. There was no benefit noted from self-help book. High rate of treatment drop out in both arms. | Poor |
| Integrated Care Models | ||||||||
| Asarnow et al., 2005 (US)54 | 418 | 13–21 years | Depression | Quality improvement intervention including depression care management, patient and provider choice of meds, cognitive behavioral therapy, or both | Enhanced usual care | 6 months | Intervention associated with significantly improved receipt of treatment, depressive symptoms, mental health related quality of life, and satisfaction with care. | Good |
| Richardson et al., 2014 (US)53 | 101 | 13–17 years | Depression | Collaborative care intervention delivered by depression care management, patient and family choice of meds, cognitive behavioral therapy or both; stepped care algorithms and psychiatric supervision | Enhanced usual care | 6 & 12 months | Intervention associated with significantly improved receipt of treatment, depressive symptoms, and functional status as well as higher rates of depression remission. | Good |
| Clarke et al., 2005 (US)55 | 152 | 12–18 years | Depression | Cognitive behavioral therapy intervention provided by therapist in conjunction with primary provider-prescribed antidepressant | Medications alone | 12 weeks | Intervention associated with non-significant reduction in depressive symptoms | Good |
| Mufson et al. 200456 | 63 | 12–18 years | Depression | Interpersonal psychotherapy intervention provided by a therapist in school-based health clinic | Treatment as usual | 12 weeks | Intervention associated with reduction in depressive symptoms compared to treatment as usual | Good |
Our review identified a total of 21 randomized controlled trials with behavioral health outcome measurement among adolescents and young adults: 17 in the category of “coordinated care”, 0 in the category of “co-located care”, and 4 in the category of “integrated care”. Results are discussed by category below and details of specific studies within each category are provided in Table 2.
“Coordinated Care” Research
Our review identified 17 studies meeting the criteria for “coordinated care”. Eight studies described interventions in which enhanced behavioral health care was provided by the primary care provider.32–39 One study examined provider communication skills training aimed at increasing patient and family engagement in behavioral health care and found improvements in parent-reported child functioning for minority, but not White, youth.32 Five studies examined the effectiveness of provider training in screening, brief motivational interviewing, and referral for substance misuse among adolescent33,34and young adult populations35–37and found the use of these methods to be effective in reducing alcohol or other substance misuse, increasing patient’s readiness to change substance misuse behaviors and/or decreasing consequences of substance misuse. One additional study found that training providers to implement a behavioral health contract paired with consultation among college students reduced the frequency of drinking and driving but not overall substance misuse.38 A final study found that screening coupled with access to a telephone-based parenting intervention was associated with reductions in child aggressive and delinquent behaviors and attention problems.39
Seven studies examined technological approaches to providing behavioral health care in the primary care setting.40–48 Four examined computer-facilitated brief intervention for substance misuse for adolescent and young adults either with40 or without41–43 brief advice from the primary care provider and found such strategies to be effective in reducing substance misuse. In one of these studies, even a single dose of computer-facilitated motivational interviewing showed sustained effects for a year.42 The remaining three studies used technological interventions to improve outcomes for depression. One study examined the use of mobile health symptom-tracking technology for adolescent and young adult depression and found significant improvements in provider-reported skills and patient-reported emotional self-awareness but not in mental health outcomes or treatment engagement.44,45 The second study found a cognitive behavioral therapy-informed computer game to have comparable effectiveness to in-person counseling in reducing depressive symptoms among adolescents.46 The third study found that adolescents with depressive symptoms who received motivational interviewing from their providers were more likely to participate in a web-based cognitive behavioral therapy program designed to prevent worsening of symptoms than those who received only brief advice.47,48
Finally, there were two studies employing the integration of self-administered manualized cognitive behavioral therapy into primary care management of Bulimia Nervosa among predominantly young adult women.49,50 In one study, manualized treatment was associated with significant reductions in bulimic behaviors compared to wait-listed controls.49 The second study did not find any reductions in bulimic behaviors associated with the manualized treatment, but did find reductions in bulimic behaviors among individuals in medication treatment arms.50
“Co-Located Care” Research
Our search did not identify any randomized trials examining outcomes for “co-located care” models. We found only two studies that examined behavioral outcomes for youth receiving “co-located care”, both used technological solutions to create virtual co-location and are included here for reference. One retrospective study of a convenience sample of youth who had received a telehealth behavioral consultation found improved behavioral outcomes at 3 months post-consultation.51 Additionally, a large cohort study of the provision of telephone access to mental health specialists in primary care found high rates of completion of recommended mental health consultation and reduced symptoms over time for referred youth.52
