Abstract
Background:
Chronic constipation is described as a common complication determined by difficult and/or rare passage of stool or both. The difference in definition of constipation has led to a wide range of reported prevalence (i.e., between 1% and 80%). Various factors are involved in the pathogenesis of the disease, including type of diet, genetic predisposition, colonic motility, absorption, social economic status, daily behaviors, and biological and pharmaceutical factors. Diagnostic and therapeutic options play a key role in the treatment of chronic constipation. There are still debates about the timing of these diagnostic and therapeutic algorithms.
Methods:
A systematic and comprehensive search will be performed using MEDLINE, PubMed, EMBASE, AMED, the Cochrane Library and Google Scholar. Better understanding of the pathophysiology of chronic constipation and efficacy of pharmacological agent can help physicians for treating and managing symptoms.
In this study, some of the old and new therapies in the treatment of chronic constipation have been studied based on the controlled studies and strong evidence. We are trying to address some of the controversial issues to manage the disease and to provide appropriate diagnostic options in an efficient and cost-effective way.
Results:
The results of this systematic review will be published in a peer-reviewed journal.
Conclusion:
To our knowledge, our study will provide an overall estimate of chronic constipation to assess controversial issues, available diagnostic and therapeutic strategies of chronic constipation.
Ethics and dissemination:
Ethical approval and informed consent are not required, as the study will be a literature review and will not involve direct contact with patients or alterations to patient care.
Keywords: clinical presentation, constipation, controversial issues, diagnostic and therapeutic strategies
1. Introduction
Constipation is a disorder in the gastrointestinal tract, which can result in the infrequent stools, difficult stool passage with pain and stiffness. Acute constipation may cause closure of the intestine, which may even require surgery.[1]
It is worth noting that there is currently no ideal definition for constipation; thus, history and physical examination can be considered the main initial approaches. Many definitions are described by using a self-reported constipation and the formal criteria. Many definitions of chronic constipation are related to scientific considerations such as secondary causes (medications), neurological, or systemic diseases. However, it is considered primary or idiopathic.[1]
Pathogenesis is multifactorial with focusing on genetic predisposition, socioeconomic status, low fiber consumption, lack of adequate fluid intake, lack of mobility, disturbance in the hormone balance, side effects of medications, or anatomy of the body, etc.[1]
Constipation is a common gastrointestinal problem, which causes many expenses for the community with an estimated prevalence of 1% to 80%, worldwide,[2] where the condition is characterized by a wide geographical variation. It is noteworthy that the varieties of definitions have led to a wide range of prevalence.
Chronic constipation is a complicated condition among older individuals, which is characterized by difficult stool passage.[3] In this regard, this condition has a close relationship with the patients’ quality of life,[4] and consuming health resources.[5,6]
In this regard, we aimed to perform an integrative review of the literature to provide a better understanding of the pathophysiology of chronic constipation. As a matter of fact, appropriate understanding of this disease can play a key role in managing disease and planning better treatments. The main sources selected from bibliographic databases include PubMed, Scopus, Science Direct, and Google Scholar, etc. Details of the keywords were applied to find the best resources. This study is a review article dealing with chronic constipation, which is a topic with several causes.
1.1. Prevalence and risk factors of constipation
The definition of constipation is different among studies, where most studies are based on a questionnaire and may result from an organic condition. Overall, the average prevalence of constipation in adults has been estimated as 16% worldwide (varies between 0.7% and 79%); whereas the prevalence of 33.5% was attributed to adults aged 60 to 110 years. This heterogeneous condition is correlated with the patient quality of life,[4] and healthcare resource consumption.[5] The prevalence of constipation in Iran ranged from 1.4% to 37%, while the prevalence of functional constipation was determined as 24.2%.[7] Epidemiological studies have revealed that high prevalence of chronic constipation is associated with age progression, as far as we know.[8,9]
1.2. Age and gender distribution
Constipation among older people is far more common than younger people. Common causes of constipation in the elderly are linked to several factors including lack of normal bowel movements or aging, lack of proper diet, lack of adequate fluid intake, lack of adequate physical activity, illness or the use of drugs. The prevalence of this condition is higher in adults over 65 years of age due to a loose-fitting dentures or tooth loss, resulting in chewing difficulty, which forces the patient to select soft and soft fiber materials. Low-fiber foods are consumed by those who have lost their interest or are having difficulty swallowing.
The prevalence of anatomic abnormalities such as rectocele, pelvic floor dyssynergia, and prolapse, was reported to be higher in the elderly.[7] On the other hand, constipation is more common in women than in men. Moreover, severe constipation is markedly seen in elderly women as compared with that of male individuals.[10] During pregnancy, especially in the last months, the risk of constipation is high due to a significant increase of sex hormones, a decreased intestinal movement and delayed intestinal emptying because of mechanical pressure.
It has been reported that women are more likely to suffer from constipation in the premenopausal period, where it may be related to fluctuations in female sexual hormones and feelings. Furthermore, the use of laxatives is much more likely in women when they are seeking more health care for constipation.[11]
1.3. Causes of constipation
Pathogenesis is multifactorial with focusing on the type of diet, genetic predisposition, colonic motility, and absorption, as well as behavioral, biological, and pharmaceutical factors.[12] Furthermore, low fiber dietary intake, inadequate water intake, sedentary lifestyle, irritable bowel syndrome (IBS), failure to respond to urge to defecate, and slow transit have been revealed to be associated with predisposition (Table 1).
Table 1.
Common causes of constipation.
