Abstract
A 91-year-old African American man was admitted with sudden onset diffuse abdominal pain which radiated to the right flank. CT of the abdomen with contrast showed diverticula in the jejunum with adjacent inflammation and microperforation that was contained. Conservative therapy similar to colonic diverticulitis was effective. Although rare, our case highlights the importance of having an early and high suspicion for jejunal diverticulitis when patients present with non-specific abdominal symptoms in order to avoid perforation.
Keywords: small intestine, medical management, gastroenterology
Background
Diverticulosis of the large bowel is seen in greater than 65% of patients by the age of 85 years and diverticulitis is seen in 15%–20% of those who have diverticulosis.1 Small bowel diverticulitis is not seen as commonly as colonic diverticulitis.2 It usually presents at an age over 40 and may coexist with colonic diverticulum. Small bowel diverticulum occurs more often in the duodenum than in the jejunum or ileum and is mostly an incidental finding on imaging.3 We are presenting a case of an elderly man in his 90s who presented with acute small bowel diverticulitis and was successfully treated with management similar to colonic diverticulitis.
Case presentation
The patient is a 91-year-old man without any significant past medical history who presented with an acute onset of abdominal pain for 2 days. The abdominal pain was present in all four quadrants and radiated to the right flank area. The pain was associated with nausea, vomiting, decrease in appetite and abdominal distention. He denied fevers, chills, diarrhoea, constipation, haematochezia, melanotic stools, weight loss and prior similar episodes. At presentation, he was haemodynamically stable with positive physical examination findings of mild distress due to pain and diffuse abdominal distention with tenderness to palpation in the flanks bilaterally.
Investigations
He was found to have macrocytic anaemia with a haemoglobin level of 12.8 g/dL and a lactate level of 3.0 mmol/L. There was no evidence of leucocytosis and faecal occult blood test was negative. An abdominal X-ray was initially performed for the possibility of an acute abdomen. Although there was no evidence of free air, several non-specific non-dilated air-filled loops of bowel were identified. Distal descending colon and sigmoid colon appeared to have narrowed lumen without a discrete transition point. Subsequently, a CT of the abdomen and pelvis was performed with oral and intravenous contrast that showed evidence of small bowel diverticula with inflammation and a contained microperforation (figure 1). Radiographic evidence of wall thickening of the distal gastric antrum, pylorus and proximal small bowel was attributed to inflammation of the jejunal diverticulum (figures 2 and 3). Large bowel appeared unremarkable.
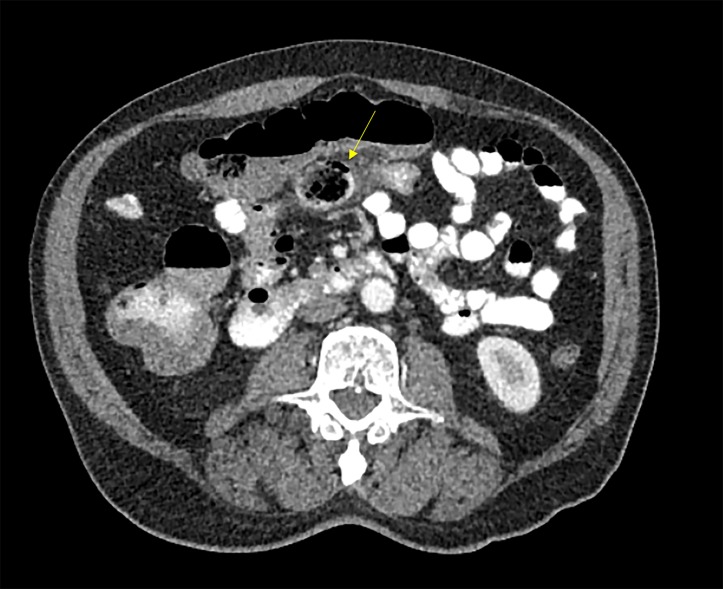
Figure 1.

