Abstract
To compare the effectiveness of total disk replacement (TDR), anterior cervical discectomy and fusion (ACDF), and laminoplasty on atypical symptoms of cervical spondylosis.
Patients with confirmed diagnosis of cervical spondylosis and reported atypical symptoms such as blurred vision, headache, nausea, palpitation, tinnitus, vertigo, hypomnesia, and abdominal discomfort were retrospectively included in the present study. They were treated with TDR, ACDF, or laminoplasty depending on the etiology and patient preference. Severity of the atypical symptoms before the surgery and at the end of 2-year follow-up was recorded and the degree of severity alleviation was compared between different surgical approaches.
A total number of 336 patients who were treated in our institute from February 2002 to March 2011 were included in the final analysis. Atypical symptoms were significantly alleviated in most patients after surgical intervention. No significant differences were found regarding the change of severity of those symptoms among patients in different surgery groups.
TDR, ACDF, and laminoplasty can equally alleviate the severity of atypical symptoms in patients with cervical spondylosis. This indicates that the neural network in the posterior longitudinal ligament may not be the cause of atypical symptoms in patients with cervical spondylosis.
Keywords: anterior cervical discectomy and fusion, atypical symptoms, cervical spondylosis, double-door laminoplasty, total disk replacement, vertigo
1. Introduction
Among the elderly population, cervical spondylosis is the most common reason for symptoms related to spinal cord dysfunction.[1,2] Patients with cervical spondylosis often demonstrate symptoms such as pain of the neck and shoulder, numbness, hypersensitivity, and impairment of the fine-motor performance of arms.[3,4] Main etiology of cervical spondylosis includes the herniation of cervical disk, ossification and hypertrophy of posterior longitudinal ligament and ligamentum flavum, osteoproliferation, cervical stenosis, and instability of cervical spine. Surgical approaches such as anterior cervical discectomy and fusion (ACDF), total disk replacement (TDR), and laminoplasty are routinely used to eliminate the compression on the spinal cord and nerve roots thus alleviate the symptoms of cervical spondylosis.[5–7]
Vertigo, headache, palpitation, nausea, abdominal discomfort, tinnitus, blurred vision, and hypomnesia are common symptoms in patients with cervical spondylosis. However, their etiology is not as clear as the typical manifestations of cervical spondylosis such as pain, numbness, and fine-motor functions. Because there are no specific pathologic or radiologic abnormalities that can be responsible for those symptoms, it is hard to choose effective treatment measures. To our knowledge, few studies have reported the efficacy of any surgical approaches on atypical symptoms in patients with cervical spondylosis. In the present study, we compared the efficacy of ACDF, TDR, and laminoplasty on atypical symptoms in patients with cervical spondylosis, and analyzed the possible mechanisms underlying those symptoms.
2. Objective
The present study compares the efficacy of TDR, ACDF, and laminoplasty on symptoms such as vertigo, headache, palpitation, nausea, abdominal discomfort, tinnitus, blurred vision, and hypomnesia in patients with cervical spondylosis and tries to explore its etiology.
3. Materials and methods
Clinical materials of all the patients included in this study were retrospectively reviewed, and the efficacy of different surgical methods for cervical spondylosis was compared. The current research was approved by the Ethics Committee of Beijing Ji Shui Tan Hospital and a written consent was obtained from the patients or patients’ guardians before the study.
3.1. Patients
Patients who were confirmed with diagnosis of cervical spondylosis, and reported at least one of the following symptoms: blurred vision, headache, nausea, palpitation, tinnitus, vertigo, hypomnesia, and abdominal discomfort were included in the present study after any possible maladies were ruled out by specialists in neurology, ophthalmology, and cardiovascular otolaryngology departments. A total of 336 patients with atypical symptoms of cervical spondylosis were treated in our department from February 2002 to March 2011.
