Abstract
The national nursing shortage translates into a gap in home nursing care available to children with complex, chronic medical conditions and their family caregivers receiving palliative care consultations. A total of 38 home health nursing surveys were completed by families receiving pediatric palliative care consultation services at a freestanding children's hospital in the Midwest. The gap in the average number of nursing hours allotted versus received was 40 h/wk per family, primarily during evening hours. Parents missed an average of 23 hours of employment per week to provide hands-on nursing care at home, ranking stress regarding personal employment due to nursing shortage at 6.2/10. Families invested an average of 10 h/mo searching for additional nursing coverage and often resorted to utilizing more than 6 different home nurse coverage personnel per month. Families reported multiple delays to hospital discharges (mean, 15 days per delay) due to inability to find home nursing coverage. Respiratory technology and lack of Medicaid coverage (P < .02) correlated with the gap in home nursing access. This study examines how the pediatric home nursing shortage translates into a lived experience for families with children with complex medical conditions receiving palliative care.
KEY WORDS: home health, pediatric nursing, pediatric palliative care
Although attentiveness toward the national nursing shortage has focused on the burden to hospital infrastructures and clinical care flow,1 the daily, lived experiential impact of the home nursing shortage on children and families receiving palliative care consultation matters.2,3 The field of pediatric palliative care is an approach to pediatric medical care that encompasses the total care of not only a child with a life-impacting illness but also the family of that child.4 Children who qualify for palliative care consultations include any child diagnosed as having a complex or significantly life-impacting diagnosis. Examples of conditions for which pediatric palliative care teams receive consultations include genetic conditions anticipated to result in pediatric death, a relapsed cancer diagnosis, or a complex congenital heart condition anticipated to require multiple surgeries. Palliative care teams help children and families achieve quality-of-life goals.5 Because of the complex needs of patients receiving pediatric palliative care consultation services, pediatric patients ideally meet the palliative care team at time of diagnosis for early integration of palliative care in the child's comprehensive care plan.6 Quality palliative care services include not only complex symptom management, but also caring for the domains of psychosocial support, transitions-of-care navigation, and community function.7,8 The home nursing shortage results in measurable indirect and direct costs, as well as an immeasurable and yet profound psychosocial toll on children receiving palliative care consultations and their families. The home nursing shortage directly impacts quality of life for children with complex medical needs and their families.
Many children with complex medical conditions (particularly those children who are technology dependent on tracheotomies or feeding devices) undergo extended hospital stays while awaiting home nursing access for safe discharge from the inpatient setting.9,10 A study from Great Britain clarified how the home nursing shortage resulted in significant delays in hospital discharge for 15 children (mean duration, 513 days per child over the child's lifetime [range, 14-1460 days]).11 In locations where home nurses with pediatric expertise are not available for children or families, these children often then move into long-term-care facilities or grow up in an inpatient hospital setting.12
The national demand for nurses continues to exponentially rise; in the decade between 2014 and 2024, the RN workforce demand is expected to increase by 16% in the United States.13 Even with creative and incentivized nursing educational tracks,14 there is concern whether the nursing training pipeline is positioned to meet the rising need for nurses over time, particularly home care nurses.15 The mean age of the current nurse faculty force in the study team's state is 54 years, with retirement on the horizon for many of these nursing teachers.16 Within the study team's Midwestern region, nursing schools are unable to accept all qualified applicants because of funding and space.7 These challenges are not unique to the study setting; the nation needs more than 1 million new nurses by the year 2024.11 The demand for nurses to care for the aging baby-boomer generation is great, with the demand greater still for qualified, trained pediatric nurses able to care for children with complex medical needs in the home setting. The staff shortage is worse in pediatric home health nursing work than all other nursing fields,17,18 particularly when considering the training expertise, comfort with care complexity, and scope of practice required for nurses caring for children in the home setting.19
The devotion of home nurses often stems more from a “richly rewarding” and deeply rooted relational commitment to a child and family rather than a financial incentive to do the work.20 Home health nurses receive a similar hourly salary when compared with inpatient nurses, but they receive fewer incentives and fewer opportunities for professional growth accompanied by adjusted compensation.2,3 Nationwide, the salary range for nurses in the home health industry ranges from $52 000 to $65 000 (with a mean annual salary of $48 000 in the study team's state).21 Time and travel investments factor into the personnel gap, as home nurses serving rural communities report spending extended time commuting from their own residence to the child's home and then driving between children's houses.22 Not all companies reimburse transportation time or mileage.19
The current home nursing shortage translates into a burden of care and lack of respite for families of children with chronic complex conditions receiving palliative care services.23 Families caring for children with life-limiting diagnosis and complex care needs without home nursing support describe lack of sleep, loss of family member employment, and social morbidity to include reduced family incomes, marital impact, and social isolation.24 The purpose of this study was to investigate the way that the nursing shortage translates into a time, economic, and psychosocial impact for family caregivers of children with complex medical conditions receiving palliative care services.
