Abstract
Transgender and gender variant (GV) youth experience elevated risk for poor health and academic outcomes due mainly to social experiences of stigma and discrimination. To supplement the growing evidence on health risks encountered by transgender/GV youth, we identified factors theorized to be protective for these youth across all four levels of Bronfenbrenner’ s socioecological model (individual, relationship, community, societal). We conducted a systematic search of peer-reviewed research. The articles included in this review were published in peer-reviewed journals in English or Spanish between 1999 and 2014, analyzed data from a sample or subsample of transgender or GV participants with a mean age between 10 and 24 years, and examined the relationship of at least one theorized protective factor to a health or behavioral outcome. Twenty-one articles met inclusion criteria. Transgender/GV youth in included articles ranged from 11 to 26 years of age, were racially/ethnically diverse, and represented varied gender identities. Within these articles, 27 unique protective factors across four levels of the ecological model were identified as related to positive health and well-being. Self-esteem at the individual level, healthy relationships with parents and peers at the relationship-level, and gay-straight alliances at the community level emerged as protective factors across multiple studies. Our findings underscore the relative lack of research on transgender/GV youth and protective factors. Novel recruitment strategies for transgender/GV youth and better measurement of transgender identities are needed to confirm these protective relationships and identify others. Growth in these areas will contribute to building a body of evidence to inform interventions.
Keywords: Youth, Transgender, Gender variance, Protective factors
Introduction
Transgender and gender variant youth experience multiple stressors that negatively affect their health and well-being. Transgender youth are adolescents and young adults with a self-identified gender different from their sex assigned at birth (Fenway Health, 2010), while gender variant (GV) youth are those whose characteristics, traits, or identities do not neatly align with societal expectations of traditional male and female roles (e.g., boys and men who behave in ways that society labels feminine; girls and women who behave in ways that society labels masculine; Carroll, Gilroy, & Ryan, 2002). GV youth may include youth who identify as transgender. Neither being transgender nor GV implies that a youth is also a sexual minority (i.e., lesbian, gay, bisexual, and other non-heterosexual individuals), as gender identity and sexual orientation are distinct. Transgender/GV youth experience stigma due to negative cultural beliefs about gender variance (Gordon & Meyer, 2007; Reisner et al., 2015a), and most GV youth report higher levels of verbal and physical victimization than their gender normative peers (Aspenlieder et al., 2009; D’Augelli, Grossman, & Starks, 2005; Toomey et al., 2010). Harassment, violence, discrimination, and childhood abuse are particularly well documented for transgender youth (Grossman & D’Augelli, 2006; Reisner et al., 2014b). These youth experience elevated risk within many domains traditionally associated with positive youth development (Factor & Rothblum, 2008; Grossman & D’Augelli, 2006; Reisner et al., 2015a). For example, family networks may be unsupportive if parents reject children who disclose a transgender identity (Factor & Rothblum, 2008; Sevelius, 2013) and schools can be inhospitable as coming out to peers, teachers, and staff can result in bullying or verbal and physical harassment (McGuire et al., 2010; Reisner et al., 2015a).
These compounding risk factors have well-documented effects on health and well-being. For transgender/GV adults, experiences of stigma are linked with mental health difficulties including depression, anxiety, reduced quality of life, and attempted suicide (Bockting et al., 2013; Hendricks & Testa, 2012; Newfield et al., 2006). Transgender youth are diagnosed with depression and anxiety at rates that surpass cisgender (i.e., non-transgender) peers, and experience up to three times the rate of suicidal ideation, non-lethal self-harm, and suicide attempts as cisgender youth (Reisner et al., 2015b). Violence, stigma, and discrimination are tied to elevated rates of HIV infection among transgender women (De Santis, 2009); rates of HIV are disproportionately high among transwomen with population averages ranging from 15 to 40% among adults and 5–22% among youth age 16–25 years (Baral et al., 2013; Clements-Nolle et al., 2001; Garofalo et al., 2006; Herbst et al., 2008; Nemoto et al., 2004; Operario et al. 2008; Simon, Reback, & Bernis, 2000; Wilson et al., 2015). Approximately 27% of young transmen and transwomen in one study reported having had gonorrhea, chlamydia, and/or syphilis in the past year (Stephens, Bernstein, & Philip, 2011).
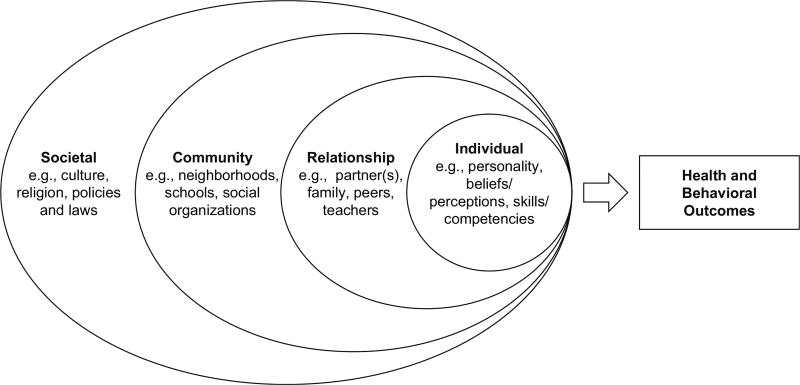
Given the compounding effects of risk encountered by transgender/GV youth, researchers should consider what helps prevent poor health and well-being. Literature on adolescent development suggests that strengthening protective factors among at-risk youth is an important intervention strategy (Fergus & Zimmerman, 2005; Resnick, 2000a, 2000b). Protective factors are characteristics, conditions, and behaviors that enable individuals to avoid or decrease negative health consequences associated with risks and hazards (Fergus & Zimmerman, 2005; Resnick, 2000a, 2000b). Bronfenbrenner’s socioecological model provides a useful framework for conceptualizing protective factors within individual, relationship, community, and societal levels (Bronfenbrenner, 1979). Public health scientists have historically used this model to map protective factors among subgroups of adolescents, such as those at risk for violence (Hall, Simon, Lee, & Mercy, 2012), those who identify as sexual minorities (Armstrong, Steiner, Jayne, & Beltran, 2016), and those in developing countries (Mmari & Blum, 2009). Consideration of protective factors within this model highlights the dynamic relationship between factors at each level and how they collaboratively influence health and well-being. This dynamism enables researchers to identify important missing links between factors and outcomes in need of future study, and allows practitioners to specify multi-level pathways through which interventions may best improve adolescent health. While some emerging scholarship about protective factors that reduce risk and improve health outcomes among subpopulations of transgender/GV youth exists (Ignatavicius, 2013; Testa, Jimenez, & Rankin, 2014), empirical study of this topic remains underdeveloped.
The purpose of this systematic review is to map the empirical literature on protective factors among transgender/GV youth within a socioecological framework. To advance scientific inquiry in this area, we: (1) summarize the existent empirical research on transgender/GV youth and protective factors; (2) organize evidence within the socioecological framework; and 3) identify theoretical and methodological gaps. This conceptual overview should help researchers design future studies of protective factors and transgender/GV youth.
Methods
To identify and categorize protective factors, we developed a conceptual guide a priori via a non-systematic scan of peer-reviewed and gray literature that we organized using the socioecological model and adolescent development theories (Bronfenbrenner, 1979; Hall et al., 2012; Mmari & Blum, 2009). Factors were integrated into the conceptual guide if we found evidence that they were theoretically or empirically described as a protective factor for any health outcome among any population of adolescents or young adults (i.e., not just transgender/GV youth). We subsequently organized these factors by (1) socioecological level and (2) types of factors within each level. This conceptualization guided the development of search terms and data extraction. Figure 1 offers a visual representation of this socioecological conceptualization of protective factors.
Fig. 1.
Socioecological Model of Protective Factors. This figure provides a visual depiction of types protective factors organized within Bronfenbrenner’s socioecological model. Factors at each level collaboratively influence individual health and behavioral outcomes. Note. Adapted from: Ivankovich, M.B., Fenton, K.A., & Douglas, J.M. (2013). Considerations for national public health leadership in advancing sexual health. Public Health Research, 128 suppl 1, 102–110.
We identified relevant articles via a systematic review of 19 English and 13 Spanish databases, using keywords from three core domains (i.e., adolescence, gender identity, protective factors) to create the search strategy (see Table 1). Inclusion required at least one search term from each of the three core domains. We also performed manual database searches and reviewed reference lists of included articles to identify additional relevant articles.
Table 1.