“Integrated Care” Research
We identified four studies meeting the criteria of “integrated care” in the adolescent and young adult age group all of which focused on adolescent depression.53–56 Two studies examined adaptations of adult collaborative care models and involved depression care managers in primary care practices who helped primary care providers with depression assessment, symptom tracking, evidence-based treatment delivery, and advancement of treatment based on pre-specified algorithms and with input from psychiatric consultants. Both found that the collaborative care was associated with increased treatment engagement and significantly improved outcomes for depression among adolescents compared to usual care.53,54 A third study examined the addition of a brief psychotherapy protocol for antidepressant-treated adolescents in primary care and found that psychotherapy was associated with only mild non-significant reductions in depressive symptoms.55 The authors noted that youth in the intervention arm were more likely to choose to prematurely discontinue antidepressants than those receiving usual care and hypothesized that this discontinuation may have attenuated the effects of the intervention. The final study examined the integration of interpersonal therapy delivered by trained therapists for teens with depression seen in the school-based health clinic setting. They found benefit of interpersonal psychotherapy over treatment as usual particularly in youth with high levels of conflict with mothers and social dysfunction with friends.56
Discussion and Recommendations
While behavioral health disorders have a significant impact on the functioning and impairment of adolescents and young adults, our literature review revealed a relatively small number of research studies testing behavioral health integration in this population. This limited body of literature is particularly surprising in light of the extensive array of collaborative care studies addressing these conditions in adult populations57–59 and points to the need for further development and testing of interventions among the adolescent and young adult populations. Our review also identified several gaps in the literature in which research would be beneficial in moving the field forward.
First, more high quality research is needed in the implementation of integrated care models for the behavioral health conditions that most commonly occur among adolescents and young adults. A recent Cochrane review identified 79 randomized controlled trials of integrated care models for depression and anxiety among adult populations with overwhelming evidence for effectiveness in reducing depression and anxiety symptoms.58 In contrast, our search revealed only three randomized controlled trial studies of integrated care models among adolescents, all of which focused on depression. We did not identify any randomized controlled trials addressing behavioral health integration for anxiety, the most prevalent disorder during adolescence, nor eating disorders among adolescents which are often medically managed in primary care. Similarly, although integrated care models have been tested among younger children with attention deficit disorder,60–63 studies have not included adolescents above age 13 or young adults. Additional opportunities for new research areas include: examining effectiveness of brief interventions developed for primary care administration in adult settings among adolescent and young adult populations, evaluation of technological strategies to increase access to psychotherapy in primary care, and improved models for the primary care integration of web-based psychotherapy methods that have been shown to be effective for depression and anxiety in adolescent and young adult populations.64
Our review also suggested the need for more research addressing how developmental stage affects the types of needed supports and interventions. Prior research suggests that developmental factors can influence the presentation of mental health symptoms, the ability to be independent in care, the impact of stigma, and the efficacy of particular types of interventions.65–67 For younger teens, parents are often the ones initiating care which may influence interest and engagement in treatment interventions.68–70 The studies in our review differed in the range of included ages and none were designed with adequate numbers to explore if the intervention was similarly effective across developmental stage. Future studies should address this gap and examine if there are consistent patterns to the types of components (e.g. parental engagement, behavioral skills) required at different ages. One notable area of absence of developmental information was in the young adult population. While most adult studies include individuals who are 18 and older, our search identified relatively few studies in which integrated behavioral health care was specifically examined in young adults, most of which were focused on substance use in college health settings.36–38,41,42,44,49,50 However, compared to older adults, young adults have little experience in navigating the system to reach care.18 More research is needed to determine if existing adult collaborative care models are reaching and meeting the needs of this population.