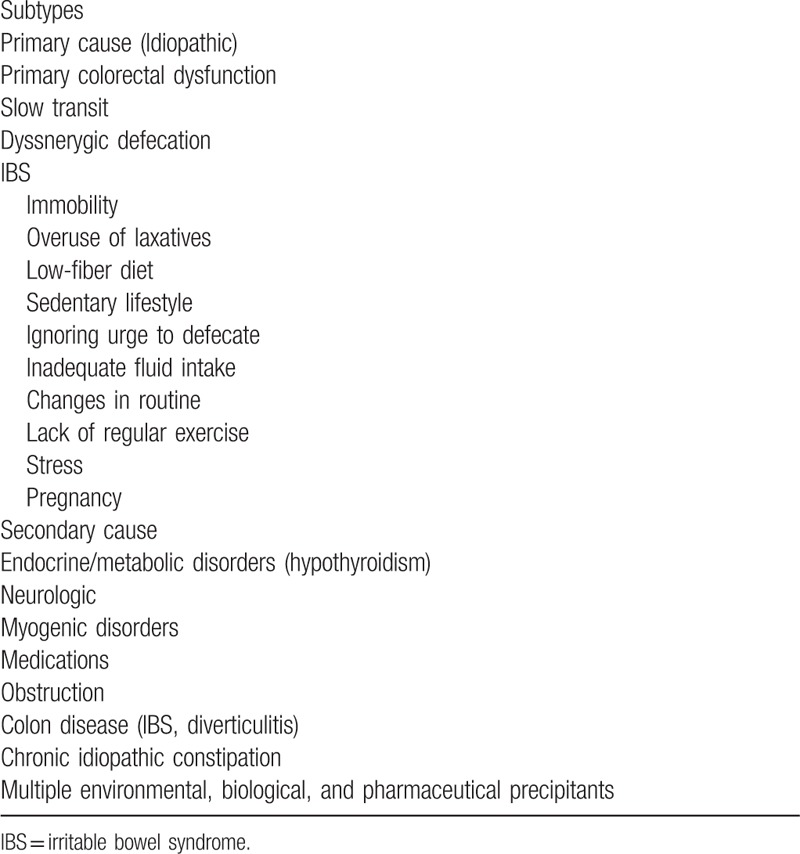
Overall, a number of factors contribute to constipation including lower social economic status, lower parental education, physical activity, medications, depression, physical and sexual abuse, and everyday life events.[4,13–15]
The long list and heterogeneity of related factors indicate which many pathophysiological factors cause the same symptoms, and are often undetectable from early forms. Regarding the complex interactions of various pathophysiological factors, caution should be used in applying therapeutic strategies based on only one of them.
Different studies have investigated the effects of 1 factor on constipation, while their multiplicity, mutual interaction, and overlapping nature should be considered for avoiding oversimplification. The lack of a diet containing vegetables and low consumption of fluids can lead to constipation.
Some medications and physiological conditions (e.g., pregnancy and age) have been revealed to increase the risk of consumption. Moreover, a number of diseases are also associated with reduced movement, such as spinal cord injury or musculoskeletal disorders (muscular dystrophy), which are also common causes of this condition. Furthermore, some diseases of the large intestine have appeared to interfere with the movements of the colon, such as IBS, pelvic floor dysfunction, and depression disorders. It is worth noting that the following sections have provided the causes of constipation and other aspects.
1.4. Diet
Common causes of chronic constipation include a lack of fiber (inadequate consumption of fruits, vegetables, and other foods containing fibers), no sufficient drinking water or liquids. In these cases, constipation is usually not a serious problem and can be controlled and treated by correcting nutritional habits and lifestyles.
Studies have indicated that a high-fiber diet can increase stool weight, resulting in a decreased colon transit time, while poor-fiber diet induces constipation.[16] Moreover, it has been revealed that increased fiber diet could improve symptoms in patients with normal colonic transit and anorectal function, while constipated patients with delayed colonic transit patients have not improved by increasing dietary fiber.[17] Increasing fiber consumption does not make colonic transit normal, and may even worsen their symptoms through the fiber's metabolism as a result of the gas produced.[18] On the other hand, it has been demonstrated that diets with soluble fiber (i.e., psyllium or ispaghula), but not fiber insoluble diet (wheat Bran), can be associated with the improvement of the symptoms in chronic constipation.[19] A systematic review showed that soluble fiber improved constipation symptoms in IBS with varying effects on abdominal pain.[20]
1.5. Diseases and conditions as secondary cause of constipation
Mechanical cause of constipation: colon, rectal, or anal stricture, megacolon rectocele, intestinal pseudo obstruction, injured tissues, diverticulosis, and abnormal narrowing of the intestine or rectum.
Organic stenosis: cancer or cancer-related causes (e.g., colorectal cancer and tumor, intestinal radiation, etc.), diverticulitis, sigmoid or cecal volvulus, intestinal masses, inflammatory, and ischemic or surgical stenosis.
Psychological conditions: depression, anxiety, eating disease.
Enteric neuropathies: people with Hirschsprung disease are more susceptible to constipation, as well as to chronic intestinal pseudo-obstruction.
Neurological disorders: multiple sclerosis, Parkinson disease, stroke, spinal cord injury, paraplegia, spina bifida, and autonomic neuropathy.
Endocrine and metabolic conditions: diabetes mellitus, hypercalcemia, porphyria, hypothyroidism, hyperthyroidism, and pregnancy.
Myopathic disorders: scleroderma and amyloidosis.
Anorectal disorders: anal strictures, anal fissures, and hemorrhoids are anal diseases that delay the removal of stool and exacerbate chronic constipation due to pain during fecal excretion.
Connective tissue disorders: lupus.
Uncertain cause: idiopathic chronic constipation.
1.6. Medications
Several constipation-causing medications (Table 2) are indicated as causative agents of constipation including antipyretic drugs (e.g., morphine and codeine), anticholinergic drugs (Hyoscine), antidepressants (Imipramine and fluoxetine), antiepileptic drugs (e.g., phenytoin and carbamazepine), antipsychotics (haloperidol and clozapine), food supplements containing iron and calcium.
Table 2.
Medications associated with constipation.
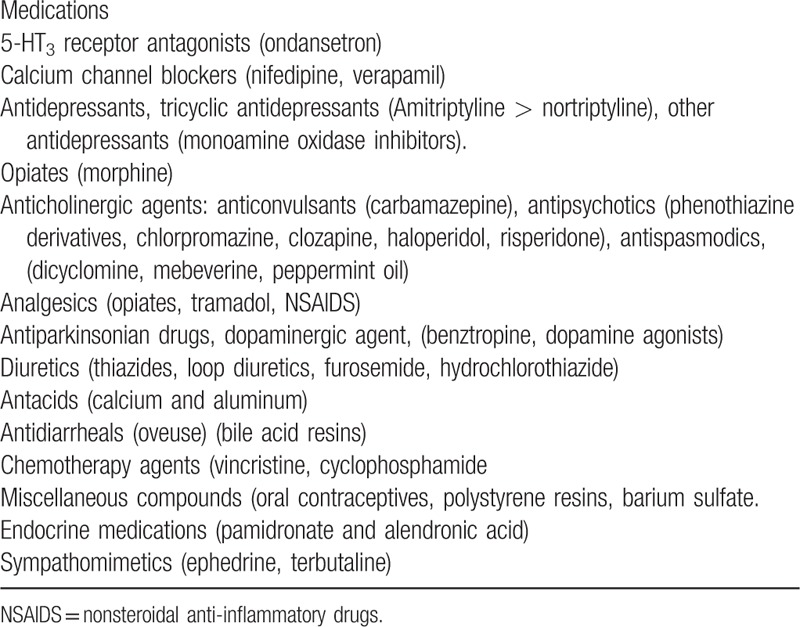
On the other hand, some blood pressure-lowering drugs, lipid-lowering drugs, muscle relaxant drugs, anti-ulcer drugs, antihistamines, and antioxidants (i.e., drugs containing aluminum and calcium) are commonly associated with constipation. Continuous consumption of opioids leads to chronic constipation in addicts. Opiate combinations weaken gastrointestinal motility movements and the susceptibility of rectal dilation to stimulation, whereas these increase the ileocecal tone and internal anal sphincter tone; thus prolonging the duration of excretion in the intestine, causing constipation.
