Abstract
Introduction
Daily or weekly averages of physical activity and sedentary behavior could mask patterns of behavior throughout the week that independently impact cardiovascular health. We examined associations between day-to-day physical activity and sedentary behavior latent classes and cardiovascular disease (CVD) risk factors in US youth.
Methods
Data were from 3,984 youth ages 6-17y from the National Health and Nutrition Examination Survey (2003-2006) and from previously published accelerometry latent classes characterizing average counts/minute and percent of wear time in moderate to vigorous physical activity (MVPA) and sedentary behavior. Multiple linear regression was used to examine associations of the classes with waist circumference, systolic and diastolic blood pressure, high- and low-density lipoprotein cholesterol, triglycerides, glucose, and insulin.
Results
Participants spent 50.4% of the day in sedentary behavior and 5.3% of the day in MVPA. Average counts/minute were 516.4 over a 7-day period. Significant differences in CVD risk factors were between extreme classes with few differences observed in intermediate classes. Youth in latent class 4 (highest average counts/minute) had lower systolic blood pressure (-4.11 mmHg [-7.74, -0.55]), lower glucose (-4.25 mg/dL [-7.84, -0.66]), and lower insulin (-6.83 uU/mL [-8.66, -4.99]) compared to youth in class 1 (lowest average counts/minute). Waist circumference was lower for the least sedentary class (-2.54 cm [-4.90, -0.19]) compared to the most sedentary class. Some associations were attenuated when classes were adjusted for mean physical activity or sedentary level.
Conclusions
There is some indication that patterns, in addition to the total amount of physical activity and sedentary behavior, may be important for cardiovascular health in youth. Longitudinal studies are needed to examine associations between physical activity and sedentary behavior patterns and changes in CVD risk factors.
Keywords: accelerometry, cardiovascular disease, risk factors, NHANES, latent class, pediatrics
Introduction
Cardiovascular disease (CVD) affects nearly 86 million Americans, and that number is expected to rise to nearly 116 million by 2030 (17). Clinical presentation of CVD largely appears in middle age, but the process of atherosclerosis begins in childhood (8) and is accelerated in the presence of risk factors such as obesity, high blood pressure, high cholesterol, and diabetes (1, 20). Approximately 50% of youth in the United States (US) have at least one CVD risk factor (12). These risk factors have been shown to track from childhood to adulthood (2, 9, 13, 24), but can be reduced by adherence to a healthy lifestyle (1, 8, 20).
The American Heart Association, the World Health Organization, and the 2008 Physical Activity Guidelines for Americans have emphasized the importance of physical activity for heart health and recommend that children and adolescents engage in at least 60 minutes of physical activity each day with most coming from moderate to vigorous intensity (16, 19, 27). Studies of US children show higher average time in moderate to vigorous physical activity (MVPA) has been associated with lower waist circumference, systolic blood pressure, and higher high-density lipoprotein cholesterol (4, 21). Despite the benefits of MVPA, only 8% of adolescents and 42% of children obtain the recommended amount of physical activity with 50% of their waking hours engaged in sedentary behaviors (25).
The current physical activity guidelines (19) were developed primarily based on studies using self-reported physical activity, which is susceptible to recall and social desirability bias (10, 18, 19, 22). Accelerometers record acceleration in small units of time, and are not impacted from these two sources of bias. Data are usually summarized into daily or weekly averages, but these summary measures potentially mask patterns of behavior over time that may independently impact cardiovascular health.
Latent class analysis (LCA), a data-driven statistical method, has been used in previous studies to describe patterns, or classes, of physical activity and sedentary behavior in children and adolescents (6, 14, 15, 23), but the studies are limited by the use of self-report data or (14, 15), a combination of self-report and accelerometry data (23). Further, previous LCA studies of physical activity did not include children of younger ages (14, 15, 23). Previous work has used accelerometry (without self-report) to derive day-to-day physical activity and sedentary behavior latent classes in youth ages 6 to 17 years (6), but the relationships between the latent classes and CVD risk factors were not explored. Therefore, the purpose of this study was to examine accelerometry-derived day-to-day physical activity and sedentary behavior latent classes with CVD risk factors in US children and adolescents. We hypothesized that children and adolescents with more active or less sedentary patterns would have better health outcomes than children with the least active or most sedentary patterns.
Methods
Study Population
The National Health and Nutrition Examination Survey (NHANES) is a cross-sectional survey using a complex multistage probability sampling design to select a representative sample of the US. Data were collected initially during home interviews, followed by physical exams in a mobile examination center. NHANES data for the 2003-2004 and 2005-2006 cycles were available for 5,607 youth ages 6 to 17 years. Youth who did not have accelerometer data (N=577) were excluded, resulting in 5,030 youth eligible for analysis. The participant's parent or guardian provided informed consent, and the participant provided assent prior to data collection. Consenting and assenting documents are available for 2003-2004 (http://www.cdc.gov/nchs/nhanes/nhanes2003-2004/brochures03_04.htm) and 2005-2006 (http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/brochures05_06.htm). The project was reviewed by the University of North Carolina at Chapel Hill Institutional Review Board and classified as exempt.