Additionally, more research is needed to identify key strategies to facilitate the dissemination of behavioral health integration models that have been found to be effective in randomized trials into actual primary care practice in the US. There is good evidence for the effectiveness of integrated care for depression53–56 and brief motivational interviewing for substance misuse34,41,42,71 (especially when combined with what is known in the adult literature) but significant work still exists in adopting these programs into practice under the current funding system. While our review did identify descriptive papers of large-scale implementation projects,51,52 they did not include rigorous patient-level outcome assessments or comparison groups. In the US health care system, the funding of activities related to care management and psychiatric supervision have been a particular challenge that will require creative solutions and might benefit from more research. In a recent survey, clinicians identified lack of resources as a key barrier to implementing integrated care plans in Medical Homes.72 Finally, integrated care practice requires specific skills among providers including shared management plans, group case supervision by psychiatrists, and training for depression care managers. Further investigation is needed on how to train providers for these skills possibly taking an earlier approach to multidisciplinary training between behavioral health and medical trainees.
The field of adolescent and young adult health care is rapidly shifting in ways that may create new opportunities for improving behavioral health outcomes for this population. The Affordable Care Act opens new opportunities to serve young adults through expansion of health insurance coverage.73,74 The Patient-Centered Medical Home model aims to reduce the cost of health care and improve patient experience and population health through the integration of needed services, such as behavioral health, into a single setting.15 School-based health clinics and college health clinics may provide new opportunities to test models that integrate educational and other social supports.75 By expanding our research in integrated care among adolescents and young adults, we will be positioned well to maximize these new opportunities and to improve key behavioral health outcomes.
Implications and Contribution.
Although behavioral health conditions are common sources of morbidity among adolescents and young adults, research in these populations lags behind research in older age groups. This article is the first to specifically examine integrated care research in this age group and to suggest important directions to move the field forward.
Acknowledgments
The authors would like to acknowledge Peter Scal MD, MPH for his contribution to the conceptualization of this paper, Garret Zieve for his assistance in critical review of the literature, and Elizabeth Ozer, PhD and Robin Harwood, PhD for providing input on the overall content of the paper and critically reviewing the final manuscript. This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UA6MC27378 for $960,000. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
Bibliography
- 1.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kessler RC, Avenevoli S, Costello EJ, et al. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psychiatry. 2012;69(4):372–380. doi: 10.1001/archgenpsychiatry.2011.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stroud C, Mainero T, Olson T. Improving the Health, Safety and Well-being of Young Adults: Workshop Summary. Washington D.C.: 2013. [PubMed] [Google Scholar]
- 5.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marcus SC, Wan GJ, Zhang HF, Olfson M. Injury among stimulant-treated youth with ADHD. J Atten Disord. 2008;12(1):64–69. doi: 10.1177/1087054707305168. [DOI] [PubMed] [Google Scholar]
- 7.Bardone AM, Moffitt TE, Caspi A, Dickson N, Stanton WR, Silva PA. Adult physical health outcomes of adolescent girls with conduct disorder, depression, and anxiety. J Am Acad Child Adolesc Psychiatry. 1998;37(6):594–601. doi: 10.1097/00004583-199806000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Waller MW, Hallfors DD, Halpern CT, Iritani BJ, Ford CA, Guo G. Gender differences in associations between depressive symptoms and patterns of substance use and risky sexual behavior among a nationally representative sample of U.S. adolescents. Arch Womens Ment Health. 2006;9(3):139–150. doi: 10.1007/s00737-006-0121-4. [DOI] [PubMed] [Google Scholar]
- 9.Needham BL. Adolescent depressive symptomatology and young adult educational attainment: an examination of gender differences. J Adolesc Health. 2009;45(2):179–186. doi: 10.1016/j.jadohealth.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 10.Merikangas KR, He JP, Burstein M, et al. Service utilization for lifetime mental disorders in U.S. adolescents: results of the National Comorbidity Survey-Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2011;50(1):32–45. doi: 10.1016/j.jaac.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Copeland WE, Shanahan L, Davis M, Burns BJ, Angold A, Costello EJ. Increase in untreated cases of psychiatric disorders during the transition to adulthood. Psychiatr Serv. 2015;66(4):397–403. doi: 10.1176/appi.ps.201300541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. [Accessed 8/17/2015];National Institutes of Health. http://www.nimh.nih.gov/health/statistics/prevalence/use-of-mental-health-services-and-treatment-among-adults.shtml.