1.7. Rectal sensorimotor dysfunction
Evidence suggests the role for rectal sensorimotor dysfunction as a factor in the symptoms in a proportion of patients who suffered from chronic constipation including sensation, motility, and biomechanical components. This condition is markedly related to functional evacuatory disorders and constipation. Most patients with preventable constipation complain of an evacuatory disorder.[21,22]
A number of factors are also involved in functional disorders of defecation and defined in patients with constipation including rectal hyposensitivity, altered rectoanal reflex activity, increased rectal duct capacity, and rectal motor dysfunction.[23] The role of abnormal visceral sensation is currently considered to be involved in the development of functional bowel disorders with considerable attention to visceral hypersensitivity,[23–25] whereas hyposensitivity was relatively considered. Hyposensitivity may occur in 1 quarter of adults with constipation, while one-third of these patients are involved in impairment of sensation due to a primary disorder of the afferent pathway. Attenuated sensory perception seems to be secondary factor in compliance/capacity change in adults.[23] These mentioned dysfunctions may be present together, which may vary depending on the degree of participation of the subject.
1.8. Psychoaffective disorders
Patients with constipation often have psychological disorders in a variety of stressful life events such as anxiety, depression, physical and sexual abuse, and anorexia nervosa, as well as a concomitant eating disorder.[4,13–15,26–29] It has been indicated that patients with chronic constipation, especially those with dyssynergic defecation, had had an important psychological disorder.[30]
In contrast, a study has reported that there is no relationship between psychological distress and stool frequency in patients with slow transit constipation.[31] However, it is complicated to determine how constipation is influenced by these factors.
1.9. Socioeconomic status
The impacts of socioeconomic status and educational level on the prevalence of constipation have been reported in most studies. Low-income people are more likely to suffer from constipation than their richer counterparts.[32–34] On the other hand, a reverse correlation between parental education and the incidence of constipation has been demonstrated in a number of investigations.[33,35,36] The socioeconomic status and educational level seem to be associated with these conditions in Iran.[7]
Other risk factors for constipation have also been reported in some studies, including a positive family history of constipation,[37,38] and living in a densely populated society.[36,38] However, there is a lack of consensus on some of the relevant factors in the literature.
1.10. Economic impact and the health-related quality of life
Constipation causes many physical and mental problems for many patients and can significantly affect the daily life and well-being of constipated individuals. Although a small proportion of constipated patients seek medical care, but most patients are taking medications to improve their condition.[39]
Healthcare costs among patients is significantly considerable, indicating that hundreds of millions dollars are annually spent on laxatives use. General health, mental health, and social function in people with constipation are lower than healthy subjects and are very low in hospitalized patients compared with the community.[11,40] Diagnosis and treatment of constipation impose a significant cost to the individual and the healthcare system, while constipation prevention programs will lead to cost savings.[41]
2. Diagnosis
2.1. Clinical presentation and evaluation
A number of criteria should be investigated in the clinical evaluation, including the frequency and consistency of stools, stool size, the duration of the symptoms, excessive obstruction, and history of ignoring a call to defecate, and feeling of incomplete evacuation or the use of hand palpation during defecation.[42] Clinical evaluation should be taken into consideration to identify specific symptoms of constipation (alarming symptoms), medical history, and organic causes, as well as medications.[43,44] On the other hand, the duration of this problem should be taken into account so that the duration of the problem may be helpful for the differentiation of the congenital defects from the causes in adolescents or young adults. Questions about the onset of constipation are valuable for obtaining useful etiologic information regarding changes in diet, medication, and related psychological problems. Alarm symptoms are characterized by changes in bowel habits after age 50, the acute onset of constipation in older individuals, blood mixed in the stool, weight loss, anemia, inflammatory bowel disease, symptoms of organic disorder and a strong family of colorectal cancer.
Pictorial representations of stool form, based on Bristol stool form scale and bowel diaries, have been indicated as a reliable technique for describing bowel habits, which are more promising predictor of colonic transit compared with the self-reported stool frequency.[33,45] Meanwhile, secondary causes of constipation should be taken into consideration. Clinical exact history seems sufficient to identify the disease or medications that may be involved in constipation. Basic chemistry such as complete blood count (CBC), a basic chemo panel containing electrolytes, glucose, calcium, and urine and thyroid function tests can be conducted initially in this topic.
Medication-associated constipation or structural abnormalities, such as tumors or strictures, are rare in clinical examination and tests are not performed unless there is strong evidence.
After the initial history and physical examination, a series of tests should be performed to exclude disorders that can be either treated (such as hypothyroidism) or significant to early detection (e.g., colon cancer). Specific tests are required for endocrine, metabolic, neurological, or collagen vascular disorders according to physical examination findings. Metabolic tests (e.g., biochemical profile, thyroid-stimulating hormone, glucose, and calcium) are not recommended for chronic constipation without strong evidence.
Rectal examination should be performed in patients with chronic constipation to seek secondary causes of constipation including the presence of anal pain cause (e.g., fissures or thrombosed haemorrhoids), palpation with the index finger, resting sphincter tone, digital evaluation of anal tone during rest and squeezing, as well as looking for rectocele in anterior wall.[18,46]
Appropriate treatments are needed if this clinical assessment provides a secondary cause for constipation. Patient medications can be adjusted to prevent those with constipating effects. Fiber and/or over-the-counter (OTC) laxatives (polyethylene glycol, sodium picosulfate, or bisacodyl) may be initiated.[18,47]
A digital rectal precision assessment, which involves evaluating pelvic floor movement during simulant evacuation, is a priority for a cursory examination without these maneuvers before being referred to anorectal manometry.[47]
In addition to the clinical evaluation and rectal digital examination, the following methods should be considered to diagnose chronic constipation, when patients are suspected of pelvic floor dysfunction or in the absence of response to treatment.