METHODS
Families of children receiving inpatient pediatric palliative care consultation during admission to the hospital were offered the opportunity to complete a survey on their perceived home health nursing needs and their experiences accessing home health nursing. The survey was offered in English or Spanish.
Survey questions were designed by a collaborative, interdisciplinary study team according to the Tailored Method of Survey Design.25 Most questions asked respondents to check “all that apply,” so multiple responses were available for each item. The survey instrument (available as Supplemental Digital Content 1, http://links.lww.com/JHPN/A17) consisted of 44 questions organized by topical sections. The majority of questions were multiple choice or single answer, with opportunity for free-text additional input. A 1- to 10-point Likert-type distress scale was utilized for the psychosocial stress inventory section. The survey was independently reviewed, piloted, revised, and repiloted by an interdisciplinary team (1 social worker, 1 palliative care nurse case manager, 1 pediatric palliative care nurse practitioner, and 2 pediatric palliative care physicians) prior to administration on SurveyMonkey (SurveyMonkey Inc, San Mateo, California). For those families with an e-mail address available (n = 51), a link to the SurveyMonkey questionnaire was sent in an introductory e-mail inviting participation in the survey with 2 reminder e-mails sent in 2-week intervals. For those families with nonfunctional e-mail addresses or without an e-mail address available (n = 9), a postal letter was sent with 1 reminder letter sent 2 weeks later.
Data were downloaded from SurveyMonkey into Excel (Microsoft Corp, Redmond, Washington) and SPSS (Version 22.0; IBM Corp, Armonk, New York) for analyses. The analyses were primarily grounded in tallying counts and proportion calculations. The study team utilized descriptive statistics and counts for categorical variable responses.
The study team investigated the impact of the child's level of technology and the child's insurance coverage on the child's experienced gap in nursing coverage. Fisher exact test was used to investigate the impact of level of technology on perceived nursing gap. The Freeman-Halton extension to Fisher exact test was used to investigate the impact of insurance coverage on perceived nursing gap (due to a failure of assumptions for the χ2 goodness-of-fit test).
The Office of Human Subjects Research Protections determined that the survey format and content qualified as exempt from full institutional review board review because of anonymity of responses and survey inclusion in a programmatic quality improvement initiative.
RESULTS
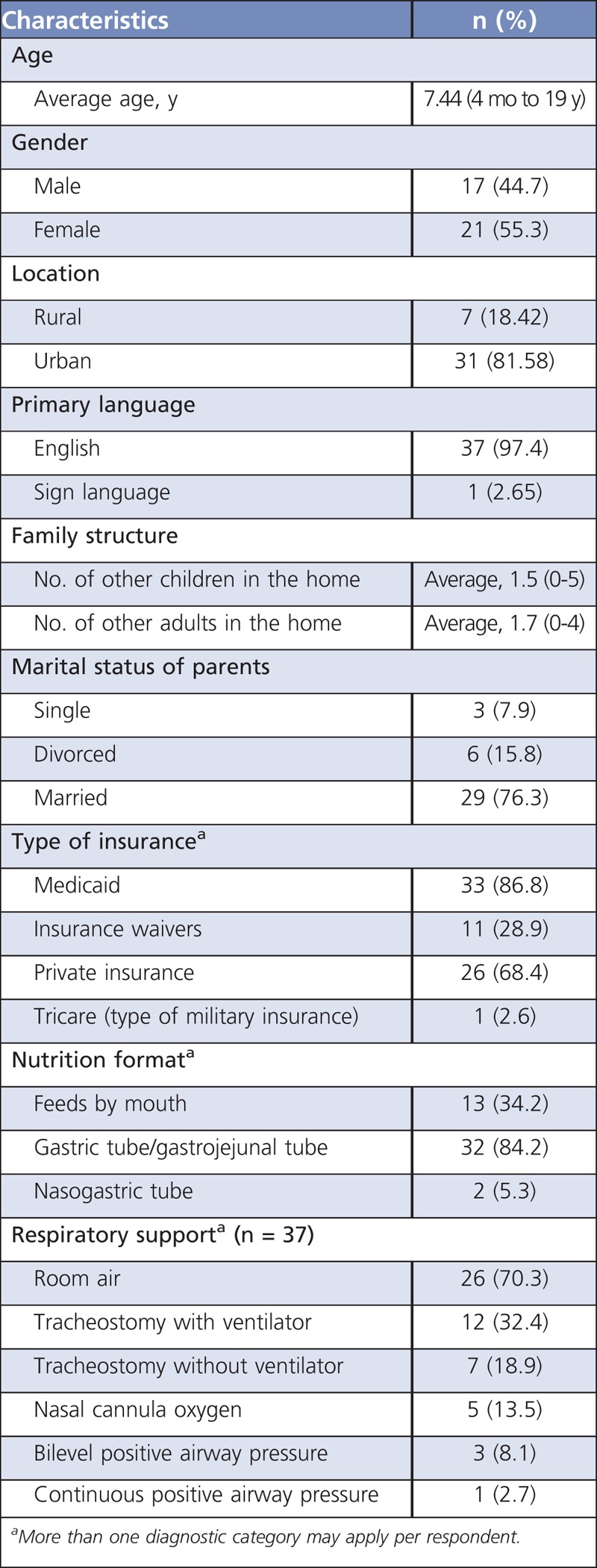
Response rate was 63% (38/60). The study population demographics are shown in the Table. Diagnosis included neurologic (n = 24), pulmonary (n = 21), cardiac (n = 18), genetic (n = 14), and oncologic (n = 7) conditions with coexisting conditions possible. The mean age of children and adolescents included in the study was 7.44 years (range, 4 months to 19 years). Although 3 surveys were completed in Spanish, English was listed as the primary home language by all respondents other than 1 family listing sign language.
