Abstract
Context:
The world is aging rapidly through “demographic transition.” The aging leads to CI Refers as Cognitive Impairment (CI) – a risk factor for dementia. A community-based cross-sectional study was conducted among the elderly aged ≥50 years.
Objectives:
The objective of the study is to estimate the prevalence of cognitive dysfunction among the elderly and to identify the associated sociodemographic variables.
Settings and Design:
This was a community-based cross-sectional study in rural and urban field areas of a medical college.
Subjects and Methods:
Participants aged ≥50 years were interviewed using a structured questionnaire and screened for cognitive dysfunction using Gujarati version of Mini-Mental Status Examination. A score of 23 out of 30 was taken as the cutoff. Written informed consent was obtained from participants.
Statistical Analysis Used:
Univariate and multivariate analyses were done using SPSS version 17 and Epi Info version 6 to identify significant variables.
Results:
Of 560 participants, 140 (25%) had CI. Rural (27.6%) and female (29.8%) prevalence was higher than urban (18.5%) and male (19.1%) prevalence. On multivariate analysis, age ≥60 years (odds ratio [OR]: 2.98) and illiteracy (OR: 39.8) had significant positive association with outcome; being employed (OR: 0.18), living with spouse (OR: 0.07), and living with spouse and children (OR: 0.08) had significant negative association with outcome.
Conclusions:
CI – a precursor of dementia – has serious clinical and public health consequences. Awareness generation and capacity building of primary health-care workers and family caregivers are core control strategies.
Keywords: CI Refers as Cognitive Impairment, elderly, mini-mental status examination, prevalence study
INTRODUCTION
The world is aging rapidly through “demographic transition.” In 2011, 11% global[1] and 8% Indian population is >60 years and would reach 19% by 2050.[2] The aging leads to CI Refers as Cognitive Impairment (CI) – a risk factor for dementia.[3,4] CI defines a transitional stage between normal aging and dementia and reflects the clinical situation where a person has memory complaints and objective evidence of CI but no evidence of dementia.[3] Although CI is not uncommon in late life and may be due to the normal process of aging, neuropathological changes of Alzheimer's disease (AD) begin in the brain in the fifth decade of life years before clinical symptoms become evident.[4] AD pathology is more common in individuals with memory impairment who are not demented. Elderly individuals with memory impairment also have a rapid rate of conversion to AD.[4] Annual rates of conversion of mild CI Refers as Cognitive Impairment to dementia were found to be 5%–15%.[3] Considering usefulness of early screening (in 50s) in extending appropriate care to those at risk, the present study included participants in their 50s.
Studies in Taiwan[5] and India[6] reported a prevalence of 18.03% and 22.2%, respectively. No study on dementia or CI in the elderly could be identified from Gujarat. Hence, a community-based cross-sectional study was conducted among the elderly aged ≥50 years with the following objectives:
To estimate the prevalence of cognitive dysfunction among people aged ≥50 years
To identify the associated sociodemographic variables.
SUBJECTS AND METHODS
The community-based cross-sectional study was conducted in the rural and urban (three slums) field practice areas of medical college of Gujarat between March 2012 and August 2013. Individuals aged ≥50 years formed the study population.
Participant selection and recruitment
All individuals aged 50 years and above in rural and three out of six urban slum areas were line-listed from family records of the Department of Community Medicine and contacted through house-to-house visit by knocking each house with elderly once. Those who were willing to participate were evaluated for exclusion criteria. Those without exclusion criteria were asked to provide written informed consent and then interviewed. Uncooperative, terminally ill, and bedridden persons without dementia and persons with severe speech, visual, and hearing impairment were excluded from the study as they would be difficult to test for cognitive performance.
Study tools
Interviews were carried out using structured, coded questionnaires, and Mini-Mental Status Examination (MMSE) was used as screening tool for CI.
MMSE[7] contains 22 items which test various areas of cognitive functions. Hindi MMSE (HMSE)[8] was thought to be an appropriate screening tool considering lower literacy level among participants. English version of HMSE was translated into Gujarati and back-translated into English by two bilingual experts (percentage correlation = 87%). The score of 23 of 30 on Gujarati version of MMSE was selected as a cutoff value with sensitivity and specificity of 88% and 82%, respectively.[9]
Sample size
The minimum sample size was estimated based on preliminary survey of randomly selected 39 participants, residing in the study area, using Epi Info (version 6) stat calculator using population survey command. Parameters entered were total population: 5500, acceptable error: 3% on either side, alpha error: 0.1, and prevalence on pretest: 28.2%. Calculated minimum sample size was 546 at 90% confidence level.
Data management and statistical analysis
Data entry was done in MS Excel 2007. Data analysis was done using SPSS software version 17.0 (SPSS Inc., Chicago) and Epi info version 6.0 (Centers for disease control and prevention: Atlanta). association between outcome, and independent variables were explored by univariate analysis. Significant variables on univariate analysis were fitted into step-wise multiple logistic regression model and adjusted prevalence odds ratios (ORs) were calculated.
