Abstract
Background
Tranexamic acid effects in older people are difficult to predict. This study investigated the following research questions: 1) Is tranexamic acid effective in older patients undergoing primary total hip arthroplasty (THA)? and 2) Is there a difference in the effect of tranexamic acid between younger and older patients?
Methods
This was a 2-phase retrospective matched-pair study of patients who underwent THA in 2007–2013. All procedures were performed by surgeons with at least 10 years’ experience as senior consultant. In the first phase, 58 patients aged 65 years or more who received tranexamic acid were matched 1:1 with patients who did not receive tranexamic acid for age, sex, American Society of Anesthesiologists (ASA) classification and body mass index. In the second phase, 58 patients aged 65 years or more who received tranexamic acid were matched 1:1 with patients less than 65 years of age who received tranexamic acid for sex, ASA classification and body mass index. The primary outcome measures were percent maximum decrease in hemoglobin level and estimated blood loss after surgery.
Results
In the first phase, patients who received tranexamic acid conserved postoperative hemoglobin by a mean of 10.26 g/L (standard deviation [SD] 9.89 g/L) compared to the control group (p < 0.001). The mean difference in the estimated perioperative blood loss between the 2 groups was 410 mL (SD 376 mL) (p < 0.001), which indicated less bleeding in the treatment group. In the second phase, there was no difference between the younger (mean age 55.1 [SD 7.28] yr) and older (mean age 75.6 [SD 6.35] yr) groups in mean lowest postoperative hemoglobin level or percent decrease in hemoglobin level.
Conclusion
Tranexamic acid reduced the postoperative decrease in hemoglobin level and blood loss in older patients. Moreover, the significant hemoglobin-sparing effect of tranexamic acid in older patients was similar to that observed in younger patients.
Abstract
Contexte
Les effets de l’acide tranexamique sont difficiles à prévoir chez les personnes âgées. Avec cette étude, nous avons voulu répondre aux 2 questions suivantes : 1) L’acide tranexamique est-il efficace chez les patients âgés soumis à une intervention chirurgicale primaire pour prothèse totale de la hanche (PTH)?, et 2) L’acide tranexamique produit-il un effet différent selon que les patients sont jeunes ou âgés?
Méthodes
Cette étude rétrospective en 2 phases sur des paires appariées a regroupé des patients soumis à une intervention pour PTH entre 2007 et 2013. Toutes les interventions ont été effectuées par des chirurgiens détenant au moins 10 ans d’expérience à titre de consultants principaux. Au cours de la première phase, 58 patients de 65 ans ou plus ayant reçu de l’acide tranexamique ont été assortis (rapport 1:1), selon l’âge, le sexe, la classification ASA (American Society of Anesthesiologists) et l’indice de masse corporelle, à des patients n’en ayant pas reçu. Au cours de la deuxième phase, 58 patients de 65 ans ou plus ayant reçu de l’acide tranexamique ont été assortis (rapport 1:1), selon le sexe, la classification ASA et l’indice de masse corporelle, à des patients de moins de 65 ans ayant aussi reçu de l’acide tranexamique. Les paramètres principaux étaient la diminution maximale en pourcentage du taux d’hémoglobine et la perte sanguine estimée après l’intervention chirurgicale.
Résultats
Pour la première phase, les patients qui ont reçu l’acide tranexamique ont maintenu une hémoglobine postopératoire moyenne à 10,26 g/L (écart-type [É.-T.] 9,89 g/L) comparativement au groupe témoin (p < 0,001). La différence moyenne entre les 2 groupes pour ce qui est des pertes sanguines periopératoires a été de 410 mL (É.-T. 376 mL) (p < 0,001), indiquant de ce fait une perte sanguine moindre dans le groupe traité. Pour la deuxième phase, on n’a noté aucune différence entre le groupe plus jeune (âge moyen 55,1 ans [É.-T. 7,28 ans]) et le groupe plus âgé (âge moyen 75,6 ans [É.-T. 6,35 ans]) pour ce qui est du taux d’hémoglobine postopératoire moyen le plus bas ou le pourcentage de baisse du taux d’hémoglobine.
Conclusion
L’acide tranexamique a permis d’atténuer la baisse postopératoire de l’hémoglobine et les pertes sanguines chez les patients âgés. De plus, l’effet significatif de l’acide tranexamique sur le maintien de l’hémoglobine chez les patients âgés a été similaire à ce qui s’observe chez les patients plus jeunes.