TABLE.
Participant Demographics (n = 38)
Quantifying the Gap
Family members spent an average of 73.5 h/wk (range, 0-168 h/wk; median, 87.5 hours) providing their child the equivalent of hands-on nursing care. The majority of families perceived a need for more nursing hours for their child than they were receiving, but they were unable to access the necessary nursing staff (n = 21 [81%]). The mean number of approved home nursing hours was 103 h/wk (range, 5-168 hours; median, 56 hours). However, the average number of home nursing hours received per week was 63 hours (range, 0-120 hours; median, 9 hours). The gap in mean nursing hours allotted and nursing hours received was found to be 40 h/wk per family. This translates to an average of 160 hours of assigned home nursing hours not fulfilled per month per family due to home nursing shortage. The gap in nursing hours was noted to be reported 3 times more often during night shifts (confidence interval, 0.349-0.652) than day shifts (confidence interval, 0.058-0.273).
Specific to respite hours for families, the average number of assigned weekly respite hours was 15 hours, and yet the average number of received weekly respite hours was 7 hours. For children attending school, the average number of school nursing hours assigned was 18, and average received was 15 hours.
Correlating the Gap—Considering Level of Technology and Insurance Coverage
The odds that the parent of a patient dependent on respiratory technology (identified as any patient not on room air or nasal cannula) identified a gap in nursing hours received and assigned were 6.1 (1.4, 26.0) times greater than a person on room air. It is therefore 2.0 (1.1, 3.6) times more likely for the family of a child who requires respiratory support to identify a gap in nursing services than it is for the family of a child on room air to identify a gap. The P value for this comparison was .0184.
There was a statistically significant association between identifying a gap in nursing coverage and type of insurance (P = .02). Those families with private insurance only (without Medicaid as primary and without Medicaid as secondary) were more likely to experience a gap in the number of home nursing hours assigned versus the number of home nursing hours received (P = .01) as compared with those families with some form of Medicaid coverage.
Impact to Parental Employment
Of 73 parental members represented by the survey, 4 (5%) were employed inside the home full time; 5 (7%) were employed inside the home part time; 5 (7%) were employed outside the home part time; 14 (19%) were unemployed (19%); and 45 (62%) were employed outside the home full time. Survey respondents reported that at least 1 parental adult is missing an average of 23 hours of work per week in order to provide nursing care for the child (0-40 hours). More than half (n = 20 [54%]) of question responders report they do not receive waiver fund reimbursement for their care time.
