Abstract
Objective
College students with anxiety and depressive symptomatology face escalated risk for alcohol-related negative consequences. While it is well-established that normative perceptions of proximal peers’ drinking behaviors influence students’ own drinking behaviors, it is not clear how mental health status impacts this association. In the current study, we examined cross-sectional relationships between anxiety and depressed mood, perceived drinking behaviors and attitudes of important peers, and past month alcohol consumption and related problems in a first-semester college student social network.
Method
Participants (N = 1,254, 55% female, 47% non-Hispanic White) were first-year students residing on campus at a single university who completed a web-based survey assessing alcohol use, mental health, and social connections among first-year student peers. Network autocorrelation models were used to examine the independent and interactive associations between mental health and perceptions of close peers’ drinking on drinking outcomes, controlling for important variables.
Results
Mental health interacted with perceptions to predict past-month drinking outcomes, such that higher anxiety and higher perceptions that peers drink heavily was associated with more drinks consumed and consequences, and higher depression and perceptions was associated with more drinks consumed, heavy drinking frequency, and consequences. Attitudes that peers approve of heavy drinking were associated with more drinks consumed and heavy drinking frequency among students with lower (vs. higher) depressed mood.
Conclusions
This study provides strong evidence that perceiving that close peers drink heavily is particularly risk-enhancing for anxious and depressed college students, and offers implications about alcohol intervention targeted at these subgroups.
Keywords: alcohol, depressed mood, anxiety, college peers, social network, perceptions
1.0 INTRODUCTION
An estimated 31 to 39% of U.S. college students report at least mild current depression and 27% report current anxiety (Gress-Smith, Roubinov, Andreotti, Compas, & Luecken, 2015; Herman et al., 2011; Ibrahim, Kelly, Adams, & Glazebrook, 2013; Mahmoud, Staten, Hall, & Lennie, 2012). College is also associated with peak lifetime drinking risk (Patrick & Schulenberg, 2011; White & Hingson, 2013), with approximately 30% of women and 40% of men reporting consumption of five or more drinks in one sitting in the past two weeks (ACHA, 2017), and one in five students meeting the criteria for alcohol use disorder per DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition) criteria (Blanco et al., 2008). The risk of experiencing negative consequences as a result of alcohol use (e.g., academic problems, college withdrawal, unsafe sex, overdose, suicidality) is substantially greater among students experiencing depressive symptoms (Martens et al., 2008; Miller, Miller, Verhegge, Linville, & Pumariega, 2002) and anxiety symptoms (Geisner, Larimer, & Neighbors, 2004; Linden, Lau-Barraco, & Milletich, 2013), even at drinking levels equivalent to those of peers (Dawson, Grant, Stinson, & Chou, 2005; Dennhardt & Murphy, 2011; Kenney, Lac, Labrie, Hummer, & Pham, 2013; Labrie, Kenney, & Lac, 2010; Weitzman, 2004). Furthermore, adults with persistent alcohol dependence from adolescence to adulthood exhibit higher rates of depression or anxiety diagnoses in adolescence (Meier et al., 2013). Therefore, identifying factors in the college environment that minimize or exacerbate alcohol-related risk in students with depressive or anxiety symptoms is important.
Among the strongest influences of college student psychosocial well-being and drinking behavior are peer networks (Borsari & Carey, 2001; Mason, Zaharakis, & Benotsch, 2014). Peer network drinking is strongly tied to personal alcohol use (Barnett et al., 2014; Cruz, Emery, & Turkheimer, 2012; Lau-Barraco & Linden, 2014; Meisel, Clifton, MacKillop, & Goodie, 2015), and college students’ perceptions and beliefs about peers’ drinking behavior are primary predictors of personal drinking behavior (e.g., Neighbors, Lee, Lewis, Fossos, & Larimer, 2007). The few studies that have examined how students’ depressive or anxiety symptoms may impact the relationship between peer norms and alcohol outcomes show mixed results. Pearson and Hustad (2014) found that higher perceptions of peer drinking (descriptive norms) mediated the relationship between hopelessness and alcohol use and problems in a sample of mandated college students. Thus, students experiencing hopelessness and social anxiety may be particularly conscious of their peers’ drinking behaviors, and may conform to these norms in order to try to connect socially or avoid negative evaluation.
In support of this interpretation, Neighbors, Fossos, et al. (2007) found the relationship between descriptive norms and drinking to be stronger among college students with high (as opposed to low) social anxiety. However, Buckner, Ecker, and Proctor (2011) found that among students with high descriptive norms, those with lower social interaction anxiety drank more than their socially anxious peers, contradicting findings from Neighbors et al., and suggesting that socially anxious students may drink less when they perceive that peers drink heavily, perhaps in an attempt to avoid potential embarrassment they witness in their social environment. Methodological differences may explain these differential findings. Whereas Neighbors at al. (2007) assessed social anxiety using a relatively broad measure of self-consciousness in a sample of drinkers and non-drinkers, Buckner et al. (2011) used a clinical cut-score to assess the presence of social interaction anxiety in a sample of current drinkers. It is possible that among student drinkers with heightened perceptions of heavy peer drinking, those without social interaction anxiety and accompanying inhibitions may be more inclined to drink in ways consistent with perceptions of college drinking contexts.
There are also mixed findings on the relationship between anxiety, perceived peer approval of drinking (injunctive norms), and alcohol use; Pearson and Hustad (2014) found that anxiety sensitivity was inversely associated with perceptions of peer approval of drinking and alcohol use in a sample of college students mandated for alcohol violations. Buckner et al. (2011) found no correlation between social interaction anxiety and injunctive norms, although students with high injunctive norms and high social interaction anxiety experienced the most alcohol-related problems. While Pearson’s study did not assess moderating effects, Buckner’s findings show that beliefs that friends approve of heavy drinking may be particularly risk-enhancing for students with social interaction anxiety, perhaps because they believe they will not be negatively evaluated by friends if they drink heavily. In sum, more research is needed to determine the extent to which the relationships between students’ perceptions about peers’ alcohol use and attitudes differentially impact their alcohol risk outcomes depending on the presence of depressed mood and anxiety.
There is strong theoretical [e.g. Social Comparison Theory (Festinger, 1954) and Social Impact Theory (Latane, 1981)] and empirical (Collins & Spelman, 2013; McAlaney & McMahon, 2007) support demonstrating that an individual’s perceptions of the behavior of close friends is more predictive of that person’s drinking behavior than more distal referents. In a social network study of 670 college students (Mason et al., 2014), those reporting greater contact with and perceiving greater alcohol use among their three best friends were exponentially more likely to report hazardous drinking themselves. In our prior work examining a college dormitory social network (Kenney, Ott, Meisel, & Barnett, 2017), we found that students held more accurate perceptions of drinking among peers they identified as important to them than peers in their dormitory as a whole. Moreover, these descriptive perceptions of important peers were more strongly associated with personal drinking than their dormitory descriptive norms. Therefore, accounting for and better understanding the role of salient (as opposed to typical or more distal) peers in college students’ alcohol risk behavior appears warranted.
