Abstract
Numerous studies attest to the salubriousness of social participation across contexts. Factors such as health-related behaviour, health risk aversion, and psychosocial traits partly explain this association. While a study of these factors contributes to an understanding of the role that social participation plays in health-related outcomes, significant gaps still exist in this field of investigation. In particular, existing studies have not explored the relationship between social participation and health literacy and how it affects health and well-being adequately. This paper addresses this gap by examining the responses of some 779 rural and urban residents in Ashanti Region in Ghana. The study used path analyses within structural equation modelling (SEM) to assess the mediational role of health literacy in the association between social participation (religious participation, volunteer activities and group membership), and health status and subjective well-being. All the proxies of social participation significantly predicted health literacy. It was also evident that social participation influences health and well-being substantially. After controlling for socio-demographic variables, religious participation and group membership indirectly predicted well-being and health status through health literacy. Volunteer activities showed a negative indirect effect; thus, social participation does not always have a favourable effect on health and well-being. However, the findings suggest that overall, enhancing social participation may be promising for effective health promotion.
Keywords: Health literacy, Social capital, Social participation, Health promotion, Well-being
Highlights
-
•
Social participation predicts health literacy, self-rated health and well-being.
-
•
Health literacy is associated with health and well-being.
-
•
Social participation predicts health and wellbeing through health literacy.
-
•
Social participation can potentially be harnessed for health promotion.
Background
After several years of inquiry, the pathways linking and explaining the relationship between social participation—social sharing of individual resources through active involvement in collective social actions (such as religious activities, hobby clubs, sports groups, cultural and political events) (Lee, Jang, Lee, Cho & Park, 2008)—and health remain unclear and mostly theoretical (Putland et al., 2013, Kawachi and Berkman, 2014, Bruhn, 2009). A similar assertion extends to social capital itself—the resources embedded in actual and potential social relationships—which is tightly bound up with social engagement, mutual trust and community building (Bourdieu, 1986, Putnam, 1995, Kawachi and Berkman, 2014). One potential mechanism that may link social participation and health is health literacy (Lori et al., 2016, Andrzejewski et al., 2009, Lee et al., 2009). Nevertheless, health literacy has also been least studied in several contexts including Ghana (Amoah et al., 2017, Lori et al., 2016). Health literacy refers to “the cognitive and social skills which determine the motivation and ability for individuals to gain access to, understand and use information in ways which propose and maintain good health” (Nutbeam, 2000 p. 264).
Research that backs the influence of social participation on health and well-being is persuasive and consistent across contexts (Yamaoka, 2008, Hyyppä and Mäki, 2003, Väänänen et al., 2009, Takahashi et al., 2011, Helliwell and Putnam, 2004, Yeary et al., 2012). It is argued that social engagements enhance trust and sense of coherence and identity, which are central to the production and maintenance of well-being (Bruhn, 2009, Berkman and Krishna, 2014). For instance, a study in five East Asian countries namely Japan, South Korea, Singapore, China, and Taiwan, observed a positive relationship between group membership and self-rated somatic health (Yamaoka, 2008). Also, using data from over 49 countries, Helliwell and Putnam (2004) attributed the well-being of many adults to elements of social participation such as religious and community ties. In Ghana, Avogo (2013) found that direct participation in voluntary groups is associated with the likelihood of reporting positive health status in Ghana. Nonetheless, few studies have been conducted on social participation and health and well-being in Ghana. Moreover, the existing ones have rarely examined the dynamics that inform the relationships between health-related well-being and the social environment. Probably, it is this knowledge gap that has rendered some public and social health initiatives less effective as the Ghana Health Service (GHS) suggests (GHS, 2015).
Health literacy and health and well-being
Health literacy has become an essential component of health systems because of its potential to reduce inequalities in health outcomes (Haun et al., 2015). From a public health perspective, health literacy is now a requisite for individuals and groups as health systems continue to make more complex demands on consumers, and expect greater understanding from them (Nielsen-Bohlman, Panzer & Kindig, 2004). A significant body of literature has reported a positive relationship between health literacy and health-related outcomes among different population groups across several contexts (Berkman et al., 2011, Protheroe et al., 2012). For instance, a study among the general population in Japan identified low health literacy as an independent predictor of both poor physical and mental well-being (Tokuda, Doba, Butler & Passche-Orlow, 2009). In Ghana, Amoah et al. (2017) recently found that among young people, low health literacy significantly predict poor health status as has also been observed in Britain (von Wagner, Knight, Steptoe & Wardle, 2007). Health literacy also reduces the probability of indulging in health-damaging behaviours such as poor dieting, smoking and excessive alcohol intake and increases the probability of utilising preventive health services (von Wagner et al., 2007, Fernandez et al., 2016). Some studies thus argue that there is enough reason to stipulate a causal relationship between health literacy and health (Nielsen-Bohlman et al., 2004). Nonetheless, knowledge of the factors that account for health literacy itself remains complicated and limited (Clouston et al., 2017, Nielsen-Bohlman et al., 2004).
Social participation, health literacy and health-related well-being
Kawachi and Berkman (2014) present three group-level properties namely 1) social contagion (i.e., behavioural transfer); 2) informal social control (i.e., the ability of some members to intervene when they witness deviant behaviours by others); and 3) collective efficacy (i.e., mobilisation needed to take collective action that is health promoting), that account for the relationship between social participation and health-related outcomes. However, these remain hypothetical and require empirical studies to deepen understanding of the nuances and mechanisms involved, particularly in least explored contexts.