- 13.Wang PS, Berglund PA, Olfson M, Kessler RC. Delays in initial treatment contact after first onset of a mental disorder. Health Serv Res. 2004;39(2):393–415. doi: 10.1111/j.1475-6773.2004.00234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Asarnow JR, Jaycox LH, Anderson M. Depression among youth in primary care models for delivering mental health services. Child Adolesc Psychiatr Clin N Am. 2002;11(3):477–497. viii. doi: 10.1016/s1056-4993(02)00006-8. [DOI] [PubMed] [Google Scholar]
- 15.Ader J, Stille CJ, Keller D, Miller BF, Barr MS, Perrin JM. The medical home and integrated behavioral health: advancing the policy agenda. Pediatrics. 2015;135(5):909–917. doi: 10.1542/peds.2014-3941. [DOI] [PubMed] [Google Scholar]
- 16. [Accessed July 10, 2012];Screening for Major Depressive Disorder in Children and Adolescents, Topic Page, March 2009. 2009 http://www.uspreventiveservicestaskforce.org/uspstf/uspschdepr.htm.
- 17.Mulye TP, Park MJ, Nelson CD, Adams SH, Irwin CE, Jr, Brindis CD. Trends in adolescent and young adult health in the United States. J Adolesc Health. 2009;45(1):8–24. doi: 10.1016/j.jadohealth.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 18.Lau JS, Adams SH, Irwin CE, Jr, Ozer EM. Receipt of preventive health services in young adults. J Adolesc Health. 2013;52(1):42–49. doi: 10.1016/j.jadohealth.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chisolm DJ, Klima J, Gardner W, Kelleher KJ. Adolescent behavioral risk screening and use of health services. Adm Policy Ment Health. 2009;36(6):374–380. doi: 10.1007/s10488-009-0245-8. [DOI] [PubMed] [Google Scholar]
- 20.Kramer T, Garralda ME. Psychiatric disorders in adolescents in primary care. Br J Psychiatry. 1998;173:508–513. doi: 10.1192/bjp.173.6.508. [DOI] [PubMed] [Google Scholar]
- 21.Burnett-Zeigler I, Walton MA, Ilgen M, et al. Prevalence and correlates of mental health problems and treatment among adolescents seen in primary care. J Adolesc Health. 2012;50(6):559–564. doi: 10.1016/j.jadohealth.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 22.Katon W, Lozano P, Russo J, McCauley E, Richardson L, Bush T. The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared with controls. J Adolesc Health. 2007;41(5):455–463. doi: 10.1016/j.jadohealth.2007.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richardson LP, Russo JE, Lozano P, McCauley E, Katon W. The effect of comorbid anxiety and depressive disorders on health care utilization and costs among adolescents with asthma. Gen Hosp Psychiatry. 2008;30(5):398–406. doi: 10.1016/j.genhosppsych.2008.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lawrence JM, Standiford DA, Loots B, et al. Prevalence and correlates of depressed mood among youth with diabetes: the SEARCH for Diabetes in Youth study. Pediatrics. 2006;117(4):1348–1358. doi: 10.1542/peds.2005-1398. [DOI] [PubMed] [Google Scholar]
- 26.Katon W, Lin EH, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry. 2007;29(2):147–155. doi: 10.1016/j.genhosppsych.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 27.Garrison MM, Katon WJ, Richardson LP. The impact of psychiatric comorbidities on readmissions for diabetes in youth. 2005;28(9):2150–2154. doi: 10.2337/diacare.28.9.2150. Web Site: www.diabetes.org. [DOI] [PubMed] [Google Scholar]
- 28.Asarnow JR, Rozenman M, Wiblin J, Zeltzer L. Integrated Medical-Behavioral Care Compared With Usual Primary Care for Child and Adolescent Behavioral Health: A Meta-analysis. JAMA Pediatr. 2015;169(10):929–937. doi: 10.1001/jamapediatrics.2015.1141. [DOI] [PubMed] [Google Scholar]
- 29.Goy E, Kansagara D, Freeman M. A Systematic Evidence Review of Interventions for Non-professional Caregivers of Individuals with Dementia. Washington (DC): 2010. [PubMed] [Google Scholar]
- 30.Collins C, Hewson DL, Munger R, Wade T. Evolving Models of Behavioral Health Integration in Primary Care. New York, NY: 2010. [Google Scholar]