Parental Search for Home Nursing Coverage
Families reported spending an average of 10 h/mo (range, 0-30 hours; median, 17 h/mo) completing paperwork and phone calls in order to coordinate home nursing coverage and to search for home nursing options. Families reported they have been searching for additional nursing coverage for a mean of 11.5 months (range, 0-60 months).
Parental Piecing Together Home Nursing Coverage
In order to find nurses to staff their child's care at home, it is required that multiple home health company nurses and private-duty nurses work with the same child in order to achieve coverage for the child's needs during the day and night hours. Families tend to have an average of 3 home health nurses (range, 0-10) and 3 private-duty nurses (range, 0-8) working in their home every month to piece together coverage for their child.
Perceived Psychosocial Stress Related to Home Nursing Shortage
The mean perceived parental stress level during the past month regarding home health nursing access was reported at 5.5 using a 1- to 10-point Likert-type stress range, with 10 being highest stress level. Stress level for ability to focus on parenting other children based on home health nursing access was reported as 4.9/10; that for adult couple unity based on home health nurse access was 5.3/10; and that for parent's own ability to work/pursue employment based on home health nursing access was 6.0/10.
Delays to Discharge
Delays to discharge from inpatient hospitalizations due not to biomedical reasons but due to lack of nursing coverage for their child outside the hospital were reported by 9 of 23 families (39%). These families remained in inpatient status for an average of 15 days beyond biomedical clearance for discharge because of the lack of home nursing access (range, 1-60 days; median, 20 days). Nine families reported that such delays had occurred multiple times in their child's lifetime.
DISCUSSION
This survey of families with children receiving palliative care for chronic, complex medical conditions reveals that families do not receive their allocated number of nursing hours. Families with children with complex chronic conditions carry the economic and time investment in caring for their children at home because of the nursing shortage. The survey results show a 40-hour average gap in home nursing care coverage for children receiving palliative care per week per family (equivalent to full-time employment hours). This translates into a 160-hour gap per month per family. Parents try to fill the gap in access to home nursing by engaging in proactive, time-consuming, extended searches for nursing care providers for their children to include up to 10 h/mo average search time for additional home nursing help via Internet, phone, and paperwork requests for additional nurse support. Parents describe a managerial role in trying to coordinate and organize nursing coverage as a second full-time job in addition to hands-on care.
Parents often take on the role of the nursing staff that they are missing, with an average of 73.5 h/wk of such care. While parenting surely involves hands-on care for a loved child, the concern is that serving as a child's full-time home nurse without respite from the medication administration, diapering, or technology supervision may cumulatively risk detracting parental energies from those special moments of memory making in a mom or dad role rather than a health provider role.26 The study team has personally witnessed families relocate from family farms, extended family member presence, and rural communities to move closer to the children's hospital in hopes of accessing the necessary home nursing hours for their loved child in a way that could maintain parental function and well-being. Sadly, a relocation to a more urban area does not actually translate into more home nursing hours as the pediatric home nursing shortage knows no geographic limit.
A recent analysis of the National Survey of Children With Special Health Care needs revealed foregone earnings for parents with children is in the upward of $11.6 billion nationally.27 This study revealed a removal of adults from the workforce, with at least 1 parental adult missing an average of 23 hours of work per week for hands-on nursing-type care for their child.7 In this survey, parents reported their highest psychosocial stress scale as “ability to access employment in setting of home nursing shortage.” Because the likelihood of nursing shortage is highest at night, many parents describe working outside the home during day hours but then doing awake hands-on care of their child during night hours: a perpetual sleep deprivation.
Impact to parental marital union and child raising of the chronically ill child's siblings is described to be lower than our study team would have perceived based on care encounters, possibly testifying to the resiliency or worldview of parents who have been forced to creatively and bravely face the home nursing shortage as part of their “normal” since their child's diagnosis.
