Summary
Cardiovascular disease is the leading cause of death and disability worldwide. Among cardiovascular causes of death, venous thrombosis (VT) is ranked third most common in the world. Venous thrombi have high red blood cell and fibrin content; however, the pathophysiologic mechanisms that contribute to venous thrombus composition and stability are still poorly understood. This article reviews biological, biochemical, and biophysical contributions of fibrinogen, factor XIII, and red blood cells to VT, and new evidence suggesting interactions between these components mediate venous thrombus composition and size.
Keywords: clot retraction, factor XIII, fibrinogen, platelet, red blood cell, venous thrombosis
Introduction
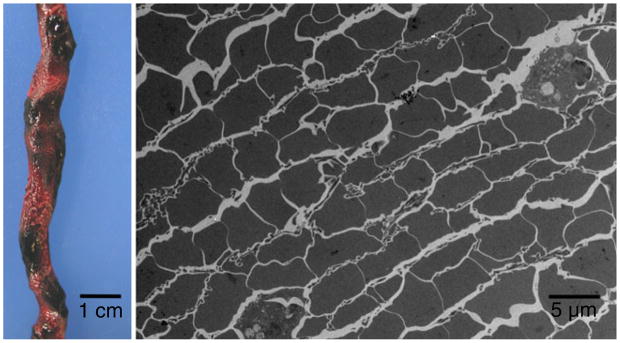
Venous thrombosis (VT) is initiated by endothelial dysfunction and inappropriate expression of plasma and cellular procoagulant activity under low blood flow/stasis (so-called Virchow’s Triad). The epidemiology, risk factors, and treatment of VT have been recently reviewed [1]. However, the pathophysiologic mechanisms that contribute to thrombus formation, composition, and stability are still poorly understood. Clues may be found in the distinctive appearance of venous thrombi, which demonstrate regions of high red blood cell (RBC) and fibrin content (so-called “red thrombi”). Notably, RBCs can be found between layers of fibrin in a ‘brick-and-mortar’ construction (Fig. 1), where they lose their typical discoid shape and acquire a compressed morphology recently named polyhedrocytes [2]. These observations suggest RBCs and fibrin(ogen) interact during VT and that thrombi undergo substantial consolidation during their maturation.
Fig. 1.
Venous thrombi contain regions of high red blood cell (RBC) and fibrin content. Left) Gross image of a segment of human venous thrombus (pulmonary embolus) collected at autopsy at UNC Hospitals. Note the presence of darker (RBC rich) regions. Image courtesy of Vincent J. Moylan, Jr, MS, PA(ASCP), UNC at Chapel Hill, School of Medicine. Right) Transmission electron micrograph of a pulmonary embolus showing the ‘brick-and-mortar’ organization of RBCs and fibrin within the thrombus.
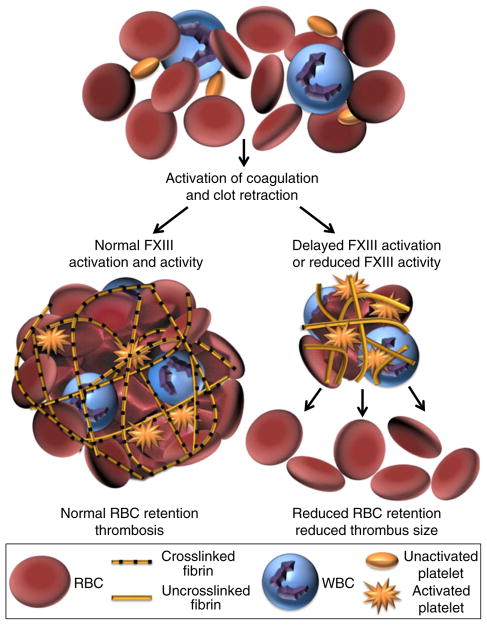
We recently investigated the contribution of factor XIII (FXIII) to clot formation in whole blood [3]. Compared to controls, FXIII-deficient whole blood clots from humans and mice exhibit significantly reduced retention of RBCs during clot retraction. Furthermore, when subjected to an in vivo VT model, FXIII-A−/− mice produce thrombi that have lower RBC content and are smaller than thrombi from wild-type mice [3]. These findings challenge the paradigm that RBCs are simply trapped during VT and suggest RBC retention in thrombi is an active process mediated, in part, by FXIII(a) (Fig. 2). However, the molecular origins of this mechanism remain poorly defined. Herein, we briefly review the established contributions of fibrinogen, FXIII, and RBCs to coagulation, and evidence supporting their potential roles in VT.
Fig. 2.
Factor XIII(a) (FXIII[a]) mediates red blood cell (RBC) retention in thrombi. During venous thrombosis (VT), platelets mediate thrombus contraction. FXIII activity increases RBC retention in retracted thrombi (left arrow). If FXIII activity is deficient or activation is delayed, fewer RBCs are retained, resulting in a smaller thrombus (right arrow).
Fibrinogen
Fibrinogen structure, fibrin formation, and fibrin mechanical properties
Fibrinogen circulates at high concentrations (2–4 mg mL−1), and levels may increase further during inflammation. The fibrinogen molecule consists of two sets each of three polypeptide chains (AαBβγ)2. The γ-chain can undergo alternative splicing, leading to replacement of 4 C-terminal amino acids with a unique 20 amino acid sequence (γ′), the γ′-chain is present in 8–15% of fibrinogen molecules (as γA/γ′) in healthy individuals. During coagulation, thrombin cleaves N-terminal peptides from the Aα- and Bβ-chains promoting the formation of protofibrils and subsequently fibrin fibers. Branching results in the characteristic fibrin network seen in micrographs of purified and plasma clots. The thrombin and fibrinogen concentrations present during clot formation influence fibrin network structure and stability [4,5].
Crosslinked fibrin may be best known for its ability to stabilize clots. This property is determined at both micro- and macroscales. Individual fibrin fibers have astounding viscoelasticity; crosslinked fibrin fibers can be stretched to 2.5 times their original length before rupturing, making fibrin as extensible as spider silk [6–8]. Moreover, elastic recovery of fibers from elongations up to 100% can occur within milliseconds [9]. Branchpoints within the fibrin network are surprisingly strong; when strained, individual fibers fail before branchpoints fail [10]. Thus, it is not surprising that fully formed fibrin clots have similar extensibility and elasticity as individual fibers. Fibrin viscoelasticity is strongly influenced by FXIII(a)-dependent crosslinking (discussed below).