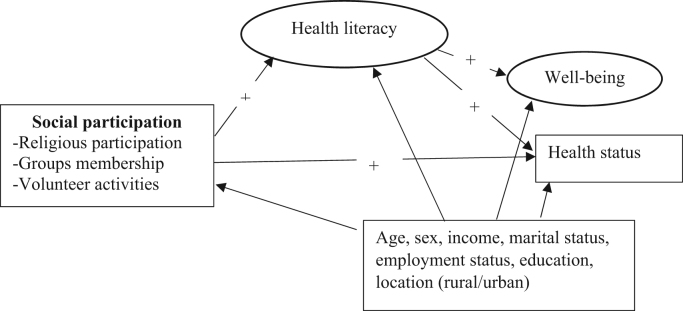
Existing studies show that social participation presents opportunities for even the socioeconomically disadvantaged to obtain health-related information from others (Lee et al., 2008). Research in Ghana indicates that when people have an opportunity to interact with others through avenues such as market centres and religious affiliation, their health-related knowledge improves (Takyi, 2003, Andrzejewski et al., 2009). This is attributed to access to potentially knowledgeable persons who can positively influence health literacy (Takyi, 2003, Andrzejewski et al., 2009). Although aspects of social participation and other sources of social capital, can also have adverse effects on health through misinformation and promotion of health defeating behaviours (Halpern, 2005), the foregoing research largely indicates that the phenomena can help to diffuse proper health information as well. This position has also been highlighted by a study among women in urban Ghana, which suggests that group-based interventions enhance health information-sharing (Lori et al., 2016). The importance of health literacy to health-related well-being is furthered by its role as a mediator between other determinants of health and well-being such as education and ethnicity (Bennett, Chen, Soroui & White, 2009). High levels of health literacy provide a boost to the ways in which support systems embedded in social relationships affect one’s well-being (Lee et al., 2009). This study empirically examines how health literacy mediates the relationship between social participation and health in Ghana and hypothesises that active social participation leads to better health and well-being through health literacy as shown in Fig. 1. Thus, health literacy acts as a mediator in the relationship between social participation and health-related well-being.
Fig. 1.
Proposed model of the relationship between social participation and health and well-being through health literacy. Rectangles represent observed variables whereas oval-shaped figures show unobserved variables.
Methods
Data collection
The study used a cross-sectional design to elicit data from 779 rural and urban adult residents as part of a Social Capital, Health Literacy, Access to Healthcare and Health Researchin Ghana. The broader study examined the role of social relations in access to healthcare and health-related knowledge. The data was gathered from five purposively selected districts in the Ashanti region. The five districts included Asokore-Mampong Municipality, Kumasi Metropolitan Area, Atwima Kwanwoma district, Kwabre East district, and Ejisu-Juaben Municipality. These districts consisted of communities and populations whose characteristics were diverse and analogous to that of the study region. The sample was drawn from eight rural and 36 urban communities/suburbs using a multi-stage cluster sampling approach (Bryman, 2012). The study used the formal criteria (the Ghana Statistical service considers communities with less than 5000 people as rural) (GSS, 2012), to select rural communities. However, the process also considered other characteristics such as access to essential social amenities (e.g. water, education and health facilities) to determine ruralness of a place. In urban areas, economic characteristics, ethnicity and classes of residence as defined by the respective districts were considered in delineating and selecting strata/suburbs to ensure a balanced sample. The data were gathered from June 2015 to October 2015.
The number of questionnaires administered in each locality was proportionate to its adult population size. A systematic sampling technique was used to select actual participants. The process derived a fixed interval for urban (every fifth house) and rural (every second house) locations to select one person from each house for an interview. These ratios were derived according to the number of houses in each urban stratum and rural community with respect to the apportioned questionnaires for each locality. This process helped to ensure a representative sample of the selected rural and urban communities. The house was used as a basis because many households lived in compound houses and shared similar facilities, while in rural areas, many were even related biologically. This strategy helped to prevent systematic similarities in responses. All the interviews were conducted using the dominant local language ‘Twi’. This is because literacy rates were not sufficiently high for self-administered questionnaires (GSS, 2012). The questionnaires were interviewer administered.
Measurements
Exogenous variables
Social participation:
Social participation was measured using individual-level responses. While social participation has sometimes been used to measure specific components of social capital, which is often conceived as an ecological construct, some measures of social participation have also been used to look at individuals’ social networks and support (Hyyppä & Mäki, 2003). This informed the use of individual-level responses to determine the extent of social participation in this study. Three dimensions were used, namely:
-
i.
Associational memberships: The questionnaire asked the number of associations a person actively joined in the past month. The associations consisted of welfare groups (e.g. credit and savings unions), occupational groups (e.g. farmers and traders association), political organisations, study circles, sports groups and hobby clubs. Any association which had a direct connection to one’s religious affiliation was considered separately.
-
ii.
Volunteer activities: The study measured the number of times each person joined his community members or neighbours to address a joint social problem in the past year. The volunteer activities referred mainly to engagement in collective activities rather than a selfless act towards others or community (e.g. communal labour activities such as sanitation; community watchdogs) and;
-
iii.
Religious participation: The study asked whether a person actively participated in religious activities more than once in the past month. Religious activities consisted of joining in religious gathering/meetings as well as other group-based religious events (e.gs. church services, salah and Jumu’ah, traditional worship events and other religious groups such as men/women’s fellowship, singing groups). Religious groups may have ramifications for social life and also health (Obeng, 1996, Takyi, 2003).
The first two dimensions were adapted from the Short version of the Adapted Social Capital Assessment Tool (S-ASCAT) (Harpham et al., 2002, Harpham, 2008). Numerous studies have tested the instrument rigorously across several contexts including those in Africa (Ethiopia) and South America (Peru) and Asia (Vietnam) (De Silva et al., 2006, Takahashi et al., 2011). The third question was taken from a study conducted by Lee et al. (2008) in South Korea.
