Abstract
Rationale:
Focal myositis (FM) is a very rare myopathy of unknown etiology characterized by focal enlargement within one single skeletal muscle. In particular, it occurs only involving the Sartorius muscle has never been reported.
Patient concerns:
A 25-year-old man was admitted to the hospital with progressive restricted left hip joint extension, left thigh discomfort and gait disturbance for 6 years.
Diagnoses:
Combining clinical manifestations with results of radiological and pathological examinations, it was consistent with the diagnosis of FM
Interventions:
The patient received a surgery under general anesthesia to release the contracted Sartorius tendon.
Outcomes:
The range of motion of the patient's left hip and ipsilateral knee has significantly improved as well as the discomfort of his left thigh relieved obviously after the surgery.
Lessons:
This case report is the first to report FM presenting as sartorius muscle contracture and the surgery is an alternative therapy for these patients.
Keywords: focal myositis, joint contracture, Sartorius muscle
1. Introduction
Focal myositis (FM) is a rare, benign myopathy characterized by focal inflammatory pseudotumor of the skeletal muscle, which was initially reported in 1977 by Heffner et al[1]. The etiology of FM has not been clarified well and possible triggering factors include genetic susceptibility, nerve lesions, mechanical lesions, and some immunological or infectious diseases.[2–4] It mostly occurs at the lower extremities but can also involve the muscles from the other locations including the neck and the head. Generally, the blood tests and other laboratory examinations are usually within normal ranges. The magnetic resonance imaging (MRI) is one of the most useful methods for diagnosis as it usually showed abnormal signal intensity of the involved muscle. Most cases could improve spontaneously within a few months. In addition, muscle pain and some minor complications can relieved by some conservative treatments such as nonsteroidal antiinflammatory drugs (NSAIDs), physiotherapy, and steroid treatment. However, if these conservative measures failed and the patient's quality of life is greatly affected, appropriate surgical treatments should be adopted.[5]
2. Case report
A 25-year-old man visited our clinic with a chief complaint of progressive restricted left hip joint extension, left thigh discomfort and gait disturbance for 6 years. The patient received the NSAIDs in other hospitals but did not work. There were no other symptoms and no history of trauma, recent surgery and special disease, the related family history is absent too. On physical examination, the patient walked with a limp gait and showed flexion contracture of his left hip (Fig. 1). The range-of-motion (ROM) test revealed limitation of extension, abduction, and external rotation of the affected hip. With the development of the disease, his left knee joint was also affected that could not straighten completely. The circumference of the left thigh was the same as the right one and no shortening deformity of the left lower limb observed. He had no muscle weakness and sensory disturbance of both extremities. Blood tests indicated blood routine, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), serum creatinine kinase (CK) and some infection markers like HIV, hepatitis B and C were within normal ranges. The rheumatoid factor (RF) and other antinuclear antibodies were also negative. Plain radiographs of the pelvis and lower extremities plus computed tomography (CT) of the left femur did not show any bony lesion. The fibrosis and degeneration of the left Sartorius muscle without echogenic foci was detected on ultrasonography. MRI scan of the left thigh revealed the slightly enlarged left Sartorius muscle. On T2-weighted images (T2WI), diffuse hyperintense signal presented within the left Sartorius with no involvement of adjacent muscles. On T1-weighted unenhanced images, the thickened Sartorius displayed diffuse isointense signal and patchy hypointense signal (Fig. 2). There is a “combed” contrast enhancement after gadolinium injection.
Figure 1.

The patient's lower limbs appearance before the operation. (A) The patient is in supine position; (B) the patient is in standing position. The left hip and left knee is obvious flexion deformity and localized mass involving the left Sartorius.
Figure 2.