Fibrinogen and VT
The complex relationships between fibrinogen and fibrin (collectively fibrin[ogen]) concentration, fibrin structure, fibrin viscoelastic properties, and VT risk have been the subject of numerous investigations. These studies suggest fibrin(ogen) contributes to VT via multiple mechanisms.
Hyperfibrinogenemia and VT
Elevated total fibrinogen is correlated with increased VT risk [11–15], and risk is concentration dependent and present in both men and women. Studies using transgenic mice and murine infusion models have associated elevated fibrinogen with increased prothrombotic biomarkers (e.g., D-dimer) [16], shorter time to vessel occlusion, and increased thrombus fibrin content [17]. Compared to controls, thrombi in fibrinogen-infused mice also show increased resistance to fibrinolysis [18]. These findings indicate hyperfibrinogenemia is not merely a biomarker of VT risk, but is causative in VT etiology.
Abnormal fibrin structure and stability in VT
Several studies have reported abnormal plasma clot structure and/or stability in VT, even when circulating fibrinogen levels are normal. Compared to controls, plasma clots from patients with a history of cryptogenic stroke or idiopathic VT show increased fibrin network density, reduced permeability, and increased lysis times [19,20]. Interestingly, compared to plasma clots from patients with deep vein thrombosis, plasma clots from patients that experienced pulmonary embolism are less compact and more susceptible to fibrinolysis [20,21]. In addition, although congenital dysfibrinogenemia is rare among VT patients [12], ~20% of dysfibrinogenemias are associated with thrombophilia and demonstrate abnormal fibrin network structure, reduced interactions between fibrin(ogen) and tissue plasminogen activator (tPA) [22] or plasminogen [23], and increased resistance to lysis. In total, these in vitro data suggest abnormal fibrin network structure and stability contribute to VT.
Fibrinogen γ′-chain and VT
The genes encoding the fibrinogen chains are coregulated to maintain the level of fibrinogen in circulation [reviewed in Ref. 24]. However, the levels of the γA- and γ′-chains are mediated by independent mechanisms that differentially regulate their expression. Expression of γ′-containing fibrinogen is disproportionally increased by interleukin-6-dependent inflammatory responses [25], suggesting an independent relationship between the γ′-chain, inflammation, and thrombosis. Accordingly, although total fibrinogen levels are positively correlated with thrombosis risk, the fraction of circulating γ′-fibrinogen (γ′/total fibrinogen ratio) modulates risk independently of the total fibrinogen level. Notably, a reduced γ′-to-total fibrinogen ratio is associated with increased risk of VT [26,27], suggesting γ′ fibrinogen is protective in VT.
Determining the operant mechanisms has been difficult because γA/γ′ fibrinogen exhibits both procoagulant and antithrombotic properties [reviewed in Ref. 28]. Briefly, compared to γA/γA clots, clots that contain γ′ fibrinogen have a denser network of thin fibrin fibers, reduced permeability, reduced plasminogen binding, and increased resistance to fibrinolysis. Compared to γA/γA fibrinogen, γA/γ′ fibrinogen can also bind and sequester thrombin with higher affinity, protecting thrombin from inactivation by antithrombin. These properties are consistent with prothrombotic functions. However, γ′ fibrinogen also exhibits impaired polymerization. Recent studies have shown that a γ′ carboxyl-terminal peptide reduces plasma thrombin generation even in the presence of anti-factor VIII antibody, suggesting γ′/thrombin interactions reduce factor V activation [29]. By reducing thrombin generation, this peptide also increases the sensitivity of coagulation to activated protein C, thus augmenting endogenous anticoagulant mechanisms [30].
Studies to determine the contribution of the γ′-chain to thrombosis in vivo have consistently demonstrated anti-thrombotic effects [31–33]. Transgenic expression of the human γ′-chain reduces thrombus volume in mice that are heterozygous for the factor V Leiden mutation [31]. A peptide mimicking the γ′-chain C-terminus inhibits fibrin-rich thrombus formation in a baboon model [32]. We recently infused mice with γA/γA or γA/γ′ fibrinogen isolated from human plasma [33]. Compared to controls, γA/γA infusion shortens the time to carotid artery occlusion, whereas γA/γ′ infusion does not. Additionally, γA/γ′ infusion reduces levels of circulating thrombin–anti-thrombin complexes [33]. These data are consistent with the premise that the γ′-chain reduces thrombin activity. By extension, these data implicate the γA-chain as the prothrombotic mediator in hyperfibrinogenemia-related thrombosis. Together, these findings illustrate pleiotropic contributions of fibrinogen to VT.
Fibrin(ogen) interactions with blood proteins and cells
Most studies of fibrin(ogen) function have used purified systems or plasmas. These studies have identified binding sites on fibrin(ogen) for soluble proteins involved in clot formation, stabilization, and fibrinolysis, including thrombin, FXIII, fibronectin, tPA, plasminogen, and plasmin. Fibrin(ogen) also interacts with cells and these interactions may contribute to the incorporation of cells into venous thrombi. For example, fibrin(ogen) contains recognition sequences for integrins including αMβ2, αIIbβ3, and αvβ3, which mediate fibrin(ogen) interactions with leukocytes, platelets, and endothelial cells, respectively. These interactions modulate leukocyte function, platelet aggregation, and clot retraction and may anchor thrombi to the endothelium. Fibrin(ogen) also binds to RBCs via a motif involving fibrinogen Aα-chain residues 207–303 [34]. This interaction influences both the erythrocyte sedimentation rate and blood viscosity (discussed below) [34–36].
FXIII
FXIII structure and activation
FXIII is a member of the transglutaminase superfamily and circulates at 14–28 μg mL−1 [reviewed in Ref. 37]. Briefly, plasma FXIII consists of two catalytic subunits (FXIII-A) and two non-catalytic subunits (FXIII-B) that are tightly associated (Kd ~10−10 M) [38] in a non-covalent, heterotetramer (FXIII-A2B2). Essentially all FXIII-A2B2 circulates bound to fibrinogen. Homodimeric FXIII-A (FXIII-A2) is also present in cells, including megakaryocytes and platelets.