Small air bubbles with adjacent inflammation and stranding suggesting microperforation secondary to diverticula in the region.
Figure 2.
Sagittal view: Air entry in a linear direction into the wall suggesting an out pouching in the proximal small bowel, specifically the jejunoileum.
Figure 3.
Axial view: Air entry in a linear direction into the wall suggesting an outpouching in the proximal small bowel, specifically the jejunoileum.
Treatment
The patient was given nothing per os, started on intravenous hydration and was treated with intravenous ciprofloxacin and metronidazole.
Outcome and follow-up
Clinically, the patient improved as pain was well controlled and regular diet was tolerated within 2 days. Currently, the patient is doing well without any complications.
Discussion
Small bowel diverticulum are mostly acquired and asymptomatic. Approximately 42% of documented cases were found incidentally via radiographic imaging. The incidence of small bowel diverticulitis diagnosed via autopsy is 0.6%–2.3% and it is more commonly located in the duodenum rather than jejunum or ileum.4 The overall incidence of jejunal diverticulum may be underestimated as most diverticulum present with symptoms when obstruction or malabsorption occur with underlying inflammation or when complications such as abscess or perforation happen.5 6 Our patient was atypical in that he presented with abdominal symptoms and at a much later age than most reported cases.
Acquired diverticula in the jejunoileum arise from the mucosal and submucosal layers and protrude through the muscular layer next to the mesenteric vessels.1 Although the origin of jejunal diverticula has not been well defined, some of the aetiologies proposed include overgrowth of the natural gut bacteria in the setting of altered peristaltic motion in the small intestine and high intraluminal pressures.5 6 Jejunoileal diverticula may exist as an independent lesion or with multiple diverticula in the colon, duodenum and in the urinary bladder. Patients with jejunoileal diverticulosis were found to be four times more likely to experience acute complications when compared with duodenal diverticulosis.7 Up to 10% of the patients may experience complications ranging from fistula formation to perforation and peritonitis with eighteen times higher likelihood of perforation than duodenal diverticulitis.8 The small bowel diverticulum in this case was found in the proximal jejunum. It was diagnosed early enough in this elderly patient before the microperforation was able to expand and lead to a poorer prognosis.
The most common diagnostic imaging modalities include CT abdomen and pelvis, endoscopic retrograde cholangiopancreatography and CT enteroclysis.4 Radiographic findings for small bowel diverticula are found to be similar to colonic diverticula. Based on prior case reports, acute diverticulitis in the small bowel has been identified with evidence of asymmetrical wall thickening next to the diverticulum surrounded by fat stranding. Other non-specific radiographic findings that have been previously documented include gas or stool filled mass with surrounding oedema and/or free air in the mesentery rather than in the peritoneum.5 Our patient’s radiographic findings were consistent with prior published cases.8 Although most cases to date were diagnosed retrospectively on CT studies, magnetic resonance enterography is the newly emerging mode of imaging for small bowel diverticulitis.
Currently, there is limited clinical literature to establish standard guidelines for small bowel diverticulitis management. Most case reports with uncomplicated jejunal diverticulitis showed effective conservative approaches similar to colonic diverticulitis management including bowel rest, intravenous antibiotics and initial parenteral nutrition with slow advancement to oral nutrition.9 Saberski et al10 described a rare case of uncomplicated jejunal diverticulitis that was diagnosed and managed with a laparoscopic wash out followed by intravenous antibiotics and bowel rest. The patient in this case did not require a segmental resection.5 Overall, recent literature has shown that it may take up to 72 hours for perforation to occur; therefore, it may be reasonable to initially monitor improvement in patients for up to 3 days with conservative management.11
Initial exploratory laparoscopic and open surgical interventions were reported in cases with symptoms of acute abdomen secondary to unknown aetiology and in patients whose symptoms mimicked acute appendicitis. Emergent surgical management has been described in cases where patients initially presented with complications including abscess formation and/or perforation and in those who failed conservative approaches.11 Surgery usually involves resection of the diseased segment and primary anastomosis thereafter.5 12 While the study by Schloericke et al supported tangential resection of diverticulum when there is only one present, solely removing the diverticulum has also been shown to increase the risk of sepsis and mortality overall.6 13 Our patient improved clinically with conservative measures.
