Abstract
Background
Sexual dysfunction is remarkably prevalent amongst psychiatric patients than general population. This might be due to either the nature of the illness itself or the unwanted effect of the medication they are taking for the illness which limits the capability of forming interpersonal and sexual relationships. This issue is rarely raised in developing countries, and the aim of this study was to assess magnitude and factors contributing to sexual dysfunction among patients with Schizophrenia.
Method
Hospital based cross sectional study was conducted at Amanuel Mental Specialized Hospital from January to June 2017. The sample required for this study was determined by using single population proportion formula and the final sample size was 423; and systematic random sampling was used to select participants. We used Change in Sexual Functioning Questionnaire to measure sexual dysfunction. The collected data was cleaned, interred in to Epi data and transferred to SPSS version 20 for farther analysis. The OR with 95% CI was used to measure association and P-value < 0.05 was used as statistically significant.
Result
A total of 422 patients with Schizophrenia were involved in the study. The prevalence of General Sexual dysfunction was 82.7%; and in male and female patients the prevalence was 84.5 and 78.6% respectively. Marital status (Unmarried, Divorced and widowed, history of relapse and poor quality of life were associated significantly to global sexual dysfunction.
Conclusion
The magnitude of Sexual dysfunction was found to be high among patients with schizophrenia and it is associated with different factors like unmarried, divorced, widowed, relapse and poor quality of life. Treating physicians should be conscious to sexual dysfunction during evaluation and treatment of patients with Schizophrenia. Special attention should be given to single, divorced, widowed patients and patients with history of relapse to improve quality of life of this patients.
Keywords: Sexual dysfunction, Schizophrenia, Amanuel hospital
Background
Sexual life is a natural and complex component of human behaviors that is determined by many physiological and psychological factors. Sexual dysfunction is a public health issue which affects an estimate of 43% women and 31% men in US [1]. The commonest dysfunction among women is sexual desire dysfunction complained by around 30 % of women. The commonest dysfunctions among men are erectile dysfunction and premature ejaculation. Any problem in main area of sexual behavior; interest, arousal, orgasm/ejaculation and like can arise as the result of either pathophysiological or psychological mechanisms [2].
Sexual dysfunction is extremely prevailing in psychiatric patients than general population. This is related to either the nature of the illness itself (negative symptoms like avolition, anhedonia and blunted affect) or the unwanted effect of the medication they are taking for the illness (effect on prolactin secretion and obesity) which limits the capability of forming interpersonal and sexual relationships [1].
The peak age of onset of schizophrenia in both sexes is during the reproductive period. Consequently impaired sexual functioning among persons with schizophrenia can affect their ability to have a family, and, thus, to fulfill traditional social expectations [3]. The role of antipsychotic drugs in sexual functioning of people with schizophrenia is becoming a recent concern of researchers since this side-effect may decrease adherence to treatment, especially among males, because they are more concerned about sexual functioning than females) [4].
Sexual dysfunction has many impacts on patients with Schizophrenia. It has direct or indirect association with quality of life, adherence, difficulty to form and maintain family, and lastly may develop depression and suicidality [3, 5, 6].
Despite the importance and high prevalence of the problem, this patients do not inform the problem either due to feeling of discomfiture or for the reason that they do not view it as a treatable problem [6]. In other hand psychiatrists and other specialists significantly undervalue or even neglect the existence of the problem probably due to embarrassment of talking about sexual problems with patients, lack of time and viewing difficulties in this area as minor compared to psychotic symptoms. In spite of these realities there are limited or no researches conducted in this country regarding sexual dysfunction and its influence on patients with Schizophrenia. Therefore, this study aims to evaluate the prevalence of sexual dysfunction among patients with schizophrenia and see if there is any association between socio-demographic factors, different clinical factors like medication related factors, co-morbid physical or psychiatric conditions, and substance use and sexual dysfunction among patients with Schizophrenia.
Methods
Study design and study period
Institutional based cross sectional study was conducted from January to June 2017.
Study area
The study was conducted at Amanuel Mental Specialized Hospital (ASMH) located in the country’s capital, Addis Ababa. Amanuel mental specialized hospital is the only mental specialized hospital where patients mainly afflicted with severe mental illness, including schizophrenia, are treated. The hospital gives service for patients from all over the country. It has a case load of more than 10,000 patients per month and schizophrenia is the number one diagnosis, diagnosed in more than 60% of the patients visiting the hospital.