The antifibrinolytic action of tranexamic acid stabilizes the formed clot and consequently enhances microvascular hemostasis.1,2 Thus, recent systematic reviews and meta-analyses of published randomized controlled trials concluded that administration of tranexamic acid reduces blood loss and the need for transfusion in patients undergoing total hip arthroplasty (THA).3–5 However, there has been a persistent lack of knowledge on the effects of tranexamic acid in older patients undergoing THA because this population has been severely underrepresented in most randomized controlled trials.6–12 In addition, the effect of tranexamic acid in older people is difficult to predict. This is because of the presence of 2 opposing factors. First, geriatric patients in general are at higher risk for perioperative surgical bleeding, which emanates from acquired coagulation disorders and use of anticoagulation and antiplatelet medications as well as osteoporosis and osteopenia. 13,14 Second, pharmacokinetic studies suggest that older patients who receive tranexamic acid may have less perioperative bleeding because of increased blood tranexamic acid levels resulting from an aging-induced decrease in glomerular filtration rate and volume of distribution.15,16
Therefore, the objective of the current study was to investigate the effect of tranexamic acid on blood loss and reduction in the incidence and volume of allogeneic blood transfusion in older patients undergoing THA. To achieve the study objective, we investigated 2 primary hypotheses: 1) tranexamic acid administered at the time of skin incision to older patients undergoing THA reduces the decrease in postoperative hemoglobin concentration and 2) tranexamic acid reduces the decrease in postoperative hemoglobin level more in younger patients than in older patients undergoing THA.
Methods
This was a retrospective single-centre multisurgeon matched-pair study including patients who underwent THA in 2007–2013. The study was conducted at a tertiary health care facility after appropriate research ethics board approval.
We retrospectively reviewed the charts of 382 patients who had primary total hip replacement during the study period. Patients included in the retrospective study had primary THA, were aged 21 years or more at the time of surgery, were classified as American Society of Anesthesiologists (ASA) level I, II or III, and received tranexamic acid (given as a single bolus intravenously just before skin incision) or did not receive tranexamic acid. Patients who had revision THA, were classified as ASA level IV, had a risk factor for thromboembolism, received an antifibrinolytic or coagulant agent preoperatively, had a blood transfusion intraoperatively or received postoperative anticoagulant therapy that differed from the institutional protocol for joint replacements were excluded. The charts of eligible patients were reviewed in detail. Data were extracted from a database kept in the orthopedic department as well as the clinic charts kept with the orthopedic surgeons. The chart review was performed by a single person (A.L.) who was not involved in the analysis of the results.
To examine the study hypotheses, this investigation was conducted in 2 phases. The first phase determined the effects of tranexamic acid administration in older patients (age ≥ 65 yr) by comparing each older patient to a matched control patient who did not receive the antifibrinolytic (negative control). Patients were matched 1:1 on age (5-yr intervals), sex, ASA level and body mass index (3-kg/m2 intervals). In the second phase, we compared the efficacy of tranexamic acid in older and younger patients (positive control). The patients in the first phase who received tranexamic acid were matched with a younger patient (< 65 yr) who received tranexamic acid on sex, ASA level and body mass index (3-kg/m2 intervals). Every younger patient should have received tranexamic acid similarly to her/his corresponding older patient.
The primary outcome measures were percent decrease in patient’s hemoglobin level and estimated blood loss after surgery. We calculated these from chart data consisting of preoperative hemoglobin level (PreHB), and lowest postoperative hemoglobin level before discharge and before any postoperative blood transfusion (PostHB). The lowest postoperative hemoglobin level usually occurred on the third or fourth postoperative day. We calculated the primary outcomes as follows: percent decrease in patient’s hemoglobin level = [PreHB – PostHB/PreHB]*100, and estimated blood loss = Estimated patient’s blood volume*[ln(PreHB/PostHB)].17 We determined estimated patient’s blood volume as follows:18
where PBV = patient’s blood volume in millilitres, Ht = height in metres and Wt = weight in kilograms.
The secondary outcome measures were occurrence of allogenic blood transfusion perioperatively, number of allogenic blood units transfused perioperatively, length of hospital stay, occurrence of surgical infection postoperatively, occurrence of deep vein thrombosis (assessed clinically) and occurrence of pulmonary embolism (assessed clinically and by imaging studies). The following confounders and cointerventions were recorded: patient demographic characteristics, medications, comorbidities, name of surgeon, duration of surgery, type of anesthesia (general v. regional), fluid administration, preoperative iron therapy, preoperative erythropoietin therapy, preoperative coagulation profile and details of the surgical technique.
Statistical analysis and sample size calculation
We compared means of categorical variables using the paired Student t test. Nonparametric data and data that deviated significantly from normal distribution were compared with the use of the Wilcoxon matched pairs signed-rank test. We performed the statistical analysis using Stata 10 (StataCorp).