FXIII-A2B2 is activated by thrombin-catalyzed release of N-terminal peptides from the FXIII-A subunits and calcium-mediated dissociation of the FXIII-B subunits, yielding activated FXIII-A2 (FXIIIa). FXIII-A2B2 activation is accelerated when it is bound to fibrinogen [39,40]. Interestingly, as FXIII-A2B2 does not compete with FXIIIa for binding to fibrin, FXIII-A2B2 and FXIIIa appear to bind to somewhat distinct sites [40]. Older studies suggested FXIII-A2B2 binds preferentially to the alternatively spliced fibrinogen γ′-chain; however, FXIII-A2B2 binds to recombinant γ- and γ′-containing fibrinogen molecules with similar affinity (Kd ~40 nM) [41], suggesting residues outside the γ′ region mediate this interaction. Smith et al. [42] detected high affinity binding of FXIII-A2B2 to a peptide containing amino acid residues 371–425 of the fibrinogen αC domain (Kd 5–30 nM); however, those experiments suggested the interaction between FXIII-A2B2 and the αC region may arise during FXIII activation and that other fibrinogen residues fulfill the carrier function for FXIII-A2B2. We recently showed that fibrin(ogen) with mutations within residues γ390–396 exhibits decreased coprecipitation with FXIII-A2B2, suggesting these γ-chain residues mediate this carrier function in blood [3]. Localization of FXIII-A2B2 at residues γ390–396 would conveniently position FXIIIa for rapid translocation to its nearby substrate residues on the γ-chain (Q398, Q399, and K406) following its activation. Interestingly, mice with alanine mutations in fibrinogen residues γ390–396 (Fibγ390–396A) exhibit delayed FXIIIa activation and delayed fibrin crosslinking [3]. Similar to the FXIII-A−/− mice, venous thrombi from Fibγ390–396A mice show reduced RBC content and smaller venous thrombi, suggesting the timing of FXIII activation and activity are critical determinants of venous thrombus composition and size [3].
FXIIIa transglutaminase activity and fibrin crosslinking
Both plasma- and platelet-derived FXIIIa catalyze the formation of ε-N-(γ-glutamyl)-lysyl crosslinks within fibrin and between fibrin and antifibrinolytic proteins (e.g., α2-antiplasmin) [43–45]. Within fibrin, FXIIIa establishes crosslinks between glutamine residues 398/399 and lysine 406 in the fibrin γ-chain and subsequently between glutamine and lysine residues in the α-chain.
Crosslinking alters fibrin network morphology, including reduced pore size, higher fiber density, and thinner fibers, although these changes are rather small [46,47]. Perhaps more importantly, FXIIIa has profound effects on fibrin integrity. Fibrin crosslinking decreases fiber extensibility and elasticity and increases the elastic modulus (stiffness) of both individual fibers [6–8] and whole clot networks [48]. FXIIIa-induced crosslinking of γ-chains, alone, is insufficient to stiffen fibrin networks, suggesting clot rigidity is associated with the formation of γ-multimers, α-polymers, and αγ-hybrid species [49]. Notably, studies using recombinant fibrinogen that cannot undergo γ-chain crosslinking (γQ398N/Q399N/K406R) reveal minor contributions of γ-chain crosslinking to fibrin elasticity, but larger contributions of α-chain crosslinking [50–52]; clot stiffness increases 2.5-fold even with only α-chain crosslinking, and only a smaller increase is observed with full (γ- and α-chain) crosslinking [50]. Collectively, these studies suggest γ- and α-chain crosslinking make distinct contributions to clot function.
FXIII polymorphisms in VT
Genetic studies have associated FXIII polymorphisms with variable risk for VT, suggesting that FXIII activation kinetics and/or function alter clot quality [reviewed in Ref. 53]. The FXIII Val34Leu polymorphism has received the most attention. This polymorphism is present in ~25% of European Caucasians and causes 2.5-fold faster FXIII activation and faster fibrin crosslinking in vitro [54–56]. The presence of this polymorphism may convey slight protection against VT in certain populations [55]. In plasmas with normal fibrinogen levels, this variant produces clots with thinner fibers and decreased permeability, whereas in plasmas with high fibrinogen, it produces thicker fibers and increased permeability and susceptibility to fibrinolysis [57]. Importantly, however, as most prior studies have used purified systems and cell-free plasmas, the contributions of FXIII activation/activity and the FXIII Val34Leu polymorphism in whole blood-based models of VT have not been fully defined.
Red blood cells
Findings that RBCs are a major determinant of venous thrombus size and that thrombus RBC content can be reduced by FXIII(a) inhibition [3] lead to important questions about the contributions of RBCs to venous thrombus formation and stability, and consequences of decreasing thrombus RBC content.
RBCs in circulation
RBCs have a characteristic biconcave but deformable structure that allows them to traverse capillary networks and deliver oxygen via their hemoglobin-rich cytoplasm. RBCs circulate at ~4.2–6.1 × 109 mL−1, although levels are slightly higher in men than in women. The RBC level can be elevated at high altitudes, in conditions associated with hypoxia (e.g., smoking, lung disease, and heart disease), and with hematologic disorders including polycythemia vera.
RBCs in coagulation and VT
Growing evidence suggests RBCs contribute to blood coagulation. For example, bleeding times shorten as hematocrit rises in anemic, normal, and polycythemic individuals [58]. In addition, elevated levels of RBCs are associated with increased VT risk in both men and women [59–62]. Abnormal RBC morphology and function, as exhibited in sickle cell disease (SCD), is also associated with VT [63]. However, the mechanism by which RBCs alter coagulation remains unclear. The effects of RBCs on coagulation are usually attributed to their rheological effects on blood. However, RBCs also interact with other blood cells, can support thrombin generation, and have antifibrinolytic activity.