Mediating variable
Health literacy:
The study used the short version of the European Health Literacy Questionnaire (HLS-EU-Q16) to measure health literacy. This instrument, which was developed by the HLS-EU project consortium (Pelikan, Röthlin, Ganahl & Peer, 2014), measures comprehensive health literacy in general populations. It comprises 16 items, which measure four competencies—obtaining, understanding, appraising and applying health information. These competencies are assessed on three health domains namely healthcare, disease prevention and health promotion (HLS-EU Consortium, 2012, Sørensen et al., 2013). The instrument measures these elements on a four-point Likert scale (1 =very difficult, 2 = difficult, 3 = easy, and 4 = very easy) and a fifth option ‘don’t know’. This instrument and other variants of it have been validated and used in several other contexts including Taiwan, Vietnam, Indonesia, Kazakhstan, Malaysia, Myanmar and Ghana (Duong et al., 2017, Amoah et al., 2017). Nonetheless, the original instrument was slightly adapted to make it relevant contextually. For example, the study replaced words and phrases about ‘mental health’ with more acceptable terms such as ‘ problems of the mind’ and mental health conditions such as stress. Relevant examples were also attached to each of the 16 items to make them more understandable. The instrument was back-translated (from English) to the dominant local language ‘Twi’ and then from Twi to English to assure its validity. Moreover, the instrument, as well as the questionnaire itself, was also pretested among 105 participants.
The responses were dichotomised. The categories ‘fairly easy’ and ‘very easy’ had a value of one (1), whereas ‘fairly difficult’ and ‘very difficult’ responses were given a value of zero (0). The ‘don’t know’ responses were regarded as missing variables. For a case to be included in the final analysis, a minimum of 14 valid responses was required. Subsequently, the scores were summed. This approach helped to group the levels of health literacy into three as recommended by the developers (HLS-EU Consortium, 2012): inadequate health literacy (scores 0–8); problematic health literacy (scores 9–12); and sufficient health literacy (scores 13–16). In the mediation analysis, however, the sum of all responses was used as a continuous variable.
Dependent variables
The study considered two outcome variables namely: self-rated health status and subjective well-being.
Health status:
The study measured self-rated health status using a single item: it required participants to rate their overall health on a 5-point ordinal scale ranging from poor (1) to excellent (5). This approach to measuring health status has been used widely and has proven to be reliable across contexts (Moriarty, Zack & Kobau, 2003).
Subjective well-being:
An adapted version of the Satisfaction with Life and Well-being and Life Scale (SWLS) (Diener, Emmons, Larsen & Griffin, 1985) was used to measure the subjective well-being of participants. This instrument has been used for a variety of purposes including social and health-related research (Helliwell & Putnam, 2004). It has shown adequate content and predictive validity among different population groups (Diener et al., 1985, Pavot et al., 1991).The instrument consists of five items designed to measure each person’s overall satisfaction with life considering other essential dimensions of his or her life. In the version used for this study, the original 7-point Likert scale was reduced to five points (1= strongly disagree to 5 = strongly agree) for ease of administration in the study context. The total score thus ranged from five to 25. Essentially, higher scores represented well-being. Those scoring 0–9, 10–14, 15, 16–20 and 21–25 were classified as very dissatisfied, dissatisfied, indifferent, slightly satisfied and satisfied respectively. The life satisfaction and well-being scale was also treated as a continuous variable.
Sociodemographic characteristics:
The demographic variables measured included age, gender, marital status (married or not married; with those cohabitating counted as married), monthly income (income of the participant), employment status, locality of residence (rural or urban), and educational attainment. These variables are known to shape health and well-being (McCracken and Phillips, 2017, Yamaoka, 2008).
Data analysis
The preliminary analysis was carried out using SPSS version 21 (IBM Corp., 2013). The study used the software to ascertain the characteristics of the participants in relation to the critical variables in the study as well as the correlation between them. Cronbach’s alpha and confirmatory factor analysis (CFA) were used to respectively examine the internal consistency and construct validity of the HLS-EU-Q16 and SWLS instruments. The CFA helped to set up the right model for each of the latent/unobserved variables (health literacy and well-being). In the process, three items (items 7, 8 and 13 on the original scale) of the health literacy instrument were removed due to weak coefficients.
Path analysis (mediation) within structural equation modelling (SEM) were specified to test the hypothesis. Fig. 1 shows the hypothesised path model of the analysis. All the variables were standardised before including them in the model to address possible multicollinearity and to improve the accuracy of the results. Health status was treated as a continuous variable with high scores representing better health. As regards social participation, each of the dimensions measured was treated as observed variables in the SEM (see Byrne, 2013). The analysis employed the maximum likelihood estimation method using 1000 bootstrap samples and a bias-corrected confidence interval of 95% to ensure a stable parameter estimate (Byrne, 2013). Moreover, to meet the requirements of bootstrapping all missing values in the data were replaced by the mean. The overall model fit was evaluated based on the suggested criteria and values for assessing SEM (see Arbuckle, 2012, Byrne, 2013). In the results, the non-significant socio-demographic predictors of social participation and health literacy were removed to improve the degree of freedom and improve fit of the data (see Yeary et al., 2012). All the CFA and SEM analysis were performed using SPSS AMOS version 21 (Arbuckle, 2012).
Ethical approval
The Committee on Human Research Publications and Ethics (CHRPE) of the School of Medical Sciences, Kwame Nkrumah University of Science and Technology and Okomfo Anokye Teaching Hospital, Kumasi, Ghana, (CHRPE/AP/345/15) provided in-country ethical approval. The study thus conforms to the principles set forth by the Council for International Organizations of Medical Sciences (CIOMS) regarding the guidelines for health-related research involving humans (CIOMS, 2016).
Results
Over half of the participants were female, and nearly one-third were between the ages of 25 and 34. The most common educational attainment was Junior High School. Table 1 shows the remainder of the socio-demographic characteristics of the participants.
Table 1.