Excluded participants
Of the 5,030 participants ages 6 to 17 years with accelerometer data, participants were further excluded for the following reasons: accelerometer was not calibrated upon return (n=351); failed to wear the accelerometer for ≥ 8 hours/day on ≥ 3 days (n=681); taking diabetic medication (n=8); had outlying values for fasting glucose or average intensity (n=6). The total number of participants used in this analysis in 3,984.
Physical activity and sedentary behavior latent classes
Details of the design of the latent classes have been previously published (6) and are available for application (7). Briefly, participants were instructed to wear the ActiGraph accelerometer (model 7164) on their right hip for 7 days, during waking hours when not engaged in water based activities. Accelerometer data were used to derive latent classes characterizing average counts/minute, and percent of wear time spent in MVPA and sedentary behavior. Average counts/minute describes the “average intensity” of physical activity. Cut-points of ≥2296 counts/minute and <100 counts/minute were used to define MVPA and sedentary behavior, respectively (5, 6). Percent of total wear time spent in MVPA and in sedentary behavior were calculated and used as indicators in the LCA. Each participant was assigned to one of four classes based on the highest posterior class membership probability using maximum likelihood methods.
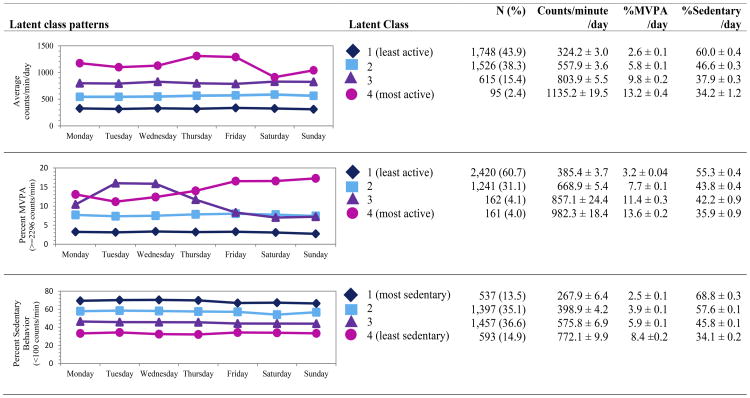
Detailed characteristics and shapes of the latent classes have been previously described (6). Figure 1 shows the distribution of participants by latent class membership. Youth in class 1 of the average counts/minute and MVPA latent classes were “least active” while youth in class 4 were “most active”. Youth in class 1 of the sedentary behavior latent classes were “most sedentary” while youth in class 4 were “least sedentary”. Latent classes 1, 2, and 3 of average counts/minute were constant across the week, differing in average intensity, while class 4 shows a non-monotonic increase in average counts/minute late in the week. MVPA latent classes 1 and 2 were constant across the week while class 3 shows a higher percentage of time spent in MVPA earlier in the week and class 4 shows a higher percentage of time spent in MVPA late in the week. Sedentary behavior latent classes were constant across the week, differing primarily in percentage of wear time spent in sedentary behavior. It should be noted that classification in one set of classes does not determine classification in a different set of classes. For example, a participant in the most active MVPA class (i.e., class 4) may not be in the most active average counts/minute class.
Figure 1.
Distribution of participants by latent class membership based on accelerometer measured average intensity (counts/minute), percent wear time in moderate-to-vigorous physical activity, and sedentary behavior, NHANES 2003-2006 (N=3,984). Adapted and used by permission from Evenson KR, Wen F, Hales D, Herring AH. National youth sedentary behavior and physical activity daily patterns using latent class analysis applied to accelerometry.
CVD risk factors
CVD risk factors were measured by trained and certified staff. We explored associations with waist circumference, systolic and diastolic blood pressure, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides, glucose, and insulin. Up to four measurements for systolic and diastolic blood pressure were completed in youth ≥8 years. The first reading was dropped and the remaining readings were averaged. Youth ≥12 years of age were asked to fast ≥8 hours prior to blood collection for LDL-C, triglycerides, glucose, and insulin. Fasting status was confirmed by self-report at the time of the examination.
Covariates
Age (continuous), gender, race/ethnicity (non-Hispanic White, non-Hispanic Black, Mexican American, Other) and socioeconomic status were included as covariates. Poverty-to-income ratio (PIR), an index for the ratio of total family income to poverty level, was used as an indicator of socioeconomic status.
Statistical analyses
The association of physical activity and sedentary behavior with each CVD risk factor was evaluated using three multiple linear regression models. Model 1 examined continuous average counts/minute, and continuous percent of time spent in MVPA and in sedentary behavior with each CVD risk factor. Model 2 examined the latent classes of counts/minute, percent of MVPA, and percent of sedentary behavior with each CVD risk factor. Model 3 combined models 1 and 2, examining the independent association of the latent classes and each CVD risk factor after controlling for the corresponding continuous measure of physical activity or sedentary behavior. For models 1 and 3, functional form of the continuous measures of physical activity and sedentary behavior were explored using linear, quadratic, cubic, and restricted cubic splines with knots at percentiles 5, 27.5, 50, 72.5, and 97.5. Wald's F tests were used to compare linear combinations and determine the best form. To account for the differential probabilities of selection, estimates were weighted to the 2000 census using 4-year sample weights provided by NHANES. All models are adjusted for age, sex, race/ethnicity, and PIR. Analyses were conducted using survey procedures of SAS statistical software, version 9.4 (SAS Institute Inc., Cary, North Carolina, USA).
