Abstract
Background:
Limited evidence is available regarding the effects of insoles on pediatric flexible flatfoot because of the heterogeneity and low methodological quality of previous studies. The purpose of this prospective trial is to examine the short-term effects of customized arch support insoles on symptomatic flexible flatfoot in children by using the International Classification of Functioning, randomized controlled Disability, and Health (ICF) framework.
Methods:
This study was conducted in a rehabilitation outpatient clinic of a teaching hospital. Fifty-two children with symptomatic flexible flatfoot were included. The children in the treatment group wore customized arch support insoles for 12 weeks, whereas those in the control group did not wear the insoles. Both clinical and radiographic measurements, including the navicular drop, foot posture index, Beighton hypermobility score, talonavicular coverage angle, calcaneal inclination angle, and calcaneal-first metatarsal angle, were used for diagnosing flexible flatfoot. Physical activity (10-m normal and fast walking, stair ascent, stair descent, and chair rising), physical function, and psychometric properties (Pediatric Outcome Data Collection Instrument and Pediatric Quality of Life Inventory) were evaluated at the baseline and 12 weeks after the intervention.
Results:
Compared with the control group, the treatment group exhibited significant improvement in pain/comfort (P = .048), physical health (P = .035), stair ascent time (P = .015), upper extremity and physical function (P = .016), and transfer and basic mobility (P = .042) during the intervention period.
Conclusion:
Children with flexible flatfoot who wore customized arch support insoles for 12 weeks exhibited significantly improved pain/comfort, physical health, stair ascent time, upper extremity and physical function, and transfer and basic mobility. These variables belong to the domains of body functions and structures and activity and participation in the ICF framework. However, because the groups were not comparable, additional studies with larger sample sizes should be conducted.
Keywords: children, effect, flatfoot, insoles
1. Introduction
Foot problems have been reported to occur in 30% of children; among the problems, flatfoot is a common foot deformity.[1] Flexible flatfoot is a condition that involves the collapse of the medial longitudinal arch of the foot during weight-bearing stress and the restoration of the arch after the removal of body weight. Constitutional laxity affecting the ligaments and joints, age, overweight, or obesity, and, to a lesser extent, strength, and Achilles tendon shortening are some contributing factors for this condition.[2–4] The prevalence of flatfoot decreases with age, from 54% to 57% in children aged 2 to 3 years to 21% to 24% in those aged 5 to 6 years, and then to 15% in those aged 10 years.[2,5] Most children with flexible flatfoot develop arches with time; thus, it cannot be ruled out that this condition is a normal phase of the physiological maturation of the arch.[4,6]
Flatfoot may increase the load of the foot structure, potentially interfering with normal foot function.[7] With prolonged standing or walking, some children with flatfoot experience rapid discomfort or fatigue in the foot, pain in the plantar foot, and instability of the medial foot structure.[7] Treatment with corrective shoes or insoles for 3 years does not correct the deformity in children with a natural history of flexible flatfoot. The effects of insoles on symptomatic flexible flatfoot in children remain uncertain.[4,6]
The International Classification of Functioning, Disability, and Health (ICF) framework can be used to describe the health status of individuals through assessments of dynamic interactions between body functions and structures, activities and participation, and personal and environmental factors; this framework is widely implemented in the field of physical medicine and rehabilitation.[8] Previous studies have evaluated the effects of insoles on flatfoot but have mainly focused on body functions and structures.[9–11] Limited evidence is available regarding the effects of nonsurgical intervention on pediatric flexible flatfoot because of the heterogeneity and low methodological quality of previous studies.[6] A randomized controlled trial investigating the efficacy of any insole in the treatment of flexible flatfoot is crucial to provide evidence to support this extremely common practice. Therefore, in this study, using the ICF framework, we investigated the short-term effects of customized insoles on body functions and structures, and activities and participation in children with symptomatic flexible flatfoot. We hypothesized that the short-term use of customized insoles improves the scores for measures of body functions and structures and activities and participation.
2. Materials and methods
2.1. Participants
This prospective, randomized controlled clinical trial was conducted at Shin Kong Wu Ho-Su Memorial Hospital, an 844-bed medical center located in Northern Taiwan. This study recruited children presenting symptomatic flexible flatfoot only (pain over the foot or calf, fatigue after prolonged walking, and gait disturbances) who visited the Department of Physical Medicine and Rehabilitation between 1 January 2015 and 31 December 2015. We excluded children with a history of foot injury or surgery, foot abnormalities affecting locomotion or foot mobility, or a confirmed diagnosis of developmental delays such as developmental coordination disorder and neurological deficits.