Population
All patients with Schizophrenia who are on follow up at AMSH are the source populations and people with Schizophrenia in the age group 18 & above who were on treatment at AMSH during the study period were study population.
Eligibility criteria
All patients with Schizophrenia in age group 18 and above were included in the study and the patients in exacerbation phase were excluded from the study.
Sample size
The minimum number of sample required for this study wasdetermined by using single population proportion formula and the final sample size for this study with 10% nonresponse rate was 423.
Sampling procedure
Systematic random sampling technique with interval of 11 was used to select the participants from 4885 patients with schizophrenia came for follow up during data collection period.
Study variables
The outcome variable for this study was Sexual Dysfunction. Socio-demographic factors, duration of the illness, duration on treatment, medication, dosage and frequency, comorbid known chronic medical illness, history of admission and relapse, adherence to drug, Quality of life, Suicide, Depression and history of substance use were explanatory variables for this study.
Instruments
The gold standard instrument which is Structured Clinical Interview for DSM- ΙѴ-TR axis Ι disorders (SCID) was used to confirm a diagnosis of Schizophrenia. Sexual dysfunction was measured by using Changes in Sexual Functioning Questionnaires (CSFQ-14). It has separate forms for female (CSFQ –F-C) and for Male (CSFQ-M-C) Clinical Version. It contains14 items and is used to assess the presence/absence of sexual dysfunction in study participants. All the 14 items should be answered on a five Likert scale to assess global sexual dysfunction. The score < =47 for male and < =41 for female indicates the presence of global sexual dysfunction. The tool can also measure the sexual dysfunction components: Pleasure (Item 1), Desire/frequency (Item 2 and 3), Desire/interest (Item 4, 5 and 6), Arousal/erection (Item 7, 8 and 9) and Orgasm/ejaculation (Item 11, 12 and 13) It has Cronbach’s α of 0.91 and 0.93 for male and female scales, respectively [7, 8]. WHOQOL-BREF was used to measure quality of life. This instrument is cross culturally validated and currently in use in different languages [9]. PHQ-9 was used to measure depression in patients with schizophrenia. This instrument has sensitivity of 86% and specificity of 67%in diagnosing depression [10]. Eight –item Morisky medication adherence Scale was used to measure medication adherence. It is valid and reliable with Cronbach’s α of 83%; and, sensitivity and specificity of 93 and 53% respectively [11]. The English version of the instruments was translated to local language and back retranslated to English by language professionals and psychiatrists.
Data quality control
17 masters level mental health students were hired for data collection and two masters level mental health professionals were hired to supervise the data collectors. The data collectors were given a two days training on questionnaire and way of assessment. Pre-test was conducted 15 days before the start of actual data collection to know the time needed to complete one questionnaire and to know whether the questionnaire used is understandable to the study participants or not. The data collected during the pre-test was not included in the final analysis.
Data processing and analysis
Data was coded and entered to Epi data and transferred to Statistical Package for Social Sciences version 20 (SPSS-20) for further analysis. Descriptive statistical analysis was used to estimate the frequencies and percentages of the variables. Bivariate and multivariate logistic regression analysis was used to see the association between outcome and explanatory variables. The strength of the association was measured by odds ratio with 95% CI and P-value less than 0.05 was considered as statistically significant.
Ethical consideration
Ethical clearance was obtained from Amanuel Mental Specialized Hospital Ethical Review Committee. The Four Item Abbreviated Mental Test (AMT4) was used to measure the capacity of the patient to give consent. Then the purpose, importance and confidentiality of the information gathered was explained to each of the competent participant before the start of interview. Participants were also informed that they will never get any benefit because of participation in the study and no harm on them if they would not agree to participate or withdraw from participation during the data collection process. Finally, their willingness to be involved in the study was asked and written consent was obtained.
At the time of data collection the investigator, supervisor and data collectors followed ‘code of ethics’ and obeyed the rules & regulations of the hospital. Participant’s privacy was kept strictly at the time of data collection.
