Abstract
Although there is good evidence that sedentary behavior are associated with poor health outcomes in healthy persons and patients with cardiovascular disease, the mental health consequences of sedentary behavior have not been widely studied. In this report, we conducted a cross-sectional analysis to examine the relationship of self-reported sedentary behavior and depression in a sample of 4043 hospitalized men and women with acute coronary syndrome (ACS) enrolled in a randomized clinical trial in rural China. Sedentary behavior was assessed by self-report, while depression was assessed with the Patient Health Questionnaire-9 (PHQ-9); a subset of 1209 patients also completed the Beck Depression Inventory-II (BDI-II). Results revealed that greater sedentary behavior was associated with higher levels of depressive symptoms measured by both the PHQ-9 (P<0.001) and BDI-II (P<0.001). Compared with patients who reported that they were seldom sedentary, patients reporting that they were frequently sedentary were 4.7 times (OR 4.73, 95% CI: 2.71–8.24) more likely to be clinically depressed defined as PHQ-9 scores ≥ 10 after adjusting for demographic factors, lifestyle behaviors, clinical characteristics and in-hospital treatments. In conclusion, greater sedentary behavior is significantly related to greater depression in Chinese patients with ACS, independent of physical activity. These findings suggest that strategies to reduce sedentary behavior may improve medical outcomes and reduce risk for depression.
Keywords: Depression, Acute Coronary Syndrome, Sedentary behavior
Introduction
Physical inactivity, or lack of regular exercise, is associated with increased risk of cardiovascular disease morbidity and mortality1–3, as well as diabetes4, obesity5, hypertension6 and even certain cancers7,8. Recently, the importance of sedentary behavior, as distinct from physical inactivity, has gained increased attention. Sedentary behavior has been defined as activities that do not increase energy expenditure above the resting level (i.e., <1.5 metabolic equivalents) and includes time spent in such activities as sitting and lying down during waking hours, working on a computer, watching TV, and engaging in other forms of screen-based entertainment9. A number of observational studies have shown that excessive time spent in sedentary behaviors is associated with increased risk for adverse health outcomes independent of moderate physical activity10,11. Although the importance of sedentary behavior on physical health outcomes is recognized 12, the mental health consequences of sedentary behavior have not been widely studied. A recent meta-analysis13 found that sedentary behaviors increased the risk of depression by 25% in the general population. To our knowledge, however, no study has yet examined the relationship between sedentary behavior and depression in patients with acute coronary syndrome. Therefore, the purpose of the present study was to examine the relationship between sedentary behavior and depression in a large cohort of post-ACS patients from rural China.
Methods
Four thousand and forty three hospitalized ACS patients who were enrolled in the Integrating Depression Care in Acute Coronary Syndromes Patients (I-CARE) study (Trial registration on clinicaltrials.gov NCT02195193) served as participants for this study. I-CARE is an ongoing randomized clinical trial designed to evaluate the clinical effectiveness and cost-effectiveness of depression-integrated care to patients from rural China with ACS. This study was conducted in 16 rural hospitals around China. The first patient was enrolled on November, 2014 and the last patient was randomized on January 2017. Patients with severe cardiovascular disease (e.g., class III heart failure), medical comorbidity (e.g., cancer with life expectancy < 1 year) or disabled, acute psychosis (e.g., bipolar disorder, schizophrenia, psychotic depression, or high-risk of suicide), women who were pregnant or breast-feeding, or individuals who had cognitive impairment and were unable to provide informed consent were excluded. This study was approved by the Institutional Review Board of Peking University, and written informed consent was obtained from all participants.
During the index hospitalization, we assessed self-reported sedentary behavior prior to admission using a single item, written in Chinese, and translated as: “During the past 3 months, how often do you spend in sedentary behavior (sitting, lying on bed, watching TV, playing Mahjong, games, cards, etc.) in your typical day.” Responses were scored on a 3-point rating scale, as frequently, occasionally and seldom.
Depression was assessed with the Patient Health Questionnaire (PHQ-9)14. The PHQ-9 scale is a 9-item, self-report instrument, translated into Chinese, that is designed to map onto the depression diagnostic criteria in Diagnostic and Statistical Manual of Mental Disorders Fifth Edition. Each item ranges from 0 (not at all) to 3 (nearly every day); scores range from 0 to 27, with higher scores reflecting greater depression symptoms. Scores ≥10 are clinically significant and indicate moderate to severe depressive symptoms. Items were read by a trained research assistant to any patient unable to read.