Results
Characteristics of the 3,984 youth used in this analysis are presented in Table 1. Mean age was 11.5 years, 51.0% were male, 60.2% were non-Hispanic white, and mean PIR was 2.6 indicating a household income of 160% above the poverty threshold. Youth spent 50.4% of an average day in sedentary behavior and 5.3% of an average day in MVPA. Average intensity was 516.4 counts.
Table 1. Characteristics of the overall study population and remaining sample after exclusions, among youth ages 6-17 years old, NHANES 2003-2006.
| Overall1 (n =5,607) | Analytic sample2 (n =3,984) | p-value3 | |
|---|---|---|---|
| Age, years, Mean ± SE | 12.17 ± 0.06 | 11.48 ± 0.09 | 0.01 |
| Gender, n (%) | 0.08 | ||
| Male | 2,804 (51.16) | 2,001 (51.00) | |
| Female | 2,803 (48.84) | 1,983 (49.00) | |
| Race/Ethnicity, n (%) | 0.02 | ||
| Non-Hispanic White | 1,469 (61.16) | 1,007 (60.15) | |
| Non-Hispanic Black | 1,902 (14.82) | 1,332 (14.74) | |
| Mexican American | 1,776 (12.44) | 1,331 (13.33) | |
| Other | 460 (11.58) | 314 (11.79) | |
| Poverty to income ratio, Mean ± SE | 2.13 ± 0.06 | 2.64 ± 0.08 | 0.3 |
| Accelerometer activity, Mean ± SE | |||
| % MVPA/day | 5.32 ± 0.09 | 5.32 ± 0.09 | 0.6 |
| % Sedentary/day | 51.40 ± 0.28 | 50.36 ± 0.33 | 0.9 |
| Counts per minute | 505.35 ± 5.43 | 516.35 ± 5.73 | 0.6 |
| Cardiovascular disease risk factors, Mean ± SE | |||
| Waist circumference (cm) | 74.72 ± 0.28 | 72.41 ± 0.42 | 0.6 |
| Systolic blood pressure (mmHg) | 106.28 ± 0.37 | 106.00 ± 0.37 | 0.01 |
| Diastolic blood pressure (mmHg) | 56.66 ± 0.46 | 56.67 ± 0.46 | 0.9 |
| HDL cholesterol (mg/dL) | 54.42 ± 0.30 | 54.19 ± 0.38 | 0.6 |
| LDL cholesterol (mg/dL) | 88.90 ± 0.60 | 87.85 ± 1.26 | 0.8 |
| Triglycerides (mg/dL) | 83.52 ± 1.37 | 87.39 ± 2.05 | 0.3 |
| Glucose, plasma (mg/dL) | 92.23 ± 0.46 | 91.90 ± 0.37 | 0.6 |
| Insulin (uU/mL) | 13.31 ± 0.38 | 11.64 ± 0.35 | 0.01 |
Particpants ages 6 to 17 years participating in the 2003-2006 NHANES survey.
Participants were excluded for the following reasons: did not have accelerometer data (n=577); accelerometer was not calibrated upon return (n=351); failed to wear accelerometer for ≥ 8 hours/day on ≥ 3 days (n-681); taking diabetic medication (n=8); had outlying values for fasting glucose or average intensity (n=6).
P-value test differences between the overall sample and analytic sample.
Unadjusted means of each CVD risk factor by latent class are presented in Supplemental Table 1 (see Table, Supplemental Digital Content 1, Distribution of participants by latent class membership). Mean waist circumference and systolic blood pressure tend to lower across latent classes as youth tend to become more active or less sedentary. Mean HDL-C was higher as youth tend to become more active or less sedentary. LDL-C, triglycerides, glucose, and insulin means tend to lower with more active average counts/minute or percent of MVPA classes. Glucose and insulin levels tend to be higher as youth tend to be less sedentary.