Result
A total of 422 patients with schizophrenia participated on the study with response rate of 99.76%. Among the participants 290(68.7%) were male and 132(31.3%) were female in gender. The mean age of the participants is 35.46 with ± 9.25 standard deviation. Majority of the participants 353(83.6%) were from urban area. The most frequently prescribed antipsychotic drug is chlorpromazine 184(43.6%) followed by Resperidone 111 (26.3%) (Fig. 1). Amitriptyline is the most frequently prescribed drug among the medications ordered for other comorbid psychiatric conditions 42(41.6%) followed by Fluoxetine 27(26.7%) (Fig. 2). Most of the participants take their medications once in twenty four hours (Table 1). Among the study participants, 23(5.5%) were found to have at least one comorbid other medical illness. The most frequently occurring chronic medical illness in patients with Schizophrenia is Diabetes Mellitus 10(2.4%) followed by Tuber Closes (TB) 8(1.9%) (Fig. 3). Among the substance users 71(16.8%) use cigarette and khat users were 71(16.8%) (Khat and Cigarette are equally consumed) (Fig. 4). The median score of duration of the illness is 7 years with inter quartile range of 6, and the median score of duration on treatment is 6 years with inter quartile range of 10. The median score for frequency of admission is 1 with inter quartile range of 1, and the median score for frequency of relapse is 2 with inter quartile range of 2. The mean score of Quality of Life of the participants is 60.59 with standard deviation of ± 9.43 (Table 1).
Fig. 1.
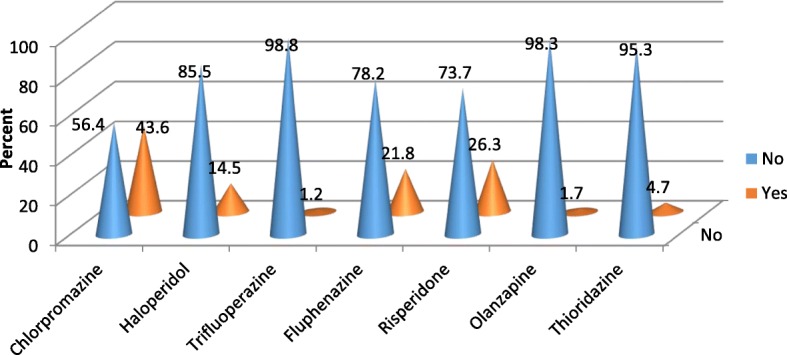
Antipsychotic Medications prescribed for the participants
Fig. 2.
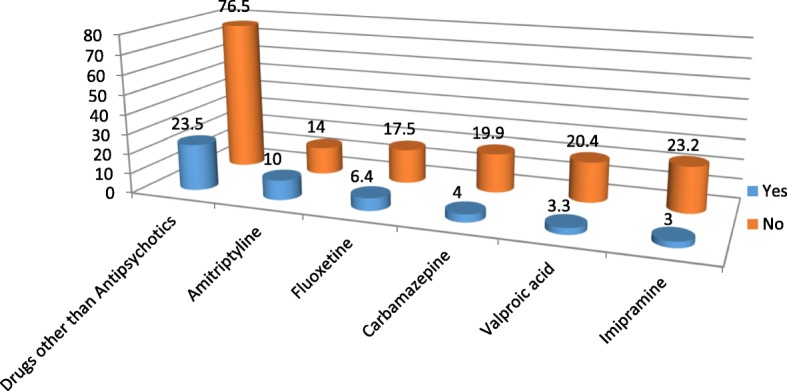
Medications prescribed for comorbid psychiatric problems
Table 1.
Distribution of participants by socio-demographic factors and clinical factors
| No. | Variables | Variables category | Frequency (422) | Percentage (100%) |
|---|---|---|---|---|
| 1 | Age | 18–24 | 35 | 8.3 |
| 25–34 | 174 | 41.2 | ||
| 35–44 | 150 | 35.5 | ||
| > = 45 | 63 | 14.9 | ||
| 2 | Sex | Female | 132 | 31.3 |
| Male | 290 | 68.7 | ||
| 3 | Marital Status | Married | 154 | 36.5 |
| Single | 224 | 53.1 | ||
| Divorced and Widowed | 44 | 10.4 | ||