Sample size calculation for the first phase was based on the difference in the primary outcome (decrease in hemoglobin level from preoperative level) between the older patients who received tranexamic acid and those who did not.19 Available data showed that tranexamic acid can produce a saving of about 25% of the preoperative mean hemoglobin value. Based on this information, the required sample size was 47 matched pairs of patients (2-tailed paired t test: effect size f = 0.36, α = 0.05, power = 0.8). We increased the sample size by about 20% to compensate for expected incomplete patient charts, resulting in 58 pairs; i.e., 116 patients. Similarly, the sample size estimate for the second phase was based on the difference in the primary outcome between the older and younger patients who received tranexamic acid.19 Based on previous experience, we expected that tranexamic acid would produce a lesser decrease in preoperative hemoglobin level, by about 20%, in younger patients than older patients. Accordingly, the required sample size was 48 matched pairs of patients (2-tailed paired t test: effect size f = 0.41, α = 0.05, power = 0.8). Again, we increased the sample size by about 20% to compensate for expected incomplete patient charts, resulting in 58 patients per group; i.e., 116 patients.
Results
In patients included in both phases of the study, the decision to administer tranexamic acid was based on the absence of risk factors for postoperative thromboembolism and surgeon’s preference. All patients had uncemented hip replacement through the lateral surgical approach. The primary THA procedures were performed by 5 orthopedic surgeons, all of whom had at least 10 years’ experience as senior consultant.
Effect of tranexamic acid in older patients
The treatment and control groups had similar demographic characteristics, which indicated adequate matching (Table 1). The mean tranexamic acid dosage was 18.07 (standard deviation [SD] 3.59) mg/kg. Postoperatively, patients in the treatment group conserved hemoglobin by a mean of 10.26 g/L (SD 9.89 g/L) compared to control (p < 0.001) (Table 2). The mean difference in the estimated blood loss between the 2 groups was 410 mL (SD 376 mL) (p < 0.001), which indicated less total perioperative bleeding in the treatment group.
Table 1.
Preoperative characteristics of matched pairs of older patients (age ≥ 65 yr)
| Characteristic | No. (%) of patients* | p value† | |
|---|---|---|---|
| Control group n = 58 |
Tranexamic acid group n = 58 |
||
| Demographic | |||
| Age, mean ± SD; yr | 75.12 ± 6.20 | 75.57 ± 6.35 | 0.08 |
| Sex | 0.5 | ||
| Female | 42 (72) | 42 (72) | |
| Male | 16 (28) | 16 (28) | |
| Body mass index, mean ± SD | 28.3 ± 4.52 | 27.8 ± 4.73 | 0.2 |
| ASA classification | 0.5 | ||
| II | 11 (19) | 11 (19) | |
| III | 47 (81) | 47 (81) | |
| Preoperative laboratory values, mean ± SD | |||
| Hemoglobin level, g/L | 131.07 ± 11.58 | 132.67 ± 11.31 | 0.4 |
| Platelet count, × 109/L | 245 ± 63 | 250 ± 82 | 0.5 |
| International normalized ratio | 1.02 ± 0.05 | 0.98 ± 0.06 | 0.7 |
| Surgery | |||
| Surgical site | 0.5 | ||
| Right | 31 (53) | 30 (52) | |
| Left | 27 (47) | 28 (48) | |
| Surgical duration, mean ± SD; min | 84.12 ± 23.61 | 76.60 ± 17.67 | 0.08 |
| Prosthesis | 0.5 | ||
| DePuy Synthes, Johnson & Johnson | 50 (86) | 40 (69) | |
| Zimmer Biomet | 8 (14) | 18 (31) | |
| Anesthesia | 0.5 | ||
| General | 19 (33) | 14 (24) | |
| Spinal | 39 (67) | 44 (76) | |
| Patients per surgeon | |||
| Surgeon 1 | 0 (0) | 38 (66) | |
| Surgeon 2 | 5 (9) | 20 (34) | |
| Surgeon 3 | 27 (47) | 0 (0) | |
| Surgeon 4 | 17 (29) | 0 (0) | |
| Surgeon 5 | 9 (16) | 0 (0) | |
| Tranexamic acid dosage, mean ± SD; mg/kg | — | 18.07 ± 3.59 | |
ASA = American Society of Anesthesiologists; SD = standard deviation.
Except where noted otherwise.
Paired t test.
Table 2.