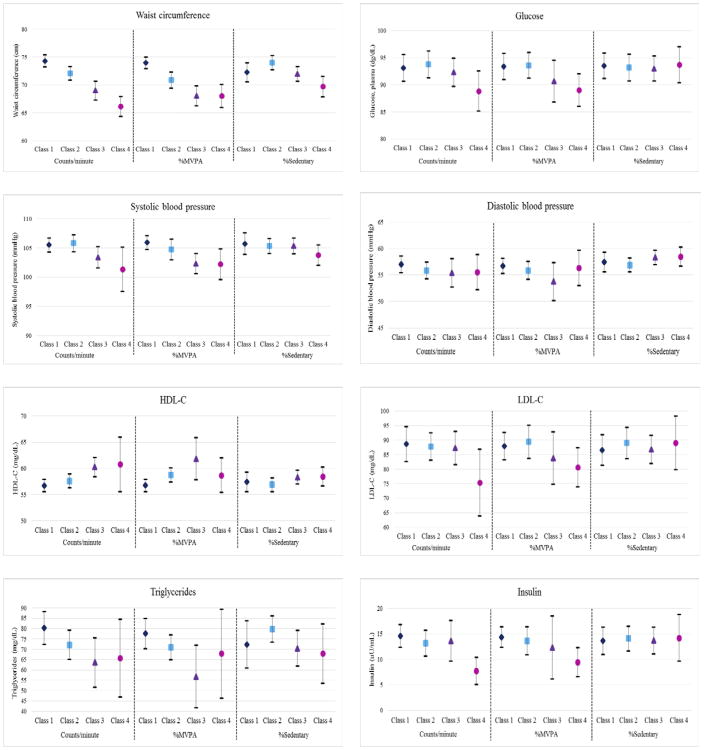
Average intensity
Adjusted associations for average counts/minute with CVD risk factors are shown in table 2. Model 1 shows adjusted associations between continuous average counts/minute and CVD risk factors. Quadratic and cubic terms for counts/minute were added to the model examining waist circumference, and a quadratic term for counts/minute was added to the model examining diastolic blood pressure. Average counts/minute was significantly associated with lower systolic blood pressure, triglycerides and insulin, and higher HDL-C. For every additional unit of average counts/minute, triglycerides was lower by 0.03 mg/dL (-0.06, -0.00) and HDL-C was higher by 0.01 mg/dL (0.00, 0.01). Model 2 shows adjusted associations between the average counts/minute latent classes and CVD risk factors. The latent classes were inversely associated with waist circumference, systolic blood pressure, glucose, and insulin, and positively associated with HDL-C. Waist circumference was significantly lower for each class (class 2 (-2.22 cm [-3.28, -1.16]); class 3 (-5.31 cm [-6.92, -3.70]);class 4 (-8.13 cm [-9.47, -6.79])) compared to class 1. This relationship is further described in Figure 2 which shows adjusted means of the latent classes by CVD risk factor. Mean waist circumference is lower in latent classes with higher average counts/minute. Systolic blood pressure was lower for class 3 (-2.11 mmHg [-3.61, -0.60]) and class 4 (-4.14 mmHg [-7.74, -0.55]) compared to class 1. HDL-C was higher for class 3 (3.54 mg/dL [1.66, 5.42]) compared to class 1. Glucose was lower for class 4 (-4.25 mg/dL [-7.84, -0.66]) and insulin was lower for class 4 (-6.83 uU/mL [-8.66, -4.99]) compared to class 1. When comparing extreme classes (class 4 vs class 1), Figure 2 shows mean waist circumference, mean systolic blood pressure, mean glucose, and mean insulin was lower in class 4, which is characterized by high average counts/minute and an increase in counts/minute late in the week, compared to class 1, which is characterized by low average counts/minute that is consistent from day-to-day. After adjustment for continuous average counts/minute in model 3 (not shown), the latent classes maintain their significant associations with systolic blood pressure (p=0.01), glucose (p=0.03), and insulin (p=0.02), though marginally attenuated.
Table 2. Associations between continuous counts/minute (model 1), counts/minute latent classes (model 2) and cardiovascular disease risk factors in youth: NHANES 2003-2006.
| Outcome | N | Model 11,2 | Model 21,3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Counts/minute | Latent Class 2 vs Class 1 | Latent Class 3 vs Class 1 | Latent Class 4 vs Class 1 | ||||||
|
|
|
|
|
||||||
| β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI | ||
| WC4 | 3775 | 0.01 | -0.02, 0.04 | -2.22 | -3.28,-1.16 | -5.31 | -6.92, -3.70 | -8.13 | -9.47, -6.79 |
| SBP | 3237 | 0.00 | -0.01, 0.00 | 0.30 | -0.66, 1.26 | -2.11 | -3.61, -0.60 | -4.14 | -7.74, -0.55 |
| DBP5 | 3237 | -0.01 | -0.02, 0.01 | -1.22 | -3.13, 0.69 | -1.65 | -4.05, 0.75 | -1.50 | -4.68, 1.68 |
| HDL-C | 3423 | 0.01 | 0.00, 0.01 | 0.89 | -0.29, 2.07 | 3.54 | 1.66, 5.42 | 4.07 | -1.05, 9.19 |
| Glucose | 1026 | 0.00 | -0.01, 0.00 | 0.67 | -1.20, 2.53 | -0.78 | -3.30, 1.73 | -4.25 | -7.84, -0.66 |
| LDL-C | 1286 | -0.01 | -0.02, 0.01 | -0.85 | -7.18, 5.48 | -1.35 | -9.36, 6.66 | -13.27 | -23.95, -2.58 |
| Triglycerides | 1288 | -0.03 | -0.06, 0.00 | -8.14 | -16.93, 0.64 | -16.71 | -31.55, -1.87 | -14.61 | -35.26, 6.05 |
| Insulin | 1007 | 0.00 | -0.01, 0.00 | -1.38 | -3.37, 0.62 | -0.87 | -4.09, 2.34 | -6.83 | -8.66, -4.99 |
Abbreviations: WC=Waist circumference; SBP=systolic blood pressure; DBP=diastolic blood pressure; HDL-C=high-density lipoprotein cholesterol; LDL-C=low-density lipoprotein cholesterol.
Adjusted for age, sex, race/ethnicity, and poverty-to-income ratio.
Model 1 are associations between the continuous measure of counts/minute and the cvd risk factors. Beta estimate and 95% CI of linear term is shown.
Model 2 are associations between counts/minute latent classes and the cvd risk factors. Class 2, 3 and 4 are compared to Class 1 (least active class).
Model 1 also includes the quadratic and cubic terms for counts/minute.