The inclusion criteria: patients reported that they have experienced at least one of the atypical symptoms in the last 3 months; no improvement of symptoms was achieved after at least 3 months of conservative treatment; one or more level cervical spinal cord compression is shown by X-ray, computed tomography (CT), or magnetic resonance imaging (MRI); myelopathy or refractory radiculopathy due to degenerative disc disease confirmed by MRI and/or CT; no neurological, cardiovascular, or other organ deficiencies were found after consulting specialists from neurology, ophthalmology, and cardiovascular otolaryngology departments; no instability on lateral flexion-extension view; motion was preserved at the index level(s); no congenital bony canal stenosis; and no history of cervical surgery.
Among the included patients, those with 1- or 2-level cervical spinal cord compression underwent either ACDF or TDR by their choice, and patients with more than 3-level cervical spinal cord compressions underwent double-door laminoplasty.
3.2. Surgical procedure
ACDF and TDR were performed through a standard Smith–Robinson approach according to the operation manual. After decompression (posterior longitudinal ligament routinely removed), the cervical disk was stabilized by titanium cages stuffed with autogenous bone and plates or Bryan TM discs (Medtronic, Minneapolis, MN). Sixty-seven patients were included in the ACDF group, including 9 cases of C3/4 level, 7 cases of C4/5 level, 19 cases of C5/6 level, 4 cases of C6/7 level, 3 cases of C3/4 and C4/5 levels, 17 cases of C4/5 and C5/6 levels, 7 cases of C5/6 and C6/7 levels, 1 case of C3/4, C4/5, and C5/6 levels. Seventy-three patients were included in TDR group. Among those patients, 62 patients had single-level cervical TDR (5 cases of C3/4; 12 cases of C4/5; 35 cases of C5/6; and 10 cases of C6/7), 10 patients had double-level cervical TDR (1 case of C3/4 and C6/7; 5 cases of C4/5 and C5/6; 4 cases of C5/6 and 6/7). One patient underwent 3-level cervical TDR (C3/4, C4/5, and C5/6). One hundred ninety-six patients underwent double-door laminoplasty by sagittal splitting of the spinous processes of C3–C6 by a wire-saw following a partial or total laminectomy of the C2 and C7, which was decided by the extent of pathology. The door was kept open by a trapezoid coral artificial bone between the spinous processes.
3.3. Data collection
All patients finished a questionnaire before the surgery and at the end of the 2-year follow up. In the questionnaire, patients were asked to state the severity of atypical symptoms. After the follow up, patient reports on the severity of atypical symptoms were translated into symptom severity scores by the following criteria: none: 0; mild: 1; medium: 2; severe: 3; and unbearable: 4. The change in severity scores (severity score at the last follow up − severity score before the surgery) was compared among the 3 surgical groups with 1-way analysis of variance using statistical software SPSS17.0.
4. Results
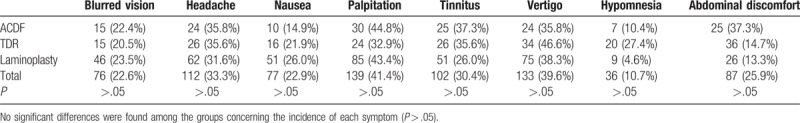
A total number of 336 patients were included in the study. Among them, 67 patients (40 males and 27 females, with an average age of 53.4 years) were treated with the ACDF; 196 patients (148 males and 48 females, mean age 54 years) were treated with the laminoplasty; and 73 patients (47 males and 26 females, mean age 48.9 years) were treated with TDR. No significant differences were found among the different surgical groups concerning the patient age (P > .05), gender (P > .05), and the severity of atypical symptoms before the surgical intervention (P > .05). Typically patients suffered from 2 to 3 of those atypical symptoms. There were no significant differences among the groups regarding the constitution ratio of each atypical symptom (Table 1).
Table 1.
Patient numbers with each symptom and surgical intervention method.
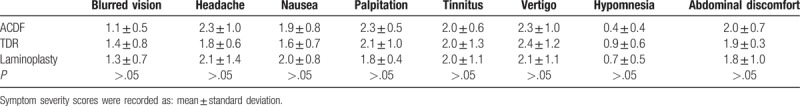
By the end of 2-year follow up, most of the atypical symptoms were significantly alleviated in the patients. No significant differences were found among the groups concerning how much the symptoms were alleviated (P > .05) (Table 2).
Table 2.