Perioperative outcomes recorded in matched pairs of older patients (age ≥ 65 yr)
| Outcome | No. (%) of patients* | p value† | |
|---|---|---|---|
| Control group n = 58 |
Tranexamic acid group n = 58 |
||
| Hematologic | |||
| Preoperative hemoglobin level, mean ± SD; g/L | 131.07 ± 11.58 | 132.67 ± 11.31 | 0.4 |
| Lowest postoperative hemoglobin level, mean ± SD; g/L | 89.53 ± 10.20 | 99.79 ± 10.43 | < 0.001 |
| % decrease in hemoglobin level, mean ± SD | 31.56 ± 6.14 | 24.65 ± 6.27 | < 0.001 |
| Estimated total blood loss, mean ± SD; mL | 1618 ± 448 | 1208 ± 407 | < 0.001 |
| Packed erythrocytes transfusion | 3 (5) | 1 (2) | 0.6 |
| Total volume of packed erythrocytes given, mL | 2100 (7 units) | 600 (2 units) | 0.3 |
| Postoperative recovery | |||
| Length of hospital stay, mean ± SD; d | 6.24 ± 3.62 | 5.31 ± 2.82 | 0.05 |
| Composite complication rate, % | 8.6 | 6.9 | 0.4 |
| Deep vein thrombosis | 2 (3) | 0 (0) | 0.1 |
| Pulmonary embolism | 2 (3) | 2 (3) | 0.5 |
| Infection | 1 (2) | 2 (3) | 0.3 |
| Discharged to rehabilitation | 11 (19) | 12 (21) | 0.4 |
SD = standard deviation.
Except where noted otherwise.
Paired t test.
The composite rate of complications (deep vein thrombosis, pulmonary embolism and infection) was not statistically significantly different between the treatment (8.6%) and control (6.9%) groups (Table 2). The hospital stay was longer in the control group than in the treatment group (6.2 d [SD 3.6 d] v. 5.3 d [SD 2.8 d], p = 0.05).
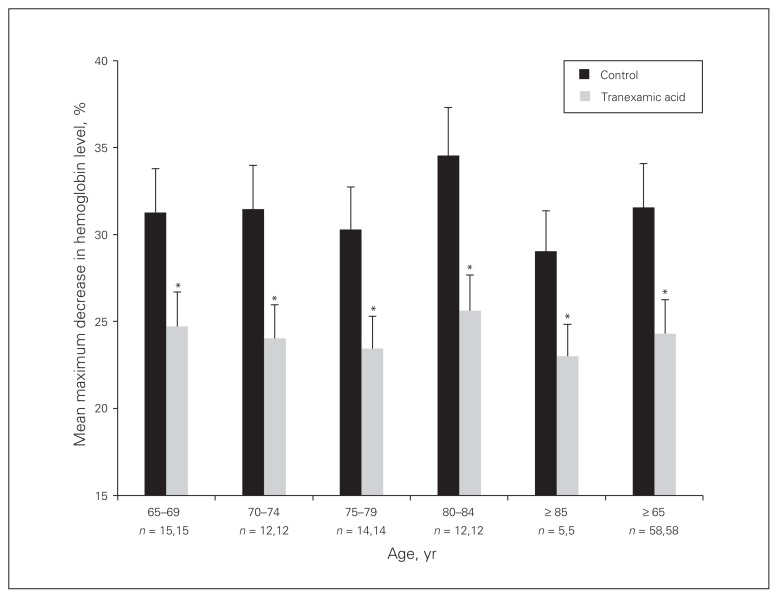
When we examined the percent maximum decrease in postoperative hemoglobin concentration by age group, in each age group, the value was statistically significantly higher in the control group than in the treatment group (Fig. 1) (p < 0.05).
Fig. 1.
Mean maximum decrease in postoperative hemoglobin level in control (no tranexamic acid) and treatment (tranexamic acid) groups, by age group. Error bars represent standard deviation. *Significantly different from control (p < 0.05).
