Abstract
PURPOSE:
The study aimed at determining the relationship between refraction and anthropometric measurements and the relationship between the level of education and refractive status in a Nigerian young adult population.
MATERIALS AND METHODS:
Healthy volunteers from the students and staff of a teaching hospital in South-Western Nigeria were studied. Demographic profiles including participants' highest educational status, parental educational level, and the age at first formal school enrollment were documented. The height and weight of the participants were measured. Noncycloplegic objective refraction was determined with autorefractor, and the spherical equivalent refraction (SER) of the right eye was used for analysis. SPSS 16 was used to explore the relationships between refraction, height, weight, and body mass index and the educational status of the participants.
RESULTS:
Two hundred and thirty-nine adults with a mean age of 28.4 ± 6.5 years comprising 116 males and 123 females were studied. The mean height, weight, body mass index, and right eye SER were 1.7 ± 0.1 m, 64.4 ± 12.2 kg, 23.6 ± 4.3 kg/m2, and −0.8 ± 1.4 D, respectively. Height was negatively correlated with the SER (R = −0.3, P < 0.01) in males but not in females. Refraction was not significantly related to weight or body mass index. Participants with higher levels of education were more likely to be myopic. Higher parental education and early formal school enrollment were significantly associated with myopia.
CONCLUSION:
This study demonstrated a significant positive relationship between height and myopia in male participants but not in females. Individual as well as parental higher levels of education have also shown a positive association with myopic tendency.
Keywords: Anthropometrics, educational status, Nigerians, refraction
Introduction
The refractive status of any individual is dependent on many factors, some of which may be genetic or environmental. Higher socioeconomic status, especially educational achievement, has been found to be a risk factor for myopia.[1] It has also been suggested that increased near work is associated with the progression of myopic refraction.[1]
However, reports from various population-based studies on the relationship between refraction and stature have remained inconsistent.[1,2,3,4,5,6,7,8,9] Although it has been documented that the axial length of the globe is significantly related to the height and the refraction of the individual,[2,5,6,10,11,12,13,14] no consistent relationship has been established between the height and refraction in adults.[1,3,9] On the contrary, positive relationship between height and myopia was established in schoolchildren in Singapore.[10]
Similarly, while some studies have identified increased weight as a risk factor for hypermetropia [7,10] and myopia in females,[8] others have not demonstrated such associations.[1,6,9] These observations informed the need to determine the relationship between refraction and some anthropometric parameters (height, weight, and body mass index) in our immediate segment of Nigerian adult population. Uncorrected refractive error is a significant cause of visual impairment in Nigeria, being responsible for over half of moderate visual impairment and >10% of severe visual impairment.[15] Furthermore, persons with myopic refractive error are at higher risk of having open-angle glaucoma [16] and retinal detachment, while short stature individuals are at risk of primary angle closure glaucoma.[17,18] It is envisaged that if simple measurable parameters such as the height and weight are found to be related to these important predictors of ocular morbidity, that is, refractive errors, they could be found useful in screening for some of these ocular diseases.
Materials and Methods
This prospective observational cross-sectional study was carried out on healthy volunteers from the staff and student population aged 18–40 years at the Eye Care Centre of Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife. The research hypothesis was “There is no relationship between refraction and height.” Sample size was calculated from n = (Zσ/E)2, where n = number of participants, Z = standard normal deviate at 95% confidence interval (1.96), σ is the standard deviation of spherical equivalent refraction (SER), which was 1.58,[19] and E = margin of error of 0.20 diopter, n = 239.7.
Ethical clearance was obtained from the Ethical and Research Committee of the hospital, and informed consent was obtained from the volunteers. The volunteers were given the participant information sheet and were invited to the Eye Care Center for the study. Individuals with a history of ocular trauma or surgery, current eye diseases except possible refractive errors, limb or spinal deformity, pregnancy, and recent significant weight loss were excluded from the study. Every second volunteer who met the inclusion criteria and was free from the exclusion criteria was included in the analysis, until desired sample size was achieved.
The respondents documented their age at last birthday, sex, highest educational status, and age at first enrollment for formal education, in a predesigned pro forma. Maternal and paternal highest educational levels were also documented. Education was grouped into no formal education, primary (primary school or equivalent), secondary (secondary school or equivalent), tertiary (postsecondary education), and postgraduate. Participants currently enrolled for tertiary education were also considered to have tertiary education.