Descriptive statistics of the variables in the study.
| Characteristics |
Total |
||
|---|---|---|---|
| N (779) | % | ||
| 1 | Sex | ||
| Male | 363 | 46.6 | |
| Female | 416 | 53.4 | |
| 2 | Age | ||
| 18–24 | 190 | 24.4 | |
| 25–34 | 235 | 30.2 | |
| 35–44 | 169 | 21.7 | |
| 45–59 | 117 | 15.0 | |
| 60+ | 68 | 8.7 | |
| 3 | Educational attainment | ||
| Never been to school | 55 | 7.1 | |
| Primary school | 117 | 15.0 | |
| JHS | 304 | 39.0 | |
| SHS | 237 | 30.4 | |
| Tertiary Level | 66 | 8.5 | |
| 4 | Marital status | ||
| Married | 350 | 44.9 | |
| Never married/single | 429 | 55.1 | |
| 5 | Employment status | ||
| Employed | 543 | 69.7 | |
| Unemployed | 236 | 30.3 | |
| 6 | Monthly incomea | ||
| <200 GH¢ | 223 | 46.7 | |
| 200–500 GH¢ | 147 | 30.8 | |
| 500–1000 GH¢ | 66 | 13.8 | |
| 1000+ GH¢ | 42 | 8.8 | |
| 7 | Location of resident | ||
| Rural | 366 | 47 | |
| Urban | 413 | 53 | |
| 8 | Number of groups joined | ||
| 0 | 44 | 5.6 | |
| 1 | 165 | 21.2 | |
| 2+ | 570 | 73.2 | |
| Mean (SD) | 2.8 (1.8) | ||
| 9 | Volunteer activities | ||
| 0 | 430 | 55.2 | |
| 1 | 239 | 30.7 | |
| 2+ | 110 | 14.1 | |
| Mean (SD) | 0.8 (1.2) | ||
| 10 | Religious participation | ||
| Yes | 633 | 81.3 | |
| No | 146 | 18.7 | |
| 11 | Health literacy | ||
| Inadequate health literacy | 187 | 24.0 | |
| Problematic health literacy | 302 | 38.8 | |
| Sufficient health literacy | 290 | 37.2 | |
| Mean (SD) | 10.73 (3.37) | ||
| 12 | Health status | ||
| Poor | 79 | 10.1 | |
| Fair | 135 | 17.3 | |
| Good | 238 | 30.6 | |
| Very good | 231 | 29.7 | |
| Excellent | 96 | 12.3 | |
| 13 | Well-being | ||
| Very dissatisfied | 147 | 18.9 | |
| Dissatisfied | 342 | 43.9 | |
| Indifferent | 64 | 8.2 | |
| Slightly satisfied | 190 | 24.4 | |
| Satisfied | 36 | 4.6 | |
| Mean (SD) | 13.26 (3.99) | ||
N = frequency. Some categories have missing or inapplicable cases.
Some rows are not up to the observed count due to missing values.
1US$ = GH¢ 3.8, as at the time of data collection
The HLS-EU-Q16 instrument demonstrated adequate internal consistency and construct validity. It had a Cronbach’s alpha of 0.85 and a split-half Spearman-Brown coefficient of 0.84. Confirmatory factor analysis of the HLS-EU-Q16 showed a good fit of the data to the hypothetical model, with the following indices: CMIN/DF = 2.39, GFI = 0.93, AGFI = 0.91, NFI = 0.96, RFI = 0.83, IFI = 0.91, TLI = 0.89, CFI = 0.91 and RMSEA = 0.04 (see Byrne, 2013, Arbuckle, 2012). The SWLS also showed good internal consistency with a Cronbach alpha coefficient of 0.80, which indicates an adequate degree of construct validity: CMIN/DF (0.54), GFI (0.99), AGFI (0.99), NFI (0.99), RFI (0.99), TLI (1.00), CFI (1.00), and RMSEA (.00).
Social participation was inconsistent among the population according to the three criteria used. More people were members of a variety of associations. This was substantiated by the fact that over 80% of the participants actively participated in religious activities. However, fewer people participated in community-based volunteer activities as Table 1 shows. Health literacy was low across the population as a whole. Three out of every five persons could be described as having limited health literacy (having either inadequate or problematic levels). In contrast with this low level of health literacy, the majority of participants rated their health as good or very good. Nonetheless, they generally rated their overall life satisfaction and well-being as low.
As expected, a positive association was observed between social participation and health literacy. There was also an association between health literacy and health status and well-being; and a relationship between social participation and health-related well-being (see Table 2). None of the variables correlated 0.5 as shown in Table 2. This reduced the chances of multicollinearity in the path analysis.
Table 2.
Spearman’s Correlation between variables.
| Group member | Religious Inv. | Joining others | Health literacy | Health Status | Well-being | Sex | Age | Location | Marital Status | Education | Income | Employment | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group member | 1 | ||||||||||||
| Joining others | .030 | 1 | |||||||||||
| Religious involvement | .047 | 1 | |||||||||||
| Health literacy | .192** | .078* | .073* | 1 | |||||||||
| Health status | .086* | .041 | .084* | .164** | 1 | ||||||||
| Well-being | .223** | .028 | .058 | .239** | .278** | 1 | |||||||
| Sex | -.083* | .066 | -.050 | -.007 | -.079* | .002 | 1 | ||||||
| Age | -.105* | -.106** | .038 | -.206** | -.119** | -.130** | -.011 | 1 | |||||
| Location | -.257** | .096** | .234** | -.191** | -.058 | -.174** | .075* | .064 | 1 | ||||
| Marital status | .049 | .067 | -.084 | .068 | .040 | .115** | -.073* | -.463** | -.082* | 1 | |||
| Education | .221** | .041 | -.071* | .429** | .072* | .155** | -.113** | -.432** | -.284** | .193** | 1 | ||
| Income | .070 | -.099* | -.084 | .121** | -.015 | .177 ** | -.074 | .103* | -.288** | -.006 | .195** | 1 | |
| Employment | -.106** | .001 | -.039 | -.031 | -.074* | -.079** | .096** | -.109** | .057 | .204** | -.094** | -.206** | 1 |
N = 779,
Correlation is significant at the 0.05 level (2-tailed)
Correlation is significant at the 0.01 level (2-tailed).
