Abstract
Objective
We aimed to investigate symptom trajectory of attention-deficit hyperactivity disorder (ADHD) in Korean school-age children.
Methods
Four hundred fifty six elementary school children were enrolled when they were in 1st grade and assessed once per year until 4th grade. Symptom severity was assessed by parents using the Korean version of the ADHD rating scale (K-ARS). High-risk was defined as a K-ARS score >18; 377, 325, and 284 children participated in the subsequent assessments. Symptom trajectory was analyzed using a mixed-model approach consistent with the longitudinal nature of the present study including missing data.
Results
K-ARS scores demonstrated significant main effects of time (F=35.33; p<0.001), sex (F=20.77; p<0.001), and first-year high-risk group (F=240.90; p<0.001). It also demonstrated a significant time×first-year high-risk group interaction effect (F=38.14; p<0.001), but not a time×sex interaction effect.
Conclusion
K-ARS scores demonstrated a tendency to decline with aging. Individuals in the high-risk group demonstrated earlier declining tendency than those in the non-high risk group. Although total K-ARS scores differed significantly between the sexes at all assessments, the declining pattern between both sexes did not differ significantly. Further studies including larger sample sizes, diagnostic interviews, and complete data sets are needed to confirm findings of the present study.
Keywords: ADHD, Symptom trajectory, School-age children
INTRODUCTION
Attention-deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder with a symptom complex that includes hyperactivity, impulsivity, and inattention. The age-of-onset criterion for ADHD required the presence of symptoms before 7 years of age until publication of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) to avoid misdiagnosing children who exhibit ADHD symptoms as school stress [1,2] and was extended to 12 years of age in DSM-5 [3]. However, most ADHD children exhibit onset during early school age, from six to nine years of age [4,5].
The prevalence of ADHD has been reported to be approximately 5% of children in most cultures [3]. Polanczyk et al. [6] reported that there were no regional differences in the prevalence of ADHD. The prevalence ratio of males to females in school-age children has been reported to be 2:1 to 3:1 [2,3]. Whereas males are more likely to be hyperactive and impulsive, females are more likely to exhibit features of inattentiveness [3,7].
The symptom severity of ADHD has been reported to decline with aging [8,9]. The persistence rate of childhood ADHD symptoms to adulthood have been reported to be approximately 50%, and previous studies reported the prevalence of adulthood ADHD to be approximately 2.5% [3,10,11]. However, declining trends of symptom severity differ according to symptom domain. Whereas hyperactivity and impulsivity improve early in childhood, the period and rate of improvement in inattention symptoms appear later and are lower than for hyperactivity/impulsivity [12]. Differences in improvement according to symptom domain may lead to a change in ADHD subtype with aging [13,14].
Studies investigating the characteristics of Korean ADHD patients have reported similar patterns to international studies. Despite methodological differences, some studies have reported the prevalence of ADHD in the Korean population to be 5.9% to 8.5% [15-17]. Regarding age of onset, Byun et al. [18] reported that 75% of ADHD patients were diagnosed as schoolage children. The prevalence ratio of males to females in the Korean population was also reported to be similar to international studies. For example, Kim et al. [15] reported a prevalence ratio of 2.4:1, favoring males; similarly, Song [19] reported a ratio of 3:1, favoring males.
School-age children comprise the most prevalent group diagnosed and experience the most symptom changes. Information regarding ADHD symptom trajectory is important for clinicians and parents to design treatment plans and predict prognosis. There have been some normative studies investigating the use of an ADHD rating scale for the general population of Korean elementary school children [20,21]. Despite some inconsistent findings, a slightly decreasing tendency in symptom severity scores with aging could be inferred from the results of those studies. However, the samples examined in previous studies were cross-sectional, and no longitudinal follow-up of the participants was performed. Moreover, those studies did not divide their samples into high-risk and nonhigh-risk ADHD groups. Thus, we cannot confirm the changing aspects of individual ADHD symptoms according to highrisk and non-high-risk ADHD groups. To our knowledge, there have been no studies investigating the symptom trajectory of ADHD in the Korean school-age population using a longitudinal follow-up sample. Therefore, the present study investigated the symptom trajectory of ADHD according to symptom subdomains in a longitudinal assessment of school-age children in Korea.