| 4 | Ethnicity | Oromo | 140 | 33.2 |
| Amhara | 126 | 29.9 | ||
| Gurage | 98 | 23.2 | ||
| Others* | 58 | 13.7 | ||
| 5 | Religion | Orthodox | 228 | 54 |
| Protestant | 79 | 18.7 | ||
| Muslim | 115 | 27.3 | ||
| 6 | Educational Status | No formal education | 31 | 7.3 |
| Primary school | 137 | 32.5 | ||
| High School | 164 | 38.9 | ||
| Diploma | 46 | 10.9 | ||
| Degree and above | 44 | 10.4 | ||
| 7 | Occupation | Private | 135 | 32 |
| Governmental | 42 | 11.1 | ||
| Unemployed | 142 | 33.6 | ||
| Others(House wife, Daily labourers) | 98 | 23.2 | ||
| 8 | Residence | Urban | 353 | 83.6 |
| Rural | 69 | 16.4 | ||
| 9 | Frequency of Chlorpromazine per day | Once/day | 149 | 81.0 |
| > = 2 | 35 | 19 | ||
| 10 | Frequency of Haloperidol per day | Once/day | 46 | 75.4 |
| > = 2 | 15 | 24.6 | ||
| 11 | Frequency of Trifluoperazine per day | Once/day | 3 | 60 |
| > = 2/day | 2 | 40 | ||
| 12 | Frequency of Fluphenazineper day | Once/month | 91 | 98.9 |
| > = 2/month | 1 | 1.1 | ||
| 13 | Frequency of Resperidone per day | Once/day | 71 | 64.5 |
| > = 2/day | 39 | 35.5 | ||
| 14 | Frequency of Olanzapine per day | Once/day | 5 | 62.5 |
| > = 2/day | 2 | 37.5 | ||
| 15 | Frequency of Thioridazine per day | Once/day | 20 | 100 |
| > = 2/day | 0 | 0 | ||
| 16 | Duration of the illness | <=5 years | 174 | 41.2 |
| 6-10 years | 119 | 28.2 | ||
| > = 11 years | 129 | 30.6 | ||
| 17 | Duration on treatment | <=5 years | 207 | 49.1 |
| 6-10 years | 103 | 24.4 | ||
| > = 11 years | 112 | 26.5 | ||
| 18 | Admission | No | 254 | 60.2 |
| Yes | 168 | 39.8 | ||
| 19 | Number of admission | <=1 | 96 | 57.1 |
| > = 2 | 72 | 42.9 | ||
| 20 | Relapse | No | 226 | 53.6 |
| Yes | 196 | 46.4 | ||
| 21 | Number of relapse | <=1 | 96 | 49 |
| > = 2 | 100 | 51 | ||
| 22 | Depression | No | 346 | 82 |
| Yes | 76 | 18 | ||
| 23 | Non-Adherence | No | 203 | 48.1 |
| Yes | 219 | 51.9 | ||
| 24 | Poor Quality of life | No | 217 | 51.4 |
| Yes | 205 | 48.6 | ||
| Yes | 0 | 0 | ||
| 25 | Suicidal Ideation | No | 373 | 88.4 |
| Yes | 49 | 11.6 | ||
| 26 | Suicidal Attempt | No | 406 | 96.2 |
| Yes | 16 | 3.8 |
Fig. 3.
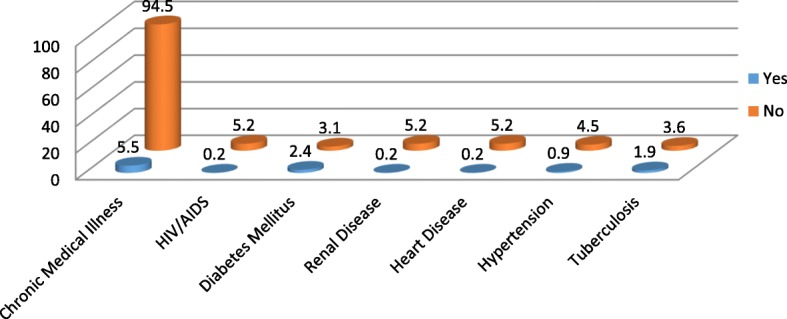
Magnitude of Chronic Medical Illness among Patients with Schizophrenia
Fig. 4.