Search strategy
| Domain | Search terms |
|---|---|
| Adolescence | English: adolescen* or youth* or teen* or high school or middle school or pubert* or tween* or student* or young adult* or emerg* adult* |
| Spanish: adolescen* or joven* or pubert* or secundaria* or preparatoria* or estudiant* | |
| Gender identity | English: transgender or gender varian* or gender conform* or gender nonconform* or gender identit* or gender fluid* or gender flex* or gender dysphori* or gender express* or gender atypical or gender bend* or gender creative* or gender independen* or intersex* or two-spirit or genderqueer or transsexual |
| Spanish: transgenero* or transex* or travest* | |
| Protective factors | English: protect* factor* or resilien* or asset* or skill* or competen* or resourceful* or coping or cope* or psychological endurance or hardiness or adapt* or adjust* or empower* or health promot* or persistenc* or positive youth development or support* |
| Spanish: persistenc* or protecc* or protect* or apoy* or promo* | |
| Database used | English: PsychInfo, PsycArticles, Web of Science, Medline, Sociological Abstracts, ERIC, CINHAL, Embase, Global Health, CAB Abstracts, ProQuest Education, Family Health, Health and Medicine, Health Management, Nursing and Allied Health, Science, Social Science, Psychology, ASSIA |
| Spanish: LILACS, CidSaude, PAHO, Repidisca, Desastres, Adolec, BBO, BDENF, HomeoIndex, MedCarib, WHOLIS, IBECS, Fuente Academica |
English search terms were also used in Spanish databases given that many journals indexed in Spanish databases require abstracts to be written in both English and Spanish
Inclusion/Exclusion Criteria
To meet inclusion criteria, articles had to: (1) be published in a peer reviewed journal, in English or Spanish, between 1999 and 2014; (2) analyze data collected from a sample or subsample of transgender or GV adolescents with a mean age between 10 and 24 years; (3) present research conducted in North America, Europe, Australia, New Zealand, or Latin America; and (4) examine at least one theorized protective factor in relation to a health or behavioral outcome. For quantitative studies, this final criterion was met by statistical testing of at least one pathway between a theorized protective factor and a health or behavioral outcome. Health and behavioral outcomes were not limited to specific topics (e.g., sexual health or substance use) or types of measures (e.g., biomarkers or self-reported behaviors); however, they did exclude risk factors like victimization and experiences of harassment. Quantitative relationships with a p value of < .05 were considered significant. Qualitative studies had to report at least one author-identified theme that connected a protective factor to a health-promoting pathway. Studies that explored these relationships in a sample that did not disaggregate transgender youth from their cisgender peers were excluded from the synthesis as we could not interpret the unique effects of theorized protective factors for transgender/GV youth. Articles meeting inclusion criteria were included, regardless of study quality, with the exception of retrospective studies of adults older than 24 years reporting their experiences as youth.
Abstract Screening and Data Extraction
Three coders screened the abstracts of all potentially relevant articles identified in the literature search. To determine intercoder reliability, an initial subset of abstracts was screened by all coders. Intercoder agreement on this subset was 95%. At that point, remaining abstracts were divided among the coding team to be screened. Any articles assessed as unclear with respect to inclusion or exclusion criteria by individual reviewers were brought back to all coders to discuss until consensus was reached.
After identifying abstracts of interest, two researchers independently reviewed and summarized the full text articles meeting inclusion criteria using a standardized extraction form. Extracted data included: (1) study background information (e.g., study design and location, sampling strategy); (2) sample characteristics (e.g., sex, gender, race/ethnicity); (3) protective factors organized by ecological domain; (4) outcomes; and (5) a summary of the relationship(s) between protective factor(s) and outcome(s). Discrepancies concerning protective factors or outcomes were discussed among co-authors until consensus was reached.
Data Analysis
To map this literature, we catalogued articles by sampling strategy, race/ethnicity and sex or gender composition within the sample, and terminology used to categorize transgender/GV youth. We organized protective factors extracted from articles within the socioecological framework, totaled the number of factors observed or tested as protective at each level, and distinguished between factors as qualitative or quantitative. We noted any factor examined in more than one article or in relationship to more than one outcome and flagged any theorized protective factors with non-significant or risk relationships to health and behavioral outcomes. We then clustered factors by thematic type within each level of the socioecological framework to highlight any existing empirical trends.
Results
Study Characteristics
The systematic search retrieved 2337 records (2165 English, 172 Spanish). After removing duplicates, we screened 1956 unique records. Of those, 50 abstracts met criteria for full-text review and an additional 15 articles were found through review of reference lists and manual searches (Fig. 2). After full text coding, 21 articles met our inclusion criteria including nine that were quantitative, nine that were qualitative, and three that were mixed-methods. All included articles were cross-sectional and written in English, and the great majority (n = 19) described research conducted in the United States. Because articles that reported data from the same study but examined different factors (Grossman & D’Augelli, 2007; Grossman, D’Augelli, & Frank, 2011) or provided separate quantitative (Wilson et al., 2009) and qualitative (Wilson, Iverson, Garofalo, & Belzer, 2012) analyses were included, results are presented in summative tables by unique article, rather than data source.
Fig. 2.
Flowchart of Inclusion and Exclusion of Articles. Note. Adapted from: Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P., & Moher, D. (2009)
Participants ranged from 11 to 26 years of age and were racially and ethnically diverse: five articles included exclusively youth of color, seven articles included > 50% youth of color, seven articles included < 50% youth of color, and two articles did not report information on race or ethnicity. While all articles used convenience samples, participants were recruited through multiple recruitment strategies including community or venue-based recruitment (e.g., placing flyers and business cards at cafes, bars, community-based organizations, and clinics), online recruitment (e.g., through lesbian, gay, bisexual, and transgender [LGBT] oriented social media/listservs), and school-based recruitment (e.g., within classes or gay-straight alliances [GSAs]). Fifteen articles recruited participants in urban areas. Seventeen articles had samples that exclusively comprised transgender/GV youth, while four articles included both transgender/GV and cisgender youth, but examined protective pathways in a transgender/GV youth subgroup. See Table 2 for article characteristics.
Table 2.
Study characteristics of included articles
| Source/ citation |
Study dates |
Location | Data collection method |
Sampling strategy |
N | Age (range) |
Sex/gender composition (male/ female/trans) |
Transgender/gender variant terminology |
Race/ethnicity |
|---|---|---|---|---|---|---|---|---|---|
| Quantitative studies | |||||||||
| Dowshen et al. (2011) | 2007–2008 | Chicago, IL, USA | CASI (computer assisted self interviews) | Convenience sample: community & online recruitment | 92 | Mean: 20.4 (16–25) | Trans/other: 100%, n = 92 | Transwoman | White, non-Hispanic: 21%, n = 19 |
| Feminine-identified/male-born person | Black, non-Hispanic: 58%, n = 53 | ||||||||
| Other: 22%, n = 20 | |||||||||
| Garofalo et al. (2006) | 2003 | Chicago, IL, USA | Online or paper surveys | Convenience sample: community recruitment | 51 | Mean: 21.6 (16–25) | Trans/other: 100%, n = 51 | Transgender | Black, non-Hispanic: 57%, n = 29 |
| MtF | Hispanic/Latino: 16%, n = 8 | ||||||||
| Female | Mixed: 22%, n = 11 | ||||||||
| Other: 5%, n = 3 | |||||||||
| Greytak et al. (2013) | Not reported | USA | Online or paper surveys | Convenience sample: community & online recruitment | 6853 | Mean: 16.3 (13–21) | Male: 34.6, n = 2369 | Transgender | White, non-Hispanic: 66.8%, n = 4576 |
| FtM | |||||||||
| Female: 59.5%, n = 4075 | MtF | Black, non-Hispanic: 3.8%, n = 259 | |||||||
| Trans/Other: 6.0%, n = 409 | Transgender and female | Hispanic/Latino: 13.7%, n = 940 | |||||||
| Transgender and male | Asian/Pacific Islander: 2.9%, n = 200 | ||||||||
| Multigender | Mixed: 10.0%, n = 687 | ||||||||
| Other: 1.9%, n = 1301 | |||||||||