RBCs mediate blood rheology
RBCs are the major determinant of blood rheology because of their prevalence, size, deformability, and ability to undergo reversible aggregation. In venous circulation (low shear), RBCs tend to aggregate (rouleaux formation) and increase blood viscosity. Increased blood viscosity is a risk factor for VT [64]. RBC aggregation and blood viscosity are mediated by interactions between the RBC membrane and plasma proteins, including fibrinogen, immunoglobulins, and albumin [65]. Consequently, inflammatory processes that increase fibrinogen levels also increase blood viscosity. These effects have been implicated in the association between elevated hematocrit, hyperfibrinogenemia, and VT. However, it remains unclear whether this relationship is merely correlative or is also causative in VT etiology.
RBCs interact with fibrin(ogen)
Two potential RBC receptors have been implicated in fibrinogen binding. Fibrinogen–RBC interactions can be inhibited by the integrin-blocking molecule eptifibatide and are not supported by RBCs lacking β3 isolated from patients with Glanzmann thrombasthenia [66], implicating β3 or a β3-like molecule on the RBC surface. However, that study [66] did not rule out the possibility that RBC-bound platelets mediate this interaction. Fibrinogen–RBC interactions can also be blocked with an antibody against the integrin-associated protein CD47 [67]. As CD47 was originally identified for its interaction with αvβ3, αIIbβ3, and α2β1 integrins, it is possible that the RBC binding site comprises a complex with both of these molecules. It is interesting to speculate that interactions between one or both of these receptors and fibrin(ogen) contribute to RBC incorporation in venous thrombi or that blocking these interactions may reduce blood viscosity, and consequently VT risk.
RBCs interact with cells
RBCs can interact with other cells, including leukocytes, platelets, and endothelial cells. For example, RBC ICAM-4 can bind leukocyte β1 and β2 integrins [68,69] and platelet αIIbβ3 [70]. RBC ICAM-4 also interacts with integrin αv [71]. RBCs are the first cells to adhere to ferric chloride-treated, intact arterial endothelium, prior to the arrival of platelets [72]. This interaction is not dependent on von Willebrand factor or GP1bα; however, the molecular receptors on RBCs and the endothelium that mediate this interaction have not been identified [72]. Interestingly, RBCs exhibit temporal changes in gene expression during erythropoiesis [73], suggesting stage-specific receptors may decorate RBCs during differentiation and further refine these interactions.
RBCs support thrombin generation
A small percentage (~0.5%) of RBCs circulate with exposed phosphatidylserine (PS) on their outer membranes [74], suggesting RBCs can assemble prothrombinase complexes and support thrombin generation. Interestingly, although levels of both PS-positive RBCs and platelets are elevated in patients with SCD genotypes, only PS-positive RBCs correlate with circulating biomarkers of coagulation activation, including F1.2 and D-dimer [74]. This finding suggests PS-positive RBCs are the primary cell responsible for thrombophilia in SCD. In vitro studies support this premise; when added to platelet-poor plasma, RBCs shorten the lag time and increase the peak of thrombin generation similar to that seen with platelets [75,76], although in contrast to platelets, thrombin generation on RBCs occurs through the meizothrombin pathway [77]. RBCs can also produce microvesicles that activate proco-agulant and complement pathways in vitro [78–80]. These findings suggest RBCs promote VT and that blocking RBC incorporation in venous thrombi would decrease fibrin formation.
RBCs alter fibrin structure and stability
RBCs alter fibrin network structure [81,82] and reduce fibrin network permeability [83]. RBCs also suppress plasmin generation and reduce clot dissolution [82]. In the presence of the substantial contractile forces induced by platelets during clot retraction [84,85], RBCs are dramatically compressed, which further reduces clot permeability and restricts access of fibrinolytic enzymes to the clot [2,86]. Although this phenomenon was noted in thrombi harvested from the arterial vasculature [2], intravascular clot contraction and polyhedrocyte formation is likely to have a significant impact on VT as well, because these thrombi contain platelets and large numbers of RBCs. These data suggest reducing RBC content in thrombi may be a novel therapeutic approach for reducing VT.
Conclusions
Continued studies are needed to delineate the pathophysiologic mechanisms that mediate fibrinogen, FXIII, and RBC interactions during VT. Identification of the RBC receptor that binds fibrin(ogen), and characterization of the FXIIIa substrate that mediates RBC retention in retracted clots may provide new therapeutic targets for reducing blood viscosity and decreasing VT. Importantly, future investigations of pathologic mechanisms mediating VT should utilize holistic systems that include plasma and cells and permit the dynamic interplay between fibrinogen, FXIII, and RBCs that occurs during VT in vivo.
Acknowledgments
We acknowledge Drs. Nathan Hudson, Matthew Whelihan, and Jonathan Foley for helpful discussion.
Footnotes
Disclosure of Conflict of Interests
The authors state that they have no conflict of interest.