METHODS
Participants
The present study included 456 elementary school students who participated in an ongoing longitudinal study investigating the correlation between environmental toxins and neurodevelopmental disorders. The present study was conducted in Cheonan, a medium-size city in South Korea with a mix of urban and rural areas. Students from three elementary schools participated in this study. Two schools were located in an urban area and the other was in a rural area. The participants were enrolled when they were in 1st grade of elementary school and assessed every year from 2013 to 2016. Each assessment was performed between March and June of each year. A total of 456 students participated in the first assessment and 245 (53.7%) were boys. Among this cohort, 377, 325, and 284 students were assessed in subsequent years, respectively. All participants and their parents were informed of the purpose of the study and provided informed written consent. The study protocol was approved by the Institutional Review Board for Human Subjects at the Dankook University Hospital (IRB No. 2013-02-014).
Measurement
For the assessment of ADHD symptom severity, the Korean version of the ADHD rating scale (i.e., K-ARS) was used. The ADHD rating scale was developed by Dupaul [22] to assess ADHD symptom severity. It consists of 18 items and is scored using a 4-point Likert scale. Nine items reflect inattentiveness, and 9 reflect hyperactivity and impulsivity. Its total score range is between 0 and 54. The K-ARS used in this study was validated by So et al. [23] The Cronbach’s alpha values of the K-ARS used in the present study were 0.932, 0.909, 0.901, and 0.915 for the assessment in each year.
Statistical analysis
Demographic variables and K-ARS score differences between sexes were analyzed using the independent t-test, chisquared test, and Fisher’s exact test. Inclusion in the high-risk group for each assessment was defined as a total K-ARS score >18 [15]. To remain consistent with the longitudinal nature of the study, a linear mixed model, including missing and available data, was used to analyze yearly changes in ADHD symptom severity. To examine changes in ADHD symptom severity in the high-risk group, children who were categorized as high-risk in the first-year assessment were categorized into the first-year high-risk group and analyzed longitudinally. Time, sex, and first-year high-risk group were included as the main effect variables, and time×sex and time×first-year high-risk group were included as interaction-effect variables in a single mixed model. Statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA) for Windows (Microsoft Corporation, Redmond, WA, USA).
RESULTS
Demographics
The number of boys who were assessed each year was 245, 202, 171, and 144. The mean age of the participants in each year was 6.88, 7.73, 8.56, and 9.67 years, respectively (Table 1). The ratio of high-risk group to total participants was 6.8% to 1.8%, and had a declining trend. The ratio of males to females in the high-risk group was significantly higher for males in the first year (χ2=9.69; p=0.002), but not in the second (χ2=2.07; p=0.150), third (χ2=3.21; p=0.073) or fourth [p>0.999 (Fisher’s exact test)] year.
Table 1.
Demographics and K-ARS scores of total participants at each assessment
| Year | 2013 | 2014 | 2015 | 2016 |
|---|---|---|---|---|
| Total (N) | 456 | 377 | 325 | 284 |
| Age, mean (SD) | 6.88 (0.30) | 7.73 (0.58) | 8.56 (0.56) | 9.67 (0.53) |
| Male, N (%) | 245 (53.7) | 202 (53.6) | 171 (52.6) | 144 (50.7) |
| High-risk group, N (%) | 31 (6.8) | 17 (3.7) | 13 (2.9) | 8 (1.8) |
| Male, N (%) | 25 (80.6) | 12 (70.6) | 10 (76.9) | 4 (50.0) |
| Total K-ARS score | ||||
| Mean (SD) | 6.60 (7.11) | 6.63 (6.33) | 5.90 (5.72) | 4.63 (5.71) |
| Median (IQR) | 4 (2–9) | 5 (2–10) | 4 (1–9) | 3 (1–7) |
| Hyperactivity/impulsivity | ||||
| Mean (SD) | 2.77 (3.54) | 2.63 (3.08) | 2.21 (2.67) | 1.63 (2.54) |
| Median (IQR) | 1 (0–4) | 2 (0–4) | 1 (0–3) | 1 (0–2) |
| Inattention | ||||
| Mean (SD) | 3.83 (3.95) | 4.02 (3.73) | 3.69 (3.48) | 3.00 (3.54) |
| Median (IQR) | 3 (1–5) | 3 (1–6) | 3 (1–6) | 2 (0–5) |
SD: standard deviation, IQR: interquartile range, K-ARS: Korean version of the ADHD rating scale
Sex differences in K-ARS scores
Total K-ARS scores and hyperactivity and inattentive subscales in boys were significantly higher than in girls at every assessment (Table 2 and Figure 1).