2.2. Endoscopy
Structural procedures including flexible sigmoidoscopy (FS) or a colonoscopy can be very effective in obtaining evidence for the cause of unexplained symptoms, the use of chronic laxative and mucosal lesions (e.g., rectal ulcers, inflammatory bowel disease, colon, and rectal cancer).[43]
Diagnostic colonoscopy is only necessary in individuals with alarm symptoms (i.e., blood in stools, anemia, rectal bleeding, inflammatory bowel disease, rectal prolapse, obstructive symptoms, weight loss, etc.) or in patients who have to undergo colorectal cancer screening. It is worth noting that constipation-related medication and structural disorders such as tumors or strictures are unusual in a clinical examination, where tests are not recommended unless sufficient evidence is proved.[42] Physical examinations and screening evaluation may eliminate diseases that are secondary to constipation.[47]
2.3. Anorectal manometry
Anorectal manometry (or ARM) is a diagnostic procedure for measuring pressure activity of anurectom, which accordingly can show rectal reflexes, rectal sensation, rectal compliance, and the rectosphincteric reflex at rest and during defecatory maneuvering.[48,49] This procedure benefits from a pressure-sensitive catheter and a balloon at the tip of the tube to evaluate the neuromuscular and sensory of the anus and rectum. It is also useful for evaluating the presence of the recto-anal inhibitory reflex (RAIR) in patients suffering from megarectum/megacolon. Therefore, manometry can also provide information for the diagnosis of defecatory disorders (dyssynergia), visceral neuropathy and Hirschsprung disease.[50,51] Manometry has the ability to evaluate anorectal sensory dysfunction by providing higher thresholds for the first sensation and desire to defecate threshold.[43,52] Furthermore, high-resolution manometry (HRM) has been applied to assess colonic motor dysfunction in chronic constipation by its closely spaced pressure sensors.[53,54] Four patterns of anorectal manometry are summarized in Fig. 1 for the dyssynergic defecation.[49,55]
Figure 1.
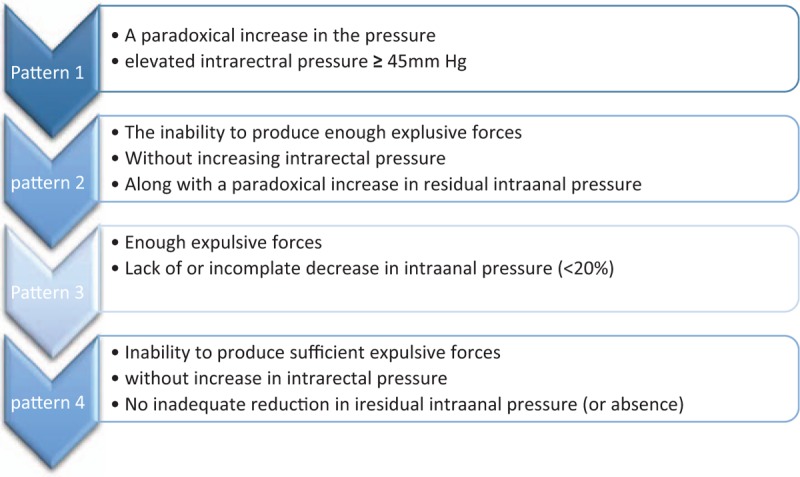
Four patterns of anorectal manometry in the dyssynergic defecation.[49,55]
2.4. Balloon expulsion testing
The balloon expulsion test (BET), along with anorectal manometry, is used for determining dyssynergic defecation. Moreover, BET has been applied as a part of pelvic floor dyssynergia detection or for excluding patients suffering from constipation without pelvic floor dyssynergia. The balloon is performed to measure the amount of time needed to expel a rectal balloon filled with 25 mL or 50 water, or air [56,57] and/ or a silicone-filled stool-like device.[58] Several studies reported impaired expulsion in 23% to 67%; this evidence indicated that BET results required more explanation along with other physiological methods.[49,56]
2.5. Barium enema
A barium enemais is a colon X-ray procedure to define changes or anatomic abnormalities of colon filled with a contrast including metallic substance (barium), but test cannot be adequately used in clinical evaluation and diagnosis of organic disease.[49,59]
2.6. Defecography and magnetic resonance defecography (MRD)
Defecography is established as a type of radiological imaging that visualizes the anorectum and pelvic floor.[49] For this test, barium is placed inside rectum and images can be taken as the barium leaves patient body for anorectal region function.
In addition, defecography has shown abnormalities in 77% of cases. Hence, there has been no strong evidence of correlation between abnormalities and symptoms, while limitation with these tests is desirable.[60] Furthermore, there is not enough information regarding its values in healthy individuals.[61] Therefore, defecography can be used as an additional tool for clinical and manometric assessment.[49]
Furthermore, MRD is a noninvasive medical technique to illustrate the physiological processes and body structures (e.g., pelvic floor anatomy and dynamic motion) for anorectal disorders.[62] MRD has been really useful to define structural abnormalities like obstructed defecation syndrome and may be favorable from surgical procedures such as stapled transanal resection of rectum.[63] It has been characterized by high soft-tissue contrast, good resolution, and lack of radiation exposure.[64] However, its routine use can be limited due to high costs and lack of standardization.[49]
2.7. Colonic transit study
In this procedure, patients may swallow a capsule that contains either a radiopaque marker or a wireless recording device. The progress of the capsule through colon will be recorded over several days and be visible on X-rays.
Measurement of colon transit is widely performed by applying radioopaque marker, wireless motility capsule (WMC), or radionuclide scintigraphy. The radioopaque marker test is the mostly applied procedure because of its cost-effectiveness and simplicity, but its limitation is radiation exposure. Scintigraphy can provide the possibility of physiological evaluation of gastrointestinal transit using gamma camera and minimal radiation.[65]
The WMC is a nonradioactive test for the assessment of regional and whole gut transit time. Furthermore, WMC is enable to measure pH and temperature of the gastrointestinal in a single, unrivaled and minimal invasive mode and eliminates many of the methodological barriers that can hinder other approaches. Moreover, WMC has been reported as an alternative method to radionuclide scintigraphy and radiopaque marker. The test failure is demonstrated in a few cases for some reason, including patient's problem in swallowing capsules, the lack of the capsule ability for recording or transferring information, lack of receiver for recording or downloading data, and software malfunctioning.[66] Its high specificity and utility have been reported for diagnosis of slow transit in constipated patients, lower gastrointestinal disorder, and lower gastrointestinal disorder.[67,68]
3. Overall approach for managing chronic constipation
3.1. Dietary fiber and laxatives
Fiber intake has been demonstrated to improve functional constipation. It has been indicated that diets with soluble fiber (psyllium 15 g daily or ispaghula) may benefit patients suffered from chronic constipation and IBS.[3] There have been studies that indicated less effectiveness of supplementation in patients suffered from slow defecatory disorders or slow- transit constipation (STC), whereas patients tend not to respond to fiber intake.[17] On the other hand, several studies reported that fiber supplements could improve bowel symptoms in patients with chronic constipation.[3] Supplements and/or an inexpensive osmotic agent have been introduced for constipation (e.g., milk of magnesia 1 or twice daily, or polyethylene Glycol (PEG) 17 g daily).