- 31.Blount A. Integrated Primary Care: Organizing the Evidence. Families, Systems, & Health. 2003;21(2):121–133. [Google Scholar]
- 32.Wissow LS, Gadomski A, Roter D, et al. Improving child and parent mental health in primary care: a cluster-randomized trial of communication skills training. Pediatrics. 2008;121(2):266–275. doi: 10.1542/peds.2007-0418. [DOI] [PubMed] [Google Scholar]
- 33.D'Amico EJ, Miles JN, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: a randomized pilot study in a primary care clinic. J Subst Abuse Treat. 2008;35(1):53–61. doi: 10.1016/j.jsat.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 34.Mason M, Pate P, Drapkin M, Sozinho K. Motivational interviewing integrated with social network counseling for female adolescents: a randomized pilot study in urban primary care. J Subst Abuse Treat. 2011;41(2):148–155. doi: 10.1016/j.jsat.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 35.Hides L, Carroll S, Scott R, Cotton S, Baker A, Lubman DI. Quik Fix: a randomized controlled trial of an enhanced brief motivational interviewing intervention for alcohol/cannabis and psychological distress in young people. Psychother Psychosom. 2013;82(2):122–124. doi: 10.1159/000341921. [DOI] [PubMed] [Google Scholar]
- 36.Mertens JR, Ward CL, Bresick GF, Broder T, Weisner CM. Effectiveness of nurse-practitioner-delivered brief motivational intervention for young adult alcohol and drug use in primary care in South Africa: a randomized clinical trial. Alcohol Alcohol. 2014;49(4):430–438. doi: 10.1093/alcalc/agu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fleming MF, Balousek SL, Grossberg PM, et al. Brief physician advice for heavy drinking college students: a randomized controlled trial in college health clinics. J Stud Alcohol Drugs. 2010;71(1):23–31. doi: 10.15288/jsad.2010.71.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Werch CE, Bian H, Moore MJ, Ames S, DiClemente CC, Weiler RM. Brief multiple behavior interventions in a college student health care clinic. J Adolesc Health. 2007;41(6):577–585. doi: 10.1016/j.jadohealth.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Borowsky IW, Mozayeny S, Stuenkel K, Ireland M. Effects of a primary care-based intervention on violent behavior and injury in children. Pediatrics. 2004;114(4):e392–399. doi: 10.1542/peds.2004-0693. [DOI] [PubMed] [Google Scholar]
- 40.Harris SK, Csemy L, Sherritt L, et al. Computer-facilitated substance use screening and brief advice for teens in primary care: an international trial. Pediatrics. 2012;129(6):1072–1082. doi: 10.1542/peds.2011-1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kypri K, Saunders JB, Williams SM, et al. Web-based screening and brief intervention for hazardous drinking: a double-blind randomized controlled trial. Addiction. 2004;99(11):1410–1417. doi: 10.1111/j.1360-0443.2004.00847.x. [DOI] [PubMed] [Google Scholar]
- 42.Kypri K, Langley JD, Saunders JB, Cashell-Smith ML, Herbison P. Randomized controlled trial of web-based alcohol screening and brief intervention in primary care. Arch Intern Med. 2008;168(5):530–536. doi: 10.1001/archinternmed.2007.109. [DOI] [PubMed] [Google Scholar]
- 43.Walton MA, Bohnert K, Resko S, et al. Computer and therapist based brief interventions among cannabis-using adolescents presenting to primary care: one year outcomes. Drug Alcohol Depend. 2013;132(3):646–653. doi: 10.1016/j.drugalcdep.2013.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reid SC, Kauer SD, Hearps SJ, et al. A mobile phone application for the assessment and management of youth mental health problems in primary care: a randomised controlled trial. BMC Fam Pract. 