References
- 1.Wolberg AS, Rosendaal FR, Weitz JI, Jaffer IH, Agnelli G, Baglin T, Mackman N. Venous thrombosis. Nat Rev Dis Pri. 2015;1:15006. doi: 10.1038/nrdp.2015.6. [DOI] [PubMed] [Google Scholar]
- 2.Cines DB, Lebedeva T, Nagaswami C, Hayes V, Massefski W, Litvinov RI, Rauova L, Lowery TJ, Weisel JW. Clot contraction: compression of erythrocytes into tightly packed polyhedra and redistribution of platelets and fibrin. Blood. 2014;123:1596–603. doi: 10.1182/blood-2013-08-523860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aleman MM, Byrnes JR, Wang J-G, Tran R, Lam WA, Di Paola J, Mackman N, Degen JL, Flick MJ, Wolberg AS. Factor XIII activity mediates red blood cell retention in venous thrombi. J Clin Invest. 2014;124:3590–600. doi: 10.1172/JCI75386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolberg AS. Thrombin generation and fibrin clot structure. Blood Rev. 2007;21:131–42. doi: 10.1016/j.blre.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Lord ST. Molecular mechanisms affecting fibrin structure and stability. Arterioscler Thromb Vasc Biol. 2011;31:494–9. doi: 10.1161/ATVBAHA.110.213389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Collet JP, Shuman H, Ledger RE, Lee S, Weisel JW. The elasticity of an individual fibrin fiber in a clot. Proc Natl Acad Sci USA. 2005;102:9133–7. doi: 10.1073/pnas.0504120102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu W, Jawerth LM, Sparks EA, Falvo MR, Hantgan RR, Superfine R, Lord ST, Guthold M. Fibrin fibers have extraordinary extensibility and elasticity. Science. 2006;313:634. doi: 10.1126/science.1127317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu W, Carlisle CR, Sparks EA, Guthold M. The mechanical properties of single fibrin fibers. J Thromb Haemost. 2010;8:1030–6. doi: 10.1111/j.1538-7836.2010.03745.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hudson NE, Ding F, Bucay I, O’Brien ET, 3rd, Gorkun OV, Superfine R, Lord ST, Dokholyan NV, Falvo MR. Submillisecond elastic recoil reveals molecular origins of fibrin fiber mechanics. Biophys J. 2013;104:2671–80. doi: 10.1016/j.bpj.2013.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlisle CR, Sparks EA, Der Loughian C, Guthold M. Strength and failure of fibrin fiber branchpoints. J Thromb Haemost. 2010;8:1135–8. doi: 10.1111/j.1538-7836.2010.03824.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koster T, Rosendaal FR, Reitsma PH, van der Velden PA, Briet E, Vandenbroucke JP. Factor VII and fibrinogen levels as risk factors for venous thrombosis. A case–control study of plasma levels and DNA polymorphisms–the Leiden Thrombophilia Study (LETS) Thromb Haemost. 1994;71:719–22. [PubMed] [Google Scholar]
- 12.Haverkate F, Samama M. Familial dysfibrinogenemia and thrombophilia. Report on a study of the SSC Subcommittee on Fibrinogen. Thromb Haemost. 1995;73:151–61. [PubMed] [Google Scholar]
- 13.Austin H, Hooper WC, Lally C, Dilley A, Ellingsen D, Wideman C, Wenger NK, Rawlins P, Silva V, Evatt B. Venous thrombosis in relation to fibrinogen and factor VII genes among African-Americans. J Clin Epidemiol. 2000;53:997–1001. doi: 10.1016/s0895-4356(00)00191-8. [DOI] [PubMed] [Google Scholar]
- 14.Kamphuisen PW, Eikenboom JC, Vos HL, Pablo R, Sturk A, Bertina RM, Rosendaal FR. Increased levels of factor VIII and fibrinogen in patients with venous thrombosis are not caused by acute phase reactions. Thromb Haemost. 1999;81:680–3. [PubMed] [Google Scholar]
- 15.van Hylckama Vlieg A, Rosendaal FR. High levels of fibrinogen are associated with the risk of deep venous thrombosis mainly in the elderly. J Thromb Haemost. 2003;1:2677–8. doi: 10.1111/j.1538-7836.2003.0543b.x. [DOI] [PubMed] [Google Scholar]
- 16.Kerlin B, Cooley BC, Isermann BH, Hernandez I, Sood R, Zogg M, Hendrickson SB, Mosesson MW, Lord S, Weiler H. Cause–effect relation between hyperfibrinogenemia and vascular disease. Blood. 2004;103:1728–34. doi: 10.1182/blood-2003-08-2886. [DOI] [PubMed] [Google Scholar]
- 17.Machlus KR, Cardenas JC, Church FC, Wolberg AS. Causal relationship between hyperfibrinogenemia, thrombosis, and resistance to thrombolysis in mice. Blood. 2011;117:4953–63. doi: 10.1182/blood-2010-11-316885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Machlus KR, Lin F-C, Wolberg AS. Procoagulant activity induced by vascular injury determines contribution of elevated factor VIII to thrombosis and thrombus stability in mice. Blood. 2011;118:390–8. doi: 10.1182/blood-2011-06-362814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Undas A, Podolec P, Zawilska K, Pieculewicz M, Jedlinski I, Stepien E, Konarska-Kuszewska E, Weglarz P, Duszynska M, Hanschke E, Przewlocki T, Tracz W. Altered fibrin clot structure/function in patients with cryptogenic ischemic stroke. Stroke. 2009;40:1499–501. doi: 10.1161/STROKEAHA.108.532812. [DOI] [PubMed] [Google Scholar]
- 20.Undas A, Zawilska K, Ciesla-Dul M, Lehmann-Kopydlowska A, Skubiszak A, Ciepluch K, Tracz W. Altered fibrin clot structure/function in patients with idiopathic venous thromboembolism and in their relatives. Blood. 2009;114:4272–8. doi: 10.1182/blood-2009-05-222380. [DOI] [PubMed] [Google Scholar]