Regarding current evidence, osmotic, and stimulant laxatives should be used as first treatment strategies in patients with chronic constipation.[18] Furthermore, there is good evidence of efficacy for using PEG with substantial osmotic activity such as a controlled trial with duration of 6 months.[69]
3.2. Newer treatment options
A new agent is required when the laxatives are not effective in reducing symptoms; therefore, lubiprostone and linaclotide can be considered 2 favorable drugs. Lubiprostone is a bicyclic fatty, which was recommended at dosage of 24 μg p.o. twice daily as a gelatin capsule. Lubiprostone can be a suitable and tolerable medication for patients who need long-term therapy of constipation.[47,70]
Linaclotide is a guanylate cyclase 2C receptor agonist, which is mostly recommended for healing secondary endpoints such as stool consistency, discomfort, bloating, and straining.[43]
Prucalopride has been described as a selective high affinity 5-HT4 receptor agonist, which works as a stimulator of gut motility. It is suitable for removing the main symptoms of chronic constipation. The safety profile was persuaded, especially the lack of arrhythmogenic potential. It has had promising effects in patients who did not respond to conventional laxatives. Long-term investigation and postsales information will be important in demining the therapeutic benefits and risks of this combination.[71]
Colchicine is an alkaloid substance, which is used as an anti-inflammatory agent. It can increase the frequency of bowel movements, where it may be prescribed as a remedy for the treatment of chronic constipation. Alvimopan and methylnaltrexone have been recently suggested as new agents for the treatment of constipation caused by opioid.
Alvimopan has been recommended for postoperative ileus after surgeries by Food and Drug Administration (FDA), while FDA indicated that methylnaltrexone could be applied for patients suffering from pioid-induced constipation. However, trials of alvimopan in the confirmed use of methylnaltrexone in inopioid-induced constipation represent seriously dangerous cardiovascular causes with opposite results in terms of efficacy.[72] In addition, the efficacy of commercially available synbiotic elements has been previously evaluated for the treatment of functional constipation in males.[73]
3.3. Biofeedback therapy
Previous studies reported that biofeedback therapy could be effectively efficient by using neuromuscular training, visual, and verbal feedback. It has priority over other therapies such as laxative and sham training.[74]
Biofeedback session implicates placing a probe into the anus to give feedback of muscle tension using a computer screen. Biofeedback therapy is an efficient and multidisciplinary approach without adverse effects of therapy.[74] It has been observed that more than 70% of patients with gastrointestinal disorders get rid of symptoms by treating biofeedback therapy.[47]
It has been revealed that biofeedback therapy could be useful for improving bowel symptoms and dyssynergic defecation with regard to therapist motivation, training (for relaxing pelvic floor muscles), severity of retraining program, neuromuscular coordination, visual, sounds, and verbal feedback methods.[47,74,75] It has been reported that the physiotherapy protocol could be effective for eliminating some symptoms using pelvic floor muscle training in female patients suffered from functional constipation.[76]
3.4. Surgical Treatment
Surgical interventions may be used as an option if medical treatment was failed in constipated patients and mechanical emptying of the colon may be recommended in patients with slow bowel movements using an enema program.[77] Colectomy with ileorectal anastomosis has been introduced to be the treatment option in patients suffering from refractory slow transit constipation (i.e., colonic inertia), where dyssynergic defecation was accepted.[78] In addition to slow transit constipation (STC), a pelvic floor retraining with biofeedback should be taken into consideration before surgery in patients suffering from evacuation disorder. Moreover, patients who suffer from considerable rectocles and intussusception need to be recommended repair and pelvic floor retraining.[77]
4. Conclusion
The prevalence is 16% in the general population (range between 0.7% and 79%). Therefore, diagnostic and therapeutic options are important for treatment of chronic constipation. Better understanding of the pathophysiology of chronic constipation and information in terms of efficacy and safety of pharmacological agent can help physicians for treating and managing symptoms of constipation. Finally, a diagnostic and management algorithm is proposed for chronic constipation in the present study (Fig. 2). The effectiveness of various treatment strategies has been revealed; however, considerable dissatisfaction among patients cannot be ignored. Therefore, it should be kept in mind that such patients need to be precisely described in terms of their components.[18] Accurate history, along with a complete physical and digital rectal evaluation and comprehensive assessment, can be used to diagnose acute or chronic constipation, as well as primary or secondary condition. However, if there is no alarming symptom and treatment is unsuccessful, favorable physiological testing, together with a Sitzmark investigation, balloon expulsion testing, defecography, and ARM can play a key role in identifying the pathophysiological subtype and primary constipation.[79,80] Diagnostic evaluation should be done with an appropriate method to define the nature of colon transit or rectal evacuation or approving the lack of a primary illness resulting in constipation symptoms.[79] Lubiprostone and linaclotide can be considered 2 favorable drugs, if the laxatives are not effective in reducing symptoms. It is noteworthy that biofeedback therapy is a useful method for improving bowel symptoms and dyssynergic defecation. Surgical interventions may be applied if medical treatment was failed in constipated patients. Furthermore, a pelvic floor retraining with biofeedback is recommended before surgery in patients suffering from evacuation disorder.
Figure 2.