1.1 Study Aims and Hypotheses
In the current study, we examined cross-sectional relationships between symptoms of anxiety and depression, descriptive and injunctive perceptions of important peers, alcohol consumption, and alcohol-related problems in a first-semester college student social network. We utilized a sociocentric (i.e., whole network) approach to assess students’ perceptions about the drinking behaviors and attitudes of up to ten nominated peers in the student network. Consistent with existing research, we expected higher anxiety and depressed mood to be associated with more alcohol-related negative consequences, after controlling for alcohol use. Based on prior work showing that student normative beliefs are differentially associated with alcohol outcomes as a function of mental health, we hypothesized that endorsing perceptions that nominated peers drink heavily and approve of heavy drinking would be particularly risky for students with higher (vs. lower) depressed mood or anxiety, such that greater endorsement of these beliefs would be associated with significantly greater drinking and consequences.
2. Method
2.1 Participants
Participants were first-semester college students recruited for a larger study on alcohol use and social networks at a mid-sized, private university in the northeastern United States. All students living in first-year dormitories (n = 1,660) were eligible to participate; students not residing in these dormitories (n = 32) were ineligible. Of these, 1,342 (81%) completed the first-wave of the longitudinal web-based survey from which these data were drawn. Eighty-eight individuals nominated 0 individuals in the sociocentric network questionnaire; hence, these individuals provided no perceptions of the behavior of close peers1. Thus, analyses were restricted to the 1,254 participants who identified one or more peers on the network survey. Participants averaged 18.65 (SD = 0.51) years old, and 55.6% were female based on sex assigned at birth. Participants identified as: 43.9% male; 54.9% female; 1.3% transgender or gender nonconforming. The racial composition was 55.9% non-Hispanic White, 23.7% Asian, 6.8% Black, 10.0% Multiracial, 0.9% American Indian/Alaskan Native, 0.2% Native Hawaiian, and 2.3% unknown. Fifteen percent reported Hispanic ethnicity. Finally, 13.6% were athletes, and 13.2% lived in a substance free dormitory.
2.2 Procedures
At the beginning of the fall 2016 academic semester, all eligible first-year students were invited to participate in a research study on social networks and health behaviors. We advertised the study with postcards mailed to campus mailboxes, e-mails, via social media, and in-person in communal areas and at campus events. Students provided consent to participate online or in person; students under 18 years of age provided assent before obtaining parental consent.
Six weeks into the first semester, students were emailed a link to a secure web-based survey that assessed demographics, alcohol and other substance use, mental health symptoms, and social network ties to other first-year students. We administered the survey during this time to allow sufficient time for students to develop ties to other students in the network. All survey questions assessing alcohol consumption were accompanied by a chart that defined a standard drink: “12 oz. beer, 5 oz. wine, or 1.5 oz. of 80 proof liquor” (NIAAA, 2017b). Participants were emailed a $50 Amazon gift card upon completion of the approximately 45-minute survey. All study procedures were approved by the Brown University Institutional Review Board.
2.3 Measures
2.3.1 Demographic characteristics
Participants reported their age, sex, gender, race, and ethnicity, as well as membership on a collegiate athletic team, and residence in a substance free dormitory.
2.3.2 Alcohol Consumption
Two past-month alcohol use measures were used: number of drinks consumed and frequency of heavy drinking, defined for all participants as five or more drinks in one occasion. Number of drinks consumed was calculated by multiplying responses to the following two questions assessed for the past 30 days: “On how many days did you have at least one drink of any alcoholic beverage?” and “On days when you drank, how many drinks did you drink on average?” Heavy drinking frequency was assessed by asking, “Considering all types of alcoholic beverages, how many times during the past 30 days did you have five or more drinks in one occasion?” Response options ranged from 0 to 30 times, and “more than 30 times.”
2.3.3 Alcohol Consequences
We used the Brief Young Adult Alcohol Consequences Questionnaire (BYAACQ; Kahler, Strong, & Read, 2005) to assess alcohol consequences (α = .82). The BYAACQ presents 24 consequences (e.g., “I have taken foolish risks when I have been drinking,” “I have passed out from drinking”). Participants indicated whether they had experienced each consequence (no=0, yes=1) in the past 30 days. Scores were summed to characterize alcohol problem severity (range: 0-24). The BYAACQ has demonstrated reliability and validity in college student populations (Borsari, Murphy, & Barnett, 2007; Kahler, Hustad, Barnett, Strong, & Borsari, 2008; Pearson, Kite, & Henson, 2013).
2.3.4 Anxiety and Depressed Mood
The Perceived Health Questionnaire (PHQ-4; Kroenke, Spitzer, Williams, & Lowe, 2009) is a four-item screener that combines two previously validated measures (PHQ-2; Kroenke, Spitzer, & Williams, 2003; GAD-2; Kroenke, Spitzer, Williams, Monahan, & Löwe, 2007). The PHQ-4 has demonstrated construct and factorial validity in a sample of primary care patients (Kroenke et al., 2009). Participants were asked to rate how often they have been bothered by two symptoms of anxiety and two symptoms of depression. We modified this measure by changing the original assessment time frame from the past two weeks to the past month to be consistent with other questions in our survey. Response values were unchanged: 0 (not at all), 1 (several days), 2 (more than half the days), and 3 (nearly every day). Summary scores for the anxiety and depression subscales range from 0 to 6, with higher scores indicating greater symptom severity.
2.3.5 Important Peer Network Survey
Participants were asked to select up to ten other students in the first-year class who were important to them in the last month, i.e. “People you socialized with, studied with, or regularly had fun with” (adapted from the Important People Instrument, Zywiak, Longabaugh, & Wirtz, 2002). Participants could select the names of important peers from a drop-down list of students in the first-year class who did not opt-out of being in this list (n = 1,6212). Next, participants answered questions about the alcohol use of each peer they selected.
2.3.6 Descriptive Perceptions of Nominated Peers
For each important peer in the network survey, participants were asked, “How many times in the past 30 days do you think this person had five or more drinks on one occasion?” Response options were 0 to 30 times. We then calculated the average perceived frequency of heavy drinking among each participants’ network of important peers.