Efficacy of tranexamic acid in younger and older patients
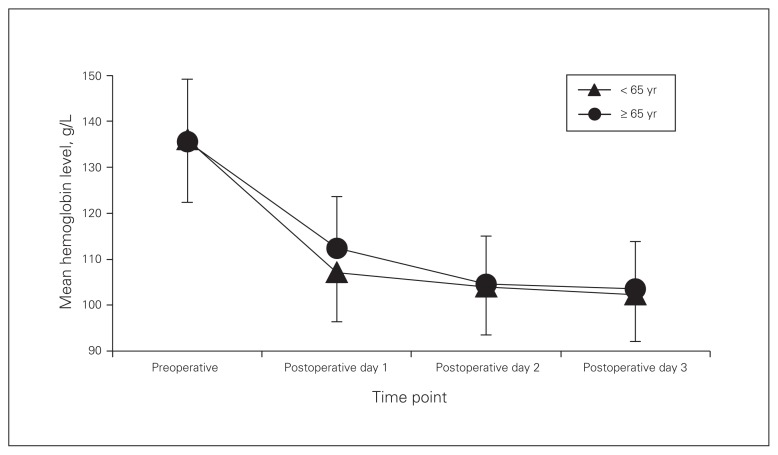
The mean age of the younger and older patients was 55.1 (SD 7.28) years and 75.6 (SD 6.35) years, respectively (Table 3). The mean tranexamic acid dosage was similar in the 2 groups (17.77 [SD 4.45] mg/kg and 18.07 [SD 3.59] mg/kg, respectively). There was no difference between the 2 groups in mean lowest postoperative hemoglobin level or percent maximum decrease in postoperative hemoglobin level. The estimated perioperative blood loss was similar in the younger (mean 1281 mL [SD 382 mL]) and older (mean 1208 mL [SD 407 mL]) patients. Postoperatively, the daily decrease in hemoglobin level was almost identical in the 2 groups (Fig. 2).
Table 3.
Preoperative characteristics of matched pairs of younger and older patients who received tranexamic acid
| Characteristic | No. (%) of patients* | p value† | |
|---|---|---|---|
| Age < 65 yr n = 58 |
Age ≥ 65 yr n = 58 |
||
| Demographic | |||
| Age, mean ± SD; yr | 55.10 ± 7.28 | 75.57 ± 6.35 | < 0.001 |
| Sex | 0.5 | ||
| Female | 42 (72) | 42 (72) | |
| Male | 16 (28) | 16 (28) | |
| Body mass index, mean ± SD | 29.3 ± 3.66 | 27.8 ± 4.73 | 0.4 |
| ASA classification | 0.5 | ||
| II | 11 (19) | 11 (19) | |
| III | 47 (81) | 47 (81) | |
| Preoperative laboratory values, mean ± SD | |||
| Hemoglobin level, g/L | 135.58 ± 10.03 | 132.67 ± 11.31 | 0.5 |
| Platelet count, × 109/L− | 230 ± 66 | 250 ± 82 | 0.7 |
| International normalized ratio | 1.10 ± 0.07 | 0.98 ± 0.06 | 0.6 |
| Surgery | |||
| Surgical site | < 0.001 | ||
| Right | 20 (34) | 30 (52) | |
| Left | 38 (66) | 28 (48) | |
| Surgical duration, mean ± SD; min | 83.38 ± 21.71 | 76.60 ± 17.67 | 0.2 |
| Prosthesis | < 0.001 | ||
| DePuy Synthes, Johnson & Johnson | 30 (52) | 40 (69) | |
| Zimmer Biomet | 28 (48) | 18 (31) | |
| Anesthesia | 0.1 | ||
| General | 10 (17) | 14 (24) | |
| Spinal | 48 (83) | 44 (76) | |
| Patients per surgeon | |||
| Surgeon 1 | 28 (48) | 38 (66) | |
| Surgeon 2 | 20 (34) | 20 (34) | |
| Surgeon 3 | 10 (17) | 0 (0) | |
| Surgeon 4 | 0 (0) | 0 (0) | |
| Surgeon 5 | 0 (0) | 0 (0) | |
| Tranexamic acid dosage, mean ± SD; mg/kg | 17.77 ± 4.45 | 18.07 ± 3.59 | 0.7 |
ASA = American Society of Anesthesiologists; SD = standard deviation.
Except where noted otherwise.
Paired t test.
Fig. 2.
Mean hemoglobin level before and after surgery in younger and older patients who received tranexamic acid. Error bars represent standard deviation.
The composite complication rate was significantly different between the younger and older patients (0% v. 6.9%, p = 0.02) (Table 4). The hospital length of stay in the younger (5.3 d [SD 2.48 d) and older (5.3 d [SD 2.82 d) groups was similar.
Table 4.