2.2. Clinical and radiographic diagnostic criteria for flexible flatfoot diagnosis
The prevalence of joint hypermobility varies from 3% to 30% in children.[12,13] In Chinese children, the prevalence of hypermobility is 100% at the age of 3 years, 67% at the age of 6 years, and 28% at the age of 12 years, whereas the prevalence in western children of the same age is 50%, 5%, and 1%, respectively.[2,14] In this study, the Beighton hypermobility score was used to measure joint mobility.[12] This scale consists of 5 items, with a total score ranging from 0 to 9. This scale has been found to be relatively insensitive and inappropriate for different ages, sex, and ethnic groups.[15] A total score of >4 is used to define generalized hypermobility of joints in the present study.[12]
The navicular drop test was used to measure the medial longitudinal arch.[16] To evaluate the navicular drop, the navicular height was measured by maintaining the subtalar joint in the neutral position under nonweight-bearing and weight-bearing conditions. The normative values of the navicular drop test for male and female children are 4 to 6 and 3 to 4 mm, respectively.[16] This test has been reported to demonstrate moderate intratester reliability (intraclass correlation coefficient, 0.61–0.79) and fair interrater reliability (0.57).[17]
The 6-item version of the foot posture index was used to evaluate the weight-bearing foot posture in the standing position.[18] Foot posture can be obtained according to a composite score of clinical observation. It can be highly pronated (+10 to +12), pronated (+6 to +9), normal (0 to +5), supinated (−1 to −4), and highly supinated (−5 to −12). The index has been reported to demonstrate satisfactory interrater reliability.[19]
Two bilateral radiographs consisting of lateral and anteroposterior views were obtained with the children in the bipedal standing position under the weight-bearing condition.[20] The calcaneal inclination angle and the calcaneal-first metatarsal angle were assessed using the images obtained in the lateral view, and the talonavicular coverage angle was assessed using the images obtained in the anteroposterior view.
In this study, the clinical criteria were a total Beighton hypermobility score of >4, navicular drop of at least 6 mm, and foot posture index of >6. At least 2 of the 3 radiographic angles should meet the criteria of flat-arched feet in the present study.[20] All clinical measurements were conducted by a qualified senior specialist in physical and rehabilitation medicine, and each angle in the radiographs was measured by a qualified senior radiologist who was blinded to the allocated groups of the children.
The parents of the children who met the clinical and radiographic eligibility criteria were invited to participate in this study. All parents provided written informed consent for themselves and their children. The age of the participants ranged from 3 to 10 years.
2.3. Ethics
This study is registered at ClinicalTrials.gov (NCT02414087). This trial was approved by the Institutional Review Board of Shin Kong Wu Ho-Su Memorial Hospital (Protocol No. /IRB No.: 20140715R; date of approval: 9 October 2014). Moreover, this study was performed in accordance with the World Medical Association Declaration of Helsinki. The experiments were performed in accordance with the approved guidelines.
2.4. Randomization
The participants were randomly assigned to the treatment group (with customized insoles) or the control group (without customized insoles) according to computer-generated random numbers (Fig. 1). Group assignment was conducted using block randomization, with a block size of 4. Allocation was initially concealed. A sealed envelope was opened for each consecutive participant to reveal the participant's group allocation when the participant was recruited to the study. One physician enrolled all participants, and another investigator generated the allocation sequence and assigned the participants to their groups.
Figure 1.

Flowchart of participant enrolment in the trial.
2.5. Intervention
All children and their parents were provided with information on the natural history of pediatric flexible flatfoot. All participants were informed that they may receive insole treatment for 12 weeks (treatment group) or only follow-up observations after 12 weeks without any intervention (control group). Each participant in the treatment group received a pair of thermoplastic insoles with medial longitudinal arch support, which were composed of high-density ethyl vinyl acetate (Fig. 2). The qualified senior specialist in physical and rehabilitation medicine used a heat gun to specifically mold the insoles to the participants’ feet; this process ensured that the subtalar joint was maintained in the neutral position for correcting the forefoot abduction and hindfoot pronation. The specialist first maintained participants’ feet in the subtalar neutral position by using the thumb and index finger and maintained the talar head both medially and laterally with equal prominence by using that same hand[21]; simultaneously, the specialist used the other hand (fixed firmly) to enhance the contour of the insole to the medial arch of the foot. The process was performed in the standing, weight-bearing position to ensure that the foot maintained in the subtalar neutral position was in total contact with the insole. Subsequently, after finishing both sides of insoles molding, the specialist checked whether participants’ feet were in the subtalar joint neutral position when the participants stood on the insoles barefoot. The subtalar neutral position was defined by a line bisecting the lower one-third of the leg that was parallel to the calcaneal bisecting line at the insertion of the Achilles tendon.[22] The insoles were remolded in case the subtalar joint neutral position was not corrected. The detailed procedure has been described in our previous studies.[23,24]
Figure 2.
Insole with medial longitudinal arch support.
In Taiwan, children usually wear shoes in kindergarten, school, and when they are outside. However, in summer, a few children may wear sandals when they are outside. The children in this study were instructed to wear the insoles inside self-selected comfortable shoes with a flat sole, rigid high-heel counter, and widened toe box with Velcro.[25] They wore the insoles for 1 hour on the first day; thereafter, they increased insole usage by 1 hour per day. Although no optimum period of insole usage has been established, a previous study reported that 5 to 10 hours of daily insole usage can produce improved outcomes.[26] Therefore, the children were encouraged to wear the insoles for at least 5 hours per day, as much as possible, whenever they wore shoes. The children in the control group were also suggested to wear self-selected comfortable shoes for at least 5 hours per day during the intervention period. Both groups were followed up after 12 weeks.
2.6. Outcome measures
One investigator blinded to group assignment assessed the following outcome measures during the whole treatment course. The participants and parents were aware of the allocation to the treatment or control group. Only the assessor was blinded to group assignment.
Baseline clinical assessment:
General information including age and sex was recorded, and the body mass index was calculated.
Activities and participation: physical activity and physical function
Physical activity was assessed using objective tests. The time taken for 10-m normal and fast walking, stair ascent, timed up and go, and chair rise tests was measured. For the 10-m normal and fast walking test, the participants walked a distance of 10 m across a hard, flat surface once at a normal comfortable speed and once as rapidly as possible. The stair ascent test measured the time taken by the participants to ascend and descend a flight of stairs (14 steps with a height of 18 cm) as rapidly as possible. The timed up and go test measured the time taken by the participants to rise from a seated position in a standard chair, walk for 3 m, and turn back to sit on the seat, as rapidly as possible. The chair rise test measured the time taken by the participants to move 5 times from the sitting to the standing position from a standard chair without using the arms for support, as rapidly as possible. Longer rising times indicated greater limitations on physical activity.