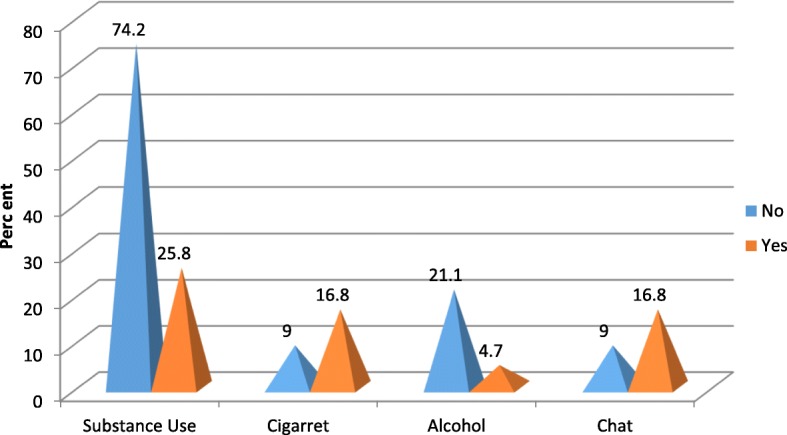
Magnitude of Substance Use among Patients with Schizophrenia
Prevalence of sexual dysfunction among patients with schizophrenia
The prevalence of General sexual dysfunction among the study participants was 349(82.7%) with 95% confidence interval of (78.9, 86.3). The overall sexual dysfunction among male participants was 246(84.5%) with 95% confidence interval of (80.3, 88.7) and it was 103(78.6%) with 95% confidence interval of (71, 84.7) in female Schizophrenic patients (Fig. 5). Erectile dysfunction 277(95.2%) is highly prevalent followed by pleasure dysfunction 274(94.2%) in male participants (Fig. 6). In female participants who had sexual dysfunction the most prevalent sexual dysfunction was pleasure dysfunction 125(94.7%) followed by arousal/excitement dysfunction 123(93.2%) (Fig. 7).
Fig. 5.
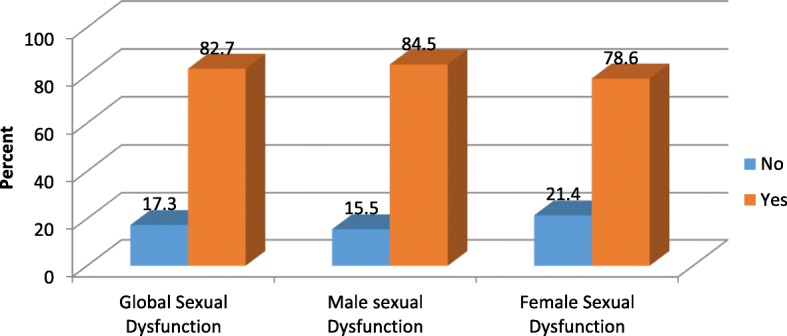
Global sexual Dysfunction and sexual Dysfunction across Male and Female participants
Fig. 6.
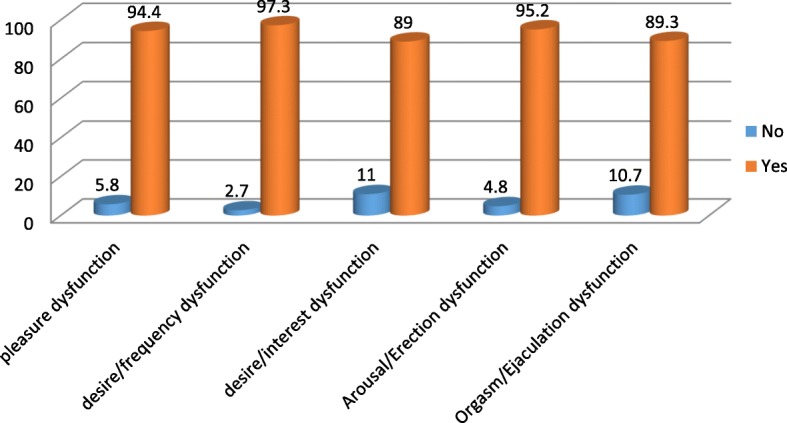
Components of Sexual Dysfunction among male participants
Fig. 7.
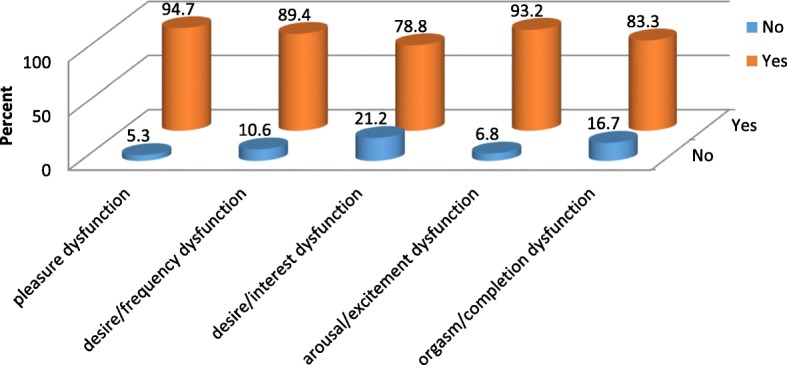
Components of Sexual Dysfunction among Female Participants
Bivariate and multivariate analysis
After bivariate logistic regression analysis, five variables (Marital status, Resperidone use, Relapse, Depression and Quality of life) met the requirement to proceed to multivariate logistic regression analysis. After multivariate analysis, marital status, history of relapse, and quality of life were found to be significantly associated with global sexual dysfunction. Compared to the married ones, being single, [aOR 4.19, 95% CI (2.30, 7.64)], and being divorced [aOR 2.86, 95% CI (1.03, 7.90)] were significantly associated with General sexual dysfunction. History of relapse, [aOR 2.21, 95% CI (1.25, 3.91)], and poor quality of life, [aOR 5.57, 95% CI (2.79, 11.09)] were also significantly associated with General sexual dysfunction at p-value< 0.05 (Table 2).