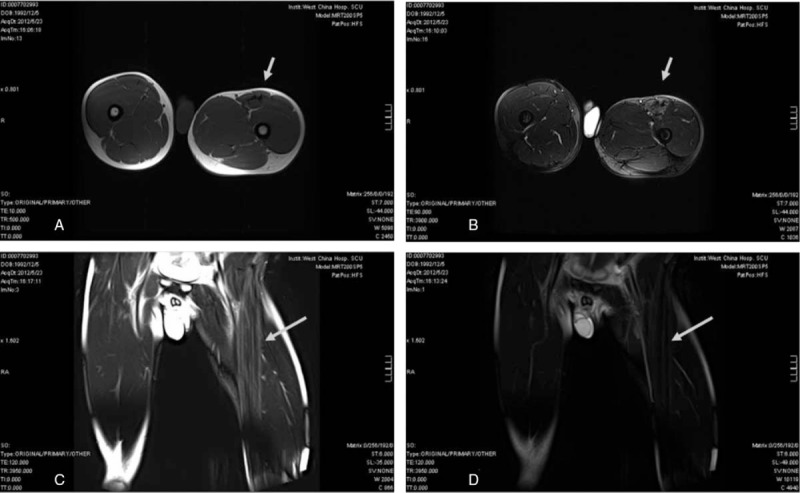
Magnetic resonance imaging (MRI) of the lower limbs. (A) and (B) Transverse T1-weighted image and T2-weighted image. Coronal T2-weighted image (C) and T2 STIR image (D). The results show the slightly enlarged left Sartorius muscle and diffuse high signal intensities within the left Sartorius (arrow in B and C).
Given the long course of the disease, failed conservative treatments due to obvious Sartorius contracture, we operated a surgery under general anesthesia to release the contracted Sartorius tendon and a pathological examination of the involved muscle performed. We took a 10 cm long incision in the middle of the left groin and exposure of the left Sartorius revealed an enlargement of the Sartorius belly and fibrosis of the lateral half muscle belly without calcification. We resected a 2 cm long belly for biopsy and found the contracture of the deep myolemma. Then we resected the contracture band and the flexion and external rotation deformity of the left lower extremity got clearly corrected. Neuropathology indicated marked variation of fiber size, focal fibrosis, necrosis of fibers and interstitial fibrosis accompanied by chronic inflammatory cells infiltrating. The immunohistochemistry results showed the major histocompatibility complex type 1 (MHC-1) antigen are focally and faintly expressed (Fig. 3).
Figure 3.
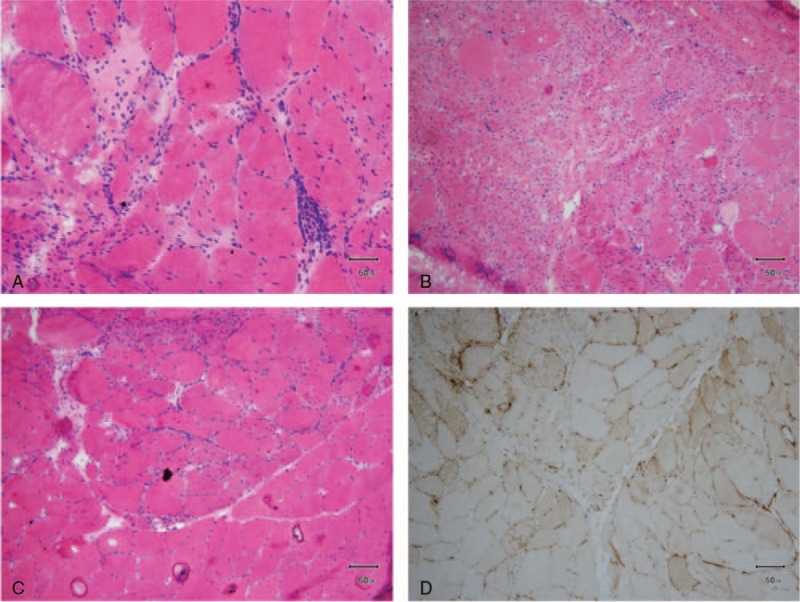
The results of the immunohistochemistry examinations. (A–C) The monocyte-based inflammatory infiltrates and the localized myositis. The major histocompatibility complex type 1 (MHC-1) antigen are focally and faintly expressed (D).