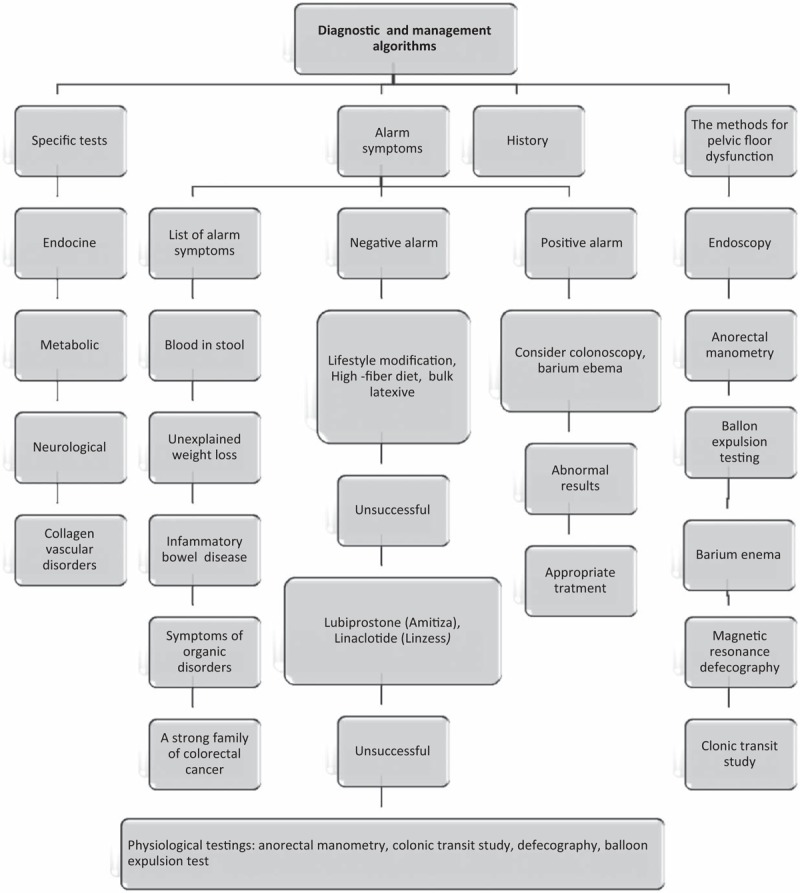
Suggested diagnostic and management algorithm for chronic constipation.
Author contributions
Conceptualization: Mohammad darvishi, Nazila bagheri.
Data curation: Mohammad darvishi, Mojgan forootan.
Formal analysis: Nazila bagheri.
Investigation: Mojgan forootan, Nazila bagheri.
Methodology: Mohammad darvishi.
Project administration: Mojgan forootan.
Validation: Nazila bagheri.
Writing – original draft: Mohammad darvishi, Mojgan forootan, Nazila bagheri.
Writing – review & editing: Mohammad darvishi.
Footnotes
Abbreviations: ARM = anorectal manometry, BET = balloon expulsion test, CBC = complete blood count, FDA = Food and Drug Administration, FS = flexible sigmoidoscopy, HRM = high-resolution manometry, MRD = magnetic resonance defecography, OTC = over-the-counter, PEG = polyethylene glycol, RAIR = recto-anal inhibitory reflex, STC = slow transit constipation, WMC = wireless motility capsule.
The authors have no conflicts of interest to disclose.
References
- [1].Benninga M, Candy DC, Catto-Smith AG, et al. The Paris Consensus on Childhood Constipation Terminology (PACCT) Group. J Pediatr Gastroenterol Nutr 2005;40:273–5. [DOI] [PubMed] [Google Scholar]
- [2].Sanchez MI, Bercik P. Epidemiology and burden of chronic constipation. Can J Gastroenterol 2011;25: 11B-L 15B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Suares NC, Ford AC. Systematic review: the effects of fibre in the management of chronic idiopathic constipation. Aliment Pharmacol Ther 2011;33:895–901. [DOI] [PubMed] [Google Scholar]
- [4].Wald A, Scarpignato C, Kamm MA, et al. The burden of constipation on quality of life: results of a multinational survey. Aliment Pharmacol Ther 2007;26:227–36. [DOI] [PubMed] [Google Scholar]
- [5].Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part II: lower gastrointestinal diseases. Gastroenterology 2009;136:741–54. [DOI] [PubMed] [Google Scholar]
- [6].Galvez C, Garrigues V, Ortiz V, et al. Healthcare seeking for constipation: a population-based survey in the Mediterranean area of Spain. Aliment Pharmacol Ther 2006;24:421–8. [DOI] [PubMed] [Google Scholar]
- [7].Iraji N, Keshteli AH, Sadeghpour S, et al. Constipation in Iran: SEPAHAN systematic review. Int J Prev Med 2012;3:S34–41. [PMC free article] [PubMed] [Google Scholar]
- [8].Chu H, Zhong L, Li H, et al. Epidemiology characteristics of constipation for general population, pediatric population, and elderly population in China. Gastroenterol Res Pract 2014;2014:532734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Mugie SM, Benninga MA, Di Lorenzo C. Epidemiology of constipation in children and adults: a systematic review. Best Pract Res Clin Gastroenterol 2011;25:3–18. [DOI] [PubMed] [Google Scholar]
- [10].Vazquez Roque M, Bouras EP. Epidemiology and management of chronic constipation in elderly patients. Clin Interv Aging 2015;10:919–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Bharucha AE, Pemberton JH, Locke GR. American gastroenterological association technical review on constipation. Gastroenterology 2013;144:218–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Tack J, Müller-Lissner S, Stanghellini V, et al. Diagnosis and treatment of chronic constipation—a European perspective. Neurogastroenterol Motil 2011;23:697–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Dukas L, Willett WC, Giovannucci EL. Association between physical activity, fiber intake, and other lifestyle variables and constipation in a study of women. Am J Gastroenterol 2003;98:1790–6. [DOI] [PubMed] [Google Scholar]
- [14].Haug TT, Mykletun A, Dahl AA. Are anxiety and depression related to gastrointestinal symptoms in the general population? Scand J Gastroenterol 2002;37:294–8. [DOI] [PubMed] [Google Scholar]
- [15].Lu CL, Chang FY, Chen CY, et al. Significance of Rome II-defined functional constipation in Taiwan and comparison with constipation-predominant irritable bowel syndrome. Aliment Pharmacol Ther 2006;24:429–38. [DOI] [PubMed] [Google Scholar]
- [16].Tucker DM, Sandstead HH, Logan GM, Jr, et al. Dietary fibre and personality factors as determinants of stool output. Gastroenterology 1981;81:879–83. [PubMed] [Google Scholar]
- [17].Voderholzer WA, Schatke W, Muhldorfer BE, et al. Clinical response to dietary fibre treatment of chronic constipation. Am J Gastroenterol 1997;92:95–8. [PubMed] [Google Scholar]
- [18].Basilisco G, Coletta M. Chronic constipation: a critical review. Dig Liver Dis 2013;45:886–93. [DOI] [PubMed] [Google Scholar]
- [19].Suares NC, Ford AC. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am J Gastroenterol 2011;106:1582–91. [DOI] [PubMed] [Google Scholar]
- [20].Bijkerk CJ, Muris JWM, Knottnerus JA, et al. Systematic review: the role of different types of fibre in the treatment of irritable bowel syndrome. Aliment Pharmacol Ther 2004;19:245–51. [DOI] [PubMed] [Google Scholar]
- [21].Cook IJ, Talley NJ, Benninga MA, et al. Chronic constipation: overview and challenges. Neurogastroenterol Motil 2009;21:1–8. [DOI] [PubMed] [Google Scholar]
- [22].Lunniss PJ, Gladman MA, Benninga MA, et al. Pathophysiology of evacuation disorders. Neurogastroenterol Motil 2009;21:31–40. [DOI] [PubMed] [Google Scholar]
- [23].Scott SM, van den Berg MM, Benninga MA. Rectal sensorimotor dysfunction in constipation. Best Pract Res Clin Gastroenterol 2011;25:103–18. [DOI] [PubMed] [Google Scholar]