Perioperative outcomes recorded in matched pairs of younger and older patients who received tranexamic acid
| Outcome | No. (%) of patients* | p value† | |
|---|---|---|---|
| Age < 65 yr n = 58 |
Age ≥ 65 yr n = 58 |
||
| Hematologic | |||
| Preoperative hemoglobin level, mean ± SD; g/L | 135.58 ± 10.03 | 132.67 ± 11.31 | 0.5 |
| Lowest postoperative hemoglobin level, mean ± SD; g/L | 101.48 ± 10.41 | 99.79 ± 10.43 | 0.6 |
| % decrease in hemoglobin level, mean ± SD | 25.06 ± 6.50 | 24.65 ± 6.27 | 0.4 |
| Estimated total blood loss, mean ± SD; mL | 1281 ± 382 | 1208 ± 407 | 0.3 |
| Packed erythrocytes transfusion | 0 (0) | 1 (2) | 0.2 |
| Total volume of packed erythrocytes given, mL | — | 600 (2 units) | 0.2 |
| Postoperative recovery | |||
| Length of hospital stay, mean ± SD; d | 5.30 ± 2.48 | 5.31 ± 2.82 | 0.3 |
| Composite complication rate, % | 0 | 6.9 | 0.02 |
| Pulmonary embolism | 0 (0) | 2 (3) | 0.08 |
| Infection | 0 (0) | 2 (3) | 0.08 |
| Discharged to rehabilitation | 2 (4) | 12 (21) | 0.004 |
SD = standard deviation.
Except where noted otherwise.
Paired t test.
Discussion
We found that a single bolus of tranexamic acid administered intravenously at the initial skin incision during primary THA surgery reduced the postoperative decrease in hemoglobin level in older patients (≥ 65 yr). The significant hemoglobin-sparing effect of tranexamic acid in older patients was similar to that in younger patients. The composite complication rate was lower in younger patients than in older patients.
Other investigators have reported different dosage regimens for the administration of tranexamic acid during THA, including single and multiple injections, and continuous infusion following a loading dose.21 A single injection of nearly 20 mg/kg at the time of the initial skin incision was used in our cohort. This dosage showed significant efficacy and is simple in application and clinical utility. In a pharmacokinetic study, Benoni and colleagues20 found that such single doses maintain therapeutic serum and joint fluid levels for 8 hours after injection. A study in which multiple tranexamic acid injections were used21 did not show results superior to ours.
Our results validated our primary hypothesis that tranexamic acid administered at the time of skin incision to older patients undergoing hip replacement surgery reduces the decrease in postoperative hemoglobin concentration. Based on recent large studies that showed aging as an independent risk factor associated with allogenic blood transfusion,22–24 we also hypothesized that older patients experience more perioperative bleeding than do younger patients and that tranexamic acid is more effective in younger patients. However, our results were at odds with this proposition: our results in older patients were unexpectedly similar to those of previously published reports in younger patients, including prospective11,25,26 and retrospective27–29 studies.
Although older patients who did not receive tranexamic acid had more perioperative bleeding and hemoglobin loss than older patients who received the antifibrinolytic in our study, the transfusion rates in the 2 groups were similar. This was expected because most patients did not reach the trigger hemoglobin levels for allogenic transfusion according to standard protocols. A large sample will be required to explore whether tranexamic acid can reduce transfusion rates in older patients undergoing primary THA. In addition, the incidence of thromboembolism in our older group was higher than that previously reported.30–32 This may have been due to the fact that our study was not powered to determine the prevalence of thromboembolism in older people undergoing total hip replacement.
Limitations
The current study has limitations. First, the cohorts were not matched for year of the procedure. However, there was no association between the extent of the primary outcomes of the study and the date of surgery in the entire cohort. Hence, there is no apparent sampling bias due to the lack of matching for surgical date. Second, the lowest postoperative hemoglobin concentration was that measured during the hospital stay. The hemoglobin level may have drifted to lower values after discharge from hospital; hence, the reported decrease in hemoglobin level may not precisely reflect the actual outcomes. However, the hemoglobin concentration would probably have reached a nadir before patients were discharged from the hospital, as is evident from Figure 2. Finally, the decision to give tranexamic acid was partly based on the surgeon’s preference. This might have led to sampling bias, especially if surgeon expertise and technique are considered. However, all the surgeons who performed the procedures in this study had more than 10 years of experience, and their surgical technique was not significantly different within the groups studied. Therefore, sampling bias was reduced to a minimum.
Conclusion
Tranexamic acid decreased perioperative blood loss and had a significant perioperative hemoglobin-sparing effect in older patients undergoing primary THA, similar to that seen in younger patients. Hence, there is no need for adjustment of the tranexamic acid dosage in older patients. Tranexamic acid administration should be an important component of blood management programs in geriatric patients undergoing hip replacement surgery.33
Acknowledgements
The authors are grateful to the nursing staff at the Department of Orthopedic Surgery, Trillium Health Partners, Mississauga Hospital for their invaluable help during data collection for the study.
Footnotes
Competing interests: None declared.