Table 2.
Sex differences of K-ARS scores at each assessment
| Year (Ages) | Score | Male | Female | Statistics | p |
|---|---|---|---|---|---|
| 2013 (6 years) | Total K-ARS score, mean (SD) | 8.07 (7.79) | 4.90 (5.80) | 4.97 | <0.001* |
| Hyperactivity/impulsivity score, mean (SD) | 3.49 (3.93) | 1.94 (2.80) | 4.87 | <0.001* | |
| inattention score, mean (SD) | 4.58 (4.26) | 2.95 (3.37) | 4.57 | <0.001* | |
| 2014 (7 years) | Total K-ARS score, mean (SD) | 7.83 (6.82) | 5.24 (5.42) | 4.10 | <0.001* |
| Hyperactivity/impulsivity score, mean (SD) | 3.23 (3.45) | 1.93 (2.40) | 4.31 | <0.001* | |
| inattention score, mean (SD) | 4.62 (3.93) | 3.31 (3.38) | 3.48 | 0.001* | |
| 2015 (8 years) | Total K-ARS score, mean (SD) | 6.96 (5.78) | 4.73 (5.44) | 3.56 | <0.001* |
| Hyperactivity/impulsivity score, mean (SD) | 2.62 (2.74) | 1.76 (2.52) | 2.97 | 0.003* | |
| inattention score, mean (SD) | 4.34 (3.48) | 2.98 (3.35) | 3.56 | <0.001* | |
| 2016 (9 years) | Total K-ARS score, mean (SD) | 5.71 (5.61) | 3.52 (5.62) | 3.29 | 0.001* |
| Hyperactivity/impulsivity score, mean (SD) | 2.08 (2.49) | 1.17 (2.53) | 3.09 | 0.002* | |
| inattention score, mean (SD) | 3.63 (3.49) | 2.35 (3.50) | 3.08 | 0.002* |
p<0.01.
K-ARS: Korean version of the ADHD rating scale
Figure 1.
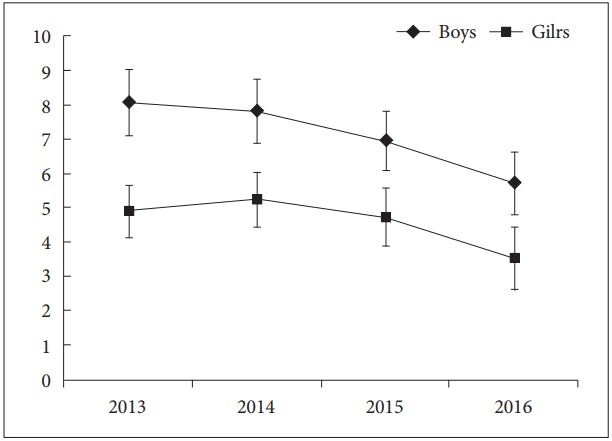
Changes of total K-ARS scores at each assessment in boys and girls (mean). K-ARS: Korean version of the ADHD rating scale, CI: confidence interval.
Changes in K-ARS scores over time
K-ARS scores of all participants had significant main effects of time, sex, and group (first-year high-risk versus nonhigh-risk group) (Figures 1, 2, and Table 3). Whereas the time×sex interaction effect was not significant (Figure 1 and Table 3), there was a significant time×group interaction effect (Figure 2 and Table 3).
Figure 2.