- [24].Chan CL, Lunniss PJ, Wang D, et al. Rectal sensorimotor dysfunction in patients with urge faecal incontinence: evidence from prolonged manometric studies. Gut 2005;54:1263–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Camilleri M. Testing the sensitivity hypothesis in practice: tools and methods, assumptions and pitfalls. Gut 2002;51:i 34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Whitehead WE, Drinkwater D, Cheskin LJ, et al. Constipation in the elderly living at home. Definition, prevalence, and relationship to lifestyle and health status. J Am Geriatr Soc 1989;37:423–9. [DOI] [PubMed] [Google Scholar]
- [27].Chun AB, Sokol MS, Kaye WH, et al. Colonic and anorectal function in constipated patients with anorexia nervosa. Am J Gastroenterol 1997;92:1879–83. [PubMed] [Google Scholar]
- [28].Hosseinzadeh ST, Poorsaadati S, Radkani B, et al. Psychological disorders in patients with chronic constipation. Gastroenterol Hepatol Bed Bench 2011;4:159–63. [PMC free article] [PubMed] [Google Scholar]
- [29].Sonnenberg A, Koch TR. Epidemiology of constipation in the United States. Dis Colon Rectum 1989;32:1–8. [DOI] [PubMed] [Google Scholar]
- [30].Rao SS, Seaton K, Miller MJ, et al. Psychological profiles and quality of life differ between patients with dyssynergia and those with slow transit constipation. J Psychosom Res 2007;63:441–9. [DOI] [PubMed] [Google Scholar]
- [31].Devroede G, Girand G, Bouchoucha M, et al. Idiopathic constipation by colonic dysfunction: relationship with personality and anxiety. Dig Dis Sci 1989;34:1428–33. [DOI] [PubMed] [Google Scholar]
- [32].Bytzer P, Howell S, Leemon M, et al. Low socioeconomic class is a risk factor for upper and lower gastrointestinal symptoms: a population based study in 15 000 Australian adults. Gut 2001;49:66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Wald A, Scarpignato C, Mueller-Lissner S, et al. A multinational survey of prevalence and patterns of laxative use among adults with self-defined constipation. Aliment Pharmacol Ther 2008;28:917–30. [DOI] [PubMed] [Google Scholar]
- [34].Sandler RS, Jordan MC, Shelton BJ. Demographic and dietary determinants of constipation in the US population. AmJ Public Health 1990;80:185–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Howell SC, Quine S, Talley NJ. Low social class is linked to upper gastrointestinal symptoms in an Australian sample of urban adults. Scand J Gastroenterol 2006;41:657–66. [DOI] [PubMed] [Google Scholar]
- [36].Ludvigsson JF. Abis Study Group. Epidemiological study of constipation and other gastrointestinal symptoms in 8000 children. Acta Paediatr 2006;95:573–80. [DOI] [PubMed] [Google Scholar]
- [37].Inan M, Aydiner CY, Tokuc B, et al. Factors associated with childhood constipation. J Paediatr Child Health 2007;43:700–6. [DOI] [PubMed] [Google Scholar]
- [38].Ip KS, Lee WT, Chan JS, et al. A community-based study of the prevalence of constipation in young children and the role of dietaryfibre. Hong Kong Med J 2005;11:431–6. [PubMed] [Google Scholar]
- [39].Pinto Sanchez MI, Bercik P. Epidemiology and burden of chronic constipation. Can J Gastroenterol 2011;25:11B–5B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Yost KJ, Haan MN, Levine RA, et al. Comparing SF-36 scores across three groups of women with different health profiles. Qual Life Res 2005;14:1251–61. [DOI] [PubMed] [Google Scholar]
- [41].Dennison C, Prasad M, Lloyd A, et al. The health-related quality of life and economic burden of constipation. Pharmacoeconomics 2005;23:461–76. [DOI] [PubMed] [Google Scholar]
- [42].Wald A. Constipation: advances in diagnosis and treatment. JAMA 2016;315:185–91. [DOI] [PubMed] [Google Scholar]
- [43].Rao SS, Go JT. Update on the management of constipation in the elderly: new treatment options. Clin Interv Aging 2010;5:163–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Ford AC, Moayyedi P, Lacy BE, et al. Task Force on the Management of Functional Bowel Disorders. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol 2014;109suppl 1:S2–6. [DOI] [PubMed] [Google Scholar]
- [45].Saad RJ, Rao SSC, Koch KL, et al. Do stool form and frequency correlate with whole-gut and colonic transit? Results from a multicenter study in constipated individuals and healthy controls. Am J Gastroenterol 2010;105:403–11. [DOI] [PubMed] [Google Scholar]
- [46].Tantiphlachiva K, Rao P, Attaluri A, et al. Digital rectal examination is a useful tool for identifying patients with dyssynergia. Clin Gastroenterol Hepatol 2010;8:955–60. [DOI] [PubMed] [Google Scholar]
- [47].American Gastroenterological Association Medical Position Statement on Constipation. Gastroenterology 2013;144:211–7. [DOI] [PubMed] [Google Scholar]
- [48].Karlbom U, Lundin E, Graf W, et al. Anorectal physiology in relation to clinical subgroups of patients with severe constipation. Colorectal Dis 2004;6:343–9. [DOI] [PubMed] [Google Scholar]
- [49].Rao SS, Meduri K. What is necessary to Diagnose Constipation? Best Pract Res Clin Gastroenterol 2011;25:127–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Tobon F, Reid NC, Talbert JL, et al. Nonsurgical test for the diagnosis of Hirschsprung's disease. Am J Gastroenterol 1968;278:188–93. [DOI] [PubMed] [Google Scholar]
- [51].Faussone-Pellegrini MS, Fociani P, Buffa R, et al. Loss of interstitial cells and a fibromuscular layer on the luminal side of the colonic circular muscle presenting as megacolon in an adult patient. Gut 1999;45:775–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Rao SS, Welcher KD, Leistikow JS. Obstructive defecation: a failure of rectoanal coordination. Am J Gastroenterol 1998;93:1042–50. [DOI] [PubMed] [Google Scholar]