Model 1 also includes the quadratic term for counts/minute.
Note: Bolded associations have a p-value <0.05
Figure 2.
Adjusted means and 95% Confidence Intervals of CVD risk factors comparing the counts per minute, percent moderate-to-vigorous physical activity, and sedentary behavior latent classes to the least active or most sedentary class (Class 1)
Moderate to vigorous physical activity
Adjusted associations for MVPA with CVD risk factors are shown in table 3. Model 1 shows adjusted associations between continuous percent of wear time in MVPA and CVD risk factors. A quadratic term for percent of wear time in MVPA was added to models examining waist circumference, diastolic blood pressure, and glucose. Percent of wear time in MVPA was significantly associated with lower waist circumference, systolic blood pressure, triglycerides, and insulin, and higher HDL-C. For every additional unit of percent of wear time in MVPA, systolic blood pressure was lower by 0.27 mmHg (-0.41, -0.13), triglycerides were lower by 2.08 mg/dL (-3.89, -0.27), insulin was lower by 0.31 uU/mL (-0.59, -0.03), and HDL-C was higher by 0.47 mg/dL (0.25, 0.69). Model 2 shows adjusted associations between the percent of MVPA latent classes and CVD risk factors. The latent classes were inversely associated with waist circumference, systolic blood pressure, glucose, LDL-C, and insulin, and positively associated with HDL-C. Waist circumference was significantly lower for each class (class 2 (-3.09 cm [-4.28, -1.90]), class 3 (-5.92 cm [-7.64, -4.21]), and class 4 (-5.95 cm [-7.80, -4.09])) compared to class 1. Systolic blood pressure was lower for class 3 (-3.59 mmHg [-5.29, -1.89]) and class 4 (-3.68 mmHg [-6.22, -1.14]) compared to class 1. HDL-C was higher for class 2 (1.99 mg/dL [0.86, 3.12]) and class 3 (5.12 mg/dL [0.91, 9.34]) compared to class 1. Insulin was lower for class 4 (-4.95 uU/mL [-6.63, -3.28]) and glucose was lower for class 4 (-4.39 mg/dL [-6.40, -2.39]) compared to class 1. These associations were attenuated after further adjustment for percent of wear time in MVPA in model 3 (not shown).
Table 3. Associations between continuous MVPA percent wear time (model 1), MVPA latent classes (model 2) and cardiovascular disease risk factors in youth: NHANES 2003-2006.
| Outcome | N | Model 11,2 | Model 21,3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| %MVPA | Latent Class 2 vs Class 1 | Latent Class 3 vs Class 1 | Latent Class 4 vs Class 1 | ||||||
|
|
|
|
|
||||||
| β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI | ||
| WC4 | 3775 | -1.09 | -1.66, -0.52 | -3.09 | -4.28, -1.90 | -5.92 | -7.64, -4.21 | -5.95 | -7.80, -4.09 |
| SBP | 3237 | -0.27 | -0.41, -0.13 | -1.16 | -2.47, 0.15 | -3.59 | -5.29, -1.89 | -3.68 | -6.22, -1.14 |
| DBP4 | 3237 | -0.32 | -0.96, 0.32 | -0.85 | -2.66, 0.96 | -2.95 | -6.22, 0.32 | -0.36 | -3.57, 2.86 |
| HDL-C | 3423 | 0.47 | 0.25, 0.69 | 1.99 | 0.86, 3.12 | 5.12 | 0.91, 9.34 | 1.95 | -1.36, 5.25 |
| Glucose4 | 1026 | 0.16 | -0.48, 0.80 | 0.21 | -1.70, 2.13 | -2.72 | -6.12, 0.67 | -4.39 | -6.40, -2.39 |
| LDL-C | 1286 | -0.38 | -1.23, 0.46 | 1.49 | -4.77, 7.75 | -4.11 | -13.88, 5.67 | -7.30 | -14.52, -0.08 |
| Triglycerides | 1288 | -2.08 | -3.89, -0.27 | -6.62 | -13.92, 0.68 | -20.82 | -37.42, -4.21 | -9.69 | -33.65, 14.27 |
| Insulin | 1007 | -0.31 | -0.59, -0.03 | -0.72 | -2.66, 1.21 | -2.09 | -7.24, 3.06 | -4.95 | -6.63, -3.28 |
Abbreviations: MVPA=moderate-to-vigorous physical activity; %MVPA=percent of wear time in moderate-to-vigorous physical activity per day; WC=Waist circumference; SBP=systolic blood pressure; DBP=diastolic blood pressure; HDL-C=high-density lipoprotein cholesterol; LDL-C=low-density lipoprotein cholesterol.
Adjusted for age, sex, race/ethnicity, and poverty-to-income ratio.
Model 1 are associations between the continuous measure of %MVPA and the cvd risk factors. Beta estimate and 95% CI of linear term is shown.
Model 2 are associations between %MVPA latent classes and the cvd risk factors. Class 2, 3 and 4 are compared to Class 1 (least active class).
Model 1 also includes the quadratic term for %MVPA.