Participants' height and weight were measured with standometer in meters (m) and standard weighing scale in kilogram, respectively, after adjusting for the zero error. Distance visual acuity was measured unaided and with pinhole; using an illuminated Snellen chart at 6 m in a well-lit room, one eye at a time. The above was carried out by a trained and validated research assistant (a registered nurse). Noncycloplegic objective refraction of each participant was determined using a Grand Seiko® autorefractor (Kagawa, Japan) by one of the investigators for all the participants. Participants were seated comfortably with their chin on the chin-rest and their forehead resting firmly on the headband of the autorefractor and instructed to constantly fixate on the internal fixation target within the autorefractor. The anterior segment was examined with bright pen torch and the slit lamp biomicroscope, while the posterior segment was examined with the direct ophthalmoscope by the same investigator. SER was recorded as the sum of the sphere and half of the cylinder in diopters. Myopia was defined as SER more than −0.50 D and hypermetropia as >+0.50 D. Emmetropia was SER between −0.50 D and +0.50 D.
The data obtained were entered into SPSS 16.0 statistical software (IBM Corporation). With this software, the body mass index (weight in kilogram divided by the square of the height in meters [kg/m2]) was calculated and correlation analysis was performed to show the relationship between the various variables. Only measurements in the right eyes were used for calculations because very strong positive correlation exists between the SER in the two eyes (R = 0.9, P < 0.01). Differences between means were examined using the t-test or analysis of variance methods. A multivariate regression model was utilized to explore the influence of height, weight, body mass index, participant's highest educational status, and maternal as well as paternal educational status on SER. Level of statistical significance was set at 5% (P < 0.05).
Results
Two hundred and thirty-nine healthy volunteers comprising 116 (48.5%) males and 123 (51.5%) females (M:F = 1:1.1) were enrolled in the study. Participants were aged 18–40 years with a mean age of 28.4 ± 6.4 years. Eleven participants (4.6%) had only primary education, while 42 (17.6%), 156 (65.3%), and 30 (12.6%) participants had secondary, tertiary, and postgraduate education, respectively. The height, weight, and body mass index ranged between 1.5 and 1.9 m; 40 and 129 kg; and 14.0 and 43.1 kg/m2, respectively.
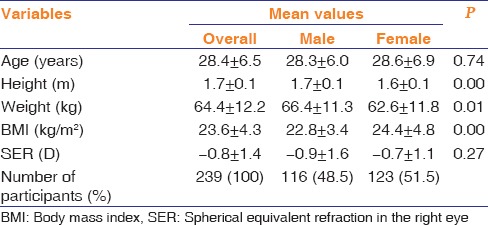
Table 1 shows the mean age, height, weight, body mass index, and average SER in the right eyes in all participants, as well as by gender distribution. The height and weight were significantly higher in males than in females, but the BMI was higher in the female volunteers.
Table 1.
Mean age, anthropometrics, and spherical equivalent refraction of participants
SER was between −7.8 D and + 2.1 D in the participants. Emmetropia was the most prevalent in 129 (54%) participants, followed by myopia in 97 (40.6%) participants. Only 13 (5.4%) participants were hypermetropic.
Table 2 shows the correlation between SER and age at last birthday, age at first formal school enrollment, anthropometrics, as well as participants' and parental educational status. There was a statistically significant positive relationship between increasing age and SER with the older participants being more likely to have hypermetropia (P = 0.01). On the other hand, a significant negative relationship was observed between height and SER in the total population and in males but not in the females meaning that taller male participants are more likely to have negative refraction (myopia). Both weight and body mass index were not significantly correlated with SER.
Table 2.