In summary, combining clinical manifestations with results of radiological and pathological examinations, it was consistent with the diagnosis of FM. On follow-up at 5 months, the patient was satisfied and the ROM of his left hip and ipsilateral knee has significantly improved as well as the discomfort of his left thigh relieved obviously during the rehabilitation.
3. Discussion
There have been approximately 200 cases about FM reported all over the world.[6] It is a rare disease characterized by inflammatory myopathy, which usually occurred at the lower extremities. According to previously reported statistics, FM can occur at any age (7–94 years old) especially the mid-adult age, with no gender difference.[6,7] The etiology remains unknown although it may be associated with genetic vulnerability, trauma, viral infection, nerve lesions, and immunological diseases. Moreover, FM may be a local form of the polymyositis has been reported.[8] In our case, it occurs in the unilateral Sartorius muscle without a history of injury or infection. To the best of our knowledge, this is the first case of FM in the Sartorius muscle reported in the world.
FM commonly presents as a circumscribed painful mass or swelling within one single muscle. However, involvement of 2 or more muscles were reported in some cases.[9] In the current case, it involves only one muscle and leads to Sartorius contracture without a painful soft tissue mass. Meaningfully, this presentation is hitherto the first report of Sartorius contracture in human that proved by both radiographic and pathological evidence except for 2 cases occurred in dogs due to ossificans myositis. MRI is one of the key tools for diagnosis. A typical appearance of FM is hyperintense on T2WI, isointense or slightly hypointense on T1-weighed unenhanced images and patchily contrast enhanced after gadolinium injection. The hallmarks of pathological features in FM include obvious variation in fiber size, inflammatory infiltrates, fiber degeneration/regeneration, and interstitial fibrosis. Actually, FM can mimic a myositis of other origin morphologically. The pathological result must be combined with clinical presentation and radiological evidence. FM should be differentiated from soft tissue tumors, myositis ossificans, polymyositis, and so on.[10,11] Myositis ossificans is essentially a heterotopic ossification that characterized by metaplasia with calcification morphologically. Polymyositis shows symmetrical involvement of the proximal muscles, marked increased CK level and MHC-1 positive expression. While FM will usually not have systemic symptoms like fever, muscle weakness, and weight loss.
Medical treatments are often unnecessary because FM is a self-limited disease and the recurrence rate is about 1% to 18%.[12] However. If the motion of the adjacent joint is limited, surgical therapy may be an alternative especially in the case of unclear diagnosis.[13] Gigante et al[14] also suggested that conservative methods including medications should be the first choice for FM in pediatric age and that surgery should be strictly reserved for selected cases where noninvasive methods have previously failed. Snell and Dowd[15] reported a case of recurrent FM presenting as flexion contractures of the fingers which had an over 3-year course. They resected the affected tissue and got a short-term, favorable clinical effect. Whilst, Jun et al[9] described a case of FM with ankle contracture which had developed 6 weeks previously. They treated with oral prednisolone and physical therapy and gained a good performance.
Our patient had suffered for 6 years and urged a surgical treatment due to the significantly limited motion and pervious failed nonsurgical methods, so we performed the proximal release in contracture of the Sartorius to relieve his symptoms and resected partial affected tissues for biopsy. All the collective results were consistent with a diagnosis of FM. Moreover, the clinical outcome is satisfactory in 5 months after surgery.
Given the unclear cause of our case and the FM located in Sartorius is very rare, we hope this case report will be helpful in diagnosis and treatment of the FM. In addition, longer-term follow-ups needed to evaluate the effectiveness of the surgery and monitor the recurrence.
Author contributions
Conceptualization: Jun Xia.
Data curation: Leiguang Zhao, Juyang, Jiao.
Investigation: Jin Wang, Jingsheng Shi.
Methodology: Guanglei Zhao.
Resources: Juyang Jiao.
Supervision: Jun Xia.
Writing – original draft: Jin Wang.
Writing – review & editing: Jun Xia, Jin Wang, Juyang Jiao.