Physical function was measured using the parent-reported Pediatric Outcome Data Collection Instrument (PODCI). We focused on the 4 domains of physical function in the PODCI: upper extremity and physical function, transfer and basic mobility, sports and physical function, and global function. The score for each scale ranges from 0 to 100, with 100 representing the highest functioning. The Chinese version of the PODCI has been reported to demonstrate high reliability.[27]
Body functions and structures: psychometric properties
Psychometric properties were assessed using the 2 domains of the PODCI, namely pain/comfort and happiness, and the Pediatric Quality of Life Inventory-Generic Core Scale (PedsQL; parent proxy-reported format) for health-related quality of life.[28] The PedsQL is rated on a 5-point Likert scale, and the physical health summary score, psychosocial health summary score, and total score can be obtained. The scores range from 0 to 100, with higher scores indicating higher health-related quality of life. The Chinese version of the PedsQL has been reported to demonstrate satisfactory validity, reliability, and feasibility.[29]
2.7. Follow-up assessment
An investigator blinded to group allocation evaluated physical activity, physical function, and psychometric properties at the baseline and 12 weeks after the intervention.
2.8. Sample size
Among the outcome measures, the PedsQL physical health score was used as the primary outcome. To detect an effect size of 0.8 at an alpha level of 0.05 and a power of 0.8, at least 24 participants must be included in each group, with a total of 48 participants.[27] Considering the possibility that 10% of the participants may drop out during follow-up, we initially selected 52 participants (26 participants in each group).
2.9. Statistical analyses
The results are expressed as mean ± standard deviation. Chi-squared and t tests were used to analyze the demographic data and baseline variables. Paired t tests were used to compare the effects of insoles on symptomatic flexible flatfoot based on the outcome measures within and between the 2 groups, by using 95% confidence interval. The effect size was estimated. The magnitude of the effect size was defined as no effect (0–0.19), small effect (0.20–0.49), intermediate effect (0.50–0.79), and large effect (0.80 and higher).[30] The results are presented as mean ± standard deviation and 95% confidence interval. The maximal scores of both PODCI and PedsQL measures are 100; a ceiling effect is present. We also performed efficiency analysis. Specifically, we defined “efficiency” as the percentage of actual improvement divided by the maximal possible improvement, that is (T1 − T0)/(100 − T0) × 100, where T0 represents the baseline score before treatment, and T1 represents the score after 12 weeks of intervention. For example, the total score of transfer and basic mobility in the PODCI is 100. Thus, for the treatment group, T0 = 82.1 and T1 = 93.9; for the control group, T0 = 94.2 and T1 = 95.4. Accordingly, efficiency can be calculated as (93.9 − 82.1)/(100 − 82.1) × 100 = 65.9% for the treatment group and (95.4 − 94.2)/(100 − 94.2) × 100 = 20.7% for the control group. Intention-to-treat analysis (previous observation carried forward) was performed for all participants. Statistical significance was set at P < .05.
3. Results
In this study, we enrolled 52 participants (28 boys and 24 girls). The mean ages of the children in the treatment and control groups were 6.9 ± 0.6 and 6.2 ± 0.4 years, respectively. No significant differences were observed in the demographic data between the 2 groups (Table 1). Two participants in the treatment group withdrew from this study because their parents had limited personal time at the 12-week follow-up. No significant differences were observed in the demographic data between the participants who completed this study and those who withdrew from this study (data not shown). All participants in the treatment group had medial longitudinal arch support; 1 participant had additional medial heel wedge with 0.4 cm in height, and 1 participant had additional medial forefoot and medial heel wedges with 0.4 cm in height. In the treatment group, 24%, 67%, and 10% of children wore shoes with insoles for less than 5 hours per day, between 5 and 10 hours per day, and more than 10 hours per day, respectively; by contrast, 22%, 74%, and 4% of children in the control group wore shoes for the corresponding periods. The children in both groups did not develop complications during the intervention period. In the treatment group, 76.2% of participants reported improvement in their symptoms related to flexible flatfoot after wearing insoles for 12 weeks, whereas 23.8% reported no change of their symptoms.
Table 1.
Basic demographics of participants.
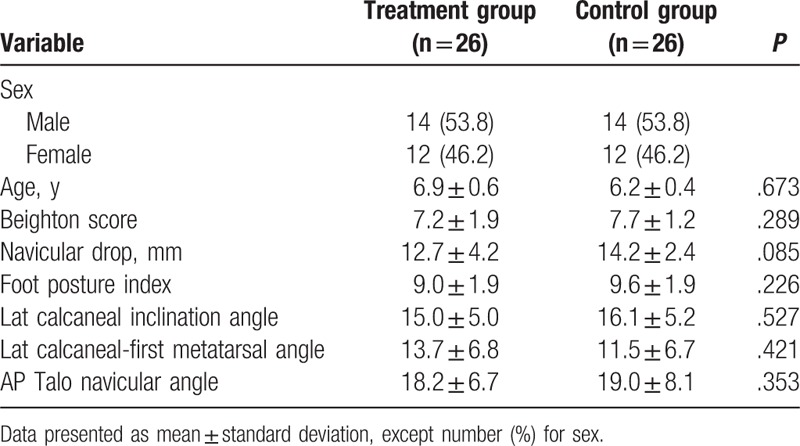
As listed in Table 2, compared with the control group, the treatment group exhibited significantly lower baseline scores for transfer and basic mobility (82.1 vs 94.2, P = .019), physical health (62.3 vs 79.2, P = .033), psychosocial health (65.6 vs 73.8, P = .028), and total health (67.5 vs 74.6, P = .046).