| Grossman & D’Augelli (2007) | 2001–2003 | New York City, NY, USA | In-person interviews | Convenience sample: community & snowball recruitment | 55 | Mean: 18.4 (15–21) | Trans/other: 100%, n = 55 | FtM | White: 74.5%, n = 41 |
| MtF | Black: 12.7%, n = 7 | ||||||||
| Asian/Pacific Islander: 1.8%, n = 1 | |||||||||
| Mixed: 5.4%, n = 3 | |||||||||
| Other: 5.4%, n = 3 | |||||||||
Separated out by ethnicity:
|
|||||||||
| Grossman et al. (2011) | 2001–2003 | New York City, NY, USA | In-person interviews | Convenience sample: community & snowball recruitment | 55 | Mean: 18.4 (15–21) | Trans/other: 100%, n = 55 | FtM | White: 74.5%, n = 41 |
| MtF | Black: 12.7%, n = 7 | ||||||||
| Asian/Pacific Islander: 1.8%, n = 1 | |||||||||
| Mixed: 5.4%, n = 3 | |||||||||
| Other: 5.4%, n = 3 | |||||||||
Separated out by ethnicity:
|
|||||||||
| Simons et al. (2013) | 2011–2012 | Los Angeles, CA, USA | CASI (computer assisted self interviews) | Convenience sample: patient population | 66 | Mean: 19.1 (12–24) | Trans/other; 100%, n = 66 | Transgender | White, non-Hispanic: 51.5%, n = 34 |
| Gender nonconforming | |||||||||
| Assigned male (asserted female) | Black, non-Hispanic: 10.6%, n = 7 | ||||||||
| Assigned female (asserted male) | Hispanic/Latino: 28.8%, n = 19 | ||||||||
| Other: 9.1%, n = 6 | |||||||||
| Stotzer (2011) | Not reported | Oahu, HI, USA | Paper surveys | Convenience sample: community recruitment | 168 | Mean: 20 (16–26) | Trans/other; 100%, n = 168 | Transgender | White, non-Hispanic:16.7%, n = 28 |
| Male | |||||||||
| Female | Black, non-Hispanic: 3.0%, n = 5 | ||||||||
| Mahu (a Hawaiian word for gender nonconforming people) | Asian/Pacific Islander: ≈ 69.0%, n ≈ 115.9 | ||||||||
| Hispanic/Latino: 20.2%, n = 34 | |||||||||
| Mixed: 56.9% n = 96 | |||||||||
| Other:11.3%, n = 191 | |||||||||
| (Results add up to > 100% because response categories were “check all that apply”; API is approximate because participants could report multiple API ethnicities and we have collapsed these into one category) | |||||||||
| Wilson et al. (2009) | Not reported | Los Angeles, CA, USA & Chicago, IL, USA | In-person interviews | Convenience sample: community recruitment via key informants | 151 | Median: 21 (15–24) | Trans/other: 100%, n = 151 | Transgender female | White, non-Hispanic: 5%, n = 1 |
| Black, non-Hispanic: 39%, n = 59 | |||||||||
Spread:
|
Hispanic/Latino: 38%, n = 58 | ||||||||
| Asian/Pacific Islander: 5%, n = 1 | |||||||||
| Mixed: 10%, n = 15 | |||||||||
| Other: n = 5, 3.3% | |||||||||
| Zucker et al. (2002) | 1975–2000 | Toronto, Ontario, Canada | Clinical interviews/ assessment | Convenience sample: patient population | Children: n = 358 |
Children:
|
Children:
|
Gender dysphoric |
Children:
|
| Adolescents: n = 72 |
Adolescents:
|
Adolescents:
|
Adolescents:
|
||||||
| Qualitative Studies | |||||||||
| Corliss et al. (2007) | 1999 | Los Angeles, California, USA | Semi-structured interviews | Convenience sample: patient population | 18 | Mean: 20 (16–24) | Trans/other: 100%, n = 18 | Male to female transgender | White, non-Hispanic: 11%, n = 2 |
| Black, non-Hispanic: 39%, n = 7 | |||||||||
| Hispanic/Latino: 44%, n = 8 | |||||||||
| Native American: 6%, n = 1 | |||||||||
| Goodrich (2012) | Not reported | Northeastern Region, USA | In-person interviews | Convenience sample: community & online recruitment | 4 | Mean: Not Reported (18–22) | Trans/other: 100%, n = 4 | Transsexual | White, non-Hispanic: 100%, n = 4 |
| Female-to-male (FtM) | |||||||||
| Male-to-female (MtF) | |||||||||
| Gutierrez (2004) | 2000 | Northeast Region, USA | In-person interviews, individual & group | Convenience sample: school-based recruitment | 4 | Mean: not reported (all under 21) | Trans/other: 100%, n = 4 | Female transgender | Students of color: 100%, n = 4 |
| Male-to-female transgender | |||||||||
| Pusch (2005) | Not reported | USA& Canada | Electronic group interview (listserv) | Convenience sample: online recruitment | 8 | Mean: Not Reported (19–25) | Trans/other: 100%, n = 8 | Transgender | Not reported |
| Transsexual | |||||||||
| Female-to-male | |||||||||
| Male-to-female | |||||||||
| Reck (2009) | 2003–2005 | San Francisco, CA, USA | In-person interviews | Convenience Sample: Community Recruitment | 5 | Mean: not reported (17–22) | Male: 40%, n = 2 | Female-to-male transsexual | Black, non-Hispanic: 40%, n = 2 |
| Trans/other: 60%, n = 3 | Genderqueer | Hispanic/Latino: 40%, n = 2 | |||||||
| Queer | Mixed: 20%, n = 1 | ||||||||
| Questioning | |||||||||
| Sausa (2005) | Not reported | Philadelphia, PA, USA | Semi-structured interviews & key informants | Convenience sample: community recruitment | 24 | Mean: 19.8 (16–21) | Trans/other: 100%, n = 24 | Trans | White, non-Hispanic: 42%, n = 10 |
| Femme queen | |||||||||
| Butch | |||||||||
| Butch queen | “People of color”: 58%, n = 14 | ||||||||
| Drag queen | |||||||||
| Drag king | |||||||||
| Freak | |||||||||
| Girl | |||||||||
| Boy | |||||||||
| Gender bender | |||||||||
| Androgynous | |||||||||
| Trannyboy | |||||||||
| MTF | |||||||||
| FTM | |||||||||
| Genderqueer | |||||||||
| Male with female qualities | |||||||||
| Singh (2013) | Not reported | Southeastern City, USA | Semi-structured interviews | Convenience sample: community & online recruitment | 13 | Mean: 19 (15–24) | Trans/other: 100%, n = 13 | Trans man | Black, non-Hispanic: 46.6%, n = 6 |
| Transgender woman | |||||||||
| Transsexual woman | Hispanic/Latino: 23.1%, n = 3 | ||||||||
| Boi/Genderqueer | Asian/Pacific Islander: 15.4%, n = 2 | ||||||||
| Genderqueer | Mixed: 15.4%, n = 2 | ||||||||
| Gender-fluid | |||||||||
| Singh et al. (2013) | Not reported | Southeast, Midwest, Northeast, and Northwest Regions, USA | Semi-structured interviews | Convenience sample: community & online recruitment | 17 | Mean: 22 (15–25) | Trans/other: 100%, n = 17 | FtM | White, non-Hispanic: n = 13, 76.5% |
| Trans guy | |||||||||
| Trans man | Asian/Pacific Islander: n = 1, 5.8% | ||||||||
| Male | |||||||||
| Genderqueer | Mixed: n = 3, 17.6% | ||||||||
| Wilson et al. (2012) | Not reported | Los Angeles, CA, USA & Chicago, IL, USA | In-depth interviews | Convenience sample: community recruitment | 21 | Mean: Not Reported (16–24) | Trans/other: 100%, n = 21 | Transgender female | White, non-Hispanic: 14%, n = 3 |
| Black, non-Hispanic: 33%, n = 7 | |||||||||
Spread:
|
Hispanic/Latino: 19%, n = 4 | ||||||||
| Asian/Pacific Islander: 14%, n = 3 | |||||||||
| Mixed: 14%, n = 3 | |||||||||
| Other: 5%, n = 1 | |||||||||
| Mixed methods studies | |||||||||
| Bopp et al. (2004)2 | 2001 | Oahu, HI, USA | Paper survey & semi-structured interviews | Convenience sample: intervention group & community control | 18 |
Intervention group:
|
Trans/other: 100%, n = 18 | Transgendered | Asian/Pacific Islander: 100% |
| TG | |||||||||
Control Group:
|
Mahu | ||||||||
| Jones & Hillier (2013)2 | 2010 | Australia | Online/paper surveys | Convenience Sample: Community & Online Recruitment | 3134 | Mean: 17 (14–21) | Male: 40.4% n = 1265 | Trans-spectrum | Not reported |
| Gender queer | |||||||||
| Female: 56.3%, n = 1766 | Transgender f-m | ||||||||
| Transgender m-f | |||||||||
| Trans/Other: 2.9%, n = 91 | Other (i.e., androgynous, gender fluid, no gender, hermaphrodite) | ||||||||
| McGuire et al. (2010) | 2003–2005 | CA, USA | Focus groups & online/paper surveys |
Study 1:
|
Study 1: 2260 | Study 1: Not reported (6–12 graders) |
Study 1:
|
Study 1: Transgender |
Study 1:
|
Study 2:
|
Study 2: 36 | Study 2: Not reported (12–23) |
Study 2:
|
Study 2:
|
Study 2:
|
||||
Racial/Ethnic categories were disaggregated further within the original article but are consolidated here for readability
Quantitative results were only descriptive or not statistically tested for differences, so not included in quantitative summary
A wide range of terminology was used to categorize gender identities of participants. Eleven articles categorized transgender participants within a gender binary (i.e., the conceptualization of maleness and femaleness as distinct categories), labeling participants as male-to-female (i.e., MtF, transgender women, transwomen, female) or female-to-male (i.e., FtM, transgender men, transmen, male). Nine articles further disaggregated the transgender umbrella using a variety of researcher-assigned and participant-identified gender identity labels, such as genderqueer, genderfluid, or Mahu (a native Hawaiian term). One article utilized diagnostic criteria (i.e., gender dysphoric) to identify participants experiencing clinically significant distress or impairment due to the difference between their lived gender (i.e., gender identity) and assigned sex (i.e., sex at birth; APA 2013).
Protective Factors
We found 27 unique protective factors with nine factors at each of the individual, relationship, and community levels of the socioecological model; no articles examined factors at the societal level. Table 3 provides a complete list of factors, organized by socioecological level, and details specific qualitative and quantitative findings. Quantitative findings are further disaggregated into protective, nonsignificant, and risk associations.
Table 3.