Ethical issues
The study was approved from Human Research Ethics Committee of the institute. Informed written consent was obtained from all participants in the local language.
RESULTS
A total of 560 (male – 251, 44.8% and female – 309, 55.2%) individuals were screened with MMSE (response rate = 64.9%). Rural (69.7%) and female (70.5%) response rates were greater than urban (55.6%) and male participants (59.1%). Distribution and prevalence of CI among study participants according to sociodemographic, education, occupation, and economic independent variables are detailed in Table 1.
Table 1.
Sociodemographic, education, occupation, and economic profile of participants (n=560)
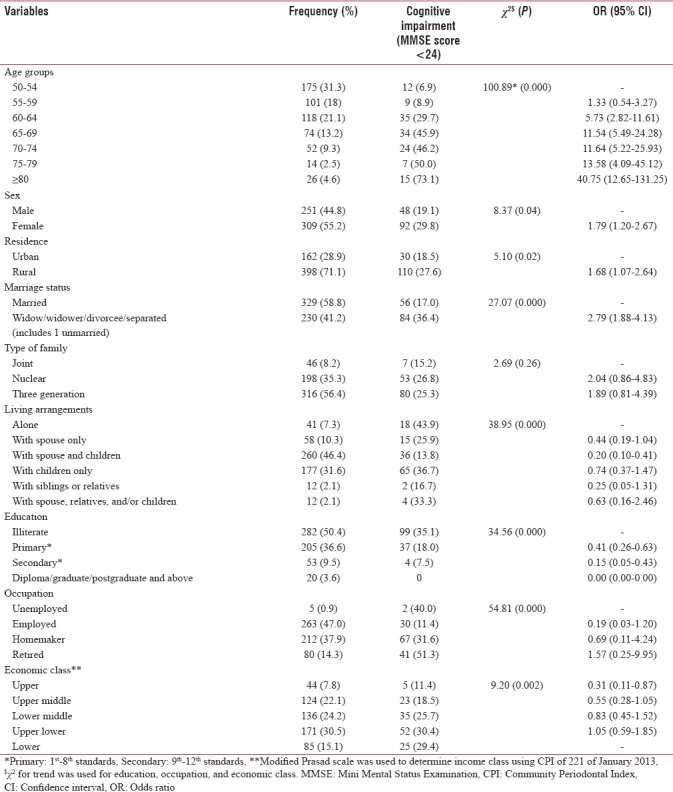
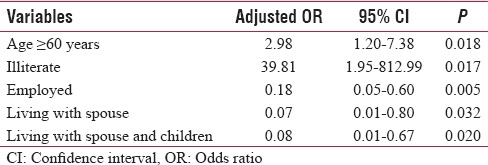
The overall prevalence of CI was 25%. Of various independent variables mentioned in Table 1, age ≥60 years (χ2 = 100.89, P = 0.000), female gender (χ2 = 8.37, P = 0.04), rural residence (χ2 = 5.10, P = 0.02), not having life partner (χ2 = 27.07, P = 0.000), living with spouse and living with spouse and children (χ2 = 38.9, P = 0.000), being educated (χ2 = 34.5, P = 0.000), being employed (χ2 = 54.8, P = 0.000), and belonging to upper economic class (χ2 = 9.2, P = 0.02) were significantly associated with CI. Type of family was not significantly associated with CI (χ2 = 2.69; P = 0.26) [Table 1]. Table 2 details significant independent variables on multivariate analysis along with respective adjusted ORs. Age ≥60 years (OR: 2.98; P = 0.018) and illiteracy (OR: 39.81; P = 0.017) have significant positive and being employed (OR: 0.18; P = 0.005), living with spouse (OR: 0.07, P = 0.032), and living with spouse and children (OR: 0.08, P = 0.02) have significant negative association with CI on multivariate analysis [Table 2].
Table 2.
Determinants of cognitive defect by step-wise logistic regression
DISCUSSION
In this study, the prevalence of CI was 25% with higher prevalence in rural and male participants. Poddar et al.[10] and Sharma et al.[11] also reported higher rural prevalence in North India. Goswami et al.[6] reported greater prevalence in females (Female: 23.7% vs. Male: 12.2%) in Haryana. The prevalence of CI increases with age in both genders. A study reported 15% prevalence in aged >80 years as to 2.6% in aged <60 years.[10] Age-related decreased brain volume, loss of myelin integrity, cortical thinning, and impaired secretion of neurotransmitters such as serotonin are attributed to CI.
Education and employment have strong negative and independent association with cognitive dysfunction.[12,13] Participants with high school or higher (8.2%) and primary education had one-fifth and one-fourth likelihood of CI than illiterates (39.6%).[5,10] Schmand et al.[13] reported consistent decline in CI prevalence as level of employment increased from unskilled (39.3%) to professional (1.3%). According to cognitive reserve (CR) hypothesis,[14] individuals with more CR (higher education, intelligence, and occupational attainment) are more successful at coping with brain damage and remain clinically intact for a longer period.