Table 2.
Scores for the participants before intervention.
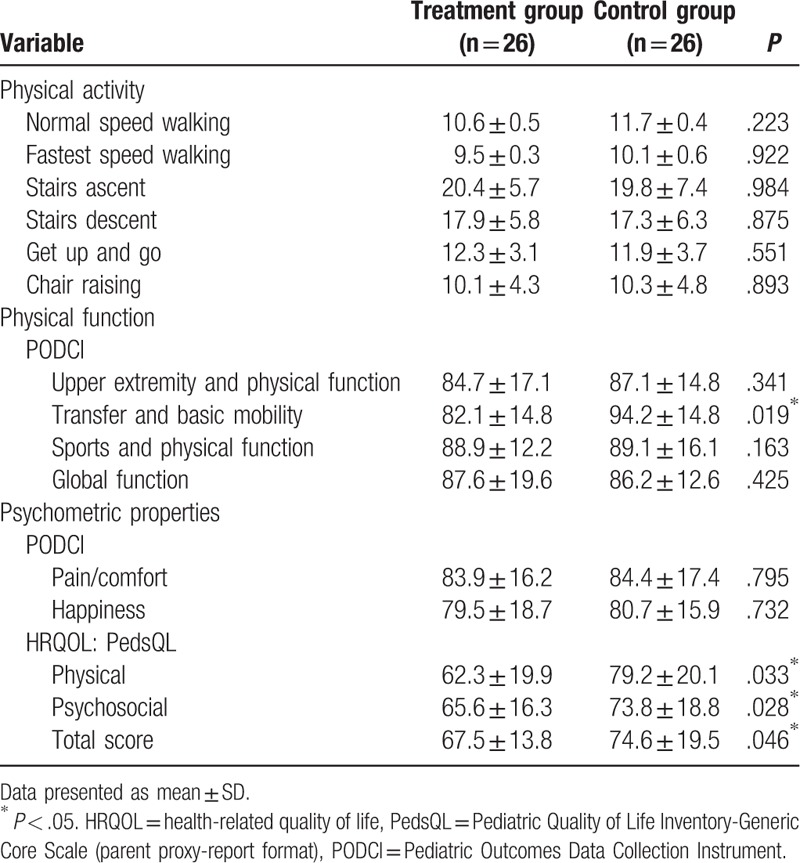
Table 3 presents a summary of the changes in the outcome measures within and between the 2 groups and the efficiency of the 2 groups. Compared with the baseline scores, the treatment group exhibited a significant improvement in fast walking (P = .001) and transfer and basic mobility (P = .002). Objective physical activity tests revealed that compared with the control group, the treatment group exhibited significant improvement in stair ascent time (−2.1, effect size: −0.33, P = .015) (Fig. 3). Compared to the control group, statistically significant improvement of the treatment group was noted in transfer and basic mobility measured by PODCI (10.6, effect size: 0.76, P = .048) and physical health assessed by PedsQL (12, effect size: 0.59, P = .011) at the 12-week follow-up. However, due to the groups were not comparable at baseline and a possible ceiling effect of PODCI and PedsQL, we further performed efficiency analysis and analysis of covariance (ANCOVA) (adjusting for baseline transfer and basic mobility, physical health, psychological health, and total heath). For stair ascent time, the results remained statistically significant using ANCOVA (P = .020). For efficiency analysis, the efficiency was statistically higher in the treatment group than in the control group for physical health by PedsQL (10.3% vs −38.9%, P = .035, and P < .001 by ANCOVA); and pain and comfort (30.4% vs −7.7%, P = .048, and P < .008 by ANCOVA), upper extremity and physical function (21.6% vs −33.3%, P = .016, and P < .001 by ANCOVA), and transfer and basic mobility by PODCI (65.9% vs 20.7%, P = .042, and P < .005 by ANCOVA) at the 12-week follow-up.
Table 3.
Changes in scores of participants after intervention.
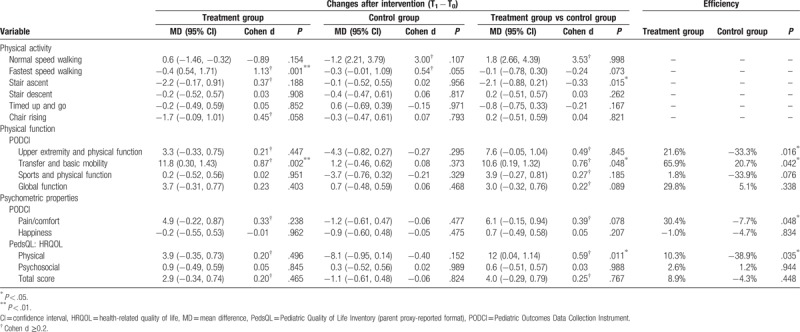
Figure 3.