Note: Bolded associations have a p-value <0.05
Sedentary behavior
Table 4 shows adjusted associations for sedentary behavior with CVD risk factors. Adjusted associations between continuous percent of wear time in sedentary behavior and CVD risk factors are presented in model 1. A quadratic term for percent of sedentary behavior was added to the model examining waist circumference. Percent of wear time spent in sedentary behavior is significantly associated with waist circumference and HDL-C. HDL-C was lower by 0.07 mg/dL (-0.13, -0.01) for each additional unit of percent of wear time in sedentary behavior. Model 2 shows adjusted associations between the percent of sedentary behavior latent classes and CVD risk factors. Waist circumference was higher for class 2 (1.73 cm [0.13, 3.33]) and lower for class 4 (-2.54 cm [-4.90, -0.19]) compared to class 1. This overall significant association was maintained in model 3 (not shown) after further adjustment for percent of wear time in sedentary behavior (p=0.004).
Table 4. Associations between continuous sedentary percent wear time (model 1), sedentary latent classes (model 2) and cardiovascular disease risk factors in youth: NHANES 2003-2006.
| Outcome | N | Model 11,2 | Model 21,3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| %SED | Latent Class 2 vs Class 1 | Latent Class 3 vs Class 1 | Latent Class 4 vs Class 1 | ||||||
|
|
|
|
|
||||||
| β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI | ||
| WC4 | 3775 | 0.55 | 0.17, 0.93 | 1.73 | 0.13,3.33 | -0.25 | -2.02,1.51 | -2.54 | -4.90,-0.19 |
| SBP | 3237 | 0.05 | 0.00, 0.10 | -0.37 | -1.91,1.16 | -0.38 | -1.88,1.12 | -1.95 | -4.11,0.21 |
| DBP | 3237 | 0.23 | -0.05, 0.50 | -0.20 | -1.96, 1.56 | -1.54 | -3.17, 0.08 | -1.42 | -3.92, 1.07 |
| HDL-C | 3423 | -0.07 | -0.13, -0.01 | -0.56 | -2.52, 1.40 | 0.90 | -1.04, 2.85 | 1.03 | -1.10, 3.16 |
| Glucose | 1026 | 0.01 | -0.06, 0.09 | -0.30 | -1.65, 1.05 | -0.48 | -1.95, 1.00 | 0.21 | -3.16, 3.57 |
| LDL-C | 1286 | 0.04 | -0.21, 0.03 | 2.41 | -4.05, 8.88 | 0.21 | -6.09, 6.50 | 2.45 | -8.29, 13.19 |
| Triglycerides | 1288 | 0.38 | -0.19, 0.95 | 7.51 | -3.73, 18.75 | -1.83 | -13.29, 9.63 | -4.40 | -20.50, 11.70 |
| Insulin | 1007 | 0.04 | -0.04, 0.13 | 0.44 | -2.05, 2.93 | 0.06 | -1.93, 2.05 | 0.55 | -3.39, 4.50 |
Abbreviations: SED=sedentary behavior; %SED=percent of wear time in sedentary behavior per day; WC=Waist circumference; SBP=systolic blood pressure; DBP=diastolic blood pressure; HDL-C=high-density lipoprotein cholesterol; LDL-C=low-density lipoprotein cholesterol.
Adjusted for age, sex, race/ethnicity, and poverty-to-income ratio.
Model 1 are associations between the continuous measure of %SED and the cvd risk factors. Beta estimate and 95% CI of linear term is shown.
Model 2 are associations between %SED latent classes and the cvd risk factors. Class 2, 3 and 4 are compared to Class 1 (most sedentary class).
Model 1 also includes the quadratic term for %SED.
Note: Bolded associations have a p-value <0.05
Discussion
This study of US children and adolescents examined the association between day-to-day patterns of physical activity and sedentary behavior with several CVD risk factors. A key observation from the analysis is that classes with higher average intensity of physical activity or higher percentage of MVPA had beneficial associations with several CVD risk factors and classes with a lower percentage of sedentary behavior were associated with lower waist circumference only. For many risk factors, the associations attenuated after controlling for total average physical activity or sedentary behavior. However, some associations remained significant after controlling for these variables. These findings indicate that some behavioral patterns of physical activity may lower certain CVD risk factors beyond the amount of physical activity attained. The overall study findings highlight the importance of the amount of physical activity and sedentary behavior for cardiovascular health, and also suggest some contribution of daily pattern.
Prior studies have used bouts (i.e., extended periods of physical activity or sedentary behavior) as an alternative way to construct patterns of physical activity and sedentary behavior, and then examine these patterns with CVD risk factors (3, 11, 26). Willis et al (26) classified nearly 400 youth ages 6 to 9 years based on MVPA bouts using latent profile analysis and reported that youth who accumulate a higher percentage of both short bouts (5 minutes to <10 minutes in length) and medium-to-long bouts (≥10 minutes) had lower waist circumference compared to youth who accumulate a lower percentage of short and medium-to-long bouts. Another study examined MVPA accumulated in bouts ≥5 consecutive minutes and MVPA accumulated in <5 consecutive minutes (i.e., sporadic MVPA) with CVD risk factors using the NHANES data of more than 2,700 youth ages 6 to 19 years (11). Their results indicate that youth obtaining ≥14 minutes/day of total MVPA (i.e., MVPA bouts and sporadic MVPA) had lower odds of a high cardiometablic risk score, high waist circumference, and high systolic blood pressure compared to youth obtaining <14 minutes/day of total MVPA (11). While the accumulation of MVPA bouts each day provides insight into the patterns in which youth may obtain the daily recommendation of physical activity for cardiometabolic benefits, daily bouts summarize MVPA into a single average measure and do not tell us if variability in MVPA across the week or maintaining a consistent level of MVPA from day-to-day is beneficial for cardiometabolic health. Our analysis showed that weekly patterns that maintain a higher percentage of MVPA or higher average intensity is associated not only with lower waist circumference and systolic blood pressure but also lower glucose, insulin, and higher HDL-C, prior to controlling for time spent in MVPA. Patterns across the week rather than patterns averaged into a summary measure highlight the importance of maintaining day-to-day physical activity behaviors for cardiometabolic health.