Social support in the form of living with spouse with/without children had protective association with CI on logistic regression. Fratiglioni et al.[15] found that being single (OR: 1.5; 95% CI: 0.9–2.5) and living alone (OR: 1.5; 95% CI: 1.0–2.1) had positive association with cognitive problems among Swedish elderly.
Our study makes significant contribution by screening older adults for the condition. It also investigates related sociodemographic factors. In our knowledge, no such study has attempted similar inquiry in the region. However, considering cross-sectional design, making causal inferences should exercise some caution and needs to be confirmed with more robust study design.
CONCLUSION
Serious clinical and public health consequences of CI Refers as Cognitive Impairment and thus dementia demands aawareness generation, capacity building of primary care workers in screening and community-based care and education of family care givers for dementia prevention and control.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge Dr. Soham Desai, Consultant Neurophysician of P. S. Medical College, Karamsad, for his technical input regarding topic and Mr. N. M. Panchal and Mrs. B. R. Patel for translation in Gujarati and back-translation in English of screening tool (MMSE), respectively.
REFERENCES
- 1.United Nations Population Division (UN), World Population Prospects: The 2010 Revision. New York: United Nations; 2011. [Last accessed on 2013 Jan 12]. Available from: http://www.esa.un.org/unpd/wpp/index.htm . [Google Scholar]
- 2.Agrawal A. Disability among the elder population of India: A public health concern. J Med Soc. 2016;30:15–9. [Google Scholar]
- 3.Burns A, Zaudig M. Mild cognitive impairment in older people. Lancet. 2002;360:1963–5. doi: 10.1016/S0140-6736(02)11920-9. [DOI] [PubMed] [Google Scholar]
- 4.DeCarli C. Mild cognitive impairment: Prevalence, prognosis, aetiology, and treatment. Lancet Neurol. 2003;2:15–21. doi: 10.1016/s1474-4422(03)00262-x. [DOI] [PubMed] [Google Scholar]
- 5.Wu MS, Lan TH, Chen CM, Chiu HC, Lan TY. Socio-demographic and health-related factors associated with cognitive impairment in the elderly in Taiwan. BMC Public Health. 2011;11:22. doi: 10.1186/1471-2458-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goswami A, Reddaiah VP, Kapoor SK, Singh B, Dey AB, Dwivedi SN, et al. Prevalence and Determinants of Cognitive Impairment in Rural Elderly Population in India, Helpage India Research and Development Journal. 2006;12:8–15. [Google Scholar]
- 7.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”.A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 8.Ganguli M, Ratcliff G, Chandra V, Sharma S, Gilbe J, Pandav R, et al. A hindi version of the MMSE: The development of a cognitive screening instrument for a largely illiterate rural elderly population in India. Indian Journal of Geriatric Psychiatry. 1995;10:367–77. [Google Scholar]
- 9.Shaji S, Bose S, Verghese A. Prevalence of dementia in an urban population in Kerala, India. Br J Psychiatry. 2005;186:136–40. doi: 10.1192/bjp.186.2.136. [DOI] [PubMed] [Google Scholar]
- 10.Poddar K, Kant S, Singh A, Singh TB. An epidemiological study of dementia among the habitants of eastern Uttar Pradesh, India. Ann Indian Acad Neurol. 2011;14:164–8. doi: 10.4103/0972-2327.85874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma D, Mazta S, Parashar A. Prevalence of cognitive impairment and related factors among elderly: A population-based study. J Dr NTR Univ Health Sci. 2013;2:171–6. [Google Scholar]
- 12.Ngandu T, von Strauss E, Helkala EL, Winblad B, Nissinen A, Tuomilehto J, et al. Education and dementia: What lies behind the association? Neurology. 2007;69:1442–50. doi: 10.1212/01.wnl.0000277456.29440.16. [DOI] [PubMed] [Google Scholar]
- 13.Schmand B, Smit JH, Geerlings MI, Lindeboom J. The effects of intelligence and education on the development of dementia. A test of the brain reserve hypothesis. Psychol Med. 1997;27:1337–44. doi: 10.1017/s0033291797005461. [DOI] [PubMed] [Google Scholar]
- 14.Stern Y. Cognitive reserve and alzheimer disease. Alzheimer Dis Assoc Disord. 2006;20:112–7. doi: 10.1097/01.wad.0000213815.20177.19. [DOI] [PubMed] [Google Scholar]
- 15.Fratiglioni L, Wang HX, Ericsson K, Maytan M, Winblad B. Influence of social network on occurrence of dementia: A community-based longitudinal study. Lancet. 2000;355:1315–9. doi: 10.1016/S0140-6736(00)02113-9. [DOI] [PubMed] [Google Scholar]