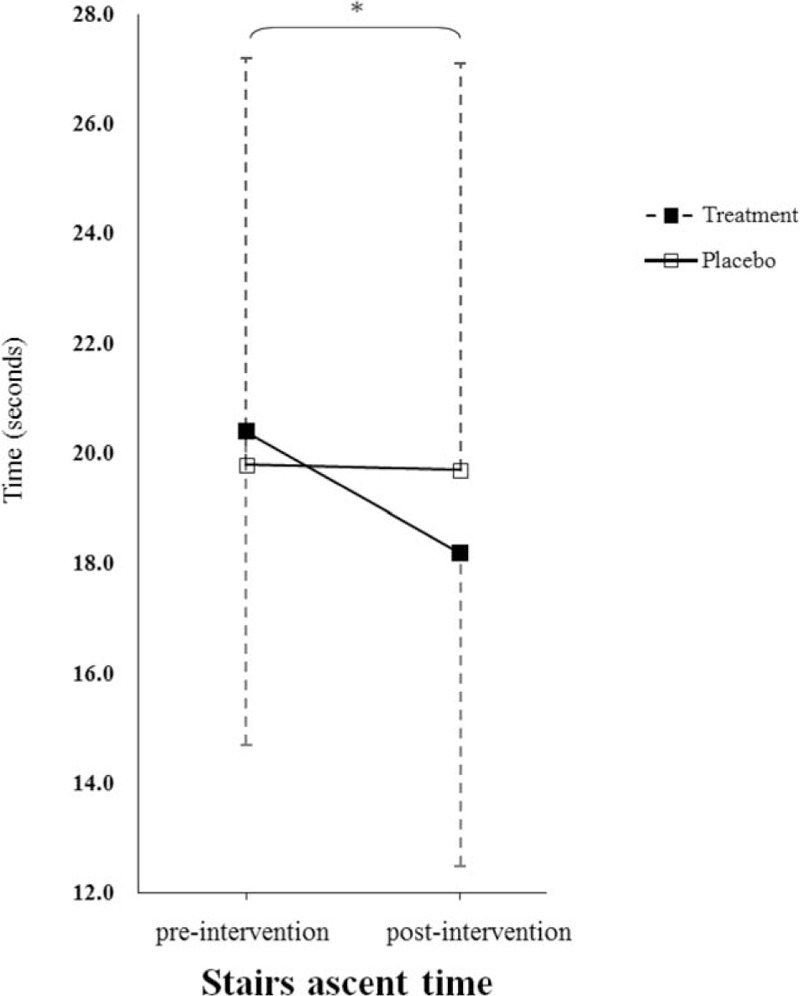
Mean and standard deviation of changes of stair ascent time associated with insole use for 12 weeks. Solid square, treatment group; hollow square, placebo group. ∗P < .05.
4. Discussion
This study applied the ICF framework to investigate the short-term effects of customized arch support insoles on both body functions and structures, and activities and participation in children with symptomatic flexible flatfoot. Although the groups were not comparable, we found that children with symptomatic flexible flatfoot who wore customized insoles for 12 weeks exhibited improved pain/comfort, physical health, stair ascent time, upper extremity and physical function, and transfer and basic mobility, which belong to the domains of body functions and structures and activity and participation in the ICF framework. However, wearing the insoles did not improve walking speed, timed up and go and chair rise test times, global functions, and psychosocial health.
Individuals with flexible flatfoot exhibit altered lower extremity kinetics and kinematics.[3,31] Compared with prefabricated insoles, custom-molded total-contact insoles have been proven to be efficient in reducing soft tissue strain and plantar pressure.[32] The feet of children have a higher percentage of polyglycans and elastic fibers and have less developed collagen cross-connections.[26] Sinha et al reported that children with flatfoot who wore a medial arch orthosis exhibited improved pain scores and foot angles compared with controls (who did not wear insoles).[33] However, the control group was not a true control because these children received analgesics during the intervention period. Different materials, designs, hardness levels, textures, contact areas, and even practitioners can influence the effects of insoles.[32,34,35] In the present study, we assessed the effects of customized, hard, arch support insoles, which were molded by the same qualified senior specialist in physical and rehabilitation medicine, in maintaining the subtalar joint in the neutral position.
Persistent subtalar joint pronation during the propulsive phase has been recognized as a possible factor contributing to major medical conditions in adult life, such as hallux valgus, tarsal tunnel syndrome, metatarsalgia, posterior tibialis tendon dysfunction, osteoarthritis of the midtarsal and subtalar joints, Achilles tendinopathy, patellofemoral joint pain, and lower back pain.[31,36,37] The surgical treatment of flexible flatfoot in children has been reported to improve biomechanics and correct deformities.[38] However, surgical intervention is associated with high costs and the risks of complications.
Compared with children without flatfoot, children with flatfoot were revealed to exhibit a dynamic functional abnormality of the lower extremity, including slower walking and poorer performance of physical tasks.[2] Moreover, flatfoot causes pain, restricted mobility, fatigue after prolonged walking, gait disturbance, and compromised QOL.[2,33] In the current study, we demonstrated significant improvement in pain/comfort in children wearing insoles for 12 weeks compared with those who did not wear insoles. Decreased symptoms related to flexible flatfoot was observed in up to 76% of the children in the treatment group. Children with flatfoot wearing insoles exhibited improved stair ascent time and transfer and basic mobility, which belong to the domain of activities. Stair ascent and transfer and basic mobility are common dynamic activities of daily living in children. In children with symptomatic flexible flatfoot, wearing insoles decreased symptoms and increased activities which might further contribute to improvement in physical health, rather than psychosocial health. However, we could not rule out the possibility that the increased activity was not necessarily caused by the insoles and might be caused by other reasons, such as more favorable weather or parents being more aware of the importance of physical activity.