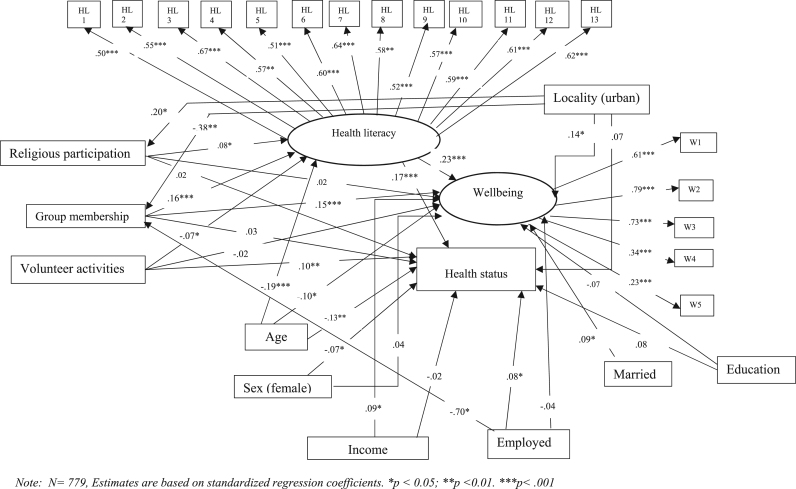
The model used (Fig. 1) to examine whether the effect of social participation on health and well-being through health literacy showed a good theoretical fit. The following indices were observed: CMIN/DF = 2.47, GFI = 0.93, AGFI = 0.91, NFI = 0.85, RFI = 0.82, IFI = 0.91, TLI = 0.89, CFI = 0.91 and RMSEA = 0.04. The results indicated that older persons and females were less likely to have good health statuses while being employed ensured better health status than being unemployed. From Fig. 2, being young, being married, higher income and living in an urban locality promoted well-being. Being married was removed from the model because it showed a very weak association with self-rated health. This helped to increase the degrees of freedom of the model. Interestingly, educational attainment did not predict either well-being or health status.
Fig. 2.
Model of relationship between (social participation), health literacy and health and well-being. Note: N = 779, Estimates are based on standardized regression coefficients. *p < 0.05; **p < 0.01. ***p < .001.
Group membership and volunteer activities directly predicted well-being and health status respectively. Religious participation did not directly predict any of the two dependent variables. Health literacy significantly predicted health status and well-being (Fig. 2; Table 3). Group membership and religious participation positively predicted health literacy (Fig. 2). However, volunteer activities negatively predicted health literacy. Consistent with the hypothesis, social participation (group membership and religious involvement) indirectly predicted health status and well-being through health literacy after controlling for the socio-demographic variables. Volunteer participation also marginally but negatively predicted health status and well-being through health literacy as Table 3 shows.
Table 3.
Effects of social participation on health-related well-being through health literacy.
|
Well-being |
Self-rated status |
|||||||
|---|---|---|---|---|---|---|---|---|
| Unstand. Estim. | Stand. Estim. | Stand. Error | P- value | Unstad.Estim. | Stand. Estim. | Stand. Error | P- value | |
| Direct effect | ||||||||
| Group membership | .117 | .154 | .033 | .002 | .028 | .028 | .038 | .517 |
| Volunteer activities | -.014 | -.019 | .035 | .686 | .098 | .098 | .038 | .009 |
| Religious involvement | .012 | .016 | .031 | .708 | .017 | .017 | .037 | .656 |
| Health literacy | .376 | .230 | .085 | .003 | .374 | .173 | .092 | .002 |
| Indirect effect | ||||||||
| Group membership → HL | .030 | .032 | .009 | .001 | .028 | .024 | .009 | .001 |
| Volunteer activities → HL | -.010 | -.013 | .007 | .078 | -.011 | -.009 | .007 | .070 |
| Religious participation → HL | .014 | .018 | .006 | .036 | .013 | .013 | .007 | .021 |
Note: N = 779. Bold numbers indicate p-vlaue < .05
Discussion
The study sought to analyse the mechanism through which social participation affects health and well-being and whether health literacy plays a role. The results supported the hypothesis that health literacy mediates the relationship between social participation and health status and well-being.
Social participation and health literacy had positive effects on health status and well-being. Active social participation in associational activities may promote access to vital health-related information, which may enhance health-promoting choices. Communities and neighbourhoods with high social cohesion often have inbuilt control mechanisms that promote health and prevent members from indulging in health-damaging behaviours (Halpern, 2005). This result is thus not different from the observations made by earlier research. Social cohesion, through active associational involvement, increases assurance of safety-nets, which are linked to general well-being (Putnam, 2000, Yamaoka, 2008, Kawachi et al., 1999). Erickson (2003) posits that people are healthier and do better in life when they have relationships, even casually, with many people. Such relationships are partly cultivated through interactive social gatherings. Moreover, in many tropical contexts, regular social activities such as community cleaning and sanitation exercises prevent the spread of infectious diseases such as malaria and cholera (WHO, 2009). These may explain the relationship between social participation and elevated levels of somatic health. The positive effect of health literacy on health outcomes is consistent with the findings of several studies across the globe, which assert that well-grounded health-related knowledge and the wherewithal to function appropriately within clinical settings have a positive effect on health and well-being regardless of age, sex and other socio-demographic statuses (Berkman et al., 2011, Protheroe et al., 2012, Amoah et al., 2017).
Being an active member of a group was associated with health and well-being through health literacy. Social groups, even those whose focus is not directly about health, tend to provide opportunities for its members to know and stay alert about health-related issues. This includes free flow of information and other resources needed to make members more astute about health-related matters (Bruhn, 2009). The resources emanating from associational involvement can have a positive effect on health and well-being (Bruhn, 2009, Tokuda et al., 2009, Yeary et al., 2012). Apparently, these may explain why religious participation (a distinct form of group involvement) showed an indirect effect on health and well-being through health literacy in this study. Indeed, religious participation informs the several decisions about health for many Ghanaians (Takyi, 2003, Osafo et al., 2013). Moreover, health literacy reduces inequalities in one of life’s fundamental resources—health (Nielsen-Bohlman et al., 2004). Such capability typifies its role in ensuring life satisfaction and well-being as the findings indicate.