Degree of alleviation in the severity of some atypical symptoms in patients treated by different surgical methods, and there were no significant differences among the 3 groups (P > .05).
5. Discussion
Prevalence of cervical spondylosis is high among the age group of over 55 years, and the with wide application of computers and increasing reliance of cell phones, the number of young patients with cervical spondylosis is also on the rise.[1,2] Pain, numbness, hypersensitivity in neck and upper extremities, impairment of the fine-motor skill of hands, difficulty in fast movement of lower extremities as well as abnormal reflex can be the main manifestations in patients with early-stage clinical cervical spondylosis. Patients with advanced cervical spondylosis may also suffer from trouble in steady walking, active reflex of tendons, and atrophy of related muscles.[8–11]
In our clinical practice, many patients who were diagnosed with cervical spondylosis also report discomfort caused by vertigo, headache, palpitation, nausea, abdominal discomfort, tinnitus, blurred vision, hypomnesia, and gastrointestinal discomfort. This set of symptoms in patients with cervical spondylosis was first reported by Barré and liéou in 1926, and was named “Barré and liéou syndrome.”[12,13] Because unlike the typical symptoms such as pain and numbness of the neck and shoulder, no specific pathologic or anatomic abnormalities were found to be responsible for those symptoms, we use “atypical” to include them all. Although the current literature has elaborate reports on the treatment for cervical spondylosis, little was known about the pathology and treatment of atypical symptoms in patients with cervical spondylosis.
One of the popular assumptions is that the degenerated structures such as osteophytes and hyperplasia of ligaments in the cervical spine could compress the surrounding blood vessels, which can partially block the blood flew into brain and cause headache and vertigo.[14–16] Some authors also proposed that whiplash injury and instability of cervical spine are related to the onset of atypical symptoms.[17,18] However, the evidence provided by those studies was not convincing enough to drive a consensus about the mechanism of atypical symptoms in patients with cervical spondylosis.
In harmony with its huge patient base with cervical spondylosis, the number of patients with atypical symptoms is also substantial. Thus, several medical centers in China have conducted clinical and basic research atypical symptoms in patients with cervical spondylosis. Two of those studies found that in patients surgically treated in their center for atypical symptoms of cervical spondylosis, there were sympathetic nerve fibers in the posterior longitudinal ligament of cervical region, and those nerve fibers have similar structures and immunohistochemical characteristics to the nerve fibers that can be found in the cardiovascular and the gastrointestinal systems. Their interpretation of this phenomenon was that atypical symptoms of cervical spondylosis, especially the symptoms related to cardiovascular and the gastrointestinal system must be the result of sympathetic nerve fiber stimulation on the posterior longitudinal ligament in the cervical section.[19,20] Two more clinical studies carried out by Changzheng Hospital, Shanghai, China[21,22] found that patients achieve significant alleviation of atypical symptoms such as vertigo and headache after ACDF. They assumed that this extra benefit of ACDF can be contributed to the disruption of sympathetic nerve fiber network in the posterior longitudinal ligament during the surgery. This seemingly plausible explanation seems to have gained dominance in Chinese academic circles, and the “atypical symptoms” we call in our paper is also called “sympathetic symptoms” in most Chinese publications.[23]
In the present study, patients who received TDR and ACDF experienced significantly alleviated symptoms compared with that of before the surgery, this is in accordance with the previous studies.[21,22] However, patients in the double-door laminoplasty group have also reported significantly alleviated symptoms after the surgery, and the degree of symptom severity alleviation was not significantly different in the laminoplasty group than TDR and ACDF groups. The currently accepted mechanism of atypical symptoms is based on the fact that the disruption of sympathetic nerve network in the posterior longitudinal ligament alleviates the severity of those atypical symptoms. However, the existing papers failed to design a compare group that does not interfere with the “sympathetic nerve network” in the posterior longitudinal ligament. In our research, however, both the intervertebral disk and posterior longitudinal ligaments were kept intact in patients in laminoplasty group, and those patients achieved the same level of symptom alleviation as the ACDF and TDR groups. Thus, it is possible that those atypical symptoms may not be triggered by the sympathetic nerve fibers in the posterior longitudinal ligament. Considering that the only thing in common with all the 3 surgeries is the decompression of dura and spinal cord, we assume that the stimulation on dura and the spinal cord and the spinal meninges might be responsible for the atypical symptoms in patients with cervical spondylosis. This is different from some of the previous assumptions that the atypical symptoms are mainly caused by the sympathetic nerves in the posterior ligament.[19,21,22] It is also possible that some trigger points exist in the ligamentum flavum and the posterior structure of the cervical vertebra.