- 21.Martinez MR, Cuker A, Mills AM, Crichlow A, Lightfoot RT, Chernysh IN, Nagaswami C, Weisel JW, Ischiropoulos H. Enhanced lysis and accelerated establishment of viscoelastic properties of fibrin clots are associated with pulmonary embolism. Am J Physiol Lung Cell Mol Physiol. 2014;306:L397–404. doi: 10.1152/ajplung.00265.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Engesser L, Koopman J, de Munk G, Haverkate F, Novakova I, Verheijen JH, Briet E, Brommer EJ. Fibrinogen nijmegen: congenital dysfibrinogenemia associated with impaired t-PA mediated plasminogen activation and decreased binding of t-PA. Thromb Haemost. 1988;60:113–20. [PubMed] [Google Scholar]
- 23.Lijnen HR, Soria J, Soria C, Collen D, Caen JP. Dysfibrinogenemia (fibrinogen Dusard) associated with impaired fibrin-enhanced plasminogen activation. Thromb Haemost. 1984;51:108–9. [PubMed] [Google Scholar]
- 24.Fish RJ, Neerman-Arbez M. Fibrinogen gene regulation. Thromb Haemost. 2012;108:419–26. doi: 10.1160/TH12-04-0273. [DOI] [PubMed] [Google Scholar]
- 25.Rein-Smith CM, Anderson NW, Farrell DH. Differential regulation of fibrinogen gamma chain splice isoforms by interleukin-6. Thromb Res. 2013;131:89–93. doi: 10.1016/j.thromres.2012.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uitte de Willige S, de Visser MC, Houwing-Duistermaat JJ, Rosendaal FR, Vos HL, Bertina RM. Genetic variation in the fibrinogen gamma gene increases the risk for deep venous thrombosis by reducing plasma fibrinogen gamma’ levels. Blood. 2005;106:4176–83. doi: 10.1182/blood-2005-05-2180. [DOI] [PubMed] [Google Scholar]
- 27.Nowak-Gottl U, Weiler H, Hernandez I, Thedieck S, Seehafer T, Schulte T, Stoll M. Fibrinogen alpha and gamma genes and factor V Leiden in children with thromboembolism: results from 2 family-based association studies. Blood. 2009;114:1947–53. doi: 10.1182/blood-2009-04-218727. [DOI] [PubMed] [Google Scholar]
- 28.Uitte de Willige S, Standeven KF, Philippou H, Ariëns RA. The pleiotropic role of the fibrinogen gamma’ chain in hemostasis. Blood. 2009;114:3994–4001. doi: 10.1182/blood-2009-05-217968. [DOI] [PubMed] [Google Scholar]
- 29.Omarova F, Uitte De Willige S, Ariëns RA, Rosing J, Bertina RM, Castoldi E. Inhibition of thrombin-mediated factor V activation contributes to the anticoagulant activity of fibrinogen gamma’. J Thromb Haemost. 2013;11:1669–78. doi: 10.1111/jth.12354. [DOI] [PubMed] [Google Scholar]
- 30.Omarova F, Uitte de Willige S, Simioni P, Ariëns RA, Bertina RM, Rosing J, Castoldi E. Fibrinogen gamma’ increases the sensitivity to activated protein C in normal and factor V Leiden plasma. Blood. 2014;124:1531–8. doi: 10.1182/blood-2014-02-554055. [DOI] [PubMed] [Google Scholar]
- 31.Mosesson MW, Cooley BC, Hernandez I, Diorio JP, Weiler H. Thrombosis risk modification in transgenic mice containing the human fibrinogen thrombin-binding gamma’ chain sequence. J Thromb Haemost. 2009;7:102–10. doi: 10.1111/j.1538-7836.2008.03213.x. [DOI] [PubMed] [Google Scholar]
- 32.Lovely RS, Boshkov LK, Marzec UM, Hanson SR, Farrell DH. Fibrinogen gamma’ chain carboxy terminal peptide selectively inhibits the intrinsic coagulation pathway. Br J Haematol. 2007;139:494–503. doi: 10.1111/j.1365-2141.2007.06825.x. [DOI] [PubMed] [Google Scholar]
- 33.Walton BL, Getz TM, Bergmeier W, Lin F-C, Uitte de Willige S, Wolberg AS. The fibrinogen gamma A/gamma’ isoform does not promote acute arterial thrombosis in mice. J Thromb Haemost. 2014;12:680–9. doi: 10.1111/jth.12534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maeda N, Seike M, Kume S, Takaku T, Shiga T. Fibrinogen-induced erythrocyte aggregation: erythrocyte-binding site in the fibrinogen molecule. Biochim Biophys Acta. 1987;904:81–91. doi: 10.1016/0005-2736(87)90089-7. [DOI] [PubMed] [Google Scholar]
- 35.Lominadze D, Dean WL. Involvement of fibrinogen specific binding in erythrocyte aggregation. FEBS Lett. 2002;517:41–4. doi: 10.1016/s0014-5793(02)02575-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rampling MW. The binding of fibrinogen and fibrinogen degradation products to the erythrocyte membrane and its relationship to haemorheology. Acta Biol Med Ger. 1981;40:373–8. [PubMed] [Google Scholar]
- 37.Muszbek L, Bereczky Z, Bagoly Z, Komaromi I, Katona E. Factor XIII: a coagulation factor with multiple plasmatic and cellular functions. Physiol Rev. 2011;91:931–72. doi: 10.1152/physrev.00016.2010. [DOI] [PubMed] [Google Scholar]
- 38.Katona E, Penzes K, Csapo A, Fazakas F, Udvardy ML, Bagoly Z, Orosz ZZ, Muszbek L. Interaction of factor XIII subunits. Blood. 2014;123:1757–63. doi: 10.1182/blood-2013-10-533596. [DOI] [PubMed] [Google Scholar]
- 39.Greenberg CS, Achyuthan KE, Fenton JW., 2nd Factor XIIIa formation promoted by complexing of alpha-thrombin, fibrin, and plasma factor XIII. Blood. 1987;69:867–71. [PubMed] [Google Scholar]
- 40.Hornyak TJ, Shafer JA. Interactions of factor XIII with fibrin as substrate and cofactor. Biochemistry. 1992;31:423–9. doi: 10.1021/bi00117a017. [DOI] [PubMed] [Google Scholar]
- 41.Gersh KC, Lord ST. An investigation of factor XIII binding to recombinant γ′/γ′ and γ/γ′ fibrinogen. Blood. 2006;108:485a. [Google Scholar]
- 42.Smith KA, Adamson PJ, Pease RJ, Brown JM, Balmforth AJ, Cordell PA, Ariëns RA, Philippou H, Grant PJ. Interactions between factor XIII and the alphaC region of fibrinogen. Blood. 2011;117:3460–8. doi: 10.1182/blood-2010-10-313601. [DOI] [PubMed] [Google Scholar]
- 43.Siebenlist KR, Mosesson MW. Progressive cross-linking of fibrin gamma-chains increases resistance to fibrinolysis. J Biol Chem. 1994;269:28414–9. [PubMed] [Google Scholar]