2.3.7 Injunctive Perceptions of Nominated Peers
We assessed perceived attitudes about heavy drinking for each nominated peer by asking participants “How do you think this person would feel about you having five or more drinks in one occasion?” Response options ranged from 1 (Strongly disapprove) to 7 (Strongly approve). We then calculated the average perceived approval of heavy drinking among each participants’ network of important peers.
2.4 Data Analysis
Network autocorrelation models were used to examine the interaction between perceptions and mental health on alcohol consumption and related consequences. Unlike traditional linear regression models, network autocorrelation models account for correlations between individuals in the network, and are thereby commonly used in social network data analysis (Anselin, 1988; Fujimoto, Chou, & Valente, 2011). Separate models were conducted to examine the two-way interaction between 1) mental health (anxiety/depressed mood) and injunctive perceptions, and 2) mental health and descriptive perceptions on three outcomes: 1) number of drinks consumed, 2) frequency of heavy drinking, and 3) total number of alcohol-related consequences in the past month. All network autocorrelation models controlled for covariates that have known association with alcohol use (birth sex, White race, athlete status, and residence in a substance free dorm). Models predicting alcohol consequences controlled for number of drinks consumed in the past month. Covariates were entered at Step 1. Main effects were entered at Step 2. Two-way interactions terms were entered at Step 3. For significant interaction terms, we examined simple slopes by generating one SD above and below the mean for each norm. All analyses were conducted in SPSS and in R using the sna (Butts, 2010).
3. Results
Means, standard deviations, and bivariate correlations between key variables were conducted and are displayed in Table 1. Anxiety and depressed mood were negatively correlated with descriptive perceptions. Depressed mood was negatively related to injunctive perceptions. Anxiety and depressed mood were negatively related to the consumption variables, but positively related to the total number of negative consequences.
Table 1.
Descriptive statistics and bivariate correlations between the key variables.
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1. Anxiety | 2.1 | 1.7 | – | |||||
| 2. Depressed mood | 1.4 | 1.4 | .59*** | – | ||||
| 3. Descriptive perceptions | 2.5 | 2.9 | −0.09** | −.06* | – | |||
| 4. Injunctive perceptions | 3.6 | 1.3 | −0.05 | −.07* | .49*** | – | ||
| 5. Number of drinks in past month | 20.1 | 24.0 | −.07* | −.07* | .64*** | .49*** | – | |
| 6. Heavy drinking days in past month | 1.8 | 2.8 | −.08** | −.07* | .65*** | .45*** | .89*** | – |
| 7. Alcohol consequences in past month | 3.8 | 3.4 | .12*** | .14*** | .37*** | .25*** | .59*** | .55*** |
3.1 Anxiety
As shown in Table 2, three network autocorrelations were conducted to examine the two-way interactions between 1) anxiety and injunctive perceptions, and 2) anxiety and descriptive perceptions on number of drinks consumed in the past month, heavy drinking frequency, and total number of alcohol-related consequences in the past month. Results at Step 2 showed significant main effects of injunctive and descriptive perceptions on both alcohol consumption measures but not consequences. There was a main effect of anxiety on alcohol-related consequences but not on drinking measures.
Table 2.
Three separate network autocorrelation models 1) number of drinks consumed, 2) drinking frequency, and 3) alcohol-related consequences in the past month. All models controlled for sex, race, athlete status, and substance free dorm residence. When predicting alcohol-related consequences, drinks per month was controlled for. Main effects were entered at Step 2 and the interactions between anxiety symptoms and injunctive perceptions, and the interaction between anxiety symptoms and descriptive perceptions were entered at Step 3.
| Number of drinks consumed | Heavy drinking frequency | Alcohol-related consequences | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | b | SE | z | p | B | SE | z | p | b | SE | z | p |
| Step 1 | ||||||||||||
| Anxiety | 0.12 | 0.51 | 0.24 | 0.81 | −0.01 | 0.06 | −0.15 | 0.88 | 0.57 | 0.10 | 5.99*** | < 0.00001 |
| Injunctive perceptions | 4.68 | 0.61 | 7.74*** | < 0.00001 | 0.42 | 0.07 | 5.92*** | < 0.00001 | 0.00 | 0.11 | −0.01 | 0.99 |
| Descriptive perceptions | 10.79 | 0.61 | 17.54*** | < 0.00001 | 1.46 | 0.07 | 20.29*** | < 0.00001 | 0.17 | 0.11 | 1.49 | 0.14 |
| Step 2 | ||||||||||||
| Anxiety X Injunctive | −1.08 | 0.56 | −1.93 | 0.054 | −0.06 | 0.07 | −0.97 | 0.33 | −0.04 | 0.11 | −0.40 | 0.69 |
| Anxiety X Descriptive | 1.77 | 0.58 | 3.07** | 0.002 | 0.08 | 0.07 | 1.13 | 0.26 | 0.32 | 0.10 | 3.23** | 0.0012 |
Results at Step 3 showed a significant two-way interaction between anxiety and descriptive perceptions on number of drinks consumed and alcohol-related consequences. As displayed in Figure 1, there was a stronger positive association between descriptive perceptions and drinks in the past month among students with higher levels of anxiety (b = 12.96, SE = 0.93, z = 14.01, p < .001) versus lower levels of anxiety (b = 9.43, SE = 0.76, z = 12.34, p < .001). Among students with high levels of anxiety, there was a positive association between descriptive perceptions and alcohol-related consequences (b = 0.56, SE = 0.17, z = 3.36, p < .001), but no association among students with low levels of anxiety (b = −0.08, SE = 0.14, z = −0.57, p = .57) (see Figure 1). As shown in Table 2, there was no interaction between anxiety and descriptive perceptions on heavy drinking frequency, and there were no significant interactions between anxiety and injunctive perceptions on any outcome measures.
Figure 1.