Table 2.
Factors Associated With Sexual Dysfunction Among Patients With Schizophrenia At Amanuel Mental Specialized Hospital/2017
| Explanatory variables | Variables category |
Sexual Dysfunction | Bivariate and Multivariate Analysis | P-Value | ||
|---|---|---|---|---|---|---|
| Absent | Present | Bivariate Analysis | Multivariate Analysis | |||
| COR (95% CI) | aOR (95% CI) | |||||
| Marital Status | Married | 44 | 110 | 1:00 | 1:00 | |
| Single | 23 | 201 | 3.49(2.01,6.10) | 4.19(2.30,7.64) | 0.000 | |
| Divorced and Widowed |
6 | 38 | 2.53(1.00,6.6.42) | 2.86(1.03,7.90) | 0.043 | |
| Resperidone | No | 62 | 249 | 1.00 | 1.00 | |
| Yes | 11 | 100 | 2.264(1.15,4.48) | 1.69(0.82,3.51) | ||
| Relapse | No | 30 | 196 | |||
| Yes | 43 | 153 | 1.84(1.10,3.06) | 2.21(1.25,3.91) | 0.007 | |
| Depression | No | 67 | 279 | 1.00 | 1.00 | |
| Yes | 6 | 70 | 2.80(1.17,6.72) | 1.49(0.58,3.83) | ||
| Quality of life | Good | 60 | 157 | 1.00 | 1.00 | |
| Poor | 13 | 192 | 5.64(2.99,10.66) | 5.57(2.79,11.09) | 0.000 | |
Discussion
This study found that magnitude of General sexual dysfunction, and sexual dysfunction across male and female patients with Schizophrenia is extremely high and needs immediate intervention. The prevalence of general sexual dysfunction among patients with Schizophrenia in this study is supported by the comparative study conducted in Egypt on paranoid and non-paranoid schizophrenic patients in which Prevalence of general sexual dysfunction was 80% in patients with paranoid schizophrenia and 86.7% in patients with non-paranoid Schizophrenia [7]. The magnitude of general sexual dysfunction in this study is very high when compared to the study conducted in Britain and Iran which was 45 and 31.1% respectively [12, 13]. The reason for this significant difference may be explained by socio-cultural difference and difference in measurement instrument to assess sexual dysfunction. In case of the study conducted in Britain, they used Sexual Functioning Questionnaire (SFQ) to assess sexual dysfunction, and the study conducted in Iran used Arizona Sexual Experience Scale (ASEX) [12, 13].
Prevalence of sexual dysfunction among male Schizophrenic patients in our study which is 84.5% in lines with the study conducted by Macdonald in which the magnitude of sexual dysfunction in male Schizophrenic patients is 82% [14]. Magnitude of sexual dysfunction among female schizophrenic patients in this study which is 78.6% is lower than that of Macdonald in which prevalence of sexual dysfunction among female schizophrenic patients is 92%, and is higher than that of USA and Turkey in which prevalence of female sexual dysfunction is 59 and 68% respectively [14–16]. The reason for the discrepancy is probably due to difference in culture and living style which may differ in different countries and population. Difference in measurement tool to assess sexual dysfunction in this particular population is also possible reason for observed difference. In case of USA they used the Global Impression of Sexual Function (GISF) and in Turkey they used Arizona Sexual Experience Scale (ASEX) to assess sexual dysfunction [15, 16]. Another possible reason for the difference might be criterion used to include the participants in the study. The study conducted in USA included patients who were on conventional antipsychotics and Resperidone where as in our study all schizophrenic patients on any antipsychotic medication were included in the study [16]. Sample size difference across the studies is also possible reason for the discrepancy. Among the factors hypothesized to be contributing factors to sexual dysfunction, unmarried participants were four times more likely to develop sexual dysfunction compared to married participants and Divorced and widowed participants were three times more likely to develop sexual dysfunction compared to married participants. This finding is supported by the study conducted in Nigeria [17]. The possible reason for the association is that the infrequent sexual activity in single and divorced/widowed individuals probably decreases frequency of sexual desire. Having history of relapse exposes two times more to sexual dysfunction compared to the patients without history of relapse. This may be explained by, the more the relapse is frequent the more the illness becomes deteriorated with predomination of negative symptoms of Schizophrenia which potentially affect sexual performance. The need for higher doses of antipsychotics in case of frequent relapse is also another possible reason for this significant association. In this study sexual dysfunction is found to be highly associated with poor quality of life. This result is supported by the study conducted by Olfson and Kandrakonda S [18, 19]. This may be due to the fact that an inproper sexual functioning may affect maintaining a satisfying intimate relationship which is the major component of Quality of life.