Correlation between spherical equivalent refraction and age, anthropometric measurements, and educational status of participants
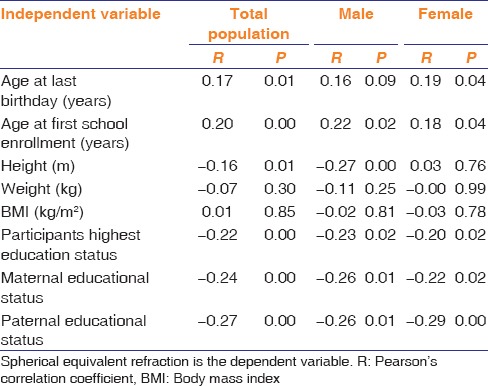
Statistically significant negative correlation was noticed between SER and participant's highest educational status. Similar significant relationships were also observed for both increasing maternal and paternal education. This means that both participants' education and parental education are related to myopia. Age at first formal school enrollment is positively related to SER. This means that individuals who start school at an older age are more prone to hypermetropia and those who start earlier have a higher tendency toward negative refraction.
Discussion
The association between refraction and stature is likely to be complex majorly because refractive status is a complex phenomenon attributable to both genetic and environmental factors such as social status, education, and occupation.[2,4,20,21,22,23] The participants' age 18–40 years recruited in this study is aimed to minimize the age-related lenticular changes that might modify refractive status of older individuals.
Findings from this study showed that majority (54%) of the participants were emmetropic, followed by myopia (40.6%), and the least prevalent refractive status in this predominantly educated population was hypermetropia (5.4%). These findings are consistent with some clinic and population-based studies in Nigeria in which myopia was found to be more common spherical refractive error.[24,25,26,27] Our finding is also close to 46.7% prevalence of myopia observed in Saudi Arabs of similar age group [19] but lower than the prevalence observed among Jordanian Arabs where more than half (53.7%) of the studied population of relatively similar age group selected from workplaces were myopic.[13]
Our findings also showed that the overall mean SER in young adults in this community is −0.8 D with slightly higher value of −0.7 D ± 1.1 D observed in the female sex against the −0.9 D ± 1.6 D observed in males. The observed overall mean SER recorded in this predominantly educated Nigerian population is higher than the −0.9 D and −1.0 D reported among Saudis and Jordanian young Arab populations, respectively.[13,19] Similarly, when compared with the earlier report from China, our findings as well as the Saudis and the Jordanian reports showed significantly much higher values than the mean SER −3.0 D recorded on young Chinese aged 19–39 years with 71% prevalence of myopia and 1.5% hypermetropia.[28] These observations suggest some regional differences in the mean SER values. The factors that may be responsible for these observed differences in the prevalence of myopia among the Arabs, Chinese, and the Nigerians remained unknown, although racial and environmental factors may account for the differences.
Finding of taller persons having a general tendency toward myopia observed in this study is similar to previous reports from Danish draftees [4] and Singaporean Chinese schoolchildren studies.[10] However, it is important to note that the relationship is only statistically significant in the total population and in the male gender but not in the females. This observation probably suggests the existence of different factors determining refraction in the gender groups. Contrary to the findings in this study, there are studies that observed no significant association between height and refractive status.[2,3,5,7,18] The height of individuals does not appear to be a strong risk factor for the development of myopia, considering the weak correlation observed between the two variables, that is, SER and the height.
In agreement with most previous studies, this study showed that there is no significant relationship between the weight and refraction and between refraction and the body mass index of young adults in this community.[1,2,3,5,6,18] The negative relationship between SER and the educational status demonstrated in our study is observed in the participants as well as their parents. This observation is in keeping with a previous study where myopia was found to be more prevalent in the academic than in the nonacademic group.[4] Other studies have also established similar relationship between myopia and education.[2,3,5] Furthermore, we found that individuals who were older at first enrollment for formal education have a higher tendency toward hypermetropia. This may probably be interpreted that early exposure to near work may contribute to the development of myopia. It is not impossible that the associations seen in this predominantly educated black population differ from other racial groups with dissimilar genetic and environmental exposures, different height and weight distributions, and higher rates of myopia.
The major limitation of this study is the fact that the studied groups were drawn predominantly from a literate population, although an attempt to minimize the impact of this was recruiting various cadres of staff in the health institution including students. Being a cross-sectional study, it is difficult to establish a causal relationship from this study. Perhaps a future larger community-based longitudinal study will be beneficial.