Contributors: H. El Beheiry and N. Clements designed the study. All authors acquired the data, which H. El Beheiry and A. Lubberdink analyzed. H. El Beheiry wrote the article, which all authors reviewed and approved for publication.
References
- 1.Mahdy AM, Webster NR. Perioperative systemic haemostatic agents. Br J Anaesth. 2004;93:842–58. doi: 10.1093/bja/aeh227. [DOI] [PubMed] [Google Scholar]
- 2.Katsumata S, Nagashima M, Kato K, et al. Changes in coagulation– fibrinolysis marker and neutrophil elastase following the use of tourniquet during total knee arthroplasty and the influence of neutrophil elastase on thromboembolism. Acta Anaesthesiol Scand. 2005;49:510–6. doi: 10.1111/j.1399-6576.2005.00621.x. [DOI] [PubMed] [Google Scholar]
- 3.Sukeik M, Alshryda S, Haddad FS, et al. Systematic review and metaanalysis of the use of tranexamic acid in total hip replacement. J Bone Joint Surg Br. 2011;93:39–46. doi: 10.1302/0301-620X.93B1.24984. [DOI] [PubMed] [Google Scholar]
- 4.Gandhi R, Evans HMK, Mahomed SR, et al. Tranexamic acid and the reduction of blood loss in total knee and hip arthroplasty: a metaanalysis. BMC Res Notes. 2013;6:184. doi: 10.1186/1756-0500-6-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xie J, Jun M, Yue C, et al. Combined use of intravenous and topical tranexamic acid following cementless total hip arthroplasty: a randomised clinical trial. Hip Int. 2016;26:36–42. doi: 10.5301/hipint.5000291. [DOI] [PubMed] [Google Scholar]
- 6.Husted H, Blønd L, Sonne-Holme S, et al. Tranexamic acid reduces blood loss and blood transfusions in primary total hip arthroplasty: a prospective randomized double-blind study in 40 patients. Acta Orthop Scand. 2003;74:665–9. doi: 10.1080/00016470310018171. [DOI] [PubMed] [Google Scholar]
- 7.Lemay E, Guay J, Côté C, et al. Tranexamic acid reduces the need for allogenic red blood cell transfusions in patients undergoing total hip replacement. Can J Anaesth. 2004;51:31–7. doi: 10.1007/BF03018543. [DOI] [PubMed] [Google Scholar]
- 8.Yamasaki S, Masuhara K, Fuji T. Tranexamic acid reduces blood loss after cementless total hip arthroplasty — prospective randomized study in 40 cases. Int Orthop. 2004;28:69–73. doi: 10.1007/s00264-003-0511-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kazemi SM, Mosaffa F, Eajazi A, et al. The effect of tranexamic acid on reducing blood loss in cementless total hip arthroplasty under epidural anesthesia. Orthopedics. 2010;33:17. doi: 10.3928/01477447-20091124-30. [DOI] [PubMed] [Google Scholar]
- 10.Malhotra R, Kumar V, Garg B. The use of tranexamic acid to reduce blood loss in primary cementless total hip arthroplasty. Eur J Orthop Surg Traumatol. 2011;21:101–4. [Google Scholar]
- 11.Imai N, Dohmae Y, Suda K, et al. Tranexamic acid for reduction of blood loss during total hip arthroplasty. J Arthroplasty. 2012;27:1838–43. doi: 10.1016/j.arth.2012.04.024. [DOI] [PubMed] [Google Scholar]
- 12.Niskanen RO, Korkala OL. Tranexamic acid reduces blood loss in cemented hip arthroplasty: a randomized, double-blind study of 39 patients with osteoarthritis. Acta Orthop. 2005;76:829–32. doi: 10.1080/17453670510045444. [DOI] [PubMed] [Google Scholar]
- 13.Nicolle AL, Talks KL, Hanley JP. Congenital and acquired bleeding problems in elderly patients. Rev Clin Gerontol. 2005;15:9–26. [Google Scholar]
- 14.Van PY, Schreiber MA. Hematologic issues in the geriatric surgical patient. Surg Clin North Am. 2015;95:129–38. doi: 10.1016/j.suc.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 15.Yang QJ, Jerath A, Bies RR. Pharmacokinetic modeling of tranexamic acid for patients undergoing cardiac surgery with normal renal function and model simulations for patients with renal impairment. Biopharm Drug Dispos. 2015;36:294–307. doi: 10.1002/bdd.1941. [DOI] [PubMed] [Google Scholar]
- 16.Aymanns C, Keller F, Maus S, et al. Review on pharmacokinetics and pharmacodynamics and the aging kidney. Clin J Am Soc Nephrol. 2010;5:314–27. doi: 10.2215/CJN.03960609. [DOI] [PubMed] [Google Scholar]