Conclusion
Prevalence of Sexual dysfunction is found to be high among patients with Schizophrenia and it needs special attention. The current prevalence of general sexual dysfunction among Schizophrenic patients in our study is high. Regarding sexual dysfunction across sex, male and female sexual dysfunction was also high. Among the hypothesized factors to be risk factors for sexual dysfunction, marital status (single, divorced, widowed), history of relapse and poor quality of life were significantly associated with sexual dysfunction.
Recommendation
To Amanuel Mental Specialized Hospital.
All Psychiatrists and mental health specialists have to be conscious to sexual dysfunction which is highly prevalent among the patients they are treating, and all patients who are on follow up at this hospital for the case of Schizophrenia should be screened for sexual dysfunction. The overall treatment and care delivered by the hospital should focus on improving quality of life by diagnosing and managing sexual dysfunction properly, rather than focusing only on decreasing the symptom of the illness. Special consideration should be given to a patients with history of relapse, single, widowed and divorced.
Acknowledgements
We are grateful to the data collectors and supervisors for their unreserved effort. Our gratitude also goes to Amanuel Mental Specialized Hospital for funding this study. Finally we are grateful to the study participants for their patience.
Funding
Funding for this study was provided by Amanuel Mental Specialized Hospital.
Availability of data and materials
The datasets used and/or analysed during the current study are available from thecorresponding author on reasonable request.
Abbreviations
- AMSH
Amanuel Mental Specialized Hospital
- CSFQ
Changes in Sexual Functioning Questionnaires
- PHQ-9
Patients Health Questionnaire nine
- SD
Sexual Dysfunction
- SMI
Severe Mental Illness
- SPSS
Statistical Package of Social Science
- USA
United States of America
- WHOQOL
World Health Organization Quality of Life
Authors’ contributions
TF involved in designing and coordinating overall progress of the study; KH, DA1, GH and DA2 equally contributed in the design of the study, performed the statistical analyses and critically revised the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Ethical clearance was obtained from Amanuel Mental Specialized Hospital Ethical Review Committee. The Four Item Abbreviated Mental Test (AMT4) was used to measure the capacity of the patient to give consent. Then the purpose, importance and confidentiality of the information gathered was explained to each of the competent participant before the start of interview. Their willingness to participate in the study was asked and written consent was obtained. Participant’s privacy was kept strictly at the time of data collection.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tolesa Fanta, Email: tole.fanta@gmail.com.
Kibrom Haile, Email: kibromhaile4@gmail.com.
Dessie Abebaw, Email: dessieabebaw96@gmail.com.
Dawit Assefa, Email: dawitnov@yahoo.com.
Getahun Hibdye, Email: guble2003@yahoo.com.