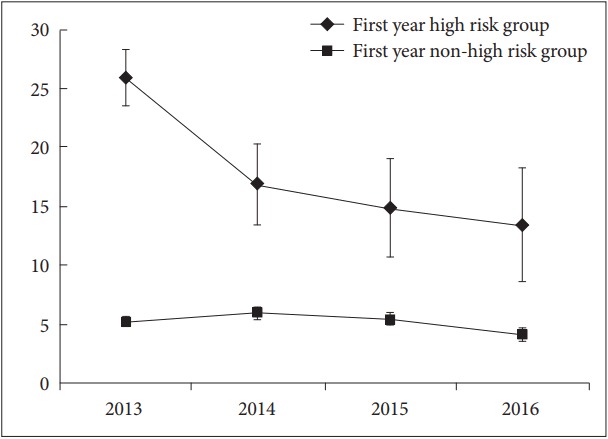
Changes of total K-ARS scores at each assessment between first year high-risk and non high-risk groups (mean). K-ARS: Korean version of the ADHD rating scale, CI: confidence interval.
Table 3.
Linear mixed model of total K-ARS scores at each assessment according to sex and first-year high risk group
| Effect | F-ratio | p |
|---|---|---|
| Time | 35.33 | <0.001* |
| Sex | 20.77 | <0.001* |
| High risk | 240.90 | <0.001* |
| Time×sex | 0.20 | 0.898 |
| Time×high risk | 38.14 | <0.001* |
High risk: first year high-risk group.
p<0.01.
K-ARS: Korean version of the ADHD rating scale
In the post-hoc analysis involving all participants, K-ARS scores among the first, second, and third years were not significantly different. However, K-ARS scores in the fourth year was significantly lower than the first, second, and third years (p<0.001, <0.001 and <0.001, respectively).
However, the post-hoc analysis according to group (i.e., first-year high-risk versus first-year non-high risk) demonstrated a different tendency in score change. K-ARS scores of second-year assessment in the first-year non-high-risk group was higher than the scores of the first-year assessment (p=0.012), and the scores of only the fourth-year assessment were significantly lower than the first-year assessment (p=0.042). In contrast, K-ARS scores of the first-year high-risk group decreased earlier than the scores of the first-year non-high-risk group. The K-ARS scores of second-year assessment in the first-year high-risk group were significantly lower than the first-year assessment (p<0.001), and there were no significant differences among second-, third- and fourth-year scores.
DISCUSSION
The present study investigated changes in ADHD symptom severity in school-age children using longitudinal assessments over a four-year period. Despite studies investigating the prevalence and symptom severity of ADHD in Korea [15,17], there have been no reports describing changes in ADHD symptom severity in Korean school-age children. Most ADHD children receive a diagnosis and start medication treatment during the preschool or elementary school years [5]. The Korean Food and Drug Administration has approved all ADHD medications prescribed from 6 years of age. Song and Shin [24] reported that approximately 97% of ADHD diagnoses were made after 6 years of age, and approximately 60% of ADHD diagnoses were made from 6 to 12 years of age. Therefore, symptom trajectory in school-age children is important information in designing treatment plans and predicting prognosis in children initially diagnosed with ADHD.
In the present study, the prevalence of high-risk ADHD at the first assessment was 6.8%. This finding is comparable with previous studies investigating the prevalence of ADHD in Korean school-age children, which reported a prevalence of 5.9% to 8.5% [16,17]. However, the prevalence of high-risk ADHD demonstrated steep declining trends, with 3.7, 2.9, and 1.8% at the second-, third-, and fourth-year assessments, respectively. It may be inferred that the prevalence of ADHD decreased substantially due to the declining tendency of ADHD symptom severity with aging [9]. Nevertheless, we should be cautious when interpreting these prevalence data because 5, 13, and 14 participants among the 31 in the first-year high-risk group were missed at the second-, third-, and fourth-year assessments. Although previous studies reported a declining tendency of ADHD symptom severity with aging, another Korean study reported similar prevalence rates in children 7 to 11 years of age [15].
Total K-ARS scores, and hyperactivity/impulsivity and inattention subscales in the total participants were significantly higher in boys than girls at every assessment. Additionally, the prevalence of high-risk group was significantly higher in boys than girls. These findings are consistent with previous reports of a high prevalence ratio of males to females [3]. Although the K-ARS scores in boys were higher than in girls, the K-ARS total scores in girls also demonstrated a declining pattern similar to boys.