- 17.Good L, Peterson E, Lisander B. Tranexamic acid decreases external blood loss but not hidden blood loss in total knee replacement. Br J Anaesth. 2003;90:596–9. doi: 10.1093/bja/aeg111. [DOI] [PubMed] [Google Scholar]
- 18.Nadler SB. Prediction of blood volume in normal human adults. Surgery. 1972;51:224–32. [PubMed] [Google Scholar]
- 19.Faul F, Erdfelder E, Lan AG, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 20.Benoni G, BjÖrkman S, Fredin H. Application of pharmacokinetic data from healthy volunteers for the prediction of plasma concentrations of tranexamic acid in surgical patients. Clin Drug Invest. 1995;10:280–7. [Google Scholar]
- 21.Niskanen RO, Korkala OL. Tranexamic acid reduces blood loss in cemented hip arthroplasty: a randomized, double-blind study of 39 patients with osteoarthritis. Acta Orthop. 2005;76:829–32. doi: 10.1080/17453670510045444. [DOI] [PubMed] [Google Scholar]
- 22.Hart A, Khalil J, Carli A, et al. Blood transfusion in primary total hip and knee arthroplasty. Incidence, risk factors and thirty-day complication rates. J Bone Joint Surg Am. 2014;96:1945–51. doi: 10.2106/JBJS.N.00077. [DOI] [PubMed] [Google Scholar]
- 23.Saleh A, Small TDO, Pillai ALPC, et al. Allogenic blood transfusion following total hip arthroplasty: results from the Nationwide Inpatient Sample, 2000 to 2009. J Bone Joint Surg Am. 2014;96:e155. doi: 10.2106/JBJS.M.00825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Browne JA, Adib F, Brown TE, et al. Transfusion rates are increasing following total hip arthroplasty: risk factors and outcomes. J Arthroplasty. 2013;28(Suppl 8):34–7. doi: 10.1016/j.arth.2013.03.035. [DOI] [PubMed] [Google Scholar]
- 25.Lee YC, Park SJ, Kim JS, et al. Effect of tranexamic acid on reducing postoperative blood loss in combined hypotensive epidural anesthesia and general anesthesia for total hip replacement. J Clin Anesth. 2013;25:393–8. doi: 10.1016/j.jclinane.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 26.Hourlier H, Fennema P. Single tranexamic acid dose to reduce perioperative morbidity in primary total hip replacement: a randomised clinical trial. Hip Int. 2014;24:63–8. doi: 10.5301/hipint.5000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.George DA, Sarraf KM, Nwaboku H. Single perioperative dose of tranexamic acid in primary hip and knee arthroplasty. Eur J Orthop Surg Traumatol. 2015;25:129–33. doi: 10.1007/s00590-014-1457-5. [DOI] [PubMed] [Google Scholar]
- 28.Wei W, Wei B. Comparison of topical and intravenous tranexamic acid on blood loss and transfusion rates in total hip arthroplasty. J Arthroplasty. 2014;29:2113–6. doi: 10.1016/j.arth.2014.07.019. [DOI] [PubMed] [Google Scholar]
- 29.March GM, Elfatori S, Beaulé PE. Clinical experience with tranexamic acid during primary total hip arthroplasty. Hip Int. 2013;23:72–9. doi: 10.5301/HIP.2013.10724. [DOI] [PubMed] [Google Scholar]
- 30.Poeran J, Rasul R, Suzuki S, et al. Tranexamic acid use and postoperative outcomes in patients undergoing total hip or knee arthroplasty in the United States: retrospective analysis of effectiveness and safety. BMJ. 2014;349:g4829. doi: 10.1136/bmj.g4829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Whiting DR, Gillette BP, Duncan C, et al. Preliminary results suggest tranexamic acid is safe and effective in arthroplasty patients with severe comorbidities. Clin Orthop Relat Res. 2014;472:66–72. doi: 10.1007/s11999-013-3134-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duncan CM, Gillette BP, Jacob AK, et al. Venous thromboembolism and mortality associated with tranexamic acid use during total hip and knee arthroplasty. J Arthroplasty. 2015;30:272–6. doi: 10.1016/j.arth.2014.08.022. [DOI] [PubMed] [Google Scholar]
- 33.Hare GM, Freedman J, David Mazer C. Review article: risks of anemia and related management strategies: Can perioperative blood management improve patient safety? Can J Anaesth. 2013;60:168–75. doi: 10.1007/s12630-012-9861-y. [DOI] [PubMed] [Google Scholar]