In conclusion, small bowel diverticulitis is a rare entity which warrants early diagnosis. It is important for clinicians to distinguish it from Crohn’s disease and neoplasms which may have similar radiographic findings. The expanding literature regarding small bowel diverticulitis may help establish comprehensive guidelines soon.
Learning points.
Small bowel diverticulitis, specifically jejunal diverticulitis, is a rare entity that is currently managed based on case reports.
As jejunal diverticulitis can be highly lethal due to a high risk of perforation, early diagnosis is crucial.
Early imaging assists in identifying complications including gangrene, bleeding, obstruction and perforation.
Our case supports the initial use of conservative management similar to colonic diverticulitis, even in the setting of perforation.
Footnotes
Contributors: DCK and MS have contributed in the authorship of the article. DN authored the radiographic imaging portion. KR has provided patient management and edited the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Shahedi K, Fuller G, Bolus R, et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol 2013;11:1609–13. 10.1016/j.cgh.2013.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferreira-Aparicio FE, Gutiérrez-Vega R, Gálvez-Molina Y, et al. Diverticular disease of the small bowel. Case Rep Gastroenterol 2012;6:668–76. 10.1159/000343598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu CY, Chang WH, Lin SC, et al. Analysis of clinical manifestations of symptomatic acquired jejunoileal diverticular disease. World J Gastroenterol 2005;11:5557–60. 10.3748/wjg.v11.i35.5557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar D, Meenakshi M. Complicated jejunal diverticulitis with unusual presentation. Radiol Case Rep 2018;13:58–64. 10.1016/j.radcr.2017.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jerraya H, Gouta EL, Safta AB, et al. Jejunal diverticulitis: a challenging diagnosis. J Gastrointest Dig Syst 2015;5. [Google Scholar]
- 6.Schloericke E, Zimmermann MS, Hoffmann M, et al. Complicated jejunal diverticulitis: a challenging diagnosis and difficult therapy. Saudi J Gastroenterol 2012;18:122–8. 10.4103/1319-3767.93816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Graña L, Pedraja I, Mendez R, et al. Jejuno-ileal diverticulitis with localized perforation: CT and US findings. Eur J Radiol 2009;71:318–23. 10.1016/j.ejrad.2008.04.023 [DOI] [PubMed] [Google Scholar]
- 8.Hoeffel C, Crema MD, Belkacem A, et al. Multi-detector row CT: spectrum of diseases involving the ileocecal area. Radiographics 2006;26:1373–90. 10.1148/rg.265045191 [DOI] [PubMed] [Google Scholar]
- 9.Costa Simões V, Santos B, Magalhães S, et al. Perforated duodenal diverticulum: Surgical treatment and literature review. Int J Surg Case Rep 2014;5:547–50. 10.1016/j.ijscr.2014.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saberski E, Novitsky YW. Laparoscopic diagnosis and management of an acute jejunal diverticulitis. Surg Laparosc Endosc Percutan Tech 2012;22:e18–e20. 10.1097/SLE.0b013e31823c9ba6 [DOI] [PubMed] [Google Scholar]
- 11.Halgas B, Peirce G, Davis K, et al. Jejunal diverticulitis, an unusual cause of a surgical abdomen. Ann Emerg Surg 2017;2:1015. [Google Scholar]
- 12.Cantao CA, Feitosa MR, Godinho M, et al. Jejunal diverticulitis as a cause of acute abdomen. J Coloproct 2015. [Google Scholar]
- 13.Johnson KN, Fankhauser GT, Chapital AB, et al. Emergency management of complicated jejunal diverticulosis. Am Surg 2014;80:600–3. [PubMed] [Google Scholar]