Protective factors among transgender/gender variant youth
| Ecological level | Type | Theorized protective factor | Quantitative outcomes with protective relationships |
Quantitative Outcomes with Non-significant or Risk relationships |
Qualitative findings |
|---|---|---|---|---|---|
| Individual | Beliefs/perceptions | Self-esteem | High-Risk Sex (i.e., unprotected anal intercourse) (Garofalo et al., 2006) |
Non-significant:
|
Transgender youth reported that more self-esteem helped them to avoid suicide (Bopp et al., 2004) |
Body esteem
|
(a, b) Suicide attempts (Grossman & D’Augelli, 2007) |
Non-significant:
|
– | ||
Religiosity
|
(a) Sexual Risk Index* (i.e., sex work, multiple anal sex partners, URAI) (Dowshen etal., 2011) |
Non-significant:
|
– | ||
| Positive sense of self | – | – | Transgender youth of color reported recognizing and defining their racial/ethnic and gender identities on their own terms as a source of empowerment and pride (Singh, 2013) | ||
| Self-efficacy | – | – | Transgender youth reported that sexual self-efficacy facilitated healthier relationships and safer sex (Bopp et al., 2004) | ||
| Skills/competencies | Personal mastery | Trauma symptoms (Grossman et al, 2011) |
Non-significant:
|
- | |
| Depression (Grossman et al, 2011) | |||||
| Internet/social media use | – | – | Transsexual college students considered the internet a good tool for finding resources, educational materials, and connecting with “other transsexuals” (Goodrich, 2012) | ||
| Transgender youth of color reported using social media to connect to role models who shared their gender and racial identities as well as to find information about transgender social and medical experiences (Singh, 2013) | |||||
| Problem solving skills | – | – | Transgender youth demonstrated problem solving skills by taking steps to better their situation; some engaged in dialogue to change opinions of family members who were anti-trans, others sought out inclusive spaces in which to live (Jones & Hillier, 2013) | ||
| Self-advocacy skills | – | – | Transgender youth of color discussed how their self-advocacy skills helped them stand up for themselves (Singh, 2013) | ||
| Relationship | Romantic or sexual partnerships | Communication with Sexual Partner | High-Risk Sex (i.e., unprotected anal intercourse) (Garofalo et al., 2006) | – | Young transwomen discussed communicating with their steady partners that they would not use condoms with each other, but use condoms with commercial or casual partners to prevent HIV infection; this was usually done alongside HIV testing (Wilson etal., 2012) |
| Parents and families | Parental support | Depressive symptoms (Simons et al., 2013) | - | Transgender college students reported that support and acceptance by family improved their mental health and contributed to a positive sense of self; the types of support that were perceived as positive were asking questions to understand transgender experience & assisting with/affirming participants’ transition (Pusch, 2005) | |
| Perceived burden (Simons et al., 2013) | |||||
| Life Satisfaction (Simons et al., 2013) | |||||
| Transgender youth discussed how support from family increased their sense of racial/ethnic and gender identity (Singh, 2013) | |||||
| Young transwomen with strong parental support reported their mothers helped them to develop a new “kinship as woman”, affirming their gender identity (Gutierrez, 2004) | |||||
| Young transwomen who had at least one supportive parent tended to use condoms more consistently than participants without parental support (Gutierrez, 2004) | |||||
| Family cohesion | Self-esteem (Stotzer et al., 2014) |
Non-significant
|
- | ||
| Sexual Self-Efficacy (Stotzer et al., 2014) | |||||
| Later Age at First Intercourse (Stotzer et al., 2014) | |||||
| Trusted adults | Supportive educators/school staff | Absenteeism (Greytak et al., 2013) | - | Transsexual college students discussed how having faculty who were aware and supportive of transgender issues improved their academic experience (Goodrich, 2012) | |
| Feelings of safety at school (McGuire et al., 2010) | |||||
| – | Transgender youth reported that intervention from teachers in on-campus harassment was infrequent, but effective when enacted (McGuire et al., 2010) | ||||
| Transgender youth noted that adult advocates inside the school system were important sources of tangible support—they worked with youth to navigate the barriers (i.e., legal names, bathrooms) to well-being inside the school system (McGuire et al., 2010) | |||||
| Transgender youth shared that having educators or school staff that cared or advocated for them stopped them from dropping out, even if they experienced victimization and harassment (Sausa, 2005) | |||||
| Transgender role models | – | – | Transgender youth shared that having a positive transgender adult role model improved their educational and career aspirations (Bopp et al., 2004) | ||
| Helpful service providers | – | – | MtF transgender youth reported that service providers advised them and offered mentorship which affirmed their trans identities (Corliss et al., 2007) | ||
| MtF transgender youth reported that helpful service providers assisted with “obtaining public health insurance, housing, legal name or gender change” (Corliss et al., 2007) | |||||
| Peers | Peer support/acceptance (includes positive relationships with peers, support of friends) | Quality of peer relations (child behavior checklist (CBC) Psychopathology; Zucker et al., 2002) | – | Transgender youth reported that friend and peer support helped combat feelings of isolation, loneliness, and depression (Bopp et al., 2004) | |
| MTF transgender youth discussed friends providing information about where to find transgender social services (Corliss et al., 2007) | |||||
| Transgender college students reported that support and acceptance by friends and peers improved their mental health and contributed to a positive sense of self (see parental support for examples) (Pusch, 2005) | |||||
| Transgender youth discussed how support from family and friends increased their sense of racial/ ethnic and gender identity (Singh, 2013) | |||||
| Transgender and genderqueer youth discussed the role their supportive social networks played in helping them avoid street homelessness, specifically they shared information on survival (Reck, 2009) | |||||
| Transgender and genderqueer youth noted that being connected with similar people increased their comfort with their identity (Reck, 2009) | |||||
| Chosen Kin (“alternatives to family of origin”) | – | – | Some young trans women without support from their families reported that building connections with other transgender women provided an alternative family to provide support (Wilson et al., 2012) | ||
| Social support | Social support | High-risk sex (i.e., unprotected anal intercourse) (Garofalo et al., 2006) |
Non-significant:
|
- | |
| Depression (Grossman et al, 2011) | |||||
| Internalizing Problems (Grossman et al, 2011) | |||||
Risk:
|
|||||
| Community | School policies | Anti-bullying/-harassment Policies in Schools | Absenteeism (Greytak et al., 2013) | – | – |
| (includes their existence and enforcement) | |||||
| School Curricula Inclusive of LGBT Identities | Absenteeism (Greytak et al., 2013) | – | – | ||
| School Protective Factors | Connection to an Adult at School (McGuire et al., 2010) |
Non-significant:
|
– | ||
| (composite of (1) teachers intervened in bias-motivated harassment, (2) presence of school harassment policy, (3) LGBT information available, (4) inclusion of LGBT content in curricula, (5) presence of a GSA) | Feelings of Safety (indirect effect through Connection to Adult at School) (McGuire et al., 2010) | ||||
| Organizational resources | GSAs | Absenteeism (Greytak et al., 2013) | – | Transgender youth believed that GSAs improved the school climate (McGuire et al., 2010) | |
| Transgender youth of color reported that joining GSAs helped them develop self-advocacy skills (Singh, 2013) | |||||
| Alternative/charter schools | – | – | Some transgender youth reported surviving in traditional school environments to be impossible, and so transferred to alternative or charter schools with more accepting climates (McGuire et al., 2010) | ||
| Transgender health and social services (includes community safe spaces for LGBT youth, transgender affirming health care on campus) | – | – | MtF transgender youth discussed how workshops and support groups for transgender people increased feeling of social support and added comfort with their identity (Corliss et al., 2007) | ||
| MtF transgender youth appreciated comprehensive transgender medical services which provided access to both hormones and medical monitoring of the hormones (Corliss et al., 2007) | |||||
| Transgender and genderqueer youth discussed how safe spaces in the Castro district (a historic LGBTQ neighborhood in San Francisco) allowed them to build community with each other, connect to the LGBT community broadly, express themselves, and feel safe (Reck, 2009) | |||||
| Trans youth disclosed that having access to trans-affirming campus health care helped them survive life obstacles including trans prejudice and lack of support (i.e., built resilience) (Singh etal., 2013) | |||||
| Community visibility | Transgender community (includes connection to and involvement in a trans community) | – |
Non-significant:
|
Transsexual college students shared that connecting with other transgender individuals enabled them to find mentors and was a positive experience (Goodrich, 2012) | |
| Transgender youth of color shared that interactions with other LGBTQQ youth of color in school or community organizations built up their resilience (Singh, 2013) | |||||
| Trans youth participants named that support from trans-affirming community/allies on campus helped facilitate their resilience and self-advocacy skills (Singh etal., 2013) | |||||
| Diverse faculty, staff, and studer body | – | – | Female transgender students of color reported feeling more comfortable when others with their gender and racial identities were present on campus (Gutierrez, 2004) | ||
| On-campus activism | – | – | Trans-spectrum youth reported that engaging in on-campus activism helped them to feel empowered and know their rights (Jones & Hillier, 2013) |
No protective factors were identified at the societal level of the ecological model
Individual-Level Protective Factors
Beliefs/Perceptions
Five factors capturing beliefs and perceptions for transgender youth demonstrated some protective associations with health and well-being: self-esteem, body esteem, religiosity, positive sense of self, and self-efficacy. In quantitative articles, higher self-esteem was protectively associated with less engagement in high risk sex among young transgender women (Garofalo et al., 2006); however, non-significant associations were found between self-esteem and various mental health outcomes, including depression (Grossman et al., 2011). Qualitatively, youth reported that increasing their self-esteem helped them avoid suicide (Bopp, Juday, & Charters, 2004). In quantitative studies, two dimensions of body esteem (i.e., weight satisfaction and positive body attribution) were associated with fewer attempted suicides, but no association was found with a third body esteem dimension (i.e., appearance satisfaction; Grossman & D’Augelli, 2007). Religiosity was measured by religious attitudes and practices. Strength of formal religious practice (e.g., meditation, attending services) had a protective association with sexual risk (i.e., an index of frequency of unprotected receptive anal intercourse or URAI, multiple anal sex partners, and sex work) for transgender youth, while religious attitudes (e.g., beliefs about God, religious self-description) was not associated with sexual risk (Dowshen et al., 2011). Youth suggested that increasing their sexual self-efficacy (i.e., the belief that they could negotiate condoms and refuse unsafe sex) allowed them to better negotiate healthy relationships and sexuality (Bopp et al., 2004), and that a clear and positive sense of self (i.e., defining their gender or racial identities in a positive way) helped them cultivate feelings of pride and empowerment (Singh, 2013).
Skills/Competencies
Four factors had some support as protective skills or competencies for transgender youth: personal mastery, ability to use internet or social media for information or support, problem solving skills, and self-advocacy skills. Personal mastery (i.e., feeling able to impact important life outcomes) was associated with a lower risk of depression and fewer symptoms of mental trauma, but was not associated with other internalizing and externalizing disorders and an overall measure of mental health problems (Grossman et al., 2011). In qualitative studies, youth discussed using problem solving skills to challenge or change their families’ anti-trans feelings, and to find more inclusive spaces (Jones & Hillier, 2013). Self-advocacy skills helped youth stand up for themselves when facing harassment (Singh, 2013). Youth also reported using the internet and social media to find resources, educational materials, and health information, and to connect to role models who shared their gender and racial identities (Goodrich, 2012; Singh, 2013).