2011;12:131. doi: 10.1186/1471-2296-12-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reid SC, Kauer SD, Hearps SJ, et al. A mobile phone application for the assessment and management of youth mental health problems in primary care: health service outcomes from a randomised controlled trial of mobiletype. BMC Fam Pract. 2013;14:84. doi: 10.1186/1471-2296-14-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Merry SN, Stasiak K, Shepherd M, Frampton C, Fleming T, Lucassen MF. The effectiveness of SPARX, a computerised self help intervention for adolescents seeking help for depression: randomised controlled non-inferiority trial. BMJ. 2012;344:e2598. doi: 10.1136/bmj.e2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Van Voorhees BW, Vanderplough-Booth K, Fogel J, et al. Integrative internet-based depression prevention for adolescents: a randomized clinical trial in primary care for vulnerability and protective factors. J Can Acad Child Adolesc Psychiatry. 2008;17(4):184–196. [PMC free article] [PubMed] [Google Scholar]
- 48.Van Voorhees BW, Fogel J, Reinecke MA, et al. Randomized clinical trial of an Internet-based depression prevention program for adolescents (Project CATCH-IT) in primary care: 12-week outcomes. J Dev Behav Pediatr. 2009;30(1):23–37. doi: 10.1097/DBP.0b013e3181966c2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Banasiak SJ, Paxton SJ, Hay P. Guided self-help for bulimia nervosa in primary care: a randomized controlled trial. Psychol Med. 2005;35(9):1283–1294. doi: 10.1017/S0033291705004769. [DOI] [PubMed] [Google Scholar]
- 50.Walsh BT, Fairburn CG, Mickley D, Sysko R, Parides MK. Treatment of bulimia nervosa in a primary care setting. Am J Psychiatry. 2004;161(3):556–561. doi: 10.1176/appi.ajp.161.3.556. [DOI] [PubMed] [Google Scholar]
- 51.Yellowlees PM, Hilty DM, Marks SL, Neufeld J, Bourgeois JA. A retrospective analysis of a child and adolescent eMental Health program. J Am Acad Child Adolesc Psychiatry. 2008;47(1):103–107. doi: 10.1097/chi.0b013e31815a56a7. [DOI] [PubMed] [Google Scholar]
- 52.Aupont O, Doerfler L, Connor DF, Stille C, Tisminetzky M, McLaughlin TJ. A collaborative care model to improve access to pediatric mental health services. Adm Policy Ment Health. 2013;40(4):264–273. doi: 10.1007/s10488-012-0413-0. [DOI] [PubMed] [Google Scholar]
- 53.Richardson LP, Ludman E, McCauley E, et al. Collaborative care for adolescents with depression in primary care: a randomized clinical trial. JAMA. 2014;312(8):809–816. doi: 10.1001/jama.2014.9259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Asarnow JR, Jaycox LH, Duan N, et al. Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: a randomized controlled trial. Jama. 2005;293(3):311–319. doi: 10.1001/jama.293.3.311. [DOI] [PubMed] [Google Scholar]
- 55.Clarke G, Debar L, Lynch F, et al. A randomized effectiveness trial of brief cognitive-behavioral therapy for depressed adolescents receiving antidepressant medication. J Am Acad Child Adolesc Psychiatry. 2005;44(9):888–898. [PubMed] [Google Scholar]
- 56.Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, Weissman MM. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry. 2004;61(6):577–584. doi: 10.1001/archpsyc.61.6.577. [DOI] [PubMed] [Google Scholar]
- 57.Bower P, Gilbody S, Richards D, Fletcher J, Sutton A. Collaborative care for depression in primary care. Making sense of a complex intervention: systematic review and meta-regression. Br J Psychiatry. 2006;189:484–493. doi: 10.1192/bjp.bp.106.023655. [DOI] [PubMed] [Google Scholar]
- 58.Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:CD006525. doi: 10.1002/14651858.CD006525.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166(21):2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 60.Kolko DJ, Campo JV, Kilbourne AM, Kelleher K. Doctor-office collaborative care for pediatric behavioral problems: a preliminary clinical trial. Arch Pediatr Adolesc Med. 2012;166(3):224–231. doi: 10.1001/archpediatrics.2011.201. [DOI] [PubMed] [Google Scholar]