Conclusion
This study demonstrated a significant positive relationship between height and myopia in males but not in the females. This study also showed that the weight and body mass index are not related to refraction. On the other hand, higher educational status of the participants and their parent showed increased tendency toward development of myopia. Since children are now starting school earlier than before, it can be expected that more of our future young generations may develop myopia since younger age at first formal school enrollment is related to myopia. This has an implication on ocular disease surveillance as more of the ophthalmic pathologies associated with myopia may become more prevalent. A larger future community-based study is advocated.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jung SK, Lee JH, Kakizaki H, Jee D. Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in Seoul, South Korea. Invest Ophthalmol Vis Sci. 2012;53:5579–83. doi: 10.1167/iovs.12-10106. [DOI] [PubMed] [Google Scholar]
- 2.Foster PJ, Broadway DC, Hayat S, Luben R, Dalzell N, Bingham S, et al. Refractive error, axial length and anterior chamber depth of the eye in British adults: The EPIC-Norfolk eye study. Br J Ophthalmol. 2010;94:827–30. doi: 10.1136/bjo.2009.163899. [DOI] [PubMed] [Google Scholar]
- 3.Jacobsen N, Jensen H, Goldschmidt E. Prevalence of myopia in Danish conscripts. Acta Ophthalmol Scand. 2007;85:165–70. doi: 10.1111/j.1600-0420.2006.00789.x. [DOI] [PubMed] [Google Scholar]
- 4.Teasdale TW, Goldschmidt E. Myopia and its relationship to education, intelligence and height-Preliminary results from an on-going study of Danish draftees. Acta Ophthalmol Suppl. 1988;185:41–3. doi: 10.1111/j.1755-3768.1988.tb02660.x. [DOI] [PubMed] [Google Scholar]
- 5.Wong TY, Foster PJ, Johnson GJ, Klein BE, Seah SK. The relationship between ocular dimensions and refraction with adult stature: The Tanjong Pagar Survey. Invest Ophthalmol Vis Sci. 2001;42:1237–42. [PubMed] [Google Scholar]
- 6.Eysteinsson T, Jonasson F, Arnarsson A, Sasaki H, Sasaki K. Relationships between ocular dimensions and adult stature among subjects in the Reykjavik eye study. Acta Ophthalmol Scand. 2005;83:734–8. doi: 10.1111/j.1600-0420.2005.00540.x. [DOI] [PubMed] [Google Scholar]
- 7.Wu HM, Gupta A, Newland HS, Selva D, Aung T, Casson RJ, et al. Association between stature, ocular biometry and refraction in an adult population in rural Myanmar: The Meiktila Eye Study. Clin Exp Ophthalmol. 2007;35:834–9. doi: 10.1111/j.1442-9071.2007.01638.x. [DOI] [PubMed] [Google Scholar]
- 8.Dirani M, Islam A, Baird PN. Body stature and myopia-the genes in myopia (GEM) twin study. Ophthalmic Epidemiol. 2008;15:135–9. doi: 10.1080/09286580801957751. [DOI] [PubMed] [Google Scholar]
- 9.Xu L, Wang YX, Zhang HT, Jonas JB. Anthropomorphic measurements and general and ocular parameters in adult Chinese: The Beijing eye study. Acta Ophthalmol. 2011;89:442–7. doi: 10.1111/j.1755-3768.2009.01734.x. [DOI] [PubMed] [Google Scholar]
- 10.Saw SM, Chua WH, Hong CY, Wu HM, Chia KS, Stone RA, et al. Height and its relationship to refraction and biometry parameters in Singapore Chinese children. Invest Ophthalmol Vis Sci. 2002;43:1408–13. [PubMed] [Google Scholar]
- 11.Song HT, Kim YJ, Lee SJ, Moon YS. Relations between age, weight, refractive error and eye shape by computerized tomography in children. Korean J Ophthalmol. 2007;21:163–8. doi: 10.3341/kjo.2007.21.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fotedar R, Wang JJ, Burlutsky G, Morgan IG, Rose K, Wong TY, et al. Distribution of axial length and ocular biometry measured using partial coherence laser interferometry (IOL master) in an older white population. Ophthalmology. 2010;117:417–23. doi: 10.1016/j.ophtha.2009.07.028. [DOI] [PubMed] [Google Scholar]