Footnotes
Abbreviations: CK = serum creatinine kinase, CRP = C-reactive protein, CT = computed tomography, ESR = erythrocyte sedimentation rate, FM = focal myositis, MHC-1 = major histocompatibility complex type 1, MRI = magnetic resonance imaging, NSAIDs = nonsteroidal antiinflammatory drugs, RF = rheumatoid factor, ROM = range of motion, T1WI = T1-weighted images, T2WI = T2-weighted images.
JW and JJ contributed equally to this work and should be considered co-first authors.
Informed consent: We have obtained written informed consent from the patient in this case report.
Ethical approval: The study was approved by the Ethics Committees of Huashan Hospital, Fudan University.
The authors have no conflicts of interest to disclose.
References
- [1].Heffner RR, Jr, Armbrustmacher VW, Earle KM. Focal myositis. Cancer 1977;40:301–6. [DOI] [PubMed] [Google Scholar]
- [2].Sekiguchi K, Kanda F, Oishi K, et al. HLA typing in focal myositis. J Neurol Sci 2004;227:21–5. [DOI] [PubMed] [Google Scholar]
- [3].Alkhawajah NM, Kiehl TR, Bril V. Ischaemia due to a vascular malformation causing focal myositis. BMJ Case Rep 2014;2014:bcr2013202442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Dawson JK, Davidson JE. Focal myositis due to Campylobacter infection. Rheumatology (Oxford, England) 2001;40:704–6. [DOI] [PubMed] [Google Scholar]
- [5].Maynie M, Robert H, Eloit S, et al. [Focal myositis in children. Apropos of a case]. Rev Chir Orthop Reparatrice Appar Mot 1997;83:382–6. [PubMed] [Google Scholar]
- [6].Auerbach A, Fanburg-Smith JC, Wang G, et al. Focal myositis: a clinicopathologic study of 115 cases of an intramuscular mass-like reactive process. Am J Surg Pathol 2009;33:1016–24. [DOI] [PubMed] [Google Scholar]
- [7].Gaeta M, Mazziotti S, Minutoli F, et al. MR imaging findings of focal myositis: a pseudotumour that may mimic muscle neoplasm. Skeletal Radiol 2009;38:571–8. [DOI] [PubMed] [Google Scholar]
- [8].Flaisler F, Blin D, Asencio G, et al. Focal myositis: a localized form of polymyositis? J Rheumatol 1993;20:1414–6. [PubMed] [Google Scholar]
- [9].Jun J, Im S, Park JH, et al. Focal myositis of unilateral leg. Ann Rehabil Med 2011;35:944–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Smith AG, Urbanits S, Blaivas M, et al. Clinical and pathologic features of focal myositis. Muscle Nerve 2000;23:1569–75. [DOI] [PubMed] [Google Scholar]
- [11].Marie I, Sauvetre G, Becker S, et al. Clinical images: focal myositis demonstrated on positron emission tomography. Arthritis Rheumatol 2014;66:1871. [DOI] [PubMed] [Google Scholar]
- [12].Yanmaz Alnigenis MN, Kolasinski SL, Kalovidouris AE. Focal myositis: a review of 100 previously published cases and a report of 2 new cases. Clin Exp Rheumatol 1999;17:631. [PubMed] [Google Scholar]
- [13].Milani GP, Mazzoni MBM, Gatti H, et al. Recurrent focal myositis in childhood: a case report and systematic review of the literature. Pediatr Neurol 2017;71:77.e1–81.e1. [DOI] [PubMed] [Google Scholar]
- [14].Gigante C, Corradin M, Alaggio R. Focal Myositis in paediatric age. Muscles Ligaments Tendons J 2015;5:45–50. [PMC free article] [PubMed] [Google Scholar]
- [15].Snell BJ, Dowd M. Recurrent focal myositis presenting as flexion contractures of the fingers. J Hand Surg Eur Vol 2007;32:714. [DOI] [PubMed] [Google Scholar]