Considering that some of the symptoms like headache, nausea, palpitation, and abdominal discomfort can be due to multiple reasons, in our research, neurological, cardiovascular, or other organ deficiencies were ruled out after consulting specialists from neurology, ophthalmology, and cardiovascular otolaryngology departments; typically, a head MRI was taken to rule out neurological deficiencies such as cerebral infarction or tumor, a psychologist was recommended if the patient excreted obvious signs of anxiety, funduscopic examination should be performed by an ophthalmologist to rule out any pathological changes in the eye, diagnosis of high blood pressure and any significant changes of cervical vessels were ruled out by a cardiologist and type-B ultrasonic specialist, an otolaryngologist was consulted to rule out any inner ear problems that may cause dizziness. In the included patients, all of those examinations came back negative, and there were no confounding reasons such as history of migraines and other medications that may be the cause of those atypical symptoms. However, conclusion of the present study totally relies on a survey form filled by patients, which could be a biased approach as each person has a different threshold for giving severity scores. No unbiased approach such as a physical or neurological examination is done, which is the biggest shortcoming of the study. Randomized controlled trials or prospective studies with more objective physical or neurological examinations are necessary to avoid such bias. Moreover, more animal and cadaveric studies should be carried out to further explore the etiology of these symptoms and to find a more direct and effective treatment measures.
6. Conclusions
TDR, ACDF, and laminoplasty can equally alleviate the severity of atypical symptoms in patients with cervical spondylosis. This indicates that there may not be a neural network in the posterior longitudinal ligament that can be the cause of atypical symptoms in patients with cervical spondylosis.
Author contributions
Yuqing Sun and Aikeremujiang Muheremu: study design, statistical analysis, and writing the paper; Wei Tian: study design, selection, and recruiting patients.
Data curation: Yuqing Sun, Aikeremujiang Muheremu.
Formal analysis: Yuqing Sun.
Funding acquisition: Aikeremujiang Muheremu.
Methodology: Yuqing Sun, Wei Tian.
Project administration: Wei Tian.
Supervision: Wei Tian.
Writing – original draft: Aikeremujiang Muheremu.
Writing – review & editing: Wei Tian.
Footnotes
Abbreviations: ACDF = anterior cervical discectomy and fusion, TDR = total disk replacement.
The study was supported by the Innovative Research Fund of Xinjiang Medical University (XYDCX2016109 and XYDCX2016108) and the National Natural Science Foundation of China (81360194).
The authors have no conflicts of interest to disclose.