Previous work using LCA identified 4 distinct patterns for average intensity, MVPA, and sedentary behavior based on average counts/minute/day and percent of wear time in MVPA and sedentary behavior, respectively, in a nationally representative sample of youth (6). Evenson et al demonstrated that youth cluster together based on distinct physical activity and sedentary behavior patterns thus warranting further exploration into how the patterns differentially impact health outcomes. Our results indicate that youth participating in more activity or less sedentary behavior had more favorable CVD risk factors. For example, compared to the least active MVPA class (class 1), youth in classes 2, 3, and 4 accumulated 4%, 8%, and 10% more MVPA per day, respectively, resulting in more favorable CVD risk factors among classes with a higher percentage of MVPA per day. An interesting finding is that while class 2 accumulated a consistent level of MVPA across the week, a day-to-day pattern that is similar to class 1, class 3 and class 4 vary across the week and were associated with differing combinations of CVD risk factors. Youth in class 3 accumulate a higher percentage of MVPA Monday through Thursday and a lower percentage of MVPA Friday through Sunday, but youth in class 4, the most active class, accumulate a lower percentage of MVPA Monday through Thursday and a higher percentage of MVPA Friday through Sunday. Both classes are significantly associated with lower waist circumference and systolic blood pressure when compared to class 1. However, class 3 is also significantly associated with HDL-C and triglycerides, but class 4 is associated with glucose and insulin. While this may be an artifact of how youth with similar behaviors cluster together, the results suggest that the manner in which youth accumulate weekly activity may support different biologic mechanisms, and further research could focus on specific weekly patterns that are associated with long-term cardiovascular health.
There has been increasing research using accelerometry to explore extended bouts of sedentary behavior with health outcomes. A study using NHANES data examined sedentary behavior in over 2,500 participants ages 6 to 19 and did not find extended bouts of sedentary behavior (≥30min) and percentage of wear time spent in sedentary behavior to be predictors of a high cardiometabolic risk score (3). The same study did not find significant associations between sedentary behavior and waist circumference or systolic blood pressure (3). While our results do not indicate a significant association between the sedentary classes and systolic blood pressure, we did find a significant association between the sedentary classes and waist circumference. This could be because our classes account for sedentary behavior each day, rather than an average daily pattern across the week.
Collectively, our study along with previous research, highlights the importance of accumulating higher amounts of physical activity and reducing the amount of time in sedentary behavior. Strengths of the current study include use of a large, nationally representative sample of US children and adolescents which increases generalizability, assessment of physical activity and sedentary behavior by accelerometry, a data-driven statistical approach to derive day-to-day patterns of physical activity and sedentary behavior, and examination of multiple CVD risk factors. Several limitations to this study are noteworthy. Proportions across classes vary making some comparisons more extreme than others. Specifically, the MVPA and average intensity referent class (class 1) represents 60% and 44% of the population, respectively, but class 4 represents 4% and 2.4% of the population. While the results identify a large proportion of youth who could improve their cardiometabolic health from interventions targeting weekly activity and sedentary behaviors, the results are cross-sectional which inhibits our ability to establish temporality. Additionally, the accelerometer protocol excluded use during water based activities, and it is possible some activities were not accounted for when developing the physical activity variables. Lastly, nearly 30% of children and adolescents were excluded from the analysis due to missing or invalid accelerometry data, or outlying risk factor or physical activity values. Comparison of youth included and excluded (Table 1) indicate differences in some sociodemographic variables and CVD risk factors. Participants included in the analytic tend to be younger, have a lower mean systolic blood pressure, and have a lower mean insulin compared to the overall sample. The analytic sample also has a smaller percentage of non-Hispanic Whites and a larger percentage of Mexican Americans.
LCA modeling identifies physical activity or sedentary behaviors that are associated with cardiovascular health, but may provide more information than simpler summary measures. We showed some indication that patterns, in addition to amount of physical activity and sedentary behavior may be important. Longitudinal studies could further improve our understanding of the impact of physical activity and sedentary behavior latent classes on CVD risk factors. Promotion strategies should continue to encourage increases in physical activity and reductions in sedentary behavior in children and adolescents for overall cardiovascular health.
Supplementary Material
Supplemental Digital Content 1. Distribution of participants by latent class membership. [Supp Table 1_rr.docx]
Acknowledgments
This research was supported by National Institutes of Health/National Heart, Lung, and Blood Institute diversity supplement 3U01HL103561-05S2 of the Childhood Obesity Prevention and Treatment Research (COPTR) study U01HL103561. The development of the latent classes was supported by NIH/NHLBI #R21 HL115385. The authors wish to acknowledge the assistance of Dr. Kimberly P. Truesdale.