Relationship-Level Protective Factors
Parents and Families
Family cohesion and parental support exhibited some support as protective. Family cohesion (i.e., strong familial ties) was associated with higher self-esteem, higher sexual self-efficacy, and later age of first intercourse for transgender youth, but was not related to number of sexual partners, substance abuse behaviors (i.e., selling drugs; age at first use of tobacco, alcohol, and illegal substances besides marijuana), incarceration, and prostitution (Stotzer, Ka’opua, & Diaz, 2014). Parental support was protectively associated with fewer depressive symptoms, perceived burden of being transgender, and improved life satisfaction (Simons, Schrager, Clark, Belzer, & Olson, 2013). In qualitative studies, transgender youth discussed how support of friends and family improved their mental health and sense of self (Pusch, 2005) and how family support improved their self-definition of marginalized gender and racial identities (Singh, 2013). Transgender girls and young women with at least one supportive parent discussed using condoms more consistently than participants without such support, and some reported developing a new “kinship as woman” through supportive relationships with their mothers (Wilson et al., 2012).
Trusted Adults
Three factors, supportive educators and staff, transgender role models, and helpful service providers, were assessed as protective. Having a relationship with a supportive educator was associated with less school absenteeism for transgender youth (Greytak, Kosciw, & Boesen, 2013) and feelings of safety at school (McGuire et al., 2010). In qualitative reports, transgender youth relayed that the presence of school staff who advocated for them, including teachers, made them less likely to drop out, even if they experienced victimization and harassment (Sausa, 2005); faculty who were aware and supportive of transgender issues also improved these youth’s academic experience (Goodrich, 2012). Transgender youth also reported that adult advocates (often school staff) were critical to the successful navigation of structural barriers in the school system (McGuire et al., 2010), that adult transgender role models improved their educational and career aspirations (Bopp et al., 2004), and that adults at social service agencies aided them in obtaining housing, health insurance, and changes to their legal name or lived gender and were sources of emotional support and mentorship (Corliss, Belzer, Forbes, & Wilson, 2007).
Peers
Peer support and networks had some evidence for being protective. In a sample of youth diagnosed with gender dysphoria, those who reported higher quality peer support also reported fewer psychological symptoms (i.e., depression, social withdrawal, aggression; Zucker et al., 2002). Qualitatively, transgender/GV youth claimed support from friends and peers improved their positive sense of self (Singh, 2013) and helped maintain their mental health (Pusch, 2005). Transgender/GV youth who increased their friend networks and peer support reported fewer of the negative effects of depression, felt more comfortable opening up and discussing issues, and felt less isolated and lonely (Bopp et al., 2004). Youth with transgender friends also reported having a more positive sense of self (Reck, 2009) and being better able to find information about transgender-supportive social services (Corliss et al., 2007; Reck, 2009). Finally, for some, friendship networks acted as a family of choice (i.e., chosen kin) after rejection from families of origin (Wilson et al., 2012).
Generalized Social Support
Generalized social support (i.e., emotional and tangible support from family and friends) demonstrated mixed effects. For young transgender women, high levels of social support were associated with a reduced likelihood of engaging in unprotected anal intercourse (Garofalo et al., 2006) and with fewer symptoms of depression and fewer problems with internalizing behaviors (Grossman et al., 2011), but had nonsignificant associations with externalizing behaviors, symptoms of trauma, and an overall measure of mental health problems (Grossman et al., 2011). Conversely, one cross-sectional article found high levels of social support to be associated with a greater likelihood of engagement in sex work among young transgender women (Wilson et al., 2009).
Romantic or Sexual Partnerships
Health protective communication (i.e., discussions about safer sex) was associated with less unprotected anal intercourse for young transgender women (Garofalo et al., 2006). Young transgender women also qualitatively reported that open communication informed sexual health decision-making with their main partner (Wilson et al., 2012). These women reported that they discussed and confirmed through testing both their own and their partners’ HIV status before stopping condom use, and continued to use condoms with casual partners outside the primary relationship to reduce the risk of HIV infection (Wilson et al., 2012).
Community-Level Protective Factors
School Policies
School policies against bullying and LGBT inclusive curricula demonstrated some evidence of being protective. McGuire et al. (2010) created a composite measure of “school protective factors” (i.e., school harassment policy, LGBT content in curricula, LGBT information on campus, GSA on campus, and teacher intervention in bias-motivated harassment). High scores on this measure were directly associated with a greater likelihood of transgender youth expressing a connection to an adult at school and indirectly associated with increased feelings of safety (i.e., an indirect effect mediated by connection to an adult at school); however, they were not directly associated with increased feelings of safety (McGuire et al., 2010). Additionally, school policies against bullying and harassment and an LGBT inclusive curriculum were each independently associated with less absenteeism among transgender students (Greytak et al., 2013).
Organizational Resources
GSAs, alternative/charter schools, and transgender health and social services were three organizational resources with support for being protective. The presence of a GSA was protectively associated with reduced absenteeism for transgender students (Greytak et al., 2013). Transgender students qualitatively reported that joining a GSA helped them to develop self-advocacy skills (Singh, 2013) and that having a GSA improved school climate (McGuire et al., 2010). Transgender youth also discussed alternative and charter schools as a critical educational resource when traditional schools did not provide a hospitable climate (McGuire et al., 2010). The availability of transgender health and social services in schools and neighborhoods was cited as important for finding emotional support for and tangible assistance with legal and medical transitions (Corliss et al., 2007; Singh, Meng, & Hansen, 2013). For homeless transgender youth, access to safe, LGBT-friendly youth centers was important to building support and feelings of safety (Reck, 2009).
Community Visibility
School diversity, on-campus activism, and a visible transgender community showed some support for being protective. Transgender youth reported that the presence of visible LGBTQQ (i.e., lesbian, gay, bisexual, transgender, queer, and questioning) communities and allies in school improved school climate and contributed to their development of self-advocacy skills and resilience (Singh, 2013; Singh et al., 2013). Youth also expressed feeling more comfortable with their racial and gender identities when they attended schools with diverse faculty and student bodies (Gutierrez, 2004). Transgender youth also appreciated opportunities for on-campus activism and found they led to increased knowledge about rights and feelings of empowerment (Jones & Hillier, 2013). Finally, transgender youth qualitatively shared that finding community with other transgender people was positive and improved their academic experiences (Goodrich, 2012), while involvement in the transgender community was not associated with engagement in sex work (Wilson et al., 2009).
Discussion
Across the 21 included articles, 27 unique factors were related to positive health and well-being for transgender/GV youth, but only seven of these factors demonstrated protective relationships in multiple quantitative and qualitative studies. While the frequency with which factors appeared as protective in the evidence does not indicate the magnitude of their effects on health, it does indicate which have the most preliminary support as protective for transgender/GV youth.
At the individual-level, self-esteem was the only factor with support as protective for transgender/GV youth across both qualitative and quantitative articles. While self-esteem was mostly protective for youth in this review, other studies indicate that self-esteem has no effect or even risky effects among LGB and non-LGBT youth groups (Armstrong et al., 2016; Goodson, Buhi, & Dunsmore, 2006; Shrier et al., 2001). As such, evaluating how self-esteem functions similarly or differently within different populations may help to understand its utility as a potential protective factor for transgender/GV youth.
At the relationship-level, support of parents, peers, and trusted adults emerged as central to the well-being of transgender/GV youth (Corliss et al., 2007; Pusch, 2005; Simons et al., 2013; Stotzer et al., 2014; Wilson et al., 2012; Zucker et al., 2002). The importance of parental support echoes research on all youth (Resnick et al., 1997) and on LGB youth in particular (Ryan et al., 2010). Furthermore, this finding is consistent with what has been observed among transgender adults, where support from family members has been tied to reductions in suicidal behavior (Bauer et al., 2015; Moody & Smith, 2013), and thus appears to be a protective factor critical to the health of individuals with stigmatized identities. The benefits of peer support to the mental health of transgender/GV youth also aligns with trends observed for all youth (Forney & Miller, 2012; La Greca & Harrison, 2005; Scott et al., 2014). However, because parent and peer relationships are frequent sources of harassment and victimization for transgender/GV youth (Factor & Rothblum, 2008; Kosciw & Diaz, 2006; Poteat et al., 2011; Roberts et al., 2012; Sevelius, 2013), questions remain about how to strengthen these connections. Other adults (e.g., teachers and school staff) are sometimes the only sources of support available (Goodrich, 2012; Greytak et al., 2013; McGuire et al., 2010; Pusch, 2005; Reck, 2009; Sausa, 2005). These extra-familial trusted adults may be resources to help families and peers better understand gender variance.
At the community level, schools can also play an important role in the lives of transgender/GV youth, both through supportive teachers and staff and through the resources they provide. School-based GSAs emerged at the community level as a potentially protective resource for transgender/GV youth with protective associations across studies (Greytak et al., 2013; McGuire et al., 2010; Singh, 2013). The protective benefits of GSAs have been documented for LGB youth (Saewyc, Konishi, Rose, & Homma, 2014; Toomey et al., 2011; Walls, Kane, & Wisneski, 2009) and their protective effect for transgender/GV youth is promising, although questions remain as to how GSAs might be better designed to meet the needs of LGB and transgender/GV youth simultaneously. Absent from the literature, and consequently this review, were articles evaluating societal level protective factors, leaving questions as to the protective effects of laws and governmental policies on transgender/GV youth.
Unexpectedly, one article found that a traditional health protective factor, the relationship-level characteristic of social support, was associated with a greater likelihood of engaging in sex work (Wilson et al., 2009); however, this may not imply direction of causality or reflect real world risk. The connection between social support and sex work was explained by article authors as potentially resulting from either a lack of measurement clarity (i.e., youth not engaged in sex work may answer social support questions about family, while youth engaged in sex work may answer about friends), or a reflection of the unique social support transgender women engaged in sex work offer each other (Wilson et al., 2009).
Additionally, this review highlights patterns within the scientific study of protective factors among transgender/GV youth. First, there is little consistency as to how researchers measure and classify transgender/GV youth identities. An academic discussion of how best to measure transgender identities in survey research is ongoing (Gates 2015; Reisner et al., 2014a; Sausa et al., 2009), with movement toward standardized use of a two-step approach (i.e., asking participants to report the sex on their birth certificate and current gender; Gates 2015; L. Sausa et al., 2009); this review reveals some tardiness as to its uptake. As more researchers employ this method, comparing protective relationships among transgender/GV youth across research studies and examining within group differences will become more possible.
Second, all the articles included in our review used convenience samples with well-recognized limits to their generalizability (Meyer & Wilson, 2009); however, using convenience samples to access hard to reach populations is consistent with early work on LGB and other marginalized populations and likely indicates the novelty of this field of study (Armstrong et al., 2016; Johns et al., 2018; Rothblum, 2007). Researchers should consider novel methods such as combining venue-based sampling with quotas to insure adequate racial and gender diversity or time–space sampling of community venues to control for sampling bias derived from recruiting the entire sample at one point in time (Meyer & Wilson, 2009). Respondent-driven sampling using key informants from hard-to-reach subpopulations of transgender/ GV youth may also increase diversity in the sample and can help to capture the experiences of youth who do not actively frequent community venues (Forrest et al., 2016). In addition, longitudinal research would facilitate examination of the pathways between factors theorized as protective and health outcomes.
Furthermore, the quantitative and qualitative findings in this review provide the reader with complementary, but distinct, implications for continued research on this topic. Factors which demonstrate some protective effects in quantitative data, such as personal mastery (Grossman et al., 2011) and supportive educators (Greytak et al., 2013; McGuire et al., 2010), would benefit from continued study. Specifically, further assessment of the protective factors in this sample with additional untested health and behavioral outcomes would enable researchers to understand the full range of these factors’ protective effects; while replication of previously observed relationships between protective factors and their outcomes within surveys using the methodological advancements suggested above would enable a more robust understanding of these factors’ generalizability. Qualitative findings unrepresented in the quantitative data, such as self-efficacy (Bopp et al., 2004) and transgender health and social services (Corliss et al., 2007; Reck, 2009; Singh et al., 2013), may be used to guide measurement and survey development for quantitative analysis. Testing qualitative pathways quantitatively in well-designed surveys could also establish the generalizability of these factors as protective for transgender/GV youth.
Although intervention research was not included in this review, two types of interventions did appear in initial search results and showed beneficial effects on both protective factors and health outcomes. Medical interventions such as pubertal suppression and gender reassignment surgery appear to improve self-concept and reduce negative mental health outcomes among youth who elect these procedures (de Vries et al. 2011, 2014; Smith, van Goozen, & Cohen-Kettenis, 2001). Additionally, peer-based interventions for transgender/GV youth appear to strengthen communication skills and support networks (Bopp et al., 2004; Garofalo et al., 2012). These findings support possibly adapting positive youth development interventions that increase protective factors and improve health and well-being of other groups of marginalized youth for transgender/GV youth (Gavin et al., 2010; Lerner et al., 2005).
Some additional limitations of this review should be noted. First, the articles included in this study are limited by our search criteria. While we aimed to be inclusive of all transgender/GV identities, articles that did not include the chosen search terms (Table 1) might have been missed. Second, our results may be limited by publication bias. While this review provides a thorough summation of the peer-reviewed science on protective factors and transgender/GV youth, researchers particularly interested in innovative methods might choose to supplement it with a scan of the gray literature.
Conclusions
Overall, our findings affirm that research on transgender/GV youth and protective factors is in a nascent stage. As the first comprehensive mapping of protective factors for transgender/gender variant youth, the results of this review may provide an introduction for scientists and practitioners who are new to this field. Mapping factors from quantitative and qualitative studies within the socioecological model provides a theoretically driven guide for identifying protective factors that have received adequate attention and those in need of continued empirical investigation. Because scientific inquiry into this topic is relatively new, expansion of the research base through novel recruitment strategies that include diverse and representative transgender/GV youth and through longitudinal studies evaluating the effects of protective factors over time is needed. Schools and other community-based organizations may use the information on protective factors provided here to inform programs and interventions that strengthen the health and well-being of transgender/ GV youth.
Acknowledgments
This research has been supported by a grant from the Arcus Foundation awarded to the CDC Foundation. The authors would like to thank Riley Steiner and Nicole Liddon for their significant contributions to the conceptualization of this study and invaluable feedback during the writing process.
Footnotes
Disclaimer The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Compliance With Ethical Standards
Conflict of Interest The authors declare they have no conflicts of interest.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Armstrong HL, Steiner RJ, Jayne PE, Beltran O. Individual-level protective factors for sexual health outcomes among sexual minority youth: A systematic review of the literature. Sex Health. 2016;13:311–327. doi: 10.1071/SH15200. https://doi.org/10.1071/SH15200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aspenlieder L, Buchanan CM, McDougall P, Sippola LK. Gender nonconformity and peer victimization in pre-and early adolescence. International Journal of Developmental Science. 2009;3(1):3–16. [Google Scholar]
- Baral SD, Poteat T, Stro¨mdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: A systematic review and meta-analysis. The Lancet Infectious Diseases. 2013;13(3):214–222. doi: 10.1016/S1473-3099(12)70315-8. https://doi.org/10.1016/s1473-3099(12)70315-8. [DOI] [PubMed] [Google Scholar]
- Bauer GR, Scheim AI, Pyne J, Travers R, Hammond R. Intervenable factors associated with suicide risk in transgender persons: A respondent driven sampling study in Ontario, Canada. BMC Public Health. 2015;15:525. doi: 10.1186/s12889-015-1867-2. https://doi.org/10.1186/s12889-015-1867-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the US transgender population. American Journal of Public Health. 2013;103(5):943–951. doi: 10.2105/AJPH.2013.301241. https://doi.org/10.2105/AJPH.2013.301241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bopp PJ, Juday TR, Charters CW. A school-based program to improve life skills and to prevent HIV infection in multicultural transgendered youth in Hawai’i. Journal of Gay & Lesbian Issues in Education. 2004;1(4):3–21. [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Carroll L, Gilroy PJ, Ryan J. Counseling transgendered, transsexual, and gender-variant clients. Journal of Counseling & Development. 2002;80:131–139. [Google Scholar]
- Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: Implications for public health intervention. American Journal of Public Health. 2001;91(6):915–921. doi: 10.2105/ajph.91.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corliss HL, Belzer M, Forbes C, Wilson EC. An evaluation of service utilization among male to female transgender youth: Qualitative study of a clinic-based sample. Journal of LGBT Health Research. 2007;3(2):49–61. doi: 10.1300/J463v03n02_06. [DOI] [PubMed] [Google Scholar]
- D’Augelli AR, Grossman AH, Starks MT. Parents’ awareness of lesbian, gay, and bisexual youths’ sexual orientation. Journal of Marriage and Family. 2005;67(2):474–482. https://doi.org/10.1111/j.0022-2445.2005.00129.x. [Google Scholar]
- De Santis JP. HIV infection risk factors among male-to-female transgender persons: A review of the literature. Journal of the Association of Nurses in AIDS Care. 2009;20(5):362–372. doi: 10.1016/j.jana.2009.06.005. https://doi.org/10.1016/j.jana.2009.06.005. [DOI] [PubMed] [Google Scholar]
- de Vries AL, McGuire JK, Steensma TD, Wagenaar EC, Doreleijers TA, Cohen-Kettenis PT. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics. 2014;134(4):696–704. doi: 10.1542/peds.2013-2958. https://doi.org/10.1542/peds.2013-2958. [DOI] [PubMed] [Google Scholar]
- de Vries AL, Steensma TD, Doreleijers TA, Cohen-Kettenis PT. Puberty suppression in adolescents with gender identity disorder: A prospective follow-up study. Journal of Sexual Medicine. 2011;8(8):2276–2283. doi: 10.1111/j.1743-6109.2010.01943.x. https://doi.org/10.1111/j.1743-6109.2010.01943.x. [DOI] [PubMed] [Google Scholar]
- Dowshen N, Forke CM, Johnson AK, Kuhns LM, Rubin D, Garofalo R. Religiosity as a protective factor against HIV risk among young transgender women. Journal of Adolescent Health. 2011;48(4):410–414. doi: 10.1016/j.jadohealth.2010.07.021. https://doi.org/10.1016/j.jadohealth.2010.07.021. [DOI] [PubMed] [Google Scholar]
- Factor RJ, Rothblum ED. A study of transgender adults and their non-transgender siblings on demographic characteristics, social support, and experiences of violence. Journal of LGBT Health Research. 2008;3(3):11–30. doi: 10.1080/15574090802092879. https://doi.org/10.1080/15574090802092879. [DOI] [PubMed] [Google Scholar]
- Fenway Health (Producer) [Accessed 15 July 2016];Glossary of gender and transgender terms. 2010 Retrieved from http://www.lgbthealtheducation.org/wp-content/uploads/Handout_7-C_Glossary_of_Gender_and_Transgender_Terms__fi.pdf.
- Fergus S, Zimmerman MA. Adolescent resilience: A framework for understanding healthy development in the face of risk. Annual Review of Public Health. 2005;26:399–419. doi: 10.1146/annurev.publhealth.26.021304.144357. https://doi.org/10.1146/annurev.publhealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]
- Forney JC, Miller RL. Risk and protective factors related to HIV-risk behavior: A comparison between HIV-positive and HIV-negative young men who have sex with men. AIDS Care. 2012;24(5):544–552. doi: 10.1080/09540121.2011.630341. https://doi.org/10.1080/09540121.2011.630341. [DOI] [PubMed] [Google Scholar]
- Forrest JI, Lachowsky NJ, Lal A, Cui Z, Sereda P, Raymond HF, et al. Factors associated with productive recruiting in a respondent-driven sample of men who have sex with men in Vancouver, Canada. Journal of Urban Health. 2016;93(2):379–387. doi: 10.1007/s11524-016-0032-2. https://doi.org/10.1007/s11524-016-0032-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Johnson AK, Kuhns LM, Cotten C, Joseph H, Margolis A. Life Skills: Evaluation of a theory-driven behavioral HIV prevention intervention for young transgender women. Journal of Urban Health. 2012;89(3):419–431. doi: 10.1007/s11524-011-9638-6. https://doi.org/10.1007/s11524-011-9638-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Osmer E, Sullivan C, Doll M, Harper G. Environmental, psychosocial, and individual correlates of HIV risk in ethnic minority male-to-female transgender youth. Journal of HIV/AIDS Prevention in Children & Youth. 2006;7(2):89–104. http://dx.doi.org/10.1300/J499v07n02_06. [Google Scholar]
- Gates GJ. The importance of CHIS in LGBT research and data collection. [Accessed 15 July 2016];The Center’s Health Policy Seminar Series. 2015 (Producer). Retrieved from https://connectpro72759986.adobeconnect.com/_a782517175/p3uaryg8a25/?launcher=false&fcsContent=true&pbMode=normal.
- Gavin LE, Catalano RF, David-Ferdon C, Gloppen KM, Markham CM. A review of positive youth development programs that promote adolescent sexual and reproductive health. Journal of Adolescent Health. 2010;46(3 Suppl):S75–S91. doi: 10.1016/j.jadohealth.2009.11.215. https://doi.org/10.1016/j.jadohealth.2009.11.215. [DOI] [PubMed] [Google Scholar]
- Goodrich KM. Lived experiences of college-age transsexual individuals. Journal of College Counseling. 2012;15(3):215–232. http://dx.doi.org/10.1002/j.2161-1882.2012.00017.x. [Google Scholar]
- Goodson P, Buhi ER, Dunsmore SC. Self-esteem and adolescent sexual behaviors, attitudes, and intentions: A systematic review. Journal of Adolescent Health. 2006;38(3):310–319. doi: 10.1016/j.jadohealth.2005.05.026. https://doi.org/10.1016/j.jadohealth.2005.05.026. [DOI] [PubMed] [Google Scholar]
- Gordon AR, Meyer IH. Gender nonconformity as a target of prejudice, discrimination, and violence against LGB indviduals. Journal of LGBT Health Research. 2007;3(3):55–71. doi: 10.1080/15574090802093562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greytak EA, Kosciw JG, Boesen MJ. Putting the “T” in “resource”: The benefits of LGBT-related school resources for transgender youth. Journal of LGBT Youth. 2013;10(1–2):45–63. http://dx.doi.org/10.1080/19361653.2012.718522. [Google Scholar]
- Grossman AH, D’Augelli AR. Transgender youth: Invisible and vulnerable. Journal of Homosexuality. 2006;51(1):111–128. doi: 10.1300/J082v51n01_06. https://doi.org/10.1300/J082v51n01_06. [DOI] [PubMed] [Google Scholar]
- Grossman AH, D’Augelli AR. Transgender youth and life-threatening behaviors. Suicide and Life-Threatening Behavior. 2007;37(5):527–537. doi: 10.1521/suli.2007.37.5.527. [DOI] [PubMed] [Google Scholar]
- Grossman AH, D’Augelli AR, Frank JA. Aspects of psychological resilience among transgender youth. Journal of LGBT Youth. 2011;8(2):103–115. [Google Scholar]
- Gutierrez N. Resisting fragmentation, living whole: Four female transgender students of color speak about school. Journal of Gay & Lesbian Social Services. 2004;16(3–4):69–79. [Google Scholar]
- Hall JE, Simon TR, Lee RD, Mercy JA. Implications of direct protective factors for public health research and prevention strategies to reduce youth violence. American Journal of Preventive Medicine. 2012;43(2 Suppl 1):S76–S83. doi: 10.1016/j.amepre.2012.04.019. https://doi.org/10.1016/j.amepre.2012.04.019. [DOI] [PubMed] [Google Scholar]
- Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the minority stress model. Professional Psychology—Research & Practice. 2012;43(5):460–467. [Google Scholar]
- Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: A systematic review. AIDS and Behavior. 2008;12(1):1–17. doi: 10.1007/s10461-007-9299-3. https://doi.org/10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- Ignatavicius S. Stress in female-identified transgender youth: A review of the literature on effects and interventions. Journal of LGBT Youth. 2013;10(4):267–286. https://doi.org/10.1080/19361653.2013.825196. [Google Scholar]
- Ivankovich MB, Fenton KA, Douglas JM. Considerations for national public health leadership in advancing sexual health. Public Health Reports. 2013;128(Supplement 1):102–110. doi: 10.1177/00333549131282S112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns MM, Liddon N, Jayne PE, Beltran O, Steiner RJ, Morris E. Systematic mapping of relationship-level protective factors and sexual health outcomes among sexual minority youth: The role of peers, parents, partners, and providers. LGBT Health. 2018 doi: 10.1089/lgbt.2017.0053. https://doi.org/10.1089/lgbt.2017.0053. [DOI] [PMC free article] [PubMed]
- Jones T, Hillier L. Comparing trans-spectrum and same-sex-attracted youth in Australia: Increased risks, increased activisms. Journal of LGBT Youth. 2013;10(4):287–307. http://dx.doi.org/10.1080/19361653.2013.825197. [Google Scholar]
- Kosciw JG, Diaz EM. The 2005 National School Climate Survey: The experiences of lesbian, gay, bisexual and transgender youth in our nation’s schools. New York: GLSEN; 2006. [Google Scholar]
- La Greca AM, Harrison HM. Adolescent peer relations, friendships, and romantic relationships: Do they predict social anxiety and depression? Journal of Clinical Child & Adolescent Psychology. 2005;34(1):49–61. doi: 10.1207/s15374424jccp3401_5. https://doi.org/10.1207/s15374424jccp3401_5. [DOI] [PubMed] [Google Scholar]
- Lerner RM, Almerigi JB, Theokas C, Lerner JV. Positive youth development: A view of the issues. Journal of Early Adolescence. 2005;25(1):10–16. https://doi.org/10.1177/0272431604273211. [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Medicine. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire JK, Anderson CR, Toomey RB, Russell ST. School climate for transgender youth: A mixed method investigation of student experiences and school responses. Journal of Youth and Adolescence. 2010;39(10):1175–1188. doi: 10.1007/s10964-010-9540-7. http://dx.doi.org/10.1007/s10964-010-9540-7. [DOI] [PubMed] [Google Scholar]
- Meyer IH, Wilson PA. Sampling lesbian, gay, and bisexual populations. Journal of Counseling Psychology. 2009;56(1):23–31. doi: 10.1037/a0012844. https://doi.org/10.1037/a0014587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mmari K, Blum RW. Risk and protective factors that affect adolescent reproductive health in developing countries: A structured literature review. Global Public Health. 2009;4(4):350–366. doi: 10.1080/17441690701664418. https://doi.org/10.1080/17441690701664418. [DOI] [PubMed] [Google Scholar]
- Moody C, Smith NG. Suicide protective factors among trans adults. Archives of Sexual Behavior. 2013;42(5):739–752. doi: 10.1007/s10508-013-0099-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemoto T, Operario D, Keatley J, Han L, Soma T. HIV risk behaviors among male-to-female transgender persons of color in San Francisco. American Journal of Public Health. 2004;94(7):1193–1199. doi: 10.2105/ajph.94.7.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newfield E, Hart S, Dibble S, Kohler L. Female-to-male transgender quality of life. Quality of Life Research. 2006;15(9):1447–1457. doi: 10.1007/s11136-006-0002-3. https://doi.org/10.1007/s11136-006-0002-3. [DOI] [PubMed] [Google Scholar]
- Operario D, Soma T, Underhill K. Sex work and HIV status among transgender women: Systematic review and meta-analysis. Journal of Acquired Immune Deficiency Syndromes. 2008;48(1):97–103. doi: 10.1097/QAI.0b013e31816e3971. [DOI] [PubMed] [Google Scholar]
- Poteat VP, Mereish EH, Digiovanni CD, Koenig BW. The effects of general and homophobic victimization on adolescents’ psychosocial and educational concerns: The importance of intersecting identities and parent support. Journal of Counseling Psychology. 2011;58(4):597–609. doi: 10.1037/a0025095. https://doi.org/10.1037/a0025095. [DOI] [PubMed] [Google Scholar]
- Pusch RS. Objects of curiosity: Transgender college students’ perceptions of the reactions of others. Journal of Gay & Lesbian Issues in Education. 2005;3(1):45–61. [Google Scholar]
- Reck J. Homeless gay and transgender youth of color in San Francisco: “No one likes street kids”—Even in the Castro. Journal of LGBT Youth. 2009;6(2–3):223–242. [Google Scholar]