- [53].Bharucha AE. Editorial: identifying colonic motor dysfunction in chronic constipation with high-resolution manometry: pan-colonic pressurizations. Am J Gastroenterol 2017;112:490–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Noelting J, Ratuapli SK, Bharucha AE, et al. Normal values for high-resolution anorectal manometry in healthy women: effects of age and significance of rectoanal gradient. Am J Gastroenterol 2012;107:1530–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Rao SSC, Mudipalli RS, Stessman M, et al. Investigation of the utility of colorectal function tests and Rome II criteria in dyssynergic defecation (Anismus). Neurogastroenterol Motil 2004;16:589–96. [DOI] [PubMed] [Google Scholar]
- [56].Rao SSC, Ozturk R, Laine L. Clinical utility of diagnostic tests for constipation in adults: a systematic review. Am J Gastroenterol 2005;100:1605–15. [DOI] [PubMed] [Google Scholar]
- [57].Minguez M, Herreros B, Sanchiz V, et al. Pelvic floor dyssynergia in constipation. Gastroenterology 2004;126:57–62. [DOI] [PubMed] [Google Scholar]
- [58].Hsu CS, Liu TT, Yi CH, et al. Utility of balloon expulsion test in patients with constipation: preliminary results in a single center. Advances in Digestive Medicine 2016;34:181–6. [Google Scholar]
- [59].Brandt LJ, Prather CM, Quigley EM, et al. Systematic review on the management of chronic constipation in North America. Am J Gastroenterol 2005;100:S5–21. [DOI] [PubMed] [Google Scholar]
- [60].Diamant NE, Kamm MA, Wald A, et al. AGA technical review on anorectal testing techniques. Gastroenterology 1999;116:735–60. [DOI] [PubMed] [Google Scholar]
- [61].Shorvon PJ, McHugh S, Diamant NE, et al. Defecography in normal volunteers: results and implications. Gut 1989;30:1737–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Fletcher JG, Busse RF, Riederer SJ, et al. Magnetic resonance imaging of anatomic and dynamic defects of the pelvic floor in defecatory disorders. Am J Gastroenterol 2003;98:399–411. [DOI] [PubMed] [Google Scholar]
- [63].Thapar RB, Patankar RV, Kamat RD, et al. MR defecography for obstructed defecation syndrome. Indian J Radiol Imaging 2015;25:25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Rao SS. Advances in diagnostic assessment of fecal incontinence and dyssynergic defecation. Clin Gastroenterol Hepatol 2010;8:910–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Kim ER, Rhee PL. How to Interpret a Functional or Motility Test - Colon Transit Study. J Neurogastroenterol Motil 2012;18:94–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Saad RJ, Hasler WL. A technical review and clinical assessment of the wireless motility capsule. Gastroenterol Hepatol 2011;7:795–804. [PMC free article] [PubMed] [Google Scholar]
- [67].Rao SSC, Kuo B, McCallum RW. Investigation of colonic and whole gut transit with wireless motility capsule and radioopaque markers in constipation. Clin Gastroenterol Hepatol 2009;7:537–44. [DOI] [PubMed] [Google Scholar]
- [68].Lee A, Michalek W, Wiener SM, et al. T1067 clinical impact of a wireless motility capsule—a retrospective review. Gastroenterology 2010;138: S-481. [Google Scholar]
- [69].Mueller-Lissner S, Kamm MA, Wald A. Multicenter, 4-week, double-blind, randomized, placebo-controlled trial of sodium picosulfate in patients with chronic constipation. Am J Gastroenterol 2010;105:897–903. [DOI] [PubMed] [Google Scholar]
- [70].Lacy BE, Levy LC. Lubiprostone: a novel treatment for chronic constipation. Clin Interv Aging 2008;3:357–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Quigley EM. Prucalopride: safety, efficacy and potential applications. Therap Adv Gastroenterol 2012;5:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Rodriguez RW. Off-label uses of alvimopan and methylnaltrexone. Am J Health Syst Pharm 2014;71:1450–5. [DOI] [PubMed] [Google Scholar]
- [73].Fateh R, Iravani S, Frootan M, et al. Synbiotic preparation in men suffering from functional constipation: a randomised controlled trial. Swiss Med Wkly 2011;141:w13239. [DOI] [PubMed] [Google Scholar]
- [74].Rao SSC. Biofeedback therapy for constipation in adults. Best practice & research. Clin Gastroenterol 2011;25:159–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Remes-Troche JM, Paulson J, Yamada T, et al. Anorectal cortical function is impaired in patients with dyssynergic defecation. Gastroenterology 2007;108:A20. [Google Scholar]
- [76].Dehghan FM, Frootan M, Javanbakhti M, et al. The effects of a physiotherapy program based on education and pelvic floor muscle training on chronic functional constipation. J Med Council Islamic Republic Iran 2013;30:400–7. [Google Scholar]
- [77].Levitt MA, Mathis KL, Pemberton JH. Surgical treatment for constipation in children and adults. Best Pract Res Clin Gastroenterol 2011;25:167–79. [DOI] [PubMed] [Google Scholar]
- [78].Hassan I, Pemberton JH, Young-Fadok TM. Ileorectal anastomosis for slow transit constipation: long-term functional and quality of life results. J Gastrointest Surg 2006;10:1330–7. [DOI] [PubMed] [Google Scholar]
- [79].Gray JR. What is chronic constipation? Definition and diagnosis. Can J Gastroenterol 2011;25suppl B:7B–10B. [PMC free article] [PubMed] [Google Scholar]
- [80].Rao SS, Rattanakovit K, Patcharatrakul T. Diagnosis and management of chronic constipation in adults. Nat Rev Gastroenterol Hepatol 2016;13:295–305. [DOI] [PubMed] [Google Scholar]