Footnotes
Conflict Of Interest: There are no conflicts of interest to disclose. The results of the present study do not constitute endorsement by ACSM or the NIH. Results of this study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
References
- 1.American Academy of Pediatrics. Cardiovascular risk reduction in high-risk pediatric populations. Pediatrics. 2007;119(3):618–21. doi: 10.1542/peds.2006-3557. [DOI] [PubMed] [Google Scholar]
- 2.Baker JL, Olsen LW, Sørensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357(23):2329–37. doi: 10.1056/NEJMoa072515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carson V, Janssen I. Volume, patterns, and types of sedentary behavior and cardio-metabolic health in children and adolescents: a cross-sectional study. BMC Public Health. 2011;11:274. doi: 10.1186/1471-2458-11-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ekelund U, Luan J, Sherar LB, et al. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA. 2012;307(7):704–12. doi: 10.1001/jama.2012.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557–6. doi: 10.1080/02640410802334196. [DOI] [PubMed] [Google Scholar]
- 6.Evenson KR, Wen F, Hales D, Herring AH. National youth sedentary behavior and physical activity daily patterns using latent class analysis applied to accelerometry. Int J Behav Nutr Phys Act. 2016;13(1):55. doi: 10.1186/s12966-016-0382-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Evenson KR, Wen F, Howard AG, Herring AH. Applying latent class assignments for accelerometry data to external populations: Data from the National Health and Nutrition Examination Survey 2003-2006. Data Brief. 2016;9:926–30. doi: 10.1016/j.dib.2016.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Expert Panel of Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(5):S213–56. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362(6):485–93. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081–93. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 11.Holman RM, Carson V, Janssen I. Does the fractionalization of daily physical activity (sporadic vs bouts) impact cardiometabolic risk factors in children and youth? PLoS One. 2011;6(10):e25733. doi: 10.1371/journal.pone.0025733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson WD, Kroon JJ, Greenway FL, Bouchard C, Ryan D, Katzmarzyk PT. Prevalence of risk factors for metabolic syndrome in adolescents: National Health and Nutrition Examination Survey (NHANES), 2001-2006. Arch Pediatr Adolesc Med. 2009;163(4):371–7. doi: 10.1001/archpediatrics.2009.3. [DOI] [PubMed] [Google Scholar]
- 13.Katzmarzyk PT, Pérusse L, Malina RM, Bergeron J, Després JP, Bouchard C. Stability of indicators of the metabolic syndrome from childhood and adolescence to young adulthood: the Québec Family Study. J Clin Epidemiol. 2001;54(2):190–5. doi: 10.1016/s0895-4356(00)00315-2. [DOI] [PubMed] [Google Scholar]
- 14.Kim Y, Barreira TV, Kang M. Concurrent Associations of Physical Activity and Screen-Based Sedentary Behavior on Obesity Among US Adolescents: A Latent Class Analysis. J Epidemiol. 2016;26(3):137–44. doi: 10.2188/jea.JE20150068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu J, Kim J, Colabianchi N, Ortaglia A, Pate RR. Co-varying patterns of physical activity and sedentary behaviors and their long-term maintenance among adolescents. J Phys Act Health. 2010;7(4):465–74. doi: 10.1123/jpah.7.4.465. [DOI] [PubMed] [Google Scholar]
- 16.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 17.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133(4):e38–60. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 18.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1435–45. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 19.Office of Disease Prevention and Health Promotion [Internet] Physical Activity Guidelines for Americans. [cited 2016 Feb 1]; Available from: http://health.gov/paguidelines/guidelines/
- 20.Oliveira FL, Patin RV, Escrivão MA. Atherosclerosis prevention and treatment in children and adolescents. Expert Rev Cardiovasc Ther. 2010;8(4):513–28. doi: 10.1586/erc.09.170. [DOI] [PubMed] [Google Scholar]
- 21.Pahkala K, Heinonen OJ, Lagström H, et al. Clustered metabolic risk and leisure-time physical activity in adolescents: effect of dose? Br J Sports Med. 2012;46(2):131–7. doi: 10.1136/bjsm.2010.073239. [DOI] [PubMed] [Google Scholar]
- 22.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–7. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 23.Patnode CD, Lytle LA, Erickson DJ, Sirard JR, Barr-Anderson DJ, Story M. Physical activity and sedentary activity patterns among children and adolescents: a latent class analysis approach. J Phys Act Health. 2011;8(4):457–67. doi: 10.1123/jpah.8.4.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raitakari OT, Juonala M, Kähönen M, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA. 2003;290(17):2277–83. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]
- 25.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 26.Willis EA, Ptomey LT, Szabo-Reed AN, et al. Length of moderate-to-vigorous physical activity bouts and cardio-metabolic risk factors in elementary school children. Prev Med. 2015;73:76–80. doi: 10.1016/j.ypmed.2015.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization [Internet] Geneva, Switzerland: Global Recommendations on Physical Activity for Health. [cited 2016 Feb 1]; Available from: http://whqlibdoc.who.int/publications/2010/9789241599979_eng.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. Distribution of participants by latent class membership. [Supp Table 1_rr.docx]