The study observed an adverse indirect effect of health literacy emanating from volunteer activities. This was in contrast to the hypothesis. The finding depicts that social participation does not always have a favourable effect on health literacy. The nature of social interactions and the kind of information, knowledge or other resources transmitted through such engagements may explain the adverse effect. For instance, in this study, volunteer activities had a positive effect on health but not through health literacy. Studies indicate that social capital proxies such as social participation may only positively affect health literacy and consequently health-related outcomes in the face of appropriate resources (Lee et al., 2009, Seeman, 1996). Considering that such voluntary activities may usually be undertaken by neighbours and people in homogenous communities (such as rural residents), it is not farfetched to argue that the resources in such networks may not necessarily be new or of high quality. Even worse, homogeneous groups are known to produce redundant resources (information and knowledge in this respect), which can consequently produce adverse effects (Halpern, 2005). To some extent, this explains why some proxies of social participation did not positively affect health and well-being. Moreover, one could also argue that the indirect negative effect observed between volunteer activities and health through health literacy partly explains why the majority of the participants demonstrated low health literacy. Indeed, it is common for people in the study context to depend on their social relations to acquire critical health-related information informally (Twumasi, 2005, Amoah and Phillips, 2017, Amoah et al., 2017). Therefore, in the event that the individuals and groups in a person’s social circle demonstrate low health literacy, it is likely that little would be passed on to them in terms of health-related knowledge. Furthermore, low health literacy can be explained by the low literacy levels among participants considering that only 38% had attained at least senior high school education. Hence, matters of adequate reading and comprehension of basic health information may be challenging for many. In fact, low literacy is the leading explanatory factor for health literacy (Berkman et al., 2011, Sentell and Braun, 2012).
Moreover, according to the findings, older persons are more likely to have poor health status. This is consistent with general medical research outcomes. Resistance to disease in older people is often compromised due to relatively weaker immune system. Sometimes, this results in multimorbidities including non-communicable diseases. Older persons are also more prone to injuries and slower to recover from them (McCracken and Phillips, 2017, Cau et al., 2016). Apparently, the poor health of older people explains why they were more likely to rate their well-being as poor. The majority of the participants also expressed dissatisfaction with their lives although many rated their health as good. This finding alludes to the underlying economic hardships and employment problems in the study contexts (GSS, 2014). Studies show that well-being is usually associated with sound economic conditions (Kobau, Sniezek, Zack, Lucas & Burns, 2010).
Furthermore, females were more likely to perceive their health as poor than males. This is not different from findings of studies in other contexts in which females emerged as having poor health (Cau et al., 2016, Ardington and Gasealahwe, 2014). Females in especially developing countries are less economically empowered than males. Poor economic standing and even low social status contribute to poor health due to limited access to healthcare and increased stress and worry about their situation (Lim, Ma, Heng, Bhalla & Chew, 2007). This explanation is also pertinent to the observation that being employed is associated with better health status (Glymour et al., 2014, Witter et al., 2017). The poor health among females is also imputable to predominantly low health literacy which affects their knowledge about health problems and how to prevent and treat them—among both young and older females in Ghana (Amoah et al., 2017, Lori et al., 2014). Some attribute the disadvantage of females particularly in developing countries to their exclusion from schooling, owing to extreme patriarchal societal structures that lord the needs of males over females (Vlassoff, 2007, MGCSP, 2015). Importantly, poor opportunities for education as can still be observed in the study context (GSS, 2014), are linked low health literacy and low economic status among women. Adequate education does not only increases the ability to access and use health information appropriately and provide economic opportunities, which are critical for health and well-being (Berkman et al., 2011, Glymour et al., 2014). Nevertheless, it is quite surprising when this finding is situated within other health outcomes such as life expectancy. Females have higher life expectancy in Ghana (WHO, 2015). This contradicts the finding that males have better health status as one would expect females to demonstrate positive health. Moreover, females are often touted as being more conscious about their health compared to men who often forsake health-promoting choices due to hegemonic masculinities (Gough, 2007, Gyasi et al., 2017). Some studies in similar and dissimilar contexts have thus observed differing findings (Leinsalu, 2002, Heistaro et al., 2001). This inconsistency may be due to methodological choices, namely subjective and objective measures of health status.
The results also buttress earlier contentions that economic prosperity does have a positive effect on the general well-being of people regardless of their age, sex, or whether they live in a rural or urban locality (Helliwell & Putnam, 2004). Nevertheless, a person’s well-being is not associated with economic stability alone but also with other social elements such as marital status. Studies indicate that being married offers protection against many life stressors by increasing access to emotional support, which is known to promote health especially in times of affliction (Cau et al., 2016, Putnam, 2000, Helliwell and Putnam, 2004).
The findings have to be interpreted carefully. The study considered only three factors in measuring social participation. Perhaps other robust measures of the concept could have been employed. For instance, the analysis did not capture the role of specific social groups as well as the nature of activities that were undertaken by the respective social units. These details could have provided further and better understanding of the research problem. The results show association and not causation. Notwithstanding, the approach employed and the findings are reasonably consistent with that of several other studies (Putnam, 1993, Putnam, 2000, Harpham, 2008). Finally, the study used a cross-sectional approach. It is likely that some respondents might have either under-rated or overrated their situations depending on the conditions of their lives during the survey. The paper also fails to account for the characteristics (particularly health literacy and health) of the individuals in the social networks of the participants. This limits the extent to which the results can be interpreted. However, the strength of the study lies in the fact that this is one of the few studies that have examined this social epidemiological issue, particularly in relation to health literacy in Ghana and many other countries in the region.
Conclusion
The study has extended the literature on social determinants of health and well-being in Ghana. It has advanced knowledge on the role of social participation in ensuring a healthy population via health literacy. The findings indicated that some aspects of social participation are associated with health and well-being through health literacy. Active associational and civic activities present plausible avenues for transmitting proper health information to the public including even the most disadvantaged in societies. However, the direction of influence—whether negative or positive—has much to do with the nature of participation and quality of the resources that emanate from the interactions. Therefore, there is a need to cautiously incorporate social elements in health promotion strategies especially in contexts where such phenomena play critical roles in everyday lives.