References
- 1.Zemishlany Z, Weizman A. The impact of mental illness on sexual dysfunction. InSexual Dysfunction 2008 Apr 8 (Vol. 29, pp. 89–106). Karger Publishers. [DOI] [PubMed]
- 2.Baggaley M. Sexual dysfunction in schizophrenia: focus on recent evidence. Hum Psychopharmacol Clin Exp. 2008;23(3):201–209. doi: 10.1002/hup.924. [DOI] [PubMed] [Google Scholar]
- 3.Kelly DL, Conley RR. Sexuality and schizophrenia: a review. Schizophr Bull. 2004;30(4):767–779. doi: 10.1093/oxfordjournals.schbul.a007130. [DOI] [PubMed] [Google Scholar]
- 4.Hanssens L, L'Italien G, Loze JY, Marcus RN, Pans M, Kerselaers W. The effect of antipsychotic medication on sexual function and serum prolactin levels in community-treated schizophrenic patients: results from the schizophrenia trial of aripiprazole (STAR) study ( NCT00237913) BMC psychiatry. 2008;8(1):1. doi: 10.1186/1471-244X-8-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kikuchi T, Iwamoto K, Sasada K, Aleksic B, Yoshida K, Ozaki N. Sexual dysfunction and hyperprolactinemia in Japanese schizophrenic patients taking antipsychotics. Prog Neuro-Psychopharmacol Biol Psychiatry. 2012;37(1):26–32. doi: 10.1016/j.pnpbp.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 6.Hashem A.H., Abd El-Gawad T., Ezzat M., Assal A., Goueily T. and El Rakhawy M. A comparative study of sexual function in paranoid versus non-paranoid schizophrenic patients and its relation to serum prolactin Level.Current psychiatry. Vol 13. No. 2. July 2006.
- 7.Maria Paz Garcia-Portilla, MD, PhD et al. Psychometric properties of the Spanish version of the changes in sexual functioning questionnaire short-form (CSFQ-14) in patients with severe mental disorders. International Society for Sexual Medicine J Sex Med 2011;8:1371–1382.. [DOI] [PubMed]
- 8.Liu-Seifert H, Kinon BJ, Tennant CJ, Sniadecki J, Volavka J. Sexual dysfunction in patients with schizophrenia treated with conventional antipsychotics or risperidone. Neuropsychiatr Dis Treat. 2009;5:47–54. doi: 10.2147/NDT.S4766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oyekanmi AK, Adelufosi AO, Abayomi O, Adebowale TO. Demographic and clinical correlates of sexual dysfunction among Nigerian male outpatients on conventional antipsychotic medications. BMC research notes. 2012;5(1):1. doi: 10.1186/1756-0500-5-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olfson M, Uttaro T, Carson WH, Tafesse E. Male sexual dysfunction and quality of life in schizophrenia. J Clin psychiatry. 2005;66(3):331–338. doi: 10.4088/JCP.v66n0309. [DOI] [PubMed] [Google Scholar]
- 11.Kandrakonda S, Jally MR, Kesava Reddy SR, Miryala G. Prevalence of sexual dysfunction in patients with mental illness receiving psychotropic medication. AP J Psychol Med. 2014;15(2):235–239. [Google Scholar]
- 12.CLAYTON ELMaAH. Reliability and construct validity of the changes in sexual functioning questionnaire short-form (CSFQ-14):. Journal of Sex & Marital Therapy,. 2006;32:43–52. Departments of Psychiatric Medicine & Health Evaluation Sciences, University of Virginia, Charlottesville, Virginia, USA. [DOI] [PubMed]
- 13.WHO. WHOQOL, user manual, division of mental health and prevention of substance abuse. Geneva, Switzerland.. 1998.
- 14.Gelaye B, et al. Validity of the patient health Questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 2013 December 15;210(2) 10.1016/j.psychres.2013.07.015. [DOI] [PMC free article] [PubMed]
- 15.Morisky E, Ang A, Wood M. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10:348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 16.Smith S, O'KEANE VE, Murray R. Sexual dysfunction in patients taking conventional antipsychotic medication. Br J Psychiatry. 2002;181(1):49–55. doi: 10.1192/bjp.181.1.49. [DOI] [PubMed] [Google Scholar]
- 17.Ahmadzadeh G, Shahin A. Sexual dysfunctions in the patients hospitalized in psychiatric wards compared to other specialized wards in Isfahan, Iran, in 2012. Advanced biomedical research. 2015;4–225. [DOI] [PMC free article] [PubMed]
- 18.Macdonald S, Halliday J, MacEwan T, Sharkey V, Farrington S, Wall S, McCreadie RG. Nithsdale schizophrenia surveys 24: sexual dysfunction. Br J Psychiatry. 2003;182(1):50–56. doi: 10.1192/bjp.182.1.50. [DOI] [PubMed] [Google Scholar]
- 19.Hocaoglu C, Celik FH, Kandemir G, Guveli H, Bahceci B. Sexual dysfunction in outpatients with schizophrenia in Turkey: a cross-sectional study. Shanghai Arch Psychiatry. 2014;26(6):347–356. doi: 10.11919/j.issn.1002-0829.214101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from thecorresponding author on reasonable request.