Delays to hospital discharge due to lack of home nursing availability are reported in this survey to not be infrequent, to not be short, and to often occur multiple times in 1 child's lifetime. Extended hospitalizations due to lack of home nursing care options result in emotional and economic toll on families with a financial impact on hospitals. Delays in hospital discharge shift the care to inpatient pediatric nursing staff, which also tends to be an understaffed workforce.4 Many children with complex medical conditions remain in the hospital away from their families, although home health care is clearly cost effective as compared with inpatient medical management.28,29
This study revealed that private insurance coverage alone (without Medicaid as primary or secondary) correlated with a gap in nursing service coverage (P = .01). While home care services may be a covered benefit listed on paper under private health plans, most do not cover private-duty nursing (83%) or home health aides (45%).30 Medicaid is the main payer to pediatric home health care, and yet Medicaid reimbursement to home health agencies is noted to be a rate often insufficient to provide beneficiaries access to home health services.26
Limitations to this study include small sample size and 1-site location at a freestanding children's hospital in the Midwest. There is a possibility that the repercussions of the nursing shortage may translate differently across the United States. However, the nursing shortage seems to be fairly consistent across the country.5
The home health nursing industry will benefit from attracting more nurses to their section of nursing, specifically, pediatric home health nursing.31 This survey revealed that children with higher level of technologies were more likely to lack home nursing access (presumably because a higher level of nursing training is required for technologies such as tracheostomy). Incentives for nursing assistants to receive additional training toward licensed nursing may then improve access to care for children with technology dependence. Scholarships and incentive plans may be set up for nursing students interested in exploring home health to stipulate postgraduation commitment working in the home health field. The home nursing shortage may be addressed through fiscal models, as improved wage for home health nurses in the form of Medicaid wage pass-through did translate into improved home nursing recruitment and employee retention in the states where this was enacted.32 Nurses should be reimbursed for the time and money that they spend driving between houses, especially in rural areas. A creative alternative may be to consider a financial reimbursement approach for family members providing hands-on nursing care for a child.
The number of children with complex chronic conditions is increasing as the shortage of nurses is also increasing.33 Pediatric palliative care providers should consider the opportunity to inquire about a family's home nursing situation as a form of whole-child, whole-family care. The nursing shortage translates into a lived experience for families with children with complex medical conditions through employment, economic, emotional, and psychosocial impact.34
Acknowledgments
The study team thanks the Hand-in-Hand interdisciplinary team, Ms Sara Woodworth, and the incredible patients and families we are privileged to care for daily.
Footnotes
The authors have no conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.jhpn.com).
References
- 1.MacLean S, Hassmiller S, Shaffer F, Rohrbaugh K, Collier T, Fairman J. Scale, cause, and implications of the primary care nursing shortage. . 2014;35:443-457. [DOI] [PubMed] [Google Scholar]
- 2.Bona J, Wolfe J. Disparities in pediatric palliative care: an opportunity to strive for equity. . 2017;140(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaye EC, Rubenstein J, Levine D, Baker JN, Dabbs D, Friebert SE. Pediatric palliative care in the community. . 2015;65(4):316-333. [DOI] [PubMed] [Google Scholar]
- 4.Mack JW. Pediatric palliative care—a shared priority. . 2017;3(9):1220-1221. [DOI] [PubMed] [Google Scholar]
- 5.Bogetz JF, Friebert S. Defining success in pediatric palliative care while tackling the quadruple aim. . 2017;20(2):116-119. [DOI] [PubMed] [Google Scholar]
- 6.Friedrichsdorf SJ. Contemporary pediatric palliative care: myths and barriers to integration into clinical care. . 2017;13(1):8-12. [DOI] [PubMed] [Google Scholar]
- 7.Center to Advance Palliative Care (CAPC). . 2016. https://www.capc.org/topics/pediatric-palliative-care/. Accessed December 6, 2017.
- 8.Weaver MS, Schroeder D, Wichman C, Bace S, Vail C, Macfadyen A. Pediatric palliative care needs assessments: from paper forms to actionable patient care. . 2017;20(3):216-217. [DOI] [PubMed] [Google Scholar]
- 9.Abode KA, Reilly C, Davis SD, Zdanski CJ, Retsch-Bogart GZ. Barriers to hospital discharge for young children with new tracheostomies. . 2011;183(1):A6273. [Google Scholar]
- 10.Amin R, Sayal A, Syed F, et al. How long does it take to initiate a child on long-term invasive ventilation? Results from a Canadian pediatric home ventilation program. . 2015;22(2):103-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Margolan H, Fraser J, Lenton S. Parental experience of services when their child requires long-term ventilation. Implications for commissioning and providing services. . 2004;30(3):257-264. [DOI] [PubMed] [Google Scholar]
- 12.Well E. Lack of community staff forces children to spend months in hospital. . 2009;21(3):3-5. [Google Scholar]
- 13.Rosseter Robert. American Association of Colleges of Nursing. . May 18, 2017. http://www.aacn.nche.edu/media-relations/fact-sheets/nursing-shortage. Accessed June 10, 2017. [Google Scholar]
- 14.American Academy of Colleges of Nursing. Strategies to reverse the new nursing shortage. 2001. http://www.aacn.nche.edu/publications/position/tri-council-shortage. Accessed July 14, 2017.
