Abstract
Background
Transportation to primary care is a well-documented barrier for patients with Medicaid, despite access to non-emergency medical transportation (NEMT) benefits. Rideshare services, which offer greater convenience and lower cost, have been proposed as an NEMT alternative.
Objective
To evaluate the impact of rideshare-based medical transportation on the proportion of Medicaid patients attending scheduled primary care appointments.
Design
In one of two similar practices, all eligible Medicaid patients were offered rideshare-based transportation (“rideshare practice”). A difference-in-difference analytical approach using logistic regression with robust standard errors was employed to compare show rate changes between the rideshare practice and the practice where rideshare was not offered (“control practice”).
Participants
Our study population included residents of West Philadelphia who were insured by Medicaid and were established patients at two academic general internal medicine practices located in the same building.
Intervention
We designed a rideshare-based transportation pilot intervention. Patients were offered the service during their reminder call 2 days before the appointment, and rides were prescheduled by research staff. Patients then called research staff to schedule their return trip home.
Main Measures
We assessed the effect of offering rideshare-based transportation on appointment show rates by comparing the change in the average show rate for the rideshare practice, from the baseline period to the intervention period, with the change at the control practice.
Key Results
At the control practice, the show rate declined from 60% (146/245) to 51% (34/67). At the rideshare practice, the show rate improved from 54% (72/134) to 68% (41/60). In the adjusted model, controlling for patient demographics and provider type, the odds of showing up for an appointment before and after the intervention increased 2.57 (1.10–6.00) times more in the rideshare practice than in the control practice.
Conclusions
Results of this pilot program suggest that offering a rideshare-based transportation service can increase show rates to primary care for Medicaid patients.
KEY WORDS: access to care, socioeconomic factors, Medicaid, underserved populations, primary care
INTRODUCTION
Low-income patients frequently face transportation barriers in accessing primary care. In several large surveys, 24–51% reported missing or rescheduling an outpatient appointment because of lack of access to transportation.1,2 Barriers include costs (e.g., affordability of transport), physical factors (e.g., requiring a wheelchair-accessible vehicle or mobility assistance getting from their room to the vehicle), availability (e.g., car ownership or living near transit stops), and reliability (e.g., timeliness of pick-ups and drop-offs).2,3 Patients who face transportation barriers tend to shift their care toward more costly, acute care settings for low-acuity needs, for reasons of preference and convenience.2,4–9 For providers, missed appointments have a negative effect on clinical productivity, with disjointed care or missed treatment opportunities.2,4,5,10 Unused clinical space and staff time equate to lost revenue.
Non-emergency medical transportation (NEMT) is a benefit available for Medicaid beneficiaries to help overcome transportation barriers. Despite the availability of this service, however, transportation barriers remain substantial for Medicaid patients for a number of reasons.3,11,12 First, patients may not be aware of how to access the service. Enrollment often requires social work intervention and the completion of forms to designate eligibility. Second, states place various restrictions on the service, including the number of rides, types of rides (public transit, taxis, or shared vans, depending on availability), and ride distance.12 These limits create wide variability in NEMT implementation nationally, and the degree to which these act as barriers may be site-specific.13 Third, the design of NEMT services may be a factor—the services have been criticized because they require advanced scheduling (often days in advance), long transportation times due to indirect travel routes to appointments with van shares or car pools, and long wait times for vehicle pick-ups.3
Rideshare services provided by companies such as Uber and Lyft have been proposed as NEMT alternatives, as they may be more convenient and lower-cost than shared vans or taxi services, key transportation modes within the NEMT benefit.14,15 Therefore, as part of a pilot, we designed a rideshare-based transportation intervention for Medicaid patients to test its effectiveness in improving primary care show rates and to determine the costs of operating this service.
METHODS
Design
We used a difference-in-difference approach to compare changes in show rates at two similar primary care practices. At the rideshare practice, all eligible Medicaid patients were offered rideshare-based transportation. At the control practice, all eligible Medicaid patients received usual care. This study was approved by the institutional review board of the University of Pennsylvania.