In the present study, K-ARS scores in all participants indicated the significant age-dependent decline in tendency. These findings are consistent with previous studies that reported an age-dependent, declining trend of ADHD symptom severity [9]. In particular, children demonstrated significantly decreased K-ARS scores when they were 10 years of age (4th grade of elementary school). This finding is consistent with a previous study that reported normative data from the original ARS by DuPaul et al. [25] That study reported mean ARS scores of 18.76 and 15.28 in 8- to 10-, and 11- to 13-year-old boys, respectively.
Previous Korean studies of K-ARS normative data reported a relatively inconsistent pattern of K-ARS scores. Whereas Jang et al. [20] reported a slightly declining tendency of K-ARS scores with aging, Kim et al. [21] did not report the declining tendency of the scores with aging. However, both of the studies may not reflect the changing tendency of ADHD symptom severity exactly because they were not longitudinal studies involving the same participants.
The high-risk group also demonstrated a significantly declining tendency with age in K-ARS scores. However, the high-risk group demonstrated an earlier declining pattern of ADHD symptom severity than the non-high risk group, which may result in the steep decline in the prevalence rate of the high-risk group with aging. Whereas the K-ARS scores of the first-year non-high risk group decreased only in the fourth year, those of first-year high-risk group decreased from the second year. The average age of ADHD symptom alleviation in school-age children is important information for clinicians to design treatment plans that also accommodate the interests of parents.
Although the present study investigated the period of alleviation of ADHD symptoms in high-risk and non-high risk groups, our study had many missing data points and small sample size in the ADHD high-risk group. Therefore, additional longitudinal studies involving larger sample sizes and fewer missing data points are needed to determine more precise estimates of symptom trajectory in ADHD, and to confirm the findings of our study.
This study had several limitations that should be addressed. Our assessment was limited to a parent-rating scale and clinicians did not perform structured diagnostic interviews, which limits interpretation of the results because the diagnosis was not confirmed. Furthermore, we did not obtain information regarding treatment history for ADHD. This may also limit the interpretation of our results because the treatment of ADHD could affect symptom severity. However, treatment effect may not be as significant given that the treatment incidence of ADHD in Korea is low [26]. Further studies including diagnostic interviews and more information about treatment history are needed to examine the precise symptom trajectory of ADHD in a Korean sample population. Despite these limitations, the significance of the present study is highlighted because it is the first to report ADHD symptom trajectory in early school-age children in a Korean population, and provides clinicians and parents with important information about the period of ADHD symptom severity alleviation.
Acknowledgments
This study was financially supported by the Ministry of Environment, Republic of Korea.
REFERENCES
- 1.Polanczyk G, Caspi A, Houts R, Kollins SH, Rohde LA, Moffitt TE. Implications of extending the ADHD age-of-onset criterion to age 12: results from a prospectively studied birth cohort. J Am Acad Child Adolesc Psychiatry. 2010;49:210–216. [PubMed] [Google Scholar]
- 2.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Text Revision. 4th Ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 3.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. (Fifth Edition) Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 4.Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustun TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 2007;20:359–364. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 6.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942–948. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 7.Hasson R, Fine JG. Gender differences among children with ADHD on continuous performance tests: a meta-analytic review. J Atten Disord. 2012;16:190–198. doi: 10.1177/1087054711427398. [DOI] [PubMed] [Google Scholar]