- 15.Snavely TM. A brief economic analysis of the looming nursing shortage in the United States. . 2016;34(2):96-100. [PubMed] [Google Scholar]
- 16.University of Nebraska Medical Center. The nursing shortage. 2017. https://www.unmc.edu/nursing/programs/the-nursing-shortage.html. Accessed July 14, 2017.
- 17.Child palliative care limited by nurse numbers. . 2015;111(39):5. [PubMed] [Google Scholar]
- 18.Leonard BJ. Staff shortage affects care for families of seriously ill children. . 2016;28(2):6. [DOI] [PubMed] [Google Scholar]
- 19.Lanning S. Demands on nursing staff providing home-based care for children—interviews of interdisciplinary teams by using the critical incident technique. . 2014;15(4):42. [Google Scholar]
- 20.Doyle C, Buckley S. An account of nursing a child with complex needs in the home. . 2012;24(5):19-22. [DOI] [PubMed] [Google Scholar]
- 21.Nurse Journal. Home Healthcare Nurse Careers & Salary Outlook. 2014. http://nursejournal.org/home-healthcare-nursing/home-healthcare-nurse-careers-salary-outlook/. Accessed July 6, 2017.
- 22.Skillman SM, Patterson DG, Coulthard C, Mroz TM . Seattle, WA: WWAMI Rural Health Research Center, University of Washington; 2016. [Google Scholar]
- 23.Lazzarin P, Schiavin B, Brugnaro L, Benini F. Parents spend an average of nine hours a day providing palliative care for children at home and need to maintain an average of five life-saving devices [published online ahead of print September 25, 2017]. . 2017. [DOI] [PubMed] [Google Scholar]
- 24.Walter JK, DeCamp LR, Warrier KS, Murphy TP, Keefer PM. Care of the complex chronically ill child by generalist pediatricians: lessons learned from pediatric palliative care. . 2013;3(2):129-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dillman D, Smyth J, Christian L . 3rd ed Hoboken, NJ: John Wiley & Sons, Inc; 2009. [Google Scholar]
- 26.Thomas S, Price M. Respite care in seven families with children with complex care needs. . 2012;24(8):24-27. [DOI] [PubMed] [Google Scholar]
- 27.Romley JA, Shah AK, Chung PJ, Elliott MN, Vestal KD, Schuster MA. Family-provided health care for children with special health care needs. . 2017;139:1-10. [DOI] [PubMed] [Google Scholar]
- 28.Kerr CW, Donohue KA, Tangeman JC, et al. Cost savings and enhanced hospice enrollment with a home-based palliative care program. . 2014;17(12):1328-1335. [DOI] [PubMed] [Google Scholar]
- 29.Goldhagen J, Fafard M, Komatz K, Eason T, Livingood WC. Community-based pediatric palliative care for health related quality of life, hospital utilization, and costs lessons learned from a pilot study. . 2016;15:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Academy of Pediatrics Committee on Child Health Financing, Section on Home Care. Financing of home health care. . 2016;118(2):834-838. [DOI] [PubMed] [Google Scholar]
- 31.Davis KG, Johnson CD. Contemporary pediatric public health challenges. . 2016;63(5):xvii-xviii. [DOI] [PubMed] [Google Scholar]
- 32.Baughman RA, Smith K. The effect of Medicaid wage pass-through programs on the wages of direct care workers. . 2010;48(5):426-432. [DOI] [PubMed] [Google Scholar]
- 33.Cervasio K. The role of the pediatric home healthcare nurse. . 2010;28(4):24-431. [DOI] [PubMed] [Google Scholar]
- 34.Mooney-Doyle K, Deatrick JA, Ulrich CM, Meghani SH, Feudtner C. Parenting in childhood life-threatening illness: a mixed-methods study [published online ahead of print October 3, 2017]. . 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]