- 44.Fraser SR, Booth NA, Mutch NJ. The antifibrinolytic function of factor XIII is exclusively expressed through alpha-antiplasmin cross-linking. Blood. 2011;117:6371–4. doi: 10.1182/blood-2011-02-333203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mitchell JL, Lionikiene AS, Fraser SR, Whyte CS, Booth NA, Mutch NJ. Functional factor XIII-A is exposed on the stimulated platelet surface. Blood. 2014;124:3982–90. doi: 10.1182/blood-2014-06-583070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ryan EA, Mockros LF, Weisel JW, Lorand L. Structural origins of fibrin clot rheology. Biophys J. 1999;77:2813–26. doi: 10.1016/S0006-3495(99)77113-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hethershaw EL, Cilia La Corte AL, Duval C, Ali M, Grant PJ, Ariëns RA, Philippou H. The effect of blood coagulation factor XIII on fibrin clot structure and fibrinolysis. J Thromb Haemost. 2014;12:197–205. doi: 10.1111/jth.12455. [DOI] [PubMed] [Google Scholar]
- 48.Glover CJ, McIntire LV, Brown CH, 3rd, Natelson EA. Rheological properties of fibrin clots. Effects of fibrinogen concentration, factor XIII deficiency, and factor XIII inhibition. J Lab Clin Med. 1975;86:644–56. [PubMed] [Google Scholar]
- 49.Ryan EA, Mockros LF, Stern AM, Lorand L. Influence of a natural and a synthetic inhibitor of factor XIIIa on fibrin clot rheology. Biophys J. 1999;77:2827–36. doi: 10.1016/S0006-3495(99)77114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Standeven KF, Carter AM, Grant PJ, Weisel JW, Chernysh I, Masova L, Lord ST, Ariëns RA. Functional analysis of fibrin {gamma}-chain cross-linking by activated factor XIII: determination of a cross-linking pattern that maximizes clot stiffness. Blood. 2007;110:902–7. doi: 10.1182/blood-2007-01-066837. [DOI] [PubMed] [Google Scholar]
- 51.Helms CC, Ariëns RA, Uitte de Willige S, Standeven KF, Guthold M. Alpha-alpha cross-links increase fibrin fiber elasticity and stiffness. Biophys J. 2012;102:168–75. doi: 10.1016/j.bpj.2011.11.4016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Duval C, Allan P, Connell SD, Ridger VC, Philippou H, Ariëns RA. Roles of fibrin alpha- and gamma-chain specific cross-linking by FXIIIa in fibrin structure and function. Thromb Haemost. 2014;111:842–50. doi: 10.1160/TH13-10-0855. [DOI] [PubMed] [Google Scholar]
- 53.Bereczky Z, Muszbek L. Factor XIII and venous thromboembolism. Semin Thromb Hemost. 2011;37:305–14. doi: 10.1055/s-0031-1273094. [DOI] [PubMed] [Google Scholar]
- 54.Wartiovaara U, Mikkola H, Szoke G, Haramura G, Karpati L, Balogh I, Lassila R, Muszbek L, Palotie A. Effect of Val34Leu polymorphism on the activation of the coagulation factor XIII-A. Thromb Haemost. 2000;84:595–600. [PubMed] [Google Scholar]
- 55.Balogh I, Szoke G, Karpati L, Wartiovaara U, Katona E, Komaromi I, Haramura G, Pfliegler G, Mikkola H, Muszbek L. Val34Leu polymorphism of plasma factor XIII: biochemistry and epidemiology in familial thrombophilia. Blood. 2000;96:2479–86. [PubMed] [Google Scholar]
- 56.Ariëns RA, Philippou H, Nagaswami C, Weisel JW, Lane DA, Grant PJ. The factor XIII V34L polymorphism accelerates thrombin activation of factor XIII and affects cross-linked fibrin structure. Blood. 2000;96:988–95. [PubMed] [Google Scholar]
- 57.Lim BC, Ariëns RA, Carter AM, Weisel JW, Grant PJ. Genetic regulation of fibrin structure and function: complex gene–environment interactions may modulate vascular risk. Lancet. 2003;361:1424–31. doi: 10.1016/S0140-6736(03)13135-2. [DOI] [PubMed] [Google Scholar]
- 58.Ho CH. The hemostatic effect of packed red cell transfusion in patients with anemia. Transfusion. 1998;38:1011–4. doi: 10.1046/j.1537-2995.1998.38111299056308.x. [DOI] [PubMed] [Google Scholar]
- 59.Dicato M. Venous thromboembolic events and erythropoiesisstimulating agents: an update. Oncologist. 2008;13(Suppl 3):11–5. doi: 10.1634/theoncologist.13-S3-11. [DOI] [PubMed] [Google Scholar]
- 60.Braekkan SK, Mathiesen EB, Njolstad I, Wilsgaard T, Hansen JB. Hematocrit and risk of venous thromboembolism in a general population. The Tromso study. Haematologica. 2010;95:270–5. doi: 10.3324/haematol.2009.008417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Eischer L, Tscholl V, Heinze G, Traby L, Kyrle PA, Eichinger S. Hematocrit and the risk of recurrent venous thrombosis: a prospective cohort study. PLoS ONE. 2012;7:e38705. doi: 10.1371/journal.pone.0038705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Marchioli R, Finazzi G, Specchia G, Cacciola R, Cavazzina R, Cilloni D, De Stefano V, Elli E, Iurlo A, Latagliata R, Lunghi F, Lunghi M, Marfisi RM, Musto P, Masciulli A, Musolino C, Cascavilla N, Quarta G, Randi ML, Rapezzi D, et al. Cardiovascular events and intensity of treatment in polycythemia vera. N Engl J Med. 2013;368:22–33. doi: 10.1056/NEJMoa1208500. [DOI] [PubMed] [Google Scholar]
- 63.Austin H, Key NS, Benson JM, Lally C, Dowling NF, Whitsett C, Hooper WC. Sickle cell trait and the risk of venous thromboembolism among blacks. Blood. 2007;110:908–12. doi: 10.1182/blood-2006-11-057604. [DOI] [PubMed] [Google Scholar]
- 64.Atici AG, Kayhan S, Aydin D, Yilmaz YA. Plasma viscosity levels in pulmonary thromboembolism. Clin Hemorheol Microcirc. 2013;55:313–20. doi: 10.3233/CH-2012-1637. [DOI] [PubMed] [Google Scholar]
- 65.Ben-Ami R, Barshtein G, Mardi T, Deutch V, Elkayam O, Yedgar S, Berliner S. A synergistic effect of albumin and fibrinogen on immunoglobulin-induced red blood cell aggregation. Am J Physiol Heart Circ Physiol. 2003;285:H2663–9. doi: 10.1152/ajpheart.00128.2003. [DOI] [PubMed] [Google Scholar]