Children may wear various shoes at different times, depending on their personal preference and comfort.[25] Numerous types of shoes exist, such as lightweight, soft versus rigid, stability, conventional walking, and athletic shoes.[39] In the present study, we instructed the children to wear self-selected comfortable shoes with a flat sole, rigid high-heel counter, and widened toe box with Velcro. However, an insole and shoe constitute 1 unit. Different shoes may have different effects on the foot position. Additional studies examining various shoe type and insole combinations should be conducted.
The strength of the present study is that the topic of the study is of importance to practitioners, given the high number of presentations to orthopedic services that are related to lower limb conditions (approximately 35%),[40] and parental concerns regarding foot development are high on that list.[41] To the best of our knowledge, this paper also appears to be original in terms of participants and outcome measure approaches. The result is potentially valuable within the body of existing evidence, particularly for practitioners, policymakers, and those presenting with symptoms of flexible flatfoot. The use of insoles or orthotics for flatfoot treatment appears to be a common practice,[42] although limited evidence supports this practice in nonpathological pediatric populations.[43] Nevertheless, (potentially) justifiable concerns exist regarding the methodology of the available evidence; this observation suggests that existing studies have generally included nonsymptomatic participants, measured outcomes that have not all been related to activities of daily living, and used types of insole or orthosis that are different from those prescribed in clinical practice.[44] Therefore, much of the existing literature has limited external validity for practitioners working with adults or children with symptomatic flatfoot. This research addresses 2 of these concerns by including symptomatic participants and outcome measures that are valid and reliable indicators of function and disability.
4.1. Study limitations
This study has some limitations. First, although randomization was used to minimize the effect of any unknown confounding variables, some baseline differences were observed in scores between the groups. It should be noted that the 2 groups were not comparable, which may affect the study results. To exclude the possible ceiling effect in the control group, we further performed an efficiency analysis. The observed efficiency remained statistically higher in the treatment group than in the control group. However, a “regression to the mean” influence may, in part, still explain the greater effect size change in the treatment group. Second, a randomized double-blind clinical trial is the gold standard for methodology. In the present study, an investigator, blinded to group allocation, evaluated the participants at the baseline and follow-up assessment. However, parents answered the questionnaires and were aware whether their children received insoles or not. The participants and their parents were not blinded to insole treatment, and this may affect the responses to the questionnaires used as outcome measures. Thus, an ascertainment bias occurs because the results of a trial may be distorted by each participant's awareness of insole treatment.[45] By contrast, demoralization may occur when the participants in the control group are resentful of not receiving any intervention. The use of sham orthoses may reduce the resentful demoralization.[45] However, previous studies have provided evidence for the different mechanical effects of sham insoles on the foot, because the materials used for manufacturing the sham insoles are not entirely inert mechanically.[46,47] Because not all sham orthoses are perceived as being equally credible or as having the same mechanical effects, we did not use sham insoles in the present study.[47] Third, we included participants in the age range of 3 to 10 years in this study. The arch continues to grow up to the age of approximately 6 years. Although making a distinction between developmental flatfoot, which improves in the first few years of life, and persistent flatfoot, which may exert life-long effects in children, is important, we included children in the age range of 3 to 6 year in the present study because these children already exhibited clinical symptoms. Fourth, we did not evaluate biomechanics. Therefore, the kinematics and kinetics associated with customized arch support insoles should be further investigated. Fifth, we did not choose an outcome measure specific to measure the primary compliant of the children/parents: pain and fatigue. Because the aim of the present study was to examine the effects of insoles on symptomatic flexible flat foot in children by ICF framework, we attempted to address pain and function in a generic manner by using PODCI and PedsQL. Therefore, the perceived effect of an intervention on the outcome measures cannot be rule out. Finally, we did not perform long-term follow-up for the children in this study. Whether the benefits observed during short-term follow-up are also observed after long-term follow-up remains unclear.
5. Conclusions
This study is the first to examine the short-term effects of modified arch support insoles in children with symptomatic flexible flatfoot by using the ICF framework. In this study, children with symptomatic flexible flatfoot wore the customized arch support insoles for 12 weeks to maintain the subtalar joint in the neutral position. We demonstrated that these children exhibited improved pain/comfort, physical health, stair ascent time, upper extremity and physical function, and transfer and basic mobility, which belong to the domains of body functions and structures, and activities and participation in the ICF framework. However, it should be noted that the groups were not comparable, and might not be compared on the effect or this was the results of the small sample. Additional double-blind randomized studies with larger sample sizes should be conducted.
Acknowledgments
The authors thank the research grants (SKH-8302-103-DR-36, SKH-8302-104-DR-29, SKH-8302-105-DR-24, SKH-8302-106-DR-28, and 2018SKHADR028; MOST 104-2314-B-002-118-MY3, MOST-102-2314-B-341-001, MOST 105-2314-B-002-049-MY3, MOST-105-2314-B-341-002, and MOST-106-2314-B-341-003-MY2) from Shin Kong Wu Ho-Su Memorial Hospital and the Ministry of Science and Technology, Taiwan, respectively, for the support.
Author contributions
Conceptualization: Ru-Lan Hsieh.
Data curation: Ru-Lan Hsieh.
Formal analysis: Wen-Chung Lee.
Funding acquisition: Ru-Lan Hsieh.
Investigation: Ru-Lan Hsieh, Hui-Ling Peng.
Methodology: Wen-Chung Lee.
Project administration: Ru-Lan Hsieh.
Supervision: Ru-Lan Hsieh.