To confirm the relation of depression and sedentary behavior, 1209 patients from 4 select rural hospitals also completed the Beck Depression Inventory-II (BDI-II) scale15. The BDI-II is a 21-item measure of depressive symptoms in which symptoms were rated on a 4-point rating scale, with scores ranging from 0 to 63. A score of ≥14 is considered clinically significant.
Demographic and lifestyle behaviors such as smoking, alcohol consumption and physical activity were obtained from self-report questionnaire. Social support was quantified from the 5-item, ENRICHD Social Support Instrument16. Clinical characteristics as well as in-hospital adverse events (e.g., myocardial infarction or re- myocardial infarction, severe arrhythmias and congestive heart failure) were documented from hospital medical records.
Differences between patients with different levels of reported sedentary behaviors were compared using general linear models and Chi-square tests. To examine the relationship between sedentary behavior and depression, general linear model was used to compare PHQ-9 scores among patients who reported sedentary behavior frequently, occasionally and seldom. Logistic regression models also were used to assess the relationship between clinical depression defined by PHQ-9 scores >10 and sedentary behavior. We pre-specified a set of potential confounders, which were adjusted in three steps: Model 1 adjusted for age and sex. Model 2 also adjusted for education level, marital status, health insurance, social support score, body mass index (BMI), smoking status, currently alcohol use, physical activity, history of depression, history of hypertension, history of diabetes, prior myocardial infarction, type of ACS, left ventricular (LV) ejection fraction (EF), in-hospital adverse events, treatment of thrombolysis, and percutaneous coronary intervention. In Model 3, we conducted a propensity score-weighted logistic regression based on all confounders in model 2 to minimize the potential bias caused by residual confounding. All propensity score weighted confounders were well-balanced between groups. Two-way interaction terms between sedentary behavior and each of the 19 confounders were calculated to determine if the relationship between sedentary behavior and depression was affected by any confounders. In addition, sensitivity analyses were performed in a subset of patients from 4 rural hospitals who also completed the BDI-II. A two-sided p value <0.05 was considered statistically significant. Analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, North Carolina).
Results
Of the 4043 ACS patients, 363 (9.0%) were classified as frequently sedentary, 1250 (30.9%) occasionally sedentary and 2430 (60.1%) seldom sedentary. The mean PHQ-9 score was 3.6±3.0 and 135 (3.3%) patients were classified as depressed based upon a cutoff of ≥10 on the PHQ-9. In the subset of patients who also completed the BDI-II, the mean score was 6.17±6.56 and 13.4% of participants obtained scores ≥14. Patients who reported frequent sedentary behavior were older, more likely to be less educated and single, and less likely to be male, report lower social support, have more in-hospital adverse events, receive less thrombolysis therapy, and undergo more percutaneous coronary intervention interventions (Table 1).
Table 1.
Characteristics of Participants with Acute Coronary Syndromes by Level of Sedentary Behavior
| Characteristics | Total (n=4043) | Sedentary behavior
|
P-value | ||
|---|---|---|---|---|---|
| Frequently (n=363) | Occasionally (n=1250) | Seldom (n=2430) | |||
| Age (years) | 61.1 ± 9.6 | 61.7 ± 10.3 | 61.8 ± 9.6 | 60.7 ± 9.5 | 0.004 |
| Men | 2556 (63.2%) | 216 (59.5%) | 788 (63.0%) | 1552 (63.9%) | 0.271 |
| Education | |||||
| None | 733 (18.1%) | 66 (18.2%) | 244 (19.5%) | 423 (17.4%) | <0.001 |
| Primary school | 1106 (27.4%) | 90 (24.8%) | 293 (23.4%) | 723 (29.8%) | |
| High school | 1974 (48.8%) | 183 (50.4%) | 617 (49.4%) | 1174 (48.3%) | |
| College and above | 230 (5.7%) | 24 (6.6%) | 96 (7.7%) | 110 (4.5%) | |
| Married/Partnered | 3564 (88.2%) | 310 (85.4%) | 1092 (87.4%) | 2162 (89.0%) | 0.078 |
| Health insurance | 3953 (97.8%) | 356 (98.1%) | 1220 (97.6%) | 2377 (97.8%) | 0.842 |
| Body Mass Index (kg/m2) | 24.6 ± 3.4 | 25.1 ± 3.6 | 24.9 ± 3.4 | 24.4 ± 3.3 | <0.001 |
| Social support score | 21.3 ± 3.4 | 21.6 ± 3.8 | 21.4 ± 3.2 | 21.3 ± 3.4 | 0.106 |
| Smoking status | |||||
| Never | 1791 (44.3%) | 158 (43.5%) | 562 (45.0%) | 1071 (44.1%) | 0.159 |
| Former | 1111 (27.5%) | 85 (23.4%) | 353 (28.2%) | 6733 (27.7%) | |
| Current | 1139 (28.2%) | 120 (33.1%) | 335 (26.8%) | 684 (28.2%) | |
| Current alcohol use | 1143 (28.3%) | 101 (27.8%) | 347 (27.8%) | 695 (28.6%) | 0.849 |
| Physical activity | |||||
| Seldom | 2081 (51.5%) | 264 (72.7%) | 662 (53.0%) | 1155 (47.5%) | <0.001 |
| Occasionally | 675 (16.7%) | 38 (10.5%) | 262 (21.0%) | 375 (15.4%) | |
| Frequently | 1287 (31.8%) | 61 (16.8%) | 326 (26.0%) | 900 (37.0%) | |
| History of depression | 42 (1.1%) | 7 (2.0%) | 10 (0.8%) | 25 (1.0%) | 0.166 |
| History of hypertension | 2230 (55.2%) | 214 (59.0%) | 725 (58.0%) | 1291 (53.1%) | 0.002 |
| History of diabetes | 745 (18.4%) | 91 (25.1%) | 277 (22.2%) | 377 (15.5%) | <0.001 |
| Prior MI | |||||
| Yes | 418 (10.3%) | 49 (13.5%) | 129 (10.3%) | 240 (9.9%) | <0.001 |
| No | 2171 (53.7%) | 187 (51.5%) | 745 (59.6%) | 1239 (51.0%) | |
| Unknown | 1454 (36.0%) | 127 (35.0%) | 376 (30.1%) | 951 (60.1%) | |
| Type of ACS | |||||
| STEMI | 1128 (27.9%) | 88 (24.2%) | 336 (26.9%) | 704 (29.0%) | 0.026 |
| NSTEMI | 605 (15.0%) | 73 (20.1%) | 181 (14.5%) | 351 (14.4%) | |
| UAP | 2310 (57.1%) | 202 (55.7%) | 733 (58.6%) | 1375 (56.6%) | |
| LVEF (%) | |||||
| <50 | 445 (11.0%) | 66 (18.2%) | 125 (10.0%) | 254 (10.5%) | <0.001 |
| ≥50 | 2414 (59.7%) | 204 (56.2%) | 759 (60.7%) | 1451 (59.7%) | |
| Unchecked | 1184 (29.3%) | 93 (25.6%) | 366 (29.3%) | 725 (29.8%) | |
| In-hospital adverse event | 165 (4.1%) | 25 (6.9%) | 58 (4.6%) | 82 (3.4%) | 0.003 |
| Thrombolysis | 542 (13.4%) | 28 (7.7%) | 174 (13.9%) | 340 (14.0%) | 0.004 |
| Percutaneous coronary intervention | 268 (6.6%) | 41 (11.3%) | 107 (8.6%) | 120 (4.9%) | <0.001 |
Note: Data presented as N (%) or mean ± SD
STEMI=ST-elevation myocardial infarction; NSTEMI=Non-ST-elevation myocardial infarction; UAP=Unstable angina pectoris; LV=Left ventricular; EF=Ejection fraction
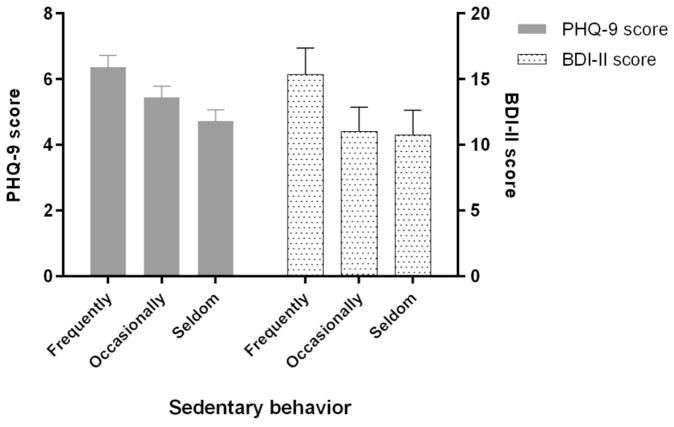
Results of the general linear model analyses, adjusting for pre-specified confounders, revealed that higher PHQ-9 scores were associated greater sedentary behavior (P for trend < 0.001) (Figure 1). When patients were classified based upon the presence of clinical depression on the PHQ-9, logistic regression models revealed a significant increased risk of depression associated with higher sedentary behavior (Table 2). In the unadjusted model, patients reporting frequent sedentary behavior were 3.41 times more likely to be classified as depressed compared to those patients who were seldom sedentary (OR 3.41, 95%CI: 2.20–5.28). This relationship remained significant after adjusted age and sex (model 1: OR 3.56, 95%CI: 2.28–5.55) and even stronger when all the other pre-specified confounders were adjusted (model 2: OR 4.73, 95%CI: 2.71–8.24). Propensity score-weighted model (model 3: OR 4.92, 95%CI: 2.89–8.36) revealed the same results. The risk of depression increased as the degree of sedentary behavior increased (p for trend <0.001). No interaction was found between sedentary behavior and any of the pre-specified confounders. Because some patients were either missing LVEF values or there was uncertainty about an MI history, we removed those patients from the analyses and results were unchanged.
Figure 1. Relation of Depression Symptoms and Sedentary Behavior.
Frequent sedentary behavior is associated with greater depressive symptoms assessed by the PHQ-9 (left panel) (P for trend < 0.001) and BDI-II (P for trend < 0.001) in post-ACS Chinese inpatients. Values represent adjusted mean score (with standard error).
Table 2.
Likelihood of Depression Assessed by Patient Health Questionnaire-9 among Patients with Acute Coronary Syndrome with Varying Levels of Sedentary Behavior
| Variable | N (%) | Crude OR | ORmodel1 | ORmodel2 | ORmodel3 |
|---|---|---|---|---|---|
| Sedentary behavior | |||||
| Frequently | 363 (9.0%) | 3.41 | 3.56 | 4.73 | 4.92 |
| (2.20–5.28) | (2.28–5.55) | (2.71–8.24) | (2.89–8.36) | ||
| Occasionally | 1250 (30.9%) | 1.05 | 1.09 | 1.29 | 1.33 |
| (0.69–1.58) | (0.72–1.65) | (0.77–2.15) | (0.81–2.17) | ||
| Seldom | 2430 (60.1%) | 1 | 1 | 1 | 1 |
| Ptrend<0.001 | Ptrend<0.001 | Ptrend<0.001 | Ptrend<0.001 | ||
Note: Model 1 adjusted for age and sex; model 2 further adjusted education level, marital status, health insurance, social support score, body mass index, smoking status, currently alcohol use, physical activity, history of depression, history of hypertension, history of diabetes, prior myocardial infarction, type of acute coronary syndrome, left ventricular ejection fraction, in-hospital adverse events, treatment of thrombolysis, and percutaneous coronary intervention; model 3 adjusted above confounders using propensity score weights.
To confirm the association of depression and sedentary behavior, we performed a sensitivity analysis in a subset of 1209 patients who also completed the BDI-II as a measure of depression. Patients who reported frequent sedentary behavior obtained higher BDI-II scores compared to their less sedentary counterparts (Figure 1) and patients who endorsed frequent sedentary behavior were than three times more likely to be depressed (i.e., BDI-II scores ≥14) compared to those patients who reported that they were seldom sedentary (OR 3.51, 95%CI: 1.62–7.65).
Discussion
In this study of more than 4000 patients with acute coronary syndrome, sedentary behavior was associated with greater depression measured by two widely used and well-validated psychometric instruments. Patients reporting greater sedentary behavior had higher PHQ-9 scores, and a subset of patients who also completed the BDI-II, also had higher depression scores compared to their non-sedentary counterparts. After adjustment for pre-specified confounders, patients reporting frequent sedentary behavior had 4.7 times greater risk of clinical depression using a cutoff of ≥10 on the PHQ-9 or 3.5 times greater risk using a cutoff of ≥14 on the BDI-II relative to those who reported being seldom sedentary.
These findings are consistent with results from previous studies of healthy adults which reported that inactive individuals were more likely to be clinically depressed or to report greater depressive symptoms17–19. Furthermore, while studies have reported that inactive patients with cardiovascular disease are more likely to be depressed, to our knowledge, this is the first study to report that sedentary behavior also was associated with depression in a large sample of hospitalized ACS patients.
Previously sedentary behavior has been shown to be associated with mental illness17 and a recent meta-analysis13 of 24 observational studies found that long-time TV viewing was associated with a 13% increase in depressive symptoms and prolonged computer or internet use was associated with a 22% increase in risk of depression in adolescents, university students, and older adults. The present findings suggest that the association between sedentary behavior and depression is even stronger in ACS patients. Furthermore, the relationship between sedentary behavior and depression was unchanged when physical activity was included in the model, suggesting that the significant relationship between sedentary behavior and depression is independent of physical activity.
The mental health implications of sedentary behavior are even more salient since sedentary behaviors have become increasingly common. In the United States, adults spend more than 50% of their time in sedentary behavior20 and a study21 among Chinese adults using accelerometry to objectively measure physical activity reported that over 500 minutes per day were spent being sedentary. It will be important to develop strategies not only to increase physical activity in post-ACS patients, but also to reduce time spent in sedentary behaviors.
Our study has several important limitations. Because this was a cross-sectional study, we are not able to draw any causal inferences between sedentary behavior and depression. It cannot be determined if greater depression resulted in more sedentary behavior or sedentary behavior caused worsening symptoms of depression. Future longitudinal analyses may help to clarify the temporal relation between these factors. Second, our sample consisted of post-ACS patients from rural hospitals in China and our results may not generalize to Western countries or to more urban environments. Finally, we used a single, self-report item to assess sedentary behavior. Although single-item, self-report measures of exercise behavior have been shown to be valid22 and have been used previously23,24, more objective measures of physical activity and sedentary behaviors, including the use of accelerometry, would be more desirable. We also note that our study has a number of strengths, including a large, well-characterized sample of ACS patients from rural China, quantified measurement of depressive symptoms derived from well-validated instruments, and statistical adjustment incorporating a wide range of potential confounders.
Our observation that patients who reported frequent sedentary behavior reported greater depressive symptoms compared to their less sedentary counterparts suggests the potential value of developing strategies to reduce sedentary behavior in post-ACS patients to improve depression.
Acknowledgments
This study is supported by a grant from the National Institute of Mental Health (R01MH100332).
Footnotes
Disclosure Statement
No conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cheng X, Li W, Guo J, Wang Y, Gu H, Teo K, Liu L, Yusuf S. Physical activity levels, sport activities, and risk of acute myocardial infarction: results of the INTERHEART study in China. Angiology. 2014;65:113–121. doi: 10.1177/0003319712470559. [DOI] [PubMed] [Google Scholar]
- 2.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 3.Soares-Miranda L, Siscovick DS, Psaty BM, Longstreth WT, Jr, Mozaffarian D. Physical Activity and Risk of Coronary Heart Disease and Stroke in Older Adults: The Cardiovascular Health Study. Circulation. 2016;133:147–155. doi: 10.1161/CIRCULATIONAHA.115.018323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care. 2007;30:744–752. doi: 10.2337/dc06-1842. [DOI] [PubMed] [Google Scholar]
- 5.Wadden TA, Webb VL, Moran CH, Bailer BA. Lifestyle modification for obesity: new developments in diet, physical activity, and behavior therapy. Circulation. 2012;125:1157–1170. doi: 10.1161/CIRCULATIONAHA.111.039453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu X, Zhang D, Liu Y, Sun X, Han C, Wang B, Ren Y, Zhou J, Zhao Y, Shi Y, Hu D, Zhang M. Dose-Response Association Between Physical Activity and Incident Hypertension: A Systematic Review and Meta-Analysis of Cohort Studies. Hypertension. 2017;69:813–820. doi: 10.1161/HYPERTENSIONAHA.116.08994. [DOI] [PubMed] [Google Scholar]
- 7.Lee IM. Physical activity and cancer prevention--data from epidemiologic studies. Med Sci Sports Exerc. 2003;35:1823–1827. doi: 10.1249/01.MSS.0000093620.27893.23. [DOI] [PubMed] [Google Scholar]
- 8.McTiernan A, Kooperberg C, White E, Wilcox S, Coates R, Adams-Campbell LL, Woods N, Ockene J. Recreational physical activity and the risk of breast cancer in postmenopausal women: the Women’s Health Initiative Cohort Study. Jama. 2003;290:1331–1336. doi: 10.1001/jama.290.10.1331. [DOI] [PubMed] [Google Scholar]
- 9.Mansoubi M, Pearson N, Clemes SA, Biddle SJ, Bodicoat DH, Tolfrey K, Edwardson CL, Yates T. Energy expenditure during common sitting and standing tasks: examining the 1. 5 MET definition of sedentary behaviour. BMC Public Health. 2015;15:516. doi: 10.1186/s12889-015-1851-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am J Prev Med. 2011;41:207–215. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 11.de Rezende LF, Rodrigues Lopes M, Rey-Lopez JP, Matsudo VK, Luiz Odo C. Sedentary behavior and health outcomes: an overview of systematic reviews. PLoS One. 2014;9:e105620. doi: 10.1371/journal.pone.0105620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young DR, Hivert MF, Alhassan S, Camhi SM, Ferguson JF, Katzmarzyk PT, Lewis CE, Owen N, Perry CK, Siddique J, Yong CM. Sedentary Behavior and Cardiovascular Morbidity and Mortality: A Science Advisory From the American Heart Association. Circulation. 2016;134:e262–279. doi: 10.1161/CIR.0000000000000440. [DOI] [PubMed] [Google Scholar]
- 13.Zhai L, Zhang Y, Zhang D. Sedentary behaviour and the risk of depression: a meta-analysis. Br J Sports Med. 2015;49:705–709. doi: 10.1136/bjsports-2014-093613. [DOI] [PubMed] [Google Scholar]
- 14.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 16.Enhancing recovery in coronary heart disease patients (ENRICHD): study design and methods. The ENRICHD investigators. Am Heart J. 2000;139:1–9. doi: 10.1016/s0002-8703(00)90301-6. [DOI] [PubMed] [Google Scholar]
- 17.Sanchez-Villegas A, Ara I, Guillen-Grima F, Bes-Rastrollo M, Varo-Cenarruzabeitia JJ, Martinez-Gonzalez MA. Physical activity, sedentary index, and mental disorders in the SUN cohort study. Med Sci Sports Exerc. 2008;40:827–834. doi: 10.1249/MSS.0b013e31816348b9. [DOI] [PubMed] [Google Scholar]
- 18.Thomee S, Harenstam A, Hagberg M. Computer use and stress, sleep disturbances, and symptoms of depression among young adults--a prospective cohort study. BMC Psychiatry. 2012;12:176. doi: 10.1186/1471-244X-12-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamer M, Stamatakis E. Prospective study of sedentary behavior, risk of depression, and cognitive impairment. Med Sci Sports Exerc. 2014;46:718–723. doi: 10.1249/MSS.0000000000000156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peters TM, Moore SC, Xiang YB, Yang G, Shu XO, Ekelund U, Ji BT, Tan YT, Liu DK, Schatzkin A, Zheng W, Chow WH, Matthews CE, Leitzmann MF. Accelerometer-measured physical activity in Chinese adults. Am J Prev Med. 2010;38:583–591. doi: 10.1016/j.amepre.2010.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.U. S. DEPARTMENT OF HEALTH AND HIUMAN SERVICES. Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. pp. 29–37. [Google Scholar]
- 23.Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, Ali S, Dowray S, Na B, Feldman MD, Schiller NB, Browner WS. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. Jama. 2008;300:2379–2388. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blumenthal JA, Babyak MA, Carney RM, Huber M, Saab PG, Burg MM, Sheps D, Powell L, Taylor CB, Kaufmann PG. Exercise, depression, and mortality after myocardial infarction in the ENRICHD trial. Med Sci Sports Exerc. 2004;36:746–755. doi: 10.1249/01.mss.0000125997.63493.13. [DOI] [PubMed] [Google Scholar]