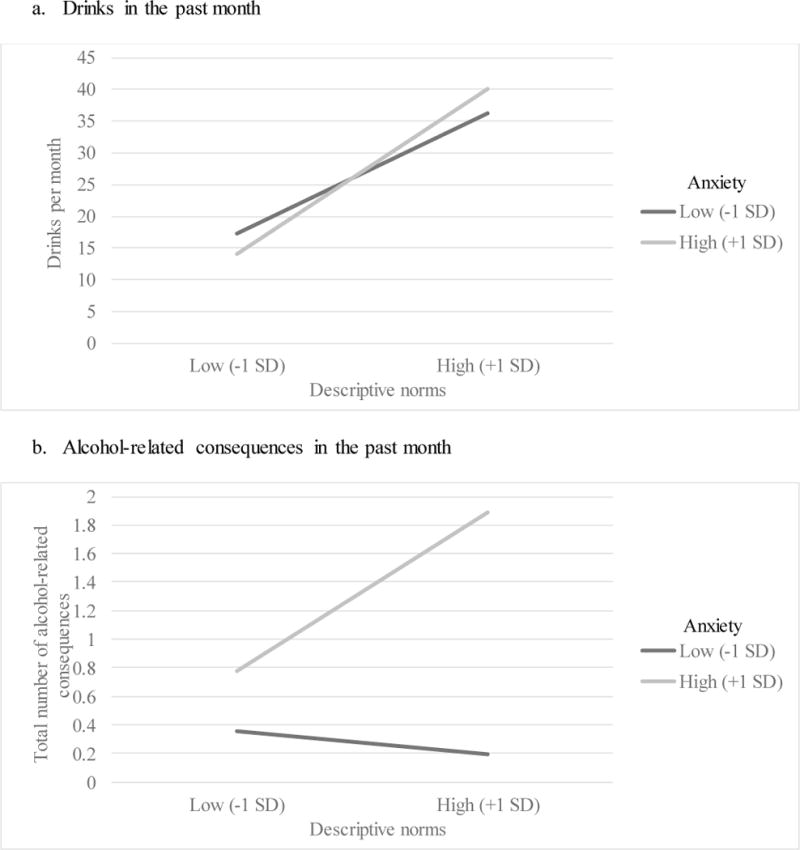
Significant interaction between anxiety and descriptive perceptions on number of drinks consumed and total number of alcohol-related consequences in the past month.
3.2 Depressed mood
As shown in Table 3, three network autocorrelations were conducted to examine the two-way interactions between 1) depressed mood and descriptive perceptions, and 2) depressed and injunctive perceptions on number of drinks consumed, heavy drinking frequency, and alcohol-related consequences. There were main effects of injunctive and descriptive perceptions on number of drinks in the past month and heavy drinking frequency but not alcohol-related consequences. There was a main effect of depressed mood on alcohol-related consequences but not on drinks in the past month or heavy drinking frequency.
Table 3.
Three separate network autocorrelation models predicting 1) drinks per month, 2) heavy drinking frequency, and 3) alcohol-related consequences. All models controlled for sex, race, athlete status, and substance free dorm residence. When predicting alcohol-related consequences, drinks per month was controlled for. Main effects were entered at Step 2 and the interactions between depressed mood and injunctive perceptions, and the interaction between depressed mood and descriptive perceptions were entered at Step 3.
| Drinks per month | Heavy drinking frequency | Alcohol-related consequences | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | b | SE | z | p | b | SE | z | p | b | SE | z | p |
| Step 1 | ||||||||||||
| Depressed mood | −0.13 | 0.51 | −0.26 | 0.79 | −0.06 | 0.06 | −0.93 | 0.35 | 0.56 | 0.09 | 6.00*** | < 0.00001 |
| Injunctive perceptions | 4.68 | 0.61 | 7.74*** | < 0.00001 | 0.42 | 0.07 | 5.90*** | < 0.00001 | 0.01 | 0.11 | 0.09 | 0.93 |
| Descriptive perceptions | 10.78 | 0.61 | 17.56*** | < 0.00001 | 1.46 | 0.07 | 20.29*** | < 0.00001 | 0.13 | 0.11 | 1.12 | 0.26 |
| Step 2 | ||||||||||||
| Depressed mood X Injunctive | −1.79 | 0.58 | −3.07** | 0.0021 | −0.20 | 0.07 | −2.80** | 0.005 | −0.03 | 0.11 | −0.25 | 0.80 |
| Depressed mood X Descriptive | 1.74 | 0.55 | 3.16** | 0.0016 | 0.16 | 0.07 | 2.47* | 0.014 | 0.32 | 0.09 | 3.50*** | 0.0005 |
Five of the six two-way interactions between perceptions and depressed mood on alcohol outcomes were statistically significant. There was a similar interaction between injunctive perceptions and depressed mood on number of drinks and heavy drinking frequency (Figure 2). Simple slopes analyses showed a stronger association between injunctive perceptions and past month drinks at low levels of depressed mood (b = 6.39, SE = 0.82, z = 7.83, p < .001) compared to high levels of depressed mood (b = 2.80, SE = 0.86, z = 3.24, p = .001). Similarly, there was a stronger relationship between injunctive perceptions and heavy drinking at low levels of depressed mood (b = 0.61, SE = 0.10, z = 6.28, p < .001) than at high levels of depressed mood (b = 0.22, SE = 0.10, z = 2.13, p = .03). There was no interaction between injunctive perceptions and depressed mood on alcohol-related consequences.
Figure 2.
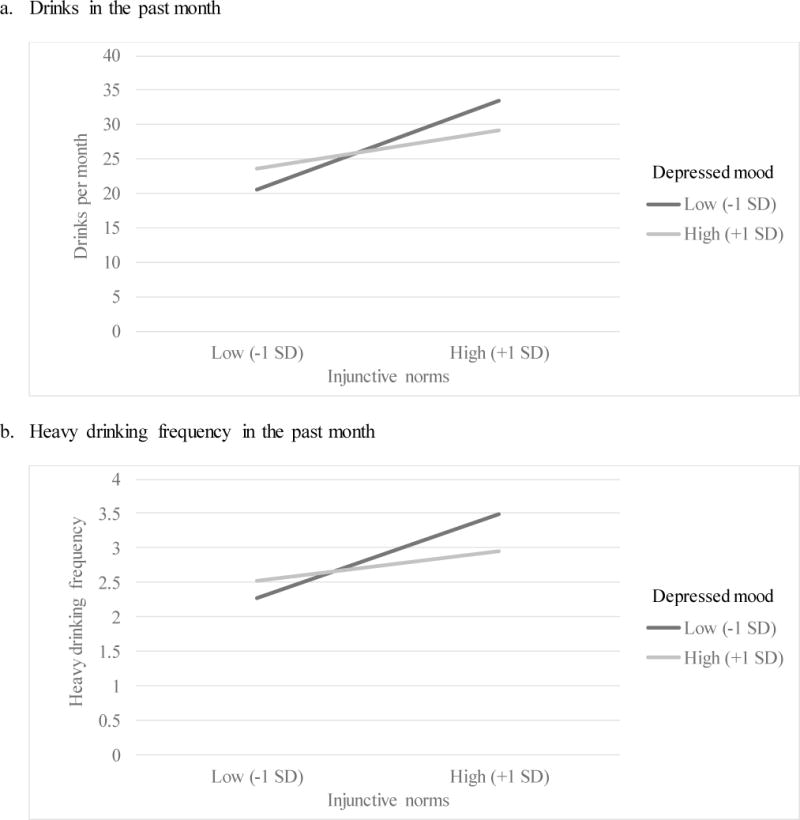
Interaction between depressed mood and injunctive perceptions on number of drinks consumed and heavy drinking frequency in the past month.