- Reisner SL, Conron KJ, Tardiff LA, Jarvi S, Gordon AR, Austin SB. Monitoring the health of transgender and other gender minority populations: Validity of natal sex and gender identity survey items in a U.S. national cohort of young adults. BMC Public Health. 2014a;14:1224. doi: 10.1186/1471-2458-14-1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Greytak EA, Parsons JT, Ybarra ML. Gender minority social stress in adolescence: Disparities in adolescent bullying and substance use by gender identity. Journal of Sex Research. 2015a;52(3):243–256. doi: 10.1080/00224499.2014.886321. https://doi.org/10.1080/00224499.2014.886321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Vetters R, Leclerc M, Zaslow S, Wolfrum S, Shumer D, et al. Mental health of transgender youth in care at an adolescent urban community health center: A matched retrospective cohort study. Journal of Adolescent Health. 2015b;56(3):274–279. doi: 10.1016/j.jadohealth.2014.10.264. https://doi.org/10.1016/j.jadohealth.2014.10.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, White JM, Bradford JB, Mimiaga MJ. Transgender health disparities: Comparing full cohort and nested matched-pair study designs in a community health center. Journal of LGBT Health. 2014b;1(3):177–184. doi: 10.1089/lgbt.2014.0009. https://doi.org/10.1089/lgbt.2014.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick MD. Protective factors, resiliency, and healthy youth development. Adolescent Medicine: State of the Art Reviews. 2000a;11(1):157–164. [PubMed] [Google Scholar]
- Resnick MD. Resilience and protective factors in the lives of adolescents. Journal of Adolescent Health. 2000b;27:1–2. doi: 10.1016/s1054-139x(00)00142-7. [DOI] [PubMed] [Google Scholar]
- Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, et al. Protecting adolescents from harm: Findings from the national longitudinal study on adolescent health. Journal of the American Medical Association. 1997;278(10):823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- Roberts AL, Rosario M, Corliss HL, Koenen KC, Austin S. Childhood gender nonconformity: A risk indicator for childhood abuse and posttraumatic stress in youth. Pediatrics. 2012;129(3):410–417. doi: 10.1542/peds.2011-1804. https://doi.org/10.1542/peds.2011-1804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothblum E. From science fiction to computer-generated technology: Sampling lesbian, gay, and bisexual individuals. In: Meyer IH, Northridge ME, editors. The health of sexual minorities: Public health perspectives on lesbian, gay, bisexual, and transgender populations. New York, NY: Springer; 2007. pp. 442–452. [Google Scholar]
- Ryan C, Russell ST, Huebner D, Diaz R, Sanchez J. Family acceptance in adolescence and the health of LGBT young adults. Journal of Child and Adolescent Psychiatric Nursing. 2010;23(4):205–213. doi: 10.1111/j.1744-6171.2010.00246.x. https://doi.org/10.1111/j.1744-6171.2010.00246.x. [DOI] [PubMed] [Google Scholar]
- Saewyc E, Konishi C, Rose H, Homma Y. School-based strategies to reduce suicidal ideation and attempts among lesbian, gay, and bisexual, as well as heterosexual adolescents in Western Canada. International Journal of Child, Youth and Family Studies. 2014;5:89–112. doi: 10.18357/ijcyfs.saewyce.512014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sausa LA. Translating research into practice: Trans youth recommendations for improving school systems. Journal of Gay & Lesbian Issues in Education. 2005;3(1):15–28. [Google Scholar]
- Sausa L, Sevelius J, Keatley J, Iniguez J, Reyes M. Recommendations for inclusive data collection of trans people in HIV prevention, care & services. San Francisco: Center of Excellence for Transgender HIV Prevention; 2009. Retrieved from http://transhealth.ucsf.edu/trans?page=lib-data-collection. [Google Scholar]
- Scott HM, Pollack L, Rebchook GM, Huebner DM, Peterson J, Kegeles SM. Peer social support is associated with recent HIV testing among young black men who have sex with men. AIDS and Behavior. 2014;18(5):913–920. doi: 10.1007/s10461-013-0608-8. https://doi.org/10.1007/s10461-013-0608-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevelius JM. Gender affirmation: A framework for conceptualizing risk behavior among transgender women of color. Sex Roles. 2013;68(11–12):675–689. doi: 10.1007/s11199-012-0216-5. https://doi.org/10.1007/s11199-012-0216-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrier LA, Harris SK, Sternberg M, Beardslee WR. Associations of depression, self-esteem, and substance use with sexual risk among adolescents. Preventive Medicine. 2001;33:179–189. doi: 10.1006/pmed.2001.0869. [DOI] [PubMed] [Google Scholar]
- Simon PA, Reback CJ, Bernis CC. HIV prevalence and incidence among male-to-female transsexuals receiving HIV prevention services in Los Angeles County. AIDS. 2000;14(18):2953–2955. doi: 10.1097/00002030-200012220-00024. [DOI] [PubMed] [Google Scholar]
- Simons L, Schrager SM, Clark LF, Belzer M, Olson J. Parental support and mental health among transgender adolescents. Journal of Adolescent Health. 2013;53(6):791–793. doi: 10.1016/j.jadohealth.2013.07.019. https://doi.org/10.1016/j.jadohealth.2013.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh AA. Transgender youth of color and resilience: Negotiating oppression and finding support. Sex Roles. 2013;68(11–12):690–702. http://dx.doi.org/10.1007/s11199-012-0149-z. [Google Scholar]
- Singh AA, Meng S, Hansen A. “It’s already hard enough being a student”: Developing affirming college environments for trans youth. Journal of LGBT Youth. 2013;10(3):208–223. http://dx.doi.org/10.1080/19361653.2013.800770. [Google Scholar]
- Smith YL, van Goozen SH, Cohen-Kettenis PT. Adolescents with gender identity disorder who were accepted or rejected for sex reassignment surgery: A prospective follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(4):472–481. doi: 10.1097/00004583-200104000-00017. https://doi.org/10.1097/00004583-200104000-00017. [DOI] [PubMed] [Google Scholar]
- Stephens SC, Bernstein KT, Philip SS. Male to female and female to male transgender persons have different sexual risk behaviors yet similar rates of STDs and HIV. AIDS and Behavior. 2011;15(3):683–686. doi: 10.1007/s10461-010-9773-1. https://doi.org/10.1007/s10461-010-9773-1. [DOI] [PubMed] [Google Scholar]
- Stotzer RL. Family cohesion among Hawai ‘i’s Mahuwahine. Journal of GLBT Family Studies. 2011;7(5):424–435. [Google Scholar]
- Stotzer RL, Ka’opua LS, Diaz TP. Is healthcare caring in Hawai’i? Preliminary results from a health assessment of lesbian, gay, bisexual, transgender, questioning, and intersex people in four counties. Hawaii Journal of Medicine & Public Health. 2014;73(6):175–180. [PMC free article] [PubMed] [Google Scholar]
- Testa RJ, Jimenez CL, Rankin S. Risk and resilience during transgender identity development: The effects of awareness and engagement with other transgender people on affect. Journal of Gay & Lesbian Mental Health. 2014;18(1):31–46. https://doi.org/10.1080/19359705.2013.805177. [Google Scholar]
- Toomey RB, Ryan C, Diaz RM, Card NA, Russell ST. Gender-nonconforming lesbian, gay, bisexual, and transgender youth: School victimization and young adult psychosocial adjustment. Developmental Psychology. 2010;46(6):1580–1589. doi: 10.1037/a0020705. https://doi.org/10.1037/a0020705. [DOI] [PubMed] [Google Scholar]
- Toomey RB, Ryan C, Diaz RM, Russell ST. High school gay-straight alliances (GSAs) and young adult well-being: An examination of GSA presence, participation, and perceived effectiveness. Applied Developmental Science. 2011;15(4):175–185. doi: 10.1080/10888691.2011.607378. https://doi.org/10.1080/10888691.2011.607378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walls NE, Kane SB, Wisneski H. Gay-straight alliances and school experiences of sexual minority youth. Youth & Society. 2009;41(3):307–332. https://doi.org/10.1177/0044118X09334957. [Google Scholar]
- Wilson EC, Chen Y-H, Arayasirikul S, Fisher M, Pomart WA, Le V, et al. Differential HIV risk for racial/ethnic minority trans*female youths and socioeconomic disparities in housing, residential stability, and education. American Journal of Public Health. 2015;105(S3):e41–e47. doi: 10.2105/AJPH.2014.302443. https://doi.org/10.2105/ajph.2014.302443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson EC, Garofalo R, Harris RD, Herrick A, Martinez M, Martinez J, Belzer M. Transgender female youth and sex work: HIV risk and a comparison of life factors related to engagement in sex work. AIDS and Behavior. 2009;13(5):902–913. doi: 10.1007/s10461-008-9508-8. http://dx.doi.org/10.1007/s10461-008-9508-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson EC, Iverson E, Garofalo R, Belzer M. Parental support and condom use among transgender female youth. Journal of the Association of Nurses in AIDS Care. 2012;23(4):306–317. doi: 10.1016/j.jana.2011.09.001. http://dx.doi.org/10.1016/j.jana.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker KJ, Owen A, Bradley SJ, Ameeriar L. Gender-dysphoric children and adolescents: A comparative analysis of demographic characteristics and behavioral problems. Clinical Child Psychology and Psychiatry. 2002;7(3):398–411. [Google Scholar]