References
- [1].Morio Y, Teshima R, Nagashima H, et al. Correlation between operative outcomes of cervical compression myelopathy and MRI of the spinal cord. Spine 2001;26:1238–45. [DOI] [PubMed] [Google Scholar]
- [2].Matsumoto M, Toyama Y, Ishikawa M, et al. Increased signal intensity of spinal cord on magnetic resonance images in cervical compressive myelopathy. Spine 2000;25:677–82. [DOI] [PubMed] [Google Scholar]
- [3].Bohlman HH, Emery SE, Goodfellow DB, et al. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy: long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 1993;75:1298–307. [DOI] [PubMed] [Google Scholar]
- [4].Chagas H, Domingues F, Aversa A, et al. Cervical spondylotic myelopathy: 10 years of prospective outcome analysis of anterior decompression and fusion. Surg Neurol 2005;64suppl 1:S30–5. [DOI] [PubMed] [Google Scholar]
- [5].Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976) 2005;30:2138–44. [DOI] [PubMed] [Google Scholar]
- [6].Rajasekaran S, Thomas A, Kanna RM, et al. Lumbar spinous process splitting decompression provides equivalent outcomes to conventional midline decompression in degenerative lumbar canal stenosis. Spine (Phila Pa 1976) 2013;38:1737–43. [DOI] [PubMed] [Google Scholar]
- [7].Yuan W, Zhu Y, Liu X, et al. Laminoplasty versus skip laminectomy for the treatment of multilevel cervical spondylotic myelopathy: a systematic review. Arch Orthop Trauma Surg 2014;134:1–7. [DOI] [PubMed] [Google Scholar]
- [8].Kim CH, Chung CK, Kim K-J, et al. Cervical extension magnetic resonance imaging in evaluating cervical spondylotic myelopathy. Acta Neurochir 2014;156:259–66. [DOI] [PubMed] [Google Scholar]
- [9].Vavasour IM, Meyers SM, MacMillan EL, et al. Increased spinal cord movements in cervical spondylotic myelopathy. Spine J 2014;14:2344–54. [DOI] [PubMed] [Google Scholar]
- [10].Endo K, Ichimaru K, Komagata M, et al. Cervical dizziness and dizziness after whiplash injury. Eur Spine J 2006;15:886–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Foster CA, Jabbour P. Barre-Lieou syndrome and the problem of the obsolete eponym. J Laryngol Otol 2007;121:680–3. [DOI] [PubMed] [Google Scholar]
- [12].Serre H, Labauge R, Simon L, et al. Barré-Liéou syndrome, designated “posterior sympathetic cervical syndrome”. Rheumatologie 1969;21:217–46. [PubMed] [Google Scholar]
- [13].Pearce JM. Barre-Lieou “syndrome”. J Neurol Neurosurg Psychiatry 2004;75:319. [PMC free article] [PubMed] [Google Scholar]
- [14].Strek P, Reron E, Maga P, et al. A possible correlation between vertebral artery insufficiency and degenerative changes in the cervical spine. Eur Arch Otorhinolaryngol 1998;255:437–40. [DOI] [PubMed] [Google Scholar]
- [15].Brandt T, Bronstein AM. Cervical vertigo. J Neurol Neurosurg Psychiatry 2001;71:8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Ito Y, Tanaka N, Fujimoto Y, et al. Cervical angina caused by atlantoaxial instability. J Spinal Disord Tech 2004;17:462–5. [DOI] [PubMed] [Google Scholar]
- [17].Qian J, Tian Y, Qiu GX, et al. Dynamic radiographic analysis of sympathetic cervical spondylotic myelopathy instability. Chin Med Sci J 2009;24:46–9. [DOI] [PubMed] [Google Scholar]
- [18].Vinchon M, Assaker R, Leclerc X, et al. Vertebrobasilar insufficiency resulting from traumatic atlantoaxial instability: case report. Neurosurgery 1995;36:839–41. [DOI] [PubMed] [Google Scholar]
- [19].Wang Z, Wang X, Yuan W, et al. Degenerative pathological irritations to cervical PLL may play a role in presenting sympathetic symptoms. J Med Hypotheses 2011;77:921–3. [DOI] [PubMed] [Google Scholar]
- [20].Gu1 Q, Jiang D, Wang X, et al. Chronic compression of the posterior longitudinal ligament of the cervical spine is associated with abnormal discharge of middle cervical ganglion. Int J Clin Exp Med 2014;7:4316–21. [PMC free article] [PubMed] [Google Scholar]
- [21].Xue R, Shen Y, Wang L, et al. Early clinical effect of resecting posterior longitudinal ligament in anterior approach for cervical spondylotic myelopathy with sympathetic symptoms. Chin J Orthop 2013;33:105–10. [Google Scholar]
- [22].Li J, Jiang D-J, Wang X-W, et al. Mid-term outcomes of anterior cervical fusion for cervical spondylosis with sympathetic symptoms. J Spinal Disord Tech 2016;29:255–60. [DOI] [PubMed] [Google Scholar]
- [23].Wang X, Gu T, Yuan W, et al. Treatment and mechanism of cervical spondylosis with sympathetic symptoms. Chin J Surg 2008;46:1424–7. [PubMed] [Google Scholar]