References
- Amoah P.A., Phillips D.R. Strengthening the referral system through social capital: a qualitative inquiry in Ghana. Healthcare. 2017;5:80. doi: 10.3390/healthcare5040080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amoah P.A., Phillips D.R., Gyasi R.M., Koduah A.O., Edusei J. Health literacy and self-perceived health status among street youth in Kumasi, Ghana. Cogent Medicine. 2017;4:1–13. [Google Scholar]
- Andrzejewski C.S., Reed H.E., White M.J. Does where you live influence what you know? Community effects on health knowledge in Ghana. Health Place. 2009;15:228–238. doi: 10.1016/j.healthplace.2008.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbuckle J.L. IBM Corporation; Armonk, NY: 2012. IBM SPSS Amos ( Windows Version 21) Computer Program. [Google Scholar]
- Ardington C., Gasealahwe B. Mortality in South Africa - socioeconomic profile and association with self-reported health. Dev South Afr. 2014;31:127–145. doi: 10.1080/0376835X.2013.853611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avogo W.A. Social capital, civic engagement, and self-rated health in Ghana. African Population Studies. 2013;27:188–202. [Google Scholar]
- Bennett I.M., Chen J., Soroui J.S., White S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. The Annals of Family Medicine. 2009;7:204–211. doi: 10.1370/afm.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman L.F., Krishna A. Social network epidemiology. In: Berkman L.F., Glymour M.M., Kawachi I., editors. Social Epidemiology. Second ed. Oxford University Press; New York: 2014. [Google Scholar]
- Berkman, N.D., Sheridan, S.L., Donahue, K.E., Halpern, D.J., Viera, A., Crotty, K., Holland, A., Brasure, M., Lohr, K., Harden, E., Tant, E., Wallace, I. & Viswanathan, M. (2011). Health Literacy Interventions and Outcomes: An Updated Systematic Review. Evidence Report/Technology Assesment No. 199.: Prepared by RTI International–University of North Carolina Evidence-based Practice Center under contract No. 290-2007-10056-I.
- Bourdieu P. The forms of capital. In: Richardson G., editor. Handbook of Theory and Research for the Sociology of Education. Greenwood Press; New York: 1986. [Google Scholar]
- Bruhn J. Springer; New York: 2009. The Group Effect: Social Cohesion and Health Outcomes. [Google Scholar]
- Bryman A. Oxford University Press; Oxford: 2012. Social Research Methods. [Google Scholar]
- Byrne B.M. Routledge; New York: 2013. Structural Equation Modeling With AMOS: Basic Concepts, Applications, and Programming. [Google Scholar]
- Cau B.M., Falcão J., Arnaldo C. Determinants of poor self-rated health among adults in urban Mozambique. BMC Public Health. 2016;16:856. doi: 10.1186/s12889-016-3552-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CIOMS . Forth ed. Council for International Organizations of Medical Sciences (CIOMS); Geneva: 2016. International Ethical Guidelines for Health-related Research Involving Humans. [Google Scholar]
- Clouston S.A.P., Manganello J.A., Richards M. A life course approach to health literacy: The role of gender, educational attainment and lifetime cognitive capability. Age and Ageing. 2017;46:493–499. doi: 10.1093/ageing/afw229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Silva M.J., Harpham T., Tuan T., Bartolini R., Penny M.E., Huttly S.R. Psychometric and cognitive validation of a social capital measurement tool in Peru and Vietnam. Social Science Medicine. 2006;62:941–953. doi: 10.1016/j.socscimed.2005.06.050. [DOI] [PubMed] [Google Scholar]
- Diener E., Emmons R.A., Larsen R.J., Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Duong T.V., Aringazina A., Baisunova G., Nurjanah, Pham T.V., Pham K.M., Truong T.Q., Nguyen K.T., Oo W.M., Mohamad E., Su T.T., Huang H.-L., Sørensen K., Pelikan J.M., Van den Broucke S., Chang P.W. Measuring health literacy in Asia: validation of the HLS-EU-Q47 survey tool in six Asian countries. Journal of Epidemiology. 2017;27:80–86. doi: 10.1016/j.je.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erickson B. Social networks: the value of variety. Contexts. 2003;2:25–31. [Google Scholar]
- Fernandez D.M., Larson J.L., Zikmund-Fisher B.J. Associations between health literacy and preventive health behaviors among older adults: Findings from the health and retirement study. BMC Public Health. 2016;16:1–8. doi: 10.1186/s12889-016-3267-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GHS (2015). Ghana Health Service 2014 Annual Report Accra: Ghana Health Service.
- Glymour M.M., Avendano M., Kawachi I. Socioeconomic status and health. In: Berkman L.F., Kawachi I., Glymour M.M., editors. Social Epidemiology. Second ed. Oxford University Press; Oxford: 2014. [Google Scholar]
- Gough B. ‘Real men don’t diet’: An analysis of contemporary newspaper representations of men, food and health. Social Science Medicine. 2007;64:326–337. doi: 10.1016/j.socscimed.2006.09.011. [DOI] [PubMed] [Google Scholar]
- GSS . Ghana Statistical Service (GSS); Accra: 2012. 2010 Population and housing census: summary report of final results. [Google Scholar]
- GSS . Ghana Statistical Service; Accra: 2014. Ghana living standards survey round 6 (GLSS 6): Poverty Profile in Ghana (2005–2013) [Google Scholar]
- Gyasi R.M., Buor D., Adu-Gyamfi S., Adjei P.O.-W., Amoah P.A. Sociocultural hegemony, gendered identity, and use of traditional and complementary medicine in Ghana. Women Health. 2017;57:1–18. doi: 10.1080/03630242.2017.1321608. [DOI] [PubMed] [Google Scholar]
- Halpern D. Polity Press; Cambridge, UK: 2005. Social capital. [Google Scholar]
- Harpham T. The measurement of community social capital through surveys. In: Kawachi I., Subramanian S.V., Kim D., editors. Social Capital and Health. Springer; New York: 2008. [Google Scholar]
- Harpham T., Grant E., Thomas E. Measuring social capital within health surveys: Keys issues. Health Policy and Planning. 2002;17:106–111. doi: 10.1093/heapol/17.1.106. [DOI] [PubMed] [Google Scholar]
- Haun J.N., Patel N.R., French D.D., Campbell R.R., Bradham D.D., Lapcevic W.A. Association between health literacy and medical care costs in an integrated healthcare system: A regional population based study. BMC Health Services Research. 2015;15:249. doi: 10.1186/s12913-015-0887-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heistaro S., Laatikainen T., Vartiainen E., Puska P., Uutela A., Pokusajeva S., Uhanov M. Self-reported health in the Republic of Karelia, Russia and in north Karelia, Finland in 1992. Eur J Public Health. 2001;11:74–80. doi: 10.1093/eurpub/11.1.74. [DOI] [PubMed] [Google Scholar]
- Helliwell J.F., Putnam R.D. The social context of well-being. Philosophical Transactions of the Royal Society B: Biological Sciences. 2004;359:1435–1446. doi: 10.1098/rstb.2004.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HLS-EU Consortium (2012). Comparative report on health lieracy in eight EU member states. The European health literacy Survey HLS-EU. The European Health Literacy Project 2009–2012.