Similar interactions emerged between descriptive perceptions and depressed mood on drinking (see Figure 3). There was a stronger positive association between descriptive perceptions and number of drinks among students with high (b = 12.64, SE = 0.84, z = 14.99, p < .001) versus low (b = 9.17, SE = 0.80, z = 11.46, p < .001) levels of depressed mood. Similarly, there was a stronger positive association between descriptive perceptions and heavy drinking frequency among students with high (b = 1.63, SE = 0.10, z = 16.52, p < .001) compared to low (b = 1.31, SE = 0.09, z = 13.91, p < .001) levels of depressed mood. Lastly, simple slopes analyses indicated a positive association between descriptive perceptions and alcohol-related consequences among students with high levels of depressed mood (b = 0.48 SE = 0.15, z = 3.11, p = .002), but not low levels of depressed mood (b = −0.17, SE = 0.14, z = −1.23, p = .22; Figure 3).
Figure 3.
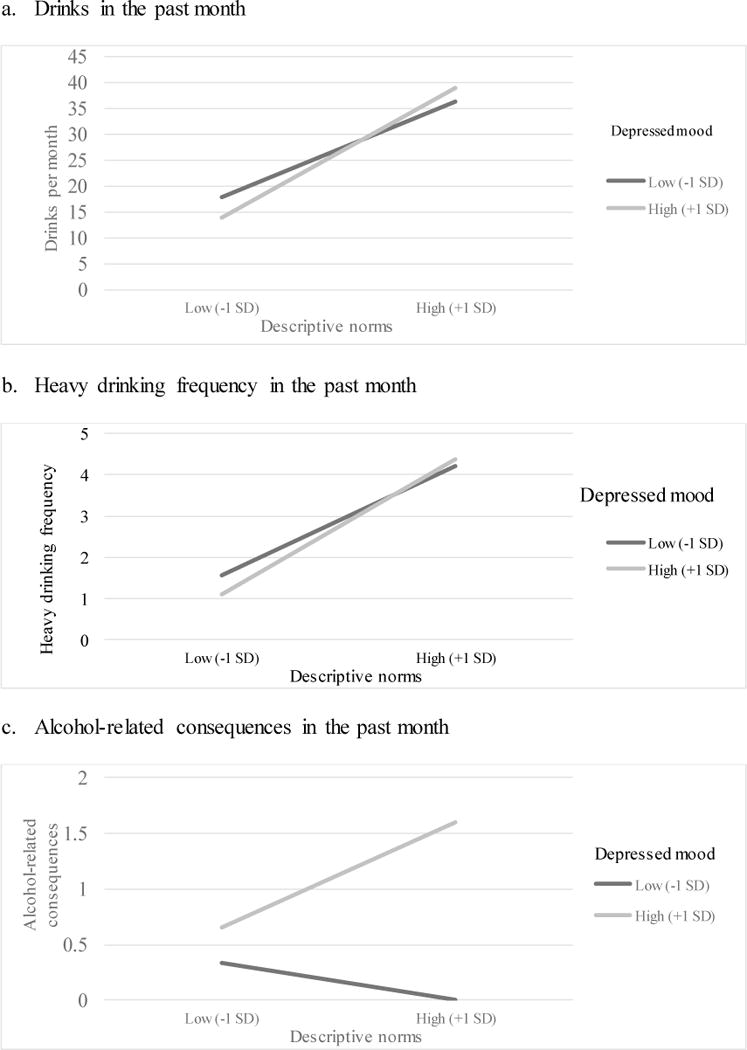
Interaction between depressed mood and descriptive perceptions on number of drinks consumed, heavy drinking frequency, and total number of alcohol-related consequences in the past month.
4. Discussion
In the current study, we examined the interactive relationships among anxiety, depressed mood, and perceptions about important, proximal peers’ alcohol behaviors and beliefs to predict alcohol consumption and consequences within a large social network of first-semester college students. Consistent with existing research, we found that higher descriptive and injunctive perceptions were independently associated with greater levels of alcohol consumption (e.g., Neighbors, Lee, et al., 2007), and poor mental health was independently associated with greater alcohol-related consequences, after controlling for the number of drinks consumed in the past month (e.g., Dennhardt & Murphy, 2011; Kenney, Jones, & Barnett, 2015; Kenney et al., 2013; Linden et al., 2013; Martens et al., 2008). Our results support that holding higher descriptive perceptions appears particularly risk-enhancing for students with elevated depressed mood or anxiety symptoms, as assessed by a global measure of anxiety. Although the relationship between mental health and normative perceptions was more strongly associated with alcohol consequences than drinking overall, perceived approval of drinking among close peers was more strongly linked to increased drinking among students with lower (as opposed to higher) depressed mood.
The most striking finding in the current study was that perceptions of close peers’ drinking was related to significantly more consequences among students reporting depressed mood or anxiety, but not associated with consequences among students with stronger mental health. These findings are consistent with research showing that higher descriptive perceptions are associated with increased drinking levels among students with high social anxiety (Neighbors, Fossos, et al., 2007) as opposed to low social anxiety (Buckner et al 2011). Relative to non-depressed and non-anxious peers who share similar perceptions, depressed and anxious student drinkers may be less attentive to risky surroundings and situations, and may lack the decision-making ability and social competency that offer protection from harm (for review see Castaneda, Tuulio-Henriksson, Marttunen, Suvisaari, & Lonnqvist, 2008). Students with poor mental health also tend to report less social support from peers (Hefner & Eisenberg, 2009; La Greca & Lopez, 1998; Mason et al., 2014) and are less likely to implement many protective behavioral strategies (Kenney & LaBrie, 2013; Labrie et al., 2010), both of which offer protection from alcohol-related harm while drinking. Furthermore, depressed and anxious student drinkers are susceptible to drinking to cope with negative affective states, a primary predictor of alcohol risk outcomes (Kenney et al., 2013; Kuntsche, Knibbe, Gmel, & Engels, 2005; Kuntsche, Stewart, & Cooper, 2008). In contrast, non-depressed and non-anxious peers tend to drink for social reasons and may avoid drinking when experiencing acute negative mood states (Stewart & Devine, 2000). Regardless of whether their close friends drink to cope with aversive states, depressed and anxious students who perceive heavy drinking to be a common behavior within their peer network may be vulnerable to use alcohol as a means to cope with aversive states.
Although descriptive perceptions are associated with alcohol consumption and consequences, particularly alcohol-related negative consequences, among students with poor mental health, we did not see a similar pattern with respect to injunctive perceptions. In contrast to Buckner et al.’s (2011) finding that injunctive perceptions and alcohol-related problems are stronger among socially anxious students, in the present study, anxiety (assessed globally) did not moderate the association between injunctive perceptions and alcohol outcomes. One way to interpret the different findings is that unlike students with social anxiety, students with global anxiety may not be inclined to drink more in order to conform to the perceived approval of peers’ attitudes about drinking (Buckner & Shah, 2015). Interestingly, the relationship between injunctive perceptions and drinking was strongest among students with lower depressed mood. Although this finding is difficult to interpret in light of the limited research, there is some evidence from the adolescent literature that injunctive perceptions are more strongly related to alcohol-related risk among adolescents without mental health problems (Pedersen et al., 2013). It is possible that depressed students may lose interest or pleasure from social activities and become more socially isolated (Hames, Hagan, & Joiner, 2013), making perceptions of peer approval less influential than for non-depressed students. It is also important to note that among students with high injunctive perceptions, even though non-depressed students drank more than depressed students, they did not experience significantly more consequences associated with drinking. These findings conflict with the theory that depressed individuals engage in excessive reassurance seeking (Joiner, Alfano, & Metalsky, 1992) and call for a better understanding of the relationship between depressed mood, injunctive perceptions, and alcohol risk.
4.1 Implications and Future Directions
Results from the current study inform existing efforts to prevent and intervene on alcohol misuse among a vulnerable population of college students. Social norms-based interventions that include a normative correction component have demonstrated efficacy in college populations, with some evidence that reducing descriptive norms leads to reduced consumption and problems among students with depressed mood (Geisner, Neighbors, Lee, & Larimer, 2007). Similar evidence exists for the efficacy of correcting normative beliefs on reducing drinking among socially anxious students (Terlecki, Buckner, Larimer, & Copeland, 2012). In light of our findings, interventions targeting descriptive perceptions of close peers, rather than injunctive perceptions, may be most effective for anxious and depressed students. Campus-based counseling approaches should screen for co-occurring anxiety, depression, and alcohol misuse; address students’ perceptions of friends’ drinking; and promote healthy coping and harm reduction strategies. Still, more research is needed to understand the reasons behind the contrasting effects associated with descriptive and injunctive perceptions among depressed and anxious students, and to establish the efficacy of social-norms based interventions for depressed and anxious college students in particular.
4.2 Strengths and Limitations
This is the first known study to examine the moderating role of depressed mood on the relationship between close peer perceptions and alcohol consumption and problems among college students. Other strengths include the enrollment of a large proportion of a first-year college class, and the use of sociocentric network methods. We also assessed normative perceptions of important, proximal peers, which may have resulted in more salient predictors of college students’ alcohol use than relying on students’ perceptions of broad reference groups.
Several limitations of this study are worth mentioning. First, depressed mood and anxiety were assessed using the brief PHQ-4 screener. Comparisons between the results of this study and previous studies examining social anxiety should be made with caution because the nature of social anxiety may have distinct relationships with alcohol use that are not captured using a brief, global measure of anxiety. In addition, we do not distinguish between clinical and non-clinical levels of anxiety or depressed mood. Second, it is unknown how social influences from outside the first-year college student network may have affected students’ drinking behaviors, or how these results may generalize to other colleges, or to college students in other class years. Third, the cross-sectional design precludes the ability to assert causality. We were not able to determine if depressed and anxious students are self-selecting into heavy drinking networks or if peer drinking behaviors are impacting their risk potential. Therefore, we were also unable to disentangle the potentially bidirectional relationships between poor mental health and alcohol-related consequences. Finally, it is important to note that the Substance Abuse and Mental Health Services Administration (SAMHSA) defines heavy episodic drinking and binge drinking as “five or more alcoholic drinks for males or four or more alcoholic drinks for females on the same occasion” (NIAAA, 2017a). In our survey, questions about peers’ heavy drinking were not gender specific in order to be consistent across all measures of heavy drinking (personal and peers’ heavy drinking).
Highlights.
Depression and anxiety were independently associated with greater alcohol consequences, controlling for drinking.
Higher anxiety and perceptions that peers drink heavily was associated with more drinks consumed and consequences.
Higher depression and perceptions that peers drink heavily was associated with more drinks consumed, heavy drinking frequency, and consequences.
Attitudes that peers approve of heavy drinking were associated with more drinks consumed and heavy drinking frequency among students with lower (vs. higher) depressed mood.
Acknowledgments
Role of Funding Source
This study was funded by the National Institute on Alcohol Abuse and Alcoholism (R01AA00015644). Trial registered at clinicaltrials.gov; Clinical Trial # NCT02895984. Dr. Kenney is funded by the National Institute on Drug Abuse (RO1 DA034261) and Dr. Meisel is funded by the National Institute on Alcohol Abuse and Alcoholism (T32AA007459 and K01AA025994).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Independent samples t-tests were conducted to compare differences in anxiety and depression symptoms between participants who nominated 0 important peers and those who nominated at least one. There was no significant difference in anxiety symptoms (M = 2.20, SD = 1.84; M = 2.13, SD = 1.69; t(1337) = 0.41, p = .68) and depression symptoms (M = 1.39, SD = 1.35; M = 1.35, SD = 1.45; t(1337) = 0.20, p = .84).
Thirty-nine students (2%) opted-out when given the opportunity during the enrollment phase.
Contributors
Dr. Barnett collected the data used in the current manuscript. Dr. Kenney, Dr. Meisel, Mr. DiGuiseppi, and Ms. Balestrieri were on the project team of the R01 through which the data were collected, and thus assisted in all aspects on the grant. All authors generated the design and analyses used in the current study. Dr. Kenney, Mr. DiGuiseppi, and Ms. Balestrieri conducted the literature review, wrote the Introduction, Methods, and Discussion, and revised the final draft of the manuscript. Dr. Meisel conducted statistical analyses and wrote the Results section. Dr. Barnett reviewed and provided feedback on drafts of the manuscript, and all authors contributed to and have approved the final manuscript.
Conflict of Interest
There are no conflicts of interest to report.
References
- ACHA. American College Health Association-National College Health Assessment II: Undergraduate Student Reference Group Executive Summary Fall 2016. Hanover, MD: 2017. Retrieved from. [Google Scholar]
- Anselin L. Spatial Econometrics: Methods and ModelsKluwer Academic. Boston, MA: 1988. [Google Scholar]
- Barnett NP, Ott MQ, Rogers ML, Loxley M, Linkletter C, Clark MA. Peer associations for substance use and exercise in a college student social network. Health Psychology. 2014;33(10):1134–1142. doi: 10.1037/a0034687. [DOI] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu SM, Olfson M. Mental health of college students and their non–college-attending peers: results from the national epidemiologic study on alcohol and related conditions. Archives of general psychiatry. 2008;65(12):1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Peer influences on college drinking: A review of the research. Journal of Substance Abuse. 2001;13(4):391–424. doi: 10.1016/s0899-3289(01)00098-0. [DOI] [PubMed] [Google Scholar]
- Borsari B, Murphy JG, Barnett NP. Predictors of alcohol use during the first year of college: Implications for prevention. Addict Behav. 2007;32(10):2062–2086. doi: 10.1016/j.addbeh.2007.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Ecker AH, Proctor SL. Social anxiety and alcohol problems: The roles of perceived descriptive and injunctive peer norms. Journal of Anxiety Disorders. 2011;25(5):631–638. doi: 10.1016/j.janxdis.2011.02.003. doi: https://doi.org/10.1016/j.janxdis.2011.02.003. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Shah SM. Fitting in and feeling fine: Conformity and coping motives differentially mediate the relationship between social anxiety and drinking problems for men and women. Addict Res Theory. 2015;23(3):231–237. doi: 10.3109/16066359.2014.978304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butts CT. sna: Tools for Social Network Analysis. R package version 2.2-0. 2010 Retrieved from http://CRAN.R-project.org/package=sna.
- Castaneda AE, Tuulio-Henriksson A, Marttunen M, Suvisaari J, Lonnqvist J. A review on cognitive impairments in depressive and anxiety disorders with a focus on young adults. J Affect Disord. 2008;106(1–2):1–27. doi: 10.1016/j.jad.2007.06.006. [DOI] [PubMed] [Google Scholar]
- Collins SE, Spelman PJ. Associations of descriptive and reflective injunctive norms with risky college drinking. Psychology of Addictive Behaviors. 2013;27(4):1175. doi: 10.1037/a0032828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz JE, Emery RE, Turkheimer E. Peer network drinking predicts increased alcohol use from adolescence to early adulthood after controlling for genetic and shared environmental selection. Dev Psychol. 2012;48(5):1390–1402. doi: 10.1037/a0027515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Psychopathology associated with drinking and alcohol use disorders in the college and general adult populations. Drug and alcohol dependence. 2005;77(2):139–150. doi: 10.1016/j.drugalcdep.2004.07.012. [DOI] [PubMed] [Google Scholar]
- Dennhardt AA, Murphy JG. Associations between depression, distress tolerance, delay discounting, and alcohol-related problems in European American and African American college students. Psychology of Addictive Behaviors. 2011;25(4):595. doi: 10.1037/a0025807. [DOI] [PubMed] [Google Scholar]
- Festinger L. A theory of social comparison processes. Human relations. 1954;7(2):117–140. [Google Scholar]
- Fujimoto K, Chou CP, Valente TW. The network autocorrelation model using two-mode data: Affiliation exposure and potential bias in the autocorrelation parameter. Social networks. 2011;33(3):231–243. doi: 10.1016/j.socnet.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisner IM, Larimer ME, Neighbors C. The relationship among alcohol use, related problems, and symptoms of psychological distress: Gender as a moderator in a college sample. Addict Behav. 2004;29(5):843–848. doi: 10.1016/j.addbeh.2004.02.024. [DOI] [PubMed] [Google Scholar]
- Geisner IM, Neighbors C, Lee CM, Larimer ME. Evaluating personal alcohol feedback as a selective prevention for college students with depressed mood. Addict Behav. 2007;32(12):2776–2787. doi: 10.1016/j.addbeh.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gress-Smith JL, Roubinov DS, Andreotti C, Compas BE, Luecken LJ. Prevalence, severity and risk factors for depressive symptoms and insomnia in college undergraduates. Stress and Health. 2015;31(1):63–70. doi: 10.1002/smi.2509. [DOI] [PubMed] [Google Scholar]
- Hames JL, Hagan CR, Joiner TE. Interpersonal processes in depression. Annu Rev Clin Psychol. 2013;9:355–377. doi: 10.1146/annurev-clinpsy-050212-185553. [DOI] [PubMed] [Google Scholar]
- Hefner J, Eisenberg D. Social support and mental health among college students. Am J Orthopsychiatry. 2009;79(4):491–499. doi: 10.1037/a0016918. [DOI] [PubMed] [Google Scholar]
- Herman S, Archambeau OG, Deliramich AN, Kim BS, Chiu PH, Frueh BC. Depressive symptoms and mental health treatment in an ethnoracially diverse college student sample. Journal of American College Health. 2011;59(8):715–720. doi: 10.1080/07448481.2010.529625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. Journal of psychiatric research. 2013;47(3):391–400. doi: 10.1016/j.jpsychires.2012.11.015. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr, Alfano MS, Metalsky GI. When depression breeds contempt: reassurance seeking, self-esteem, and rejection of depressed college students by their roommates. J Abnorm Psychol. 1992;101(1):165–173. doi: 10.1037//0021-843x.101.1.165. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Hustad JT, Barnett NP, Strong DR, Borsari B. Validation of the 30-day version of the Brief Young Adult Alcohol Consequences Questionnaire for use in longitudinal studies. Journal of Studies on Alcohol and Drugs. 2008;69(4):611–615. doi: 10.15288/jsad.2008.69.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, Read JP. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The Brief Young Adult Alcohol Consequences Questionnaire. Alcoholism: Clinical and Experimental Research. 2005;29(7):1180–1189. doi: 10.1097/01.alc.0000171940.95813.a5. [DOI] [PubMed] [Google Scholar]
- Kenney SR, Jones RN, Barnett NP. Gender Differences in the Effect of Depressive Symptoms on Prospective Alcohol Expectancies, Coping Motives, and Alcohol Outcomes in the First Year of College. J Youth Adolesc. 2015;44(10):1884–1897. doi: 10.1007/s10964-015-0311-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, LaBrie JW. Use of protective behavioral strategies and reduced alcohol risk: examining the moderating effects of mental health, gender, and race. Psychology of Addictive Behaviors. 2013;27(4):997. doi: 10.1037/a0033262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, Lac A, Labrie JW, Hummer JF, Pham A. Mental health, sleep quality, drinking motives, and alcohol-related consequences: a path-analytic model. Journal of Studies on Alcohol and Drugs. 2013;74(6):841–851. doi: 10.15288/jsad.2013.74.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, Ott MQ, Meisel MK, Barnett NP. Alcohol perceptions and behavior in a residential peer social network. Addict Behav. 2017;64:143–147. doi: 10.1016/j.addbeh.2016.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. doi: 10.1097/01.mlr.0000093487.78664.3c. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, Lowe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JW, Monahan PO, Löwe B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clinical psychology review. 2005;25(7):841–861. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Stewart SH, Cooper ML. How stable is the motive–alcohol use link? A cross-national validation of the drinking motives questionnaire revised among adolescents from Switzerland, Canada, and the United States. Journal of Studies on Alcohol and Drugs. 2008;69(3):388–396. doi: 10.15288/jsad.2008.69.388. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Lopez N. Social anxiety among adolescents: linkages with peer relations and friendships. J Abnorm Child Psychol. 1998;26(2):83–94. doi: 10.1023/a:1022684520514. [DOI] [PubMed] [Google Scholar]
- Labrie JW, Kenney SR, Lac A. The use of protective behavioral strategies is related to reduced risk in heavy drinking college students with poorer mental and physical health. J Drug Educ. 2010;40(4):361–378. doi: 10.2190/DE.40.4.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latane B. The psychology of social impact. American psychologist. 1981;36(4):343. [Google Scholar]
- Lau-Barraco C, Linden AN. Drinking buddies: Who are they and when do they matter? Addict Res Theory. 2014;22(1):57–67. doi: 10.3109/16066359.2013.772585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden AN, Lau-Barraco C, Milletich RJ. The role of protective behavioral strategies and anxiety in problematic drinking among college students. Journal of Studies on Alcohol and Drugs. 2013;74(3):413–422. doi: 10.15288/jsad.2013.74.413. [DOI] [PubMed] [Google Scholar]
- Mahmoud JSR, Staten RT, Hall LA, Lennie TA. The relationship among young adult college students’ depression, anxiety, stress, demographics, life satisfaction, and coping styles. Issues in mental health nursing. 2012;33(3):149–156. doi: 10.3109/01612840.2011.632708. [DOI] [PubMed] [Google Scholar]
- Martens MP, Martin JL, Hatchett ES, Fowler RM, Fleming KM, Karakashian MA, Cimini MD. Protective behavioral strategies and the relationship between depressive symptoms and alcohol-related negative consequences among college students. Journal of counseling psychology. 2008;55(4):535. doi: 10.1037/a0013588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason MJ, Zaharakis N, Benotsch EG. Social networks, substance use, and mental health in college students. J Am Coll Health. 2014;62(7):470–477. doi: 10.1080/07448481.2014.923428. [DOI] [PubMed] [Google Scholar]
- McAlaney J, McMahon J. Normative beliefs, misperceptions, and heavy episodic drinking in a British student sample. Journal of Studies on Alcohol and Drugs. 2007;68(3):385–392. doi: 10.15288/jsad.2007.68.385. [DOI] [PubMed] [Google Scholar]
- Meier MH, Caspi A, Houts R, Slutske WS, Harrington H, Jackson KM, Moffitt TE. Prospective developmental subtypes of alcohol dependence from age 18 to 32 years: Implications for nosology, etiology, and intervention. Development and psychopathology. 2013;25(3):785–800. doi: 10.1017/S0954579413000175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meisel MK, Clifton AD, MacKillop J, Goodie AS. A social network analysis approach to alcohol use and co-occurring addictive behavior in young adults. Addict Behav. 2015;51:72–79. doi: 10.1016/j.addbeh.2015.07.009. [DOI] [PubMed] [Google Scholar]
- Miller BE, Miller M, Verhegge R, Linville H, Pumariega A. Alcohol misuse among college athletes: self-medication for psychiatric symptoms? J Drug Educ. 2002;32(1):41–52. doi: 10.2190/JDFM-AVAK-G9FV-0MYY. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Fossos N, Woods BA, Fabiano P, Sledge M, Frost D. Social anxiety as a moderator of the relationship between perceived norms and drinking. J Stud Alcohol Drugs. 2007;68(1):91–96. doi: 10.15288/jsad.2007.68.91. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Lee CM, Lewis MA, Fossos N, Larimer ME. Are social norms the best predictor of outcomes among heavy-drinking college students? Journal of Studies on Alcohol and Drugs. 2007;68(4):556–565. doi: 10.15288/jsad.2007.68.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIAAA. Drinking Levels Defined. 2017a Retrieved from https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking.
- NIAAA. What Is A Standard Drink? 2017b Retrieved from https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/what-standard-drink.
- Patrick ME, Schulenberg JE. How trajectories of reasons for alcohol use relate to trajectories of binge drinking: National panel data spanning late adolescence to early adulthood. Dev Psychol. 2011;47(2):311. doi: 10.1037/a0021939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson MR, Hustad JT. Personality and alcohol-related outcomes among mandated college students: Descriptive norms, injunctive norms, and college-related alcohol beliefs as mediators. Addict Behav. 2014;39(5):879–884. doi: 10.1016/j.addbeh.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson MR, Kite BA, Henson JM. Predictive effects of good self-control and poor regulation on alcohol-related outcomes: Do protective behavioral strategies mediate? Psychology of Addictive Behaviors. 2013;27(1):81. doi: 10.1037/a0028818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Miles JN, Hunter SB, Osilla KC, Ewing BA, D’Amico EJ. Perceived norms moderate the association between mental health symptoms and drinking outcomes among at-risk adolescents. J Stud Alcohol Drugs. 2013;74(5):736–745. doi: 10.15288/jsad.2013.74.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, Devine H. Relations between personality and drinking motives in young adults. Personality and individual differences. 2000;29(3):495–511. [Google Scholar]
- Terlecki MA, Buckner JD, Larimer ME, Copeland AL. Brief motivational intervention for college drinking: the synergistic impact of social anxiety and perceived drinking norms. Psychol Addict Behav. 2012;26(4):917–923. doi: 10.1037/a0027982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman ER. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. J Nerv Ment Dis. 2004;192(4):269–277. doi: 10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- White A, Hingson R. The Burden of Alcohol Use Excessive Alcohol Consumption and Related Consequences Among College Students. Alcohol Research-Current Reviews. 2013;35(2):201–218. [PMC free article] [PubMed] [Google Scholar]
- Zywiak WH, Longabaugh R, Wirtz PW. Decomposing the relationships between pretreatment social network characteristics and alcohol treatment outcome. Journal of studies on alcohol. 2002;63(1):114–121. [PubMed] [Google Scholar]