Writing – original draft: Ru-Lan Hsieh.
Writing – review & editing: Ru-Lan Hsieh.
Footnotes
Abbreviations: ANCOVA = analysis of covariance, ICF = International Classification of Functioning, Disability, and Health, PedsQL = Pediatric Quality of Life Inventory-Generic Core Scale, PODCI = Pediatric Outcome Data Collection Instrument.
Funding/support: This study was partially supported by research grants (SKH-8302-103-DR-36, SKH-8302-104-DR-29, SKH-8302-105-DR-24, SKH-8302-106-DR-28, and 2018SKHADR028; MOST-102-2314-B-341-001, MOST 104-2314-B-002-118-MY3, MOST 105-2314-B-002-049-MY3, MOST-105-2314-B-341-002, and MOST-106-2314-B-341-003-MY2) from Shin Kong Wu Ho-Su Memorial Hospital and the Ministry of Science and Technology, Taiwan, respectively.
The authors have no conflicts of interest to disclose.
Trial registration number: ClinicalTrials.gov ID: NCT02414087.
References
- [1].Pauk J, Ezerskiy V, Raso JV, et al. Epidemiologic factors affecting plantar arch development in children with flat feet. J Am Podiatr Med Assoc 2012;102:114–21. [DOI] [PubMed] [Google Scholar]
- [2].Lin CJ, Lai KA, Kuan TS, et al. Correlating factors and clinical significance of flexible flatfoot in preschool children. J Pediatr Orthop 2001;21:378–82. [PubMed] [Google Scholar]
- [3].Shih YF, Chen CY, Chen WY, et al. Lower extremity kinematics in children with and without flexible flatfoot: a comparative study. BMC Musculoskelet Disord 2012;13:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Evans AM, Rome K. A Cochrane review of the evidence for non-surgical interventions for flexible pediatric flat feet. Eur J Phys Rehabil Med 2011;47:69–89. [PubMed] [Google Scholar]
- [5].Pfeiffer M, Kotz R, Ledl T, et al. Prevalence of flat foot in preschool-aged children. Pediatrics 2006;118:634–9. [DOI] [PubMed] [Google Scholar]
- [6].Jane MacKenzie A, Rome K, Evans AM. The efficacy of nonsurgical interventions for pediatric flexible flat foot: a critical review. J Pediatr Orthop 2012;32:830–4. [DOI] [PubMed] [Google Scholar]
- [7].Chen YC, Lou SZ, Huang CY, et al. Effects of foot orthoses on gait patterns of flat feet patients. Clin Biomech (Bristol, Avon) 2010;25:265–70. [DOI] [PubMed] [Google Scholar]
- [8].Gerold S, Mauro Z, Alvydas J, et al. Practice, Science and Governance in Interaction: European Effort for the System-Wide Implementation of the International Classification of Functioning, Disability and Health (ICF) in Physical and Rehabilitation Medicine. Eur J Phys Rehabil Med 2017;53:299–307. [DOI] [PubMed] [Google Scholar]
- [9].Tang SF, Chen CH, Wu CK, et al. The effects of total contact insole with forefoot medial posting on rearfoot movement and foot pressure distributions in patients with flexible flatfoot. Clin Neurol Neurosurg 2015;129suppl 1:S8–11. [DOI] [PubMed] [Google Scholar]
- [10].Karimi MT, Fereshtehnejad N, Pool F. The impact of foot insole on the energy consumption of flat-footed individuals during walking. Foot Ankle Spec 2013;6:21–6. [DOI] [PubMed] [Google Scholar]
- [11].LeCursi N. Sports shoes and orthoses. DeLee & Drez's Orthop Sports Med 2015;115:1384–91e2. [Google Scholar]
- [12].Romeo DM, Lucibello S, Musto E, et al. Assessing joint hypermobility in preschool-aged children. J Pediatr 2016;176:162–6. [DOI] [PubMed] [Google Scholar]
- [13].Kumar B, Lenert P. Joint hypermobility syndrome: recognizing a commonly overlooked cause of chronic pain. Am J Med 2017;130:640–7. [DOI] [PubMed] [Google Scholar]
- [14].Cheng JC, Chan PS, Hui PW. Joint laxity in children. J Pediatr Orthop 1991;11:752–6. [DOI] [PubMed] [Google Scholar]
- [15].Ferrari J, Parslow C, Lim E, et al. Joint hypermobility: the use of a new assessment tool to measure lower limb hypermobility. Clin Exp Rheumatol 2005;23:413–20. [PubMed] [Google Scholar]
- [16].Adhikari U, Arulsingh W, Pai G, et al. Normative values of navicular drop test and the effect of demographic parameters – a cross sectional study. Ann Biol Res 2014;5:40–8. [Google Scholar]
- [17].Weiner-Ogilvie S, Rome K. The reliability of three techniques for measuring foot position. J Am Podiatr Med Assoc 1998;88:381–6. [DOI] [PubMed] [Google Scholar]
- [18].Redmond AC, Crosbie J, Ouvrier RA. Development and validation of a novel rating system for scoring standing foot posture: the Foot Posture Index. Clin Biomech (Bristol, Avon) 2006;21:89–98. [DOI] [PubMed] [Google Scholar]
- [19].Evans AM, Nicholson H, Zakarias N. The paediatric flat foot proforma (p-FFP): improved and abridged following a reproducibility study. J Foot Ankle Res 2009;2:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Murley GS, Menz HB, Landorf KB. A protocol for classifying normal-and flat-arched foot posture for research studies using clinical and radiographic measurements. J Foot Ankle Res 2009;2:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Levinger P, Menz HB, Fotoohabadi MR, et al. Foot posture in people with medial compartment knee osteoarthritis. J Foot Ankle Res 2010;3:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Root M, Orien W, Weed J. Normal and abnormal function of the foot. Los Angeles: Clinical Biomechanics Corp; 1977:2. [Google Scholar]
- [23].Hsieh RL, Lee WC. Immediate and medium-term effects of custom-moulded insoles on pain, physical function, physical activity, and balance control in patients with knee osteoarthritis. J Rehabil Med 2014;46:159–65. [DOI] [PubMed] [Google Scholar]
- [24].Hsieh RL, Lee WC. Clinical effects of lateral wedge arch support insoles in knee osteoarthritis: a prospective double-blind randomized study. Medicine (Baltimore) 2016;95:e3952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Walther M, Herold D, Sinderhauf A, et al. Children sport shoes – a systematic review of current literature. Foot Ankle Surg 2008;14:180–9. [DOI] [PubMed] [Google Scholar]
- [26].Bennell KL, Bowles KA, Payne C, et al. Lateral wedge insoles for medial knee osteoarthritis: 12 month randomised controlled trial. BMJ 2011;342:d2912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Hsieh RL, Lin MI, Huang HY, et al. The relationship between the Pediatric Outcomes Data Collection Instrument and functional impairment in developmentally delayed Chinese children and their parents’ health: implications for child and family-centered medicine. Int J Pers Cent Med 2011;1:1–8. [Google Scholar]
- [28].Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care 1999;37:126–39. [DOI] [PubMed] [Google Scholar]
- [29].Chan LF, Chow SM, Lo SK. Preliminary validation of the Chinese version of the Pediatric Quality of Life Inventory. Int J Rehabil Res 2005;28:219–27. [DOI] [PubMed] [Google Scholar]
- [30].Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edHillsdale, NJ: L. Erlbaum Associates; 1988. [Google Scholar]
- [31].Kim M-K, Lee Y-S. Kinematic analysis of the lower extremities of subjects with flat feet at different gait speeds. J Phys Ther Sci 2013;25:531–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Vie B, Nester CJ, Porte LM, et al. Pilot study demonstrating that sole mechanosensitivity can be affected by insole use. Gait Posture 2015;41:263–8. [DOI] [PubMed] [Google Scholar]
- [33].Sinha S, Song HR, Kim HJ, et al. Medial arch orthosis for paediatric flatfoot. J Orthop Surg (Hong Kong) 2013;21:37–43. [DOI] [PubMed] [Google Scholar]
- [34].Bergera L, Rossi J, Domenge F, et al. Effects of therapeutic shoes on plantar pressure distribution on healthy subjects. Ann Phys Rehabil Med 2014. 57. [Google Scholar]
- [35].Lane TJ, Landorf KB, Bonanno DR, et al. Effects of shoe sole hardness on plantar pressure and comfort in older people with forefoot pain. Gait Posture 2014;39:247–51. [DOI] [PubMed] [Google Scholar]
- [36].Yagerman SE, Cross MB, Positano R, et al. Evaluation and treatment of symptomatic pes planus. Curr Opin Pediatr 2011;23:60–7. [DOI] [PubMed] [Google Scholar]
- [37].Vukašinović Zoran S, Spasovski Duško V, Matanović Dragana D, et al. Flatfoot in children. Acta Chir Iugosl 2011;58:103–6. [PubMed] [Google Scholar]
- [38].Giannini BS, Ceccarelli F, Benedetti MG, et al. Surgical treatment of flexible flatfoot in children a four-year follow-up study. J Bone Joint Surg Am 2001;83-ASuppl 2 Pt 2:73–9. [DOI] [PubMed] [Google Scholar]
- [39].Shakoor N, Lidtke RH, Sengupta M, et al. Effects of specialized footwear on joint loads in osteoarthritis of the knee. Arthritis Rheum 2008;59:1214–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Jordan KP, Kadam UT, Hayward R, et al. Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskelet Disord 2010;11:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Rome K, Ashford R, Evans A. Non-surgical interventions for paediatric pes planus. Cochrane Database Syst Rev 2010. CD006311. [DOI] [PubMed] [Google Scholar]
- [42].Bennett PJ. Types of foot problems seen by Australian podiatrists. Foot 2012;22:40–5. [DOI] [PubMed] [Google Scholar]
- [43].Whitford D, Esterman A. A Randomized controlled trial of two types of in-shoe orthoses in children with flexible excess pronation of the feet. Foot Ankle Int 2007;28:715–23. [DOI] [PubMed] [Google Scholar]
- [44].Banwell H, Mackintosh S, Thewlis D. Foot orthoses for adults with flexible pes planus: a systematic review. J Foot Ankle Res 2014;7:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Bonanno DR, Landorf KB, Murley GS, et al. Selecting control interventions for use in orthotic trials: the methodological benefits of sham orthoses. Contemp Clin Trials 2015;42:257. [DOI] [PubMed] [Google Scholar]
- [46].Halstead J, Chapman GJ, Gray JC, et al. Foot orthoses in the treatment of symptomatic midfoot osteoarthritis using clinical and biomechanical outcomes: a randomised feasibility study. Clin Rheumatol 2016;35:987–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].McCormick CJ, Bonanno DR, Landorf KB. The effect of customised and sham foot orthoses on plantar pressures. J Foot Ankle Res 2013;6:19. [DOI] [PMC free article] [PubMed] [Google Scholar]