- 8.Hill JC, Schoener EP. Age-dependent decline of attention deficit hyperactivity disorder. Am J Psychiatry. 1996;153:1143–1146. doi: 10.1176/ajp.153.9.1143. [DOI] [PubMed] [Google Scholar]
- 9.Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36:159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- 10.Faraone SV, Biederman J. What is the prevalence of adult ADHD? Results of a population screen of 966 adults. J Atten Disord. 2005;9:384–391. doi: 10.1177/1087054705281478. [DOI] [PubMed] [Google Scholar]
- 11.Kessler RC, Green JG, Adler LA, Barkley RA, Chatterji S, Faraone SV, et al. Structure and diagnosis of adult attention-deficit/hyperactivity disorder: analysis of expanded symptom criteria from the Adult ADHD Clinical Diagnostic Scale. Arch Gen Psychiatry. 2010;67:1168–1178. doi: 10.1001/archgenpsychiatry.2010.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biederman J, Mick E, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: impact of remission definition and symptom type. Am J Psychiatry. 2000;157:816–818. doi: 10.1176/appi.ajp.157.5.816. [DOI] [PubMed] [Google Scholar]
- 13.Hurtig T, Ebeling H, Taanila A, Miettunen J, Smalley SL, McGough JJ, et al. ADHD symptoms and subtypes: relationship between childhood and adolescent symptoms. J Am Acad Child Adolesc Psychiatry. 2007;46:1605–1613. doi: 10.1097/chi.0b013e318157517a. [DOI] [PubMed] [Google Scholar]
- 14.Lahey BB, Pelham WE, Loney J, Lee SS, Willcutt E. Instability of the DSM-IV subtypes of ADHD from preschool through elementary school. Arch Gen Psychiatry. 2005;62:896–902. doi: 10.1001/archpsyc.62.8.896. [DOI] [PubMed] [Google Scholar]
- 15.Kim MJ, Park I, Lim MH, Paik KC, Cho S, Kwon HJ, et al. Prevalence of attention-deficit/hyperactivity disorder and its comorbidity among Korean children in a community population. J Korean Med Sci. 2017;32:401–406. doi: 10.3346/jkms.2017.32.3.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park S, Kim BN, Cho SC, Kim JW, Shin MS, Yoo HJ. Prevalence, correlates, and comorbidities of DSM-IV psychiatric disorders in children in Seoul, Korea. Asia Pac J Public Health. 2015;27:NP1942–NP1951. doi: 10.1177/1010539513475656. [DOI] [PubMed] [Google Scholar]
- 17.Yang SJ, Cheong S, Hong SD. Prevalence and correlates of attention deficit hyperactivity disorder: school-based mental health services in Seoul. J Korean Neuropsychiatr Assoc. 2006;45:69–76. [Google Scholar]
- 18.Byun H, Yang J, Lee M, Jang W, Yang JW, Kim JH, et al. Psychiatric comorbidity in Korean children and adolescents with attention-deficit hyperactivity disorder: psychopathology according to subtype. Yonsei Med J. 2006;47:113–121. doi: 10.3349/ymj.2006.47.1.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Song YJ. Estimated Prevalence of ADHD Symptoms and Relationships among ADHD Symptoms, Environmental Variables, and Peer Relationships in Elementary School Students. Asian J Educ. 2014;15:189–217. [Google Scholar]
- 20.Jang SJ, Suh DS, Byun HJ. Normative study of the K-ARS (Korean ADHD Rating Scale) for parents. J Korean Acad Child Adolesc Psychiatry. 2007;18:38–48. [Google Scholar]
- 21.Kim YS, So YK, Noh JS, Choi NK, Kim SJ, Koh YJ. Normative data on the Korean ADHD Rating Scales (K-ARS) for parents and teacher. J Korean Neuropsychiatr Assoc. 2003;42:352–359. [Google Scholar]
- 22.DuPaul GJ. Parent and teacher ratings of ADHD symptoms: psychometric properties in a community-based sample. J Clin Child Psychol. 1991;20:245–253. [Google Scholar]
- 23.So YK, Noh JS, Kim YS, Ko SG, Koh YJ. The reliability and validity of Korean parent and teacher ADHD rating scale. J Korean Neuropsychiatr Assoc. 2002;41:283–289. [Google Scholar]
- 24.Song I, Shin JY. Prescribing patterns for attention deficit hyperactivity disorder medications among children and adolescents in Korea, 2007-2011. Epidemiol Health. 2016;38:e2016045. doi: 10.4178/epih.e2016045. doi: 10.4178/epih.e2016045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DuPaul GJ, Power TJ, Anastopoulos AD, Reid R, McGoey KE, Ikeda MJ. Teacher ratings of attention deficit hyperactivity disorder symptoms: factor structure and normative data. Psychol Assess. 1997;9:436–444. doi: 10.1037/pas0000166. [DOI] [PubMed] [Google Scholar]
- 26.Hong M, Kwack YS, Joung YS, Lee SI, Kim B, Sohn SH, et al. Nationwide rate of attention-deficit hyperactivity disorder diagnosis and pharmacotherapy in Korea in 2008-2011. Asia Pac Psychiatry. 2014;6:379–385. doi: 10.1111/appy.12154. [DOI] [PubMed] [Google Scholar]