- 66.Carvalho FA, Connell S, Miltenberger-Miltenyi G, Pereira SV, Tavares A, Ariëns RA, Santos NC. Atomic force microscopy-based molecular recognition of a fibrinogen receptor on human erythrocytes. ACS Nano. 2010;4:4609–20. doi: 10.1021/nn1009648. [DOI] [PubMed] [Google Scholar]
- 67.De Oliveira S, Vitorino de Almeida V, Calado A, Rosario HS, Saldanha C. Integrin-associated protein (CD47) is a putative mediator for soluble fibrinogen interaction with human red blood cells membrane. Biochim Biophys Acta. 2012;1818:481–90. doi: 10.1016/j.bbamem.2011.10.028. [DOI] [PubMed] [Google Scholar]
- 68.Hermand P, Huet M, Callebaut I, Gane P, Ihanus E, Gahmberg CG, Cartron JP, Bailly P. Binding sites of leukocyte beta 2 integrins (LFA-1, Mac-1) on the human ICAM-4/LW blood group protein. J Biol Chem. 2000;275:26002–10. doi: 10.1074/jbc.M002823200. [DOI] [PubMed] [Google Scholar]
- 69.Ihanus E, Uotila L, Toivanen A, Stefanidakis M, Bailly P, Cartron JP, Gahmberg CG. Characterization of ICAM-4 binding to the I domains of the CD11a/CD18 and CD11b/CD18 leukocyte integrins. Eur J Biochem. 2003;270:1710–23. doi: 10.1046/j.1432-1033.2003.03528.x. [DOI] [PubMed] [Google Scholar]
- 70.Hermand P, Gane P, Huet M, Jallu V, Kaplan C, Sonneborn HH, Cartron JP, Bailly P. Red cell ICAM-4 is a novel ligand for platelet-activated alphaIIbbeta3 integrin. J Biol Chem. 2003;278:4892–8. doi: 10.1074/jbc.M211282200. [DOI] [PubMed] [Google Scholar]
- 71.Spring FA, Parsons SF, Ortlepp S, Olsson ML, Sessions R, Brady RL, Anstee DJ. Intercellular adhesion molecule-4 binds alpha(4)beta(1) and alpha(V)-family integrins through novel integrin- binding mechanisms. Blood. 2001;98:458–66. doi: 10.1182/blood.v98.2.458. [DOI] [PubMed] [Google Scholar]
- 72.Barr JD, Chauhan AK, Schaeffer GV, Hansen JK, Motto DG. Red blood cells mediate the onset of thrombosis in the ferric chloride murine model. Blood. 2013;121:3733–41. doi: 10.1182/blood-2012-11-468983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.An X, Schulz VP, Li J, Wu K, Liu J, Xue F, Hu J, Mohandas N, Gallagher PG. Global transcriptome analyses of human and murine terminal erythroid differentiation. Blood. 2014;123:3466–77. doi: 10.1182/blood-2014-01-548305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Setty BN, Rao AK, Stuart MJ. Thrombophilia in sickle cell disease: the red cell connection. Blood. 2001;98:3228–33. doi: 10.1182/blood.v98.12.3228. [DOI] [PubMed] [Google Scholar]
- 75.Peyrou V, Lormeau JC, Herault JP, Gaich C, Pfliegger AM, Herbert JM. Contribution of erythrocytes to thrombin generation in whole blood. Thromb Haemost. 1999;81:400–6. [PubMed] [Google Scholar]
- 76.Horne MK, 3rd, Cullinane AM, Merryman PK, Hoddeson EK. The effect of red blood cells on thrombin generation. Br J Haematol. 2006;133:403–8. doi: 10.1111/j.1365-2141.2006.06047.x. [DOI] [PubMed] [Google Scholar]
- 77.Whelihan MF, Zachary V, Orfeo T, Mann KG. Prothrombin activation in blood coagulation: the erythrocyte contribution to thrombin generation. Blood. 2012;120:3837–45. doi: 10.1182/blood-2012-05-427856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.van der Meijden PE, van Schilfgaarde M, van Oerle R, Renne T, ten Cate H, Spronk HM. Platelet- and erythrocyte-derived microparticles trigger thrombin generation via factor XIIa. J Thromb Haemost. 2012;10:1355–62. doi: 10.1111/j.1538-7836.2012.04758.x. [DOI] [PubMed] [Google Scholar]
- 79.Jy W, Johansen ME, Bidot C, Jr, Horstman LL, Ahn YS. Red cell-derived microparticles (RMP) as haemostatic agent. Thromb Haemost. 2013;110:751–60. doi: 10.1160/TH12-12-0941. [DOI] [PubMed] [Google Scholar]
- 80.Zecher D, Cumpelik A, Schifferli JA. Erythrocyte-derived micro-vesicles amplify systemic inflammation by thrombin-dependent activation of complement. Arterioscler Thromb Vasc Biol. 2014;34:313–20. doi: 10.1161/ATVBAHA.113.302378. [DOI] [PubMed] [Google Scholar]
- 81.Gersh KC, Nagaswami C, Weisel JW. Fibrin network structure and clot mechanical properties are altered by incorporation of erythrocytes. Thromb Haemost. 2009;102:1169–75. doi: 10.1160/TH09-03-0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wohner N, Sotonyi P, Machovich R, Szabo L, Tenekedjiev K, Silva MM, Longstaff C, Kolev K. Lytic resistance of fibrin containing red blood cells. Arterioscler Thromb Vasc Biol. 2011;31:2306–13. doi: 10.1161/ATVBAHA.111.229088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.van Gelder JM, Nair CH, Dhall DP. Erythrocyte aggregation and erythrocyte deformability modify the permeability of erythrocyte enriched fibrin network. Thromb Res. 1996;82:33–42. doi: 10.1016/0049-3848(96)00048-5. [DOI] [PubMed] [Google Scholar]
- 84.Liang XM, Han SJ, Reems JA, Gao D, Sniadecki NJ. Platelet retraction force measurements using flexible post force sensors. Lab Chip. 2010;10:991–8. doi: 10.1039/b918719g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wufsus AR, Rana K, Brown A, Dorgan JR, Liberatore MW, Neeves KB. Elastic behavior and platelet retraction in low- and high-density fibrin gels. Biophys J. 2015;108:173–83. doi: 10.1016/j.bpj.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sutton JT, Ivancevich NM, Perrin SR, Jr, Vela DC, Holland CK. Clot retraction affects the extent of ultrasound-enhanced thrombolysis in an ex vivo porcine thrombosis model. Ultrasound Med Biol. 2013;39:813–24. doi: 10.1016/j.ultrasmedbio.2012.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]