- 13.Mallen EA, Gammoh Y, Al-Bdour M, Sayegh FN. Refractive error and ocular biometry in Jordanian adults. Ophthalmic Physiol Opt. 2005;25:302–9. doi: 10.1111/j.1475-1313.2005.00306.x. [DOI] [PubMed] [Google Scholar]
- 14.Chen MJ, Liu YT, Tsai CC, Chen YC, Chou CK, Lee SM, et al. Relationship between central corneal thickness, refractive error, corneal curvature, anterior chamber depth and axial length. J Chin Med Assoc. 2009;72:133–7. doi: 10.1016/S1726-4901(09)70038-3. [DOI] [PubMed] [Google Scholar]
- 15.Ezelum C, Razavi H, Sivasubramaniam S, Gilbert CE, Murthy GV, Entekume G, et al. Refractive error in Nigerian adults: Prevalence, type, and spectacle coverage. Invest Ophthalmol Vis Sci. 2011;52:5449–56. doi: 10.1167/iovs.10-6770. [DOI] [PubMed] [Google Scholar]
- 16.Los Angeles Latino Eye Study Group. Kuzin AA, Varma R, Reddy HS, Torres M, Azen SP. Ocular biometry and open-angle glaucoma: The Los Angeles Latino eye study. Ophthalmology. 2010;117:1713–9. doi: 10.1016/j.ophtha.2010.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu L, Li J, Wang Y, Jonas JB. Anthropomorphic differences between angle-closure and open-angle glaucoma: The Beijing eye study. Acta Ophthalmol Scand. 2007;85:914–5. doi: 10.1111/j.1600-0420.2007.00966.x. [DOI] [PubMed] [Google Scholar]
- 18.Xu L, Cao WF, Wang YX, Chen CX, Jonas JB. Anterior chamber depth and chamber angle and their associations with ocular and general parameters: The Beijing eye study. Am J Ophthalmol. 2008;145:929–36. doi: 10.1016/j.ajo.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 19.Osuobeni EP. Ocular components values and their intercorrelations in Saudi Arabians. Ophthalmic Physiol Opt. 1999;19:489–97. doi: 10.1046/j.1475-1313.1999.00453.x. [DOI] [PubMed] [Google Scholar]
- 20.Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K. Parental myopia, near work, school achievement, and children's refractive error. Invest Ophthalmol Vis Sci. 2002;43:3633–40. [PubMed] [Google Scholar]
- 21.Saw SM, Chua WH, Wu HM, Yap E, Chia KS, Stone RA, et al. Myopia: Gene-environment interaction. Ann Acad Med Singapore. 2000;29:290–7. [PubMed] [Google Scholar]
- 22.Wallman J, Winawer J. Homeostasis of eye growth and the question of myopia. Neuron. 2004;43:447–68. doi: 10.1016/j.neuron.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 23.Morgan IG. The biological basis of myopic refractive error. Clin Exp Optom. 2003;86:276–88. doi: 10.1111/j.1444-0938.2003.tb03123.x. [DOI] [PubMed] [Google Scholar]
- 24.Adegbehingbe BO, Majekodunmi AA, Akinsola FB, Soetan EO. Pattern of refractive errors at Obafemi Awolowo University Teaching Hospital, Ile-Ife, Nigeria. Niger J Ophthalmol. 2003;11:76–9. [Google Scholar]
- 25.Abah ER, Chinda D, Samaila E, Anyebe EE. Profile of refractive errors and presbyopia in a university community: A clinical study. Ann Niger Med. 2010;4:55–8. [Google Scholar]
- 26.Ayanniyi AA, Fadamiro CO, Adeyemi JB, Folorunso FN, Uzukwu SC. Common refractive errors among the Ekitis of South-Western Nigeria. J Med Med Sci. 2010;1:401–6. [Google Scholar]
- 27.Adeoti CO, Egbewale BE. Refractive errors in Mercyland specialist hospital, Osogbo, Western Nigeria. Niger Postgrad Med J. 2008;15:116–9. [PubMed] [Google Scholar]
- 28.Edwards MH, Lam CS. The epidemiology of myopia in Hong Kong. Ann Acad Med Singapore. 2004;33:34–8. [PubMed] [Google Scholar]