Participants and Procedures
Patients eligible for study inclusion were a) adults (≥ 18 years old), b) insured by Medicaid, c) established primary care patients (i.e., scheduled for a return visit instead of a new patient visit) at two academic general internal medicine outpatient practices (both affiliated with Penn Medicine and located in the same building), d) not scheduled for an urgent care visit, e) residing within the six West Philadelphia ZIP Codes, and f) scheduled to see a physician or nurse practitioner (e.g., not a blood pressure check by a registered nurse or follow-up immunization injection). Patients were prescreened for inclusion using data from the electronic medical record. We subsequently used an intention-to-treat approach: all patients contacted by our study staff were included in the analysis of the rideshare practice, regardless of whether they answered the phone. In the control practice, patients were included in the analytical sample if they met prescreening criteria.
Eligible patients at the rideshare practice received the intervention. Eligible patients at the control practice did not receive the intervention. The practices have different clinical staff but share a social worker, who coordinates their application for NEMT services. For both clinics, we collected appointment attendance data for eligible patients scheduled during the period before (August 4 to September 16, 2016) and after (October 12–21, 2016) the intervention began. Given the nature of a pilot, the before and after periods differed in length to allow us to accurately record the trends leading up to the intervention period and to collect enough data to inform our operational decisions. This pilot was used to develop a larger ridesharing trial, which began shortly after the completion of this pilot study.
Intervention
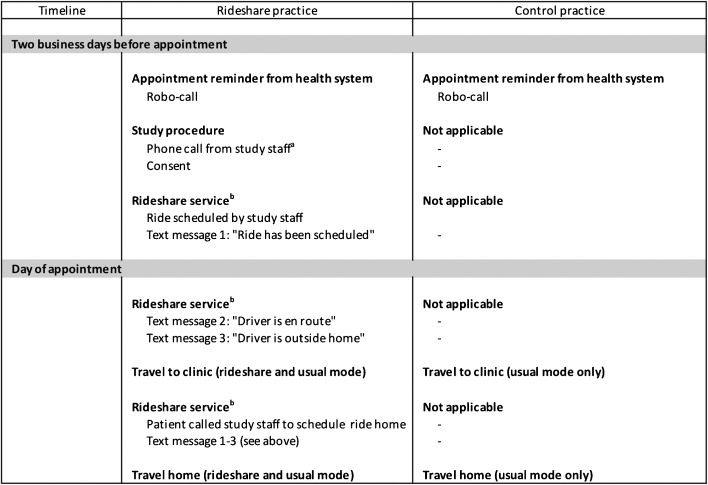
All eligible patients in the rideshare practice were prescreened using data within the electronic medical record and received a telephone reminder 2 days before their index appointment, during which they were offered free transportation to and from their appointment using Lyft (Fig. 1). No incentives were provided for participation in the study other than the free Lyft rides made available to patients in the rideshare practice.
Figure 1.
Comparison of procedures and appointment reminders for patients in the rideshare and control practices. aUp to three attempts. bAmong those who consented and utilized the service.
For patients who provided consent, their Lyft ride was prescheduled using a web-based application designed by Lyft, the Dispatch tool. The Dispatch tool mirrors the mobile phone app designed by Lyft, enabling ride requests and the ability to visualize rides while in transit to a specific destination for pick-ups and drop-offs. However, the requests were initiated and rides visualized by an intermediary—in our case, a study staff member—not the patient. The Dispatch tool circumvents the need for patients to have a smartphone or app. The tool was not designed specifically for the study and did not incur additional costs for our intervention. Lyft offers businesses, healthcare and non-healthcare, access to the tool upon request.
When a Lyft ride was scheduled using the Dispatch tool (Fig. 2), the patient received a series of three text messages informing them of the following: a) the ride had been scheduled by our team, b) a driver was assigned to pick them up (approximately 10 min prior to the driver’s arrival to the pick-up destination, which was the patient’s home or the primary care practice), c) the driver’s arrival at the pick-up destination. Similar to the process with the Lyft smartphone app, patients received a text message containing the name, telephone number, vehicle make and model, and vehicle license plate number when a driver was assigned to pick them up.
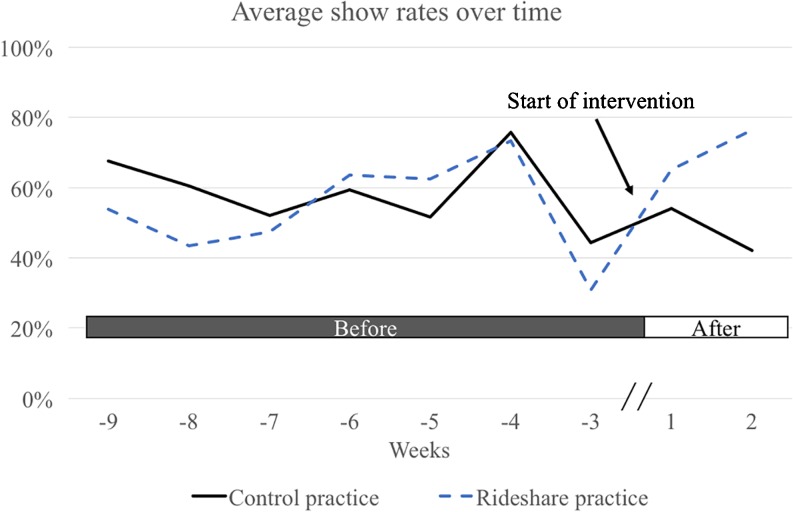
Figure 2.
Trends in show rates at the two practices.
For the return trip home, patients were provided a telephone number to call after their appointment. A research assistant received their phone call and dispatched a ride home using the Lyft Dispatch tool. Patients received the same three text message series for the return ride. Patients were provided the option of receiving round-trip or one-way transportation service (to or from their appointment). Neither patients nor the research team tipped drivers. Since the NEMT program for Medicaid is provided free of charge, this service was also offered free of charge.
For intervention practice patients who answered the initial phone call, we assessed for logistical barriers to using Lyft services (lacking a text-message-enabled phone, requiring a wheelchair-accessible vehicle, or not speaking English). Patients identified with one or more of these barriers were not offered a Lyft ride but were included in the primary intention-to-treat analysis, because patients in the control practice were not screened for these barriers.
Therefore, we preserved the comparability of patients at the two practices for the main analysis by retaining all patients at both practices who were prescreened for eligibility based on electronic medical record data.
Control
As part of usual care, each patient in the control practice received a phone call from an automated machine (i.e., “robocall”) 2 days prior to their appointment. They were not offered the rideshare service.
The automated phone calls occurred throughout each period in both the rideshare practice and the control practice. These robocalls transmit or leave automated voice messages. Therefore, patients in both practices received at least one phone call reminder for their upcoming appointments. In the rideshare practice, patients received one robocall and potentially (if they answered the call) a voice call from our research team, with a maximum of three attempts to reach the patient by our research assistants. Both robocalls and calls by our research team occurred on the same day: 2 business days prior to patients’ appointments. No voicemail messages were left by our research staff.
Research Staff Training and Oversight
To create consistent delivery of the intervention and the messaging, research assistants underwent a 2-hour training session before calling a study patient using a standardized script for the rideshare practices. Subsequently, staff were observed by the principal investigator on two separate occasions to evaluate for consistency between research assistants, and call logs were randomly checked to verify that eligible patients were called 2 business days prior to their appointments.
Measures
The primary outcome of this study was primary care appointment show rates for those in the rideshare clinic versus those in the control clinic. Show rates were extracted from the electronic medical record and were calculated as the ratio of 1 minus no-shows and same-day cancellations to total number of appointments [1 − (no-shows + same-day cancellations) / (total number of appointments)]. As one measure of program costs, we collected the cost per trip and cost per visit (the number who utilized the service as the denominator). We do not account for the cost of time on the part of the research staff, who were medical students conducting research as part of a research experience, nor do we capture the facility space costs (i.e., the rooms and computers they called from) which were shared among multiple research projects.
We also collected patient-level measures including demographic characteristics (age, gender, race, sex, and ZIP Code), Charlson Comorbidity Index, and provider characteristics (type of the primary care provider for the scheduled visit—attending physician, resident physician, or advanced practice nurse) from the electronic medical record.
Analyses of Primary Aims
Comparisons of baseline demographic data between intervention and control practice patients were conducted using t tests or χ2. We compared show rate changes at the two primary care practices (rideshare vs. control) between the two data collection periods using a difference-in-difference analytical approach. We modeled the effect using logistic regression with robust standard errors and exchangeable working correlation to adjust for patients with visits in both data collection periods. The difference-in-difference (change in adjusted odds ratio [∆ aOR]) is the interaction term between a categorical variable denoting the time period (before vs. after the intervention was implemented) and the practice type (rideshare vs. control). This design approach accounts for the influence of secular trends that do not vary between clinics and time-invariant differences between clinics. As a sensitivity analysis, we repeated the difference-in-difference model without individuals who used the rides to assess for additional effects from the added phone calls. We adjusted for patient demographics (age, gender, race, and ethnicity), ZIP Code, Charlson Comorbidity Index, and the type of provider the patient was scheduled to see during their appointment. Stata software (version 14.0; StataCorp LP, College Station, TX) was used for statistical analyses.
RESULTS
The study sample included 506 patients, with 194 (38%) from the rideshare and 312 (62%) from the control practice (Table 1). The study population was mostly middle-aged (mean 47.4, SD 12), female (75%), black (96%), and non-Hispanic (99%), with a Charlson Comorbidity Index of 2.1 (SD 2.5). The proportion of women differed between practices (78% vs. 70% in the control vs. rideshare practices, p = 0.02), and a greater number of patients were scheduled to see resident physicians in the rideshare practice (p < 0.001). During the intervention period at the rideshare practice, 60 patients were eligible and were called, 45 (75%) answered (25% were thus unreachable), 5 (8%) were not offered the service because they needed a wheelchair-accessible ride (n = 3) or had moved outside the West Philadelphia area (n = 2), 18 (30%) had a ride scheduled, and 13 (22%) ultimately used the service. Among the individuals who used the service, four used the ride to the clinic but not the ride home. The remaining individuals used the service for travel to and from the clinic.
Table 1.
Patient Characteristics for all Patients and by Practice Site
| Characteristics | All patients (n = 506) | Rideshare practice (n = 194) | Control practice (n = 312) | P value |
|---|---|---|---|---|
| Age, mean (SD), years | 47.4 (12) | 47.6 (12) | 47.3 (12) | 0.73 |
| Female, no. (%) | 376 (75) | 133 (70) | 243 (78) | 0.02 |
| Race, no. (%) | 0.34 | |||
| White | 13 (3) | 4 (2) | 9 (3) | |
| Black | 487 (97) | 187 (96) | 300 (97) | |
| Other or mixed | 5 (1) | 3 (2) | 2 (1) | |
| Ethnicity, no. (%) | 0.59 | |||
| Hispanic | 6 (1) | 2 (1) | 4 (1) | |
| Non-Hispanic | 495 (99) | 188 (99) | 307 (99) | |
| Charlson Comorbidity Index, mean (SD) | 2.1 (2.5) | 2.1 (2.5) | 2.0 (2.4) | 0.82 |
| Provider type, no. (%) | <0.001 | |||
| Resident | 292 (56) | 150 (77) | 132 (42) | |
| Attending | 151 (30) | 23 (12) | 128 (41) | |
| Nurse practitioner | 73 (14) | 21 (11) | 52 (17) | |
| Intervention uptake, no. | n = 60 | N/A | ||
| Answered the phone, no. (%) | – | 45 (75) | – | |
| Not offered a ride, no. (%) | – | 5 (8) | – | |
| Scheduled a ride for appointment, no. (%) | – | 18 (30) | – | |
| Did not use, no. (%) | – | 5 (8) | ||
| Used, no. (%) | – | 13 (22) | – |
Note: The ZIP Code distribution (19104, 19131, 19139, 19142, 19143, and 19151) was no different between the rideshare and control practices (p < 0.99). The data are not presented, because ZIP Codes are relatable only to those familiar with the Philadelphia region
For the rideshare practice, there were 134 individuals eligible in the before period and 60 eligible after the intervention was implemented. Similarly, the control practice had 245 individuals eligible before and 67 afterwards. In the weeks prior to the intervention, the trends in show rates fluctuated but were similar between practices (Fig. 2).
At the control practice, the show rate declined from 60% (146/245) to 51% (34/67; Table 2). At the rideshare practice, the show rate improved from 54% (72/134) to 68% (41/60). In the adjusted model, the odds of showing up for an appointment before and after implementation of the intervention changed significantly by a factor of 2.57 (95% CI 1.10–6.00) more in the rideshare practice compared to the control practice. In the sensitivity analysis, removing individuals who used the ride, the odds of showing up for an appointment were 1.70 (95% CI 0.71–4.05), indicating a nonsignificant increase in show rates due to the additional contact. The average cost per trip was $8.10, and the average cost per visit was $13.71.
Table 2.
Show Rates for Clinics Before and After Implementation of a Rideshare Intervention, the Adjusted Odds Ratios, and the Difference in Difference
| Rideshare practice | Control practice | ||||||
|---|---|---|---|---|---|---|---|
| Before period | After period | aOR (95% CI) | Before period | After period | aOR (95% CI) | Δ aOR | |
| No./total no. (%) | No./total no. (%) | ||||||
| Show rate | 72/134 (54) | 41/60 (68) |
1.97 (1.02–3.79)* | 146/245 (60) | 34/67 (51) |
0.78 (0.46–1.34) | 2.57 (1.10–6.00)* |
*P value <0.05
Note: The difference in difference (Δ aOR) is the interaction term between the before–after period and the clinic type (intervention vs. control clinic). The adjusted model included a variable for age, gender, race, ethnicity, Charlson Comorbidity Index, ZIP Code and provider type. aOR = adjusted odds ratio
DISCUSSION
The results of this pilot program suggest that offering a rideshare-based transportation service may increase show rates for primary care appointments among Medicaid patients. With a modest average cost per trip and modest level of uptake, our pilot study suggests that a ridesharing program could be scaled up in a cost-effective manner to increase appointment show rates for a high-need population, and that patients who do not need transportation services may not request them. Based on the best reported estimate, the cost of NEMT in 2014 was $28 per trip, although the researchers were not able to separate needs-based costs such as wheelchair versus non-wheelchair rides.13 To the best of our knowledge, our study is the first to experimentally test the impact of a transportation intervention on primary care practice attendance using rideshare-based medical transportation. Though our findings are significant, the confidence intervals for our pilot study are wide; therefore, these findings require replication and evaluation within the context of a larger trial.
Primary care practices and larger health systems could benefit financially if ridesharing services were effective in increasing appointment attendance rates. In fee-for-service and pay-for-performance environments, unused appointments (as high as 30% for clinical practices serving low-income, high-risk patients) represent significant opportunity costs and lost productivity.2,4,5,10 Face-to-face visits also serve as an opportunity for patients to engage in chronic disease management and preventive care—both important for achieving a high level of practice performance. In payment settings where providers bear the risk for the total cost of care, successful interventions that direct patients to high-value settings may be beneficial to providers as well. Though we tested this ridesharing intervention in a primary care setting, the findings may be relevant to other practice settings, including specialty care.2 One important limitation to the scalability of ridesharing interventions is that they require an adequate supply of ridesharing services, making it difficult to generalize this type of program to settings outside urban or densely populated suburban areas.
This study has several limitations. First, our primary outcome measured the effect of ridesharing services offered for free, which may limit generalizability. However, the NEMT benefit offered by Medicaid as part of usual care is also free in our setting. This cost-sharing structure may not be generalizable to other settings where copayments are a few dollars. Similarly, the decision to adopt this service will depend on local operational costs (e.g., staffing and facility space) and costs of providing NEMT, which vary widely based on contractual negotiations with local NEMT vendors. Second, there was a greater intensity of pre-appointment reminders (e.g., multiple follow-up attempts in addition to robocalls, and extended conversation about the appointment through consent procedures lasting approximately 5–10 min) for patients of the ridesharing practice, which could in part explain our results. Though an additional manual phone call for patients in ridesharing practices may have some measured effect on appointment show rates, there is little evidence that an additional phone-based reminder on the same day, 48-hours in advance, would provide an additive benefit or would change behavior.16,17 Third, the intervention required some program-level infrastructure to facilitate access to ridesharing services (i.e., study staff members readily available to dispatch rides), which may not be available for all outpatient practices or health systems. We designed the intervention in a manner to allow easy adaptability at our home institution. However, we believe the intervention is simple and can be easily scaled or modified in areas where rideshare services are easily accessible. Fourth, the low uptake among individuals who agreed to participate may reflect poor acceptability of the service, either because of concerns within this population regarding the use of ridesharing vehicles, or a technological gap in the ability to use the service because it is traditionally administered via smartphones. Alternatively, perhaps transportation is not as significant a barrier for many patients in our study sample, or those using existing NEMT services may have continued to prefer that service versus our one-time rideshare offer. Even among the patients who had rides scheduled, five (28%) did not ultimately use the service. Yet two of these showed up for their appointments, indicating there may be reasons for low uptake aside from need. Therefore, efforts to identify patients with high needs, either through predictive risk models or systematically asking about need, and efforts to understand the reasons for non-use may result in increased uptake of rideshare-based medical transportation. Fifth, we did not offer the ride to important and often marginalized populations—those with mobility challenges and predominantly non-English-speaking patients. Future efforts to improve transportation access should include these patient populations, who may have significant transportation needs which could be addressed by improved transportation services. Finally, our study was conducted at a single academic medical center, and thus our findings may not be generalizable to other health care or geographic settings, particularly in non-urban areas.
Though the social determinants of health are widely recognized as a major contributor to premature deaths in the United States,18 there are few evidence-based strategies to guide health systems toward addressing these determinants.19–21 In this study, we describe the promising results of a pilot program to address one such factor—transportation barriers. Though our findings are significant, larger transportation trials are needed to further assess whether rideshare-based transportation service models to improve health care access are worth testing before moving policy and payment in this direction.
Acknowledgments
Contributors
We thank Cheryl Garfield and Tamala Carter for helping provide perspectives on the study design as West Philadelphia community members.
Prior Presentations
A modified form of this manuscript was presented at the 2017 Society of General Internal Medicine National Meeting in Washington, DC, as a Mack Lipkin Sr. Associate Member Scientific Presentation Award Finalist.
Funders
This work was supported by a pilot grant from Penn’s Leonard Davis Institute of Health Economics. Dr. Krisda Chaiyachati received funds for training support from the VA Robert Wood Johnson Foundation Clinical Scholars Program. Lyft Incorporated provided a web-based dispatch tool for the study but did not provide any funding. The funders had no role in the preparation of the article, study design, collection of data, analysis, interpretation of data, or decision to submit the article for publication.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
References
- 1.Silver D, Blustein J, Weitzman BC. Transportation to clinic: findings from a pilot clinic-based survey of low-income suburbanites. J Immigr Minor Health. 2012;14(2):350–355. doi: 10.1007/s10903-010-9410-0. [DOI] [PubMed] [Google Scholar]
- 2.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Academies of Sciences, Engineering, and Medicine; Transportation Research Board; Health and Medicine Division; Board on Population Health and Public Health Practice . Exploring Data and Metrics of Value at the Intersection of Health Care and Transportation: Proceedings of a Workshop. Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 4.Kangovi S, Barg FK, Carter T, Long JA, Shannon R, Grande D. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Health Aff (Millwood). 2013;32(7):1196–1203. doi: 10.1377/hlthaff.2012.0825. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen DL, Dejesus RS. Increased frequency of no-shows in residents’ primary care clinic is associated with more visits to the emergency department. J Prim Care Community Health. 2010;1(1):8–11. doi: 10.1177/2150131909359930. [DOI] [PubMed] [Google Scholar]
- 6.White GB. Stranded: How America’s failing public transportation increases inequality. The Atlantic [Online]. 2015; http://www.theatlantic.com/business/archive/2015/05/stranded-how-americas-failing-public-transportation-increases-inequality/393419/. Accessed December 15, 2017.
- 7.Hwang AS, Atlas SJ, Cronin P, et al. Appointment "no-shows" are an independent predictor of subsequent quality of care and resource utilization outcomes. J Gen Intern Med. 2015;30(10):1426–1433. doi: 10.1007/s11606-015-3252-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cronk I. The Transportation Barrier. The Atlantic. August, 2015; http://www.theatlantic.com/health/archive/2015/08/the-transportation-barrier/399728/. Accessed December 15, 2017.
- 9.Agency for Healthcare Research and Quality. National Quality Measures Clearinghouse. Ambulatory care sensitive conditions age-standardized acute care hospitalization rate for conditions where appropriate ambulatory care prevents or reduces the need for admission to the hospital per 100,000 population younger than age 75 years. 2014; https://www.qualitymeasures.ahrq.gov/summaries/summary/48964. Accessed December 15, 2017.
- 10.Kaplan-Lewis E, Percac-Lima S. No-show to primary care appointments: why patients do not come. J Prim Care Community Health. 2013;4(4):251–255. doi: 10.1177/2150131913498513. [DOI] [PubMed] [Google Scholar]
- 11.The National Academy of Medicine. Accounting for Social Risk Factors in Medicare Payment: Identifying Social Risk Factors. Washington, DC: National Academies Press;2016. [PubMed]
- 12.Kaiser Family Foundation. Medicaid Benefits: Non-Emergency Medical Transportation Services. 2015; http://kff.org/medicaid/state-indicator/non-emergency-medical-transportation-services/. Accessed December 15, 2017.
- 13.Texas A&M Transportation Institute. Examining the effects of separate non-emergency medical transportation (NEMT) brokerages on transportation coordination. March 2014. https://groups.tti.tamu.edu/transit-mobility/files/2015/12/TCRP-B-44-Review-and-Summary-of-Relevant-Literature-FinalR.pdf, Access Date: December 15, 2017
- 14.Powers BW, Rinefort S, Jain SH. Nonemergency Medical Transportation: Delivering Care in the Era of Lyft and Uber. JAMA. 2016;316(9):921–922. doi: 10.1001/jama.2016.9970. [DOI] [PubMed] [Google Scholar]
- 15.Chaiyachati KH, Asch DA, Grande DT. Patient Inducements—High Graft or High Value? N Engl J Med. 2017;376(12):1107–1109. doi: 10.1056/NEJMp1613274. [DOI] [PubMed] [Google Scholar]
- 16.Hasvold PE, Wootton R. Use of telephone and SMS reminders to improve attendance at hospital appointments: a systematic review. J Telemed Telecare. 2011;17(7):358–364. doi: 10.1258/jtt.2011.110707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McLean SM, Booth A, Gee M, et al. Appointment reminder systems are effective but not optimal: results of a systematic review and evidence synthesis employing realist principles. Patient Prefer Adherence. 2016;10:479–499. doi: 10.2147/PPA.S93046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schroeder SA. Shattuck Lecture. We can do better--improving the health of the American people. N Engl J Med. 2007;357(12):1221–1228. doi: 10.1056/NEJMsa073350. [DOI] [PubMed] [Google Scholar]
- 19.Marmot M, Friel S, Bell R, Houweling TA, Taylor S, Commission on Social Determinants of Health Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 20.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(Suppl 2):19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kangovi S, Mitra N, Turr L, Huo H, Grande D, Long JA. A randomized controlled trial of a community health worker intervention in a population of patients with multiple chronic diseases: Study design and protocol. Contemp Clin Trials. 2017;53:115–121. doi: 10.1016/j.cct.2016.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]