- 61.Kolko DJ, Campo J, Kilbourne AM, Hart J, Sakolsky D, Wisniewski S. Collaborative care outcomes for pediatric behavioral health problems: a cluster randomized trial. Pediatrics. 2014;133(4):e981–992. doi: 10.1542/peds.2013-2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Myers K, Stoep AV, Thompson K, Zhou C, Unutzer J. Collaborative care for the treatment of Hispanic children diagnosed with attention-deficit hyperactivity disorder. Gen Hosp Psychiatry. 2010;32(6):612–614. doi: 10.1016/j.genhosppsych.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 63.Tse YJ, McCarty CA, Stoep AV, Myers KM. Teletherapy delivery of caregiver behavior training for children with attention-deficit hyperactivity disorder. Telemed J E Health. 2015;21(6):451–458. doi: 10.1089/tmj.2014.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ebert DD, Zarski AC, Christensen H, et al. Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: a meta-analysis of randomized controlled outcome trials. PLoS One. 2015;10(3):e0119895. doi: 10.1371/journal.pone.0119895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Blakemore SJ. Development of the social brain in adolescence. J R Soc Med. 2012;105(3):111–116. doi: 10.1258/jrsm.2011.110221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Colver A, Longwell S. New understanding of adolescent brain development: relevance to transitional healthcare for young people with long term conditions. Arch Dis Child. 2013;98(11):902–907. doi: 10.1136/archdischild-2013-303945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nelson EE, Leibenluft E, McClure EB, Pine DS. The social re-orientation of adolescence: a neuroscience perspective on the process and its relation to psychopathology. Psychol Med. 2005;35(2):163–174. doi: 10.1017/s0033291704003915. [DOI] [PubMed] [Google Scholar]
- 68.Breland DJ, McCarty CA, Zhou C, et al. Determinants of mental health service use among depressed adolescents. Gen Hosp Psychiatry. 2014;36(3):296–301. doi: 10.1016/j.genhosppsych.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wu P, Hoven CW, Cohen P, et al. Factors associated with use of mental health services for depression by children and adolescents. Psychiatr Serv. 2001;52(2):189–195. doi: 10.1176/appi.ps.52.2.189. [DOI] [PubMed] [Google Scholar]
- 70.Wu P, Hoven CW, Bird HR, et al. Depressive and disruptive disorders and mental health service utilization in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1999;38(9):1081–1090. doi: 10.1097/00004583-199909000-00010. discussion 1090-1082. [DOI] [PubMed] [Google Scholar]
- 71.Fleming TR, DeMets DL. Surrogate end points in clinical trials: are we being misled? Ann Intern Med. 1996;125(7):605–613. doi: 10.7326/0003-4819-125-7-199610010-00011. [DOI] [PubMed] [Google Scholar]
- 72.Tschudy MM, Raphael JL, Nehal US, O'Connor KG, Kowalkowski M, Stille C. Barriers to care coordination and medical home implementation. Pediatrics. 2016 Aug;:e2015–3458. doi: 10.1542/peds.2015-3458. DOI: 20153410.20151542/peds.20152015-20153458. [DOI] [PubMed] [Google Scholar]
- 73.Lau JS, Adams SH, Park MJ, Boscardin WJ, Irwin CE., Jr Improvement in preventive care of young adults after the affordable care act: the affordable care act is helping. JAMA Pediatr. 2014;168(12):1101–1106. doi: 10.1001/jamapediatrics.2014.1691. [DOI] [PubMed] [Google Scholar]
- 74.Lau JS, Adams SH, Boscardin WJ, Irwin CE., Jr Young adults' health care utilization and expenditures prior to the Affordable Care Act. J Adolesc Health. 2014;54(6):663–671. doi: 10.1016/j.jadohealth.2014.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mason-Jones AJ, Crisp C, Momberg M, Koech J, De Koker P, Mathews C. A systematic review of the role of school-based healthcare in adolescent sexual, reproductive, and mental health. Syst Rev. 2012;1:49. doi: 10.1186/2046-4053-1-49. [DOI] [PMC free article] [PubMed] [Google Scholar]