- Hyyppä M.T., Mäki J. Social participation and health in a community rich in stock of social capital. Health Education Research. 2003;18:770–779. doi: 10.1093/her/cyf044. [DOI] [PubMed] [Google Scholar]
- IBM Corp (2013). IBM SPSS Statistics for Windows [Online]. Armonk, NY: IBM Corp. [Accessed].
- Kawachi I., Berkman L.F. Social capital, social cohesion, and health. In: Berkman L.F., Kawachi I., Glymour M., M., editors. Social epidemiology. Second ed. Oxford University Press; Oxford: 2014. [Google Scholar]
- Kawachi I., Kennedy B.P., Glass R. Social capital and self-rated health: a contextual analysis. American Journal of Public Health. 1999;89:1187–1193. doi: 10.2105/ajph.89.8.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobau R., Sniezek J., Zack M.M., Lucas R.E., Burns A. Well-being assessment: an evaluation of well-being scales for public health and population estimates of well-being among US adults. Applied Psychology: Health and Well-Being. 2010;2:272–297. [Google Scholar]
- Lee H.Y., Jang S.-N., Lee S., Cho S.-I., Park E.-O. The relationship between social participation and self-rated health by sex and age: A cross-sectional survey. International Journal of Nursing Studies. 2008;45:1042–1054. doi: 10.1016/j.ijnurstu.2007.05.007. [DOI] [PubMed] [Google Scholar]
- Lee S.-Y.D., Arozullah A.M., Cho Y.I., Crittenden K., Vicencio D. Health literacy, social support, and health status among older adults. Educational Gerontology. 2009;35:191–201. [Google Scholar]
- Leinsalu M. Social variation in self-rated health in Estonia: A cross-sectional study. Soc Sci Med. 2002;55:847–861. doi: 10.1016/s0277-9536(01)00221-0. [DOI] [PubMed] [Google Scholar]
- Lim W.-Y., Ma S., Heng D., Bhalla V., Chew S.K. Gender, ethnicity, health behaviour & self-rated health in Singapore. BMC Public Health. 2007;7:184. doi: 10.1186/1471-2458-7-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lori J.R., Dahlem C.H.Y., Ackah J.V., Adanu R.M.K. Examining antenatal health literacy in Ghana. Journal of Nursing Scholarship. 2014;00:1–9. doi: 10.1111/jnu.12094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lori J.R., Munro M.L., Chuey M.R. Use of a facilitated discussion model for antenatal care to improve communication. Int J Nurs Stud. 2016;54:84–94. doi: 10.1016/j.ijnurstu.2015.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken K., Phillips D.R. Routledge; New York: 2017. Global health: an introduction to current and future trends. [Google Scholar]
- MGCSP . Ministry of Gender, Children and Social Protection; Accra, Ghana: 2015. Mainstreaming gender equality and women’s empowerment into Ghana’s development efforts. [Google Scholar]
- Moriarty D.G., Zack M.M., Kobau R. The centers for disease control and prevention’s healthy days measures – Population tracking of perceived physical and mental health over time. Health and Quality of Life Outcomes. 2003;1 doi: 10.1186/1477-7525-1-37. (37-37) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen-Bohlman L., Panzer A.M., Kindig D.A. Institute of Medicine of The National Academies; Washington, D.C.: 2004. Health literacy: A prescription to end confusion. [PubMed] [Google Scholar]
- Nutbeam D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International. 2000;15:259–267. [Google Scholar]
- Obeng P.J. E.J. Brill; New York: 1996. Asante catholicism: religious and cultural reproduction among the Akan of Ghana. [Google Scholar]
- Osafo J., Asampong E., Langmagne S., Ahiedeke C. Perceptions of parents on how religion influences adolescents' sexual behaviours in two Ghanaian Communities: implications for HIV and AIDS prevention. Journal of Religion and Health. 2013;53:959–971. doi: 10.1007/s10943-013-9689-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavot W., Diener E., Colvin C.R., Sandvik E. Further validation of the satisfaction with life scale: evidence for the cross-method convergence of well-being measures. J Pers Assess. 1991;57:149–161. doi: 10.1207/s15327752jpa5701_17. [DOI] [PubMed] [Google Scholar]
- Pelikan, J., Röthlin, F., Ganahl, K. & Peer, S. (2014). Measuring comprehensive health literacy in general populations – the HLS-EU instruments. In Proceedings of the Second International Conference of Health Literacy and Health Promotion Taipei, Taiwan. Ludwig Boltzmann Institute Health Promotion Research, Vienna, Austria.
- Protheroe J., Wolf M., Lee A. Health literacy and health outcomes. In: Begoray D., Gillis D.E., Rowlands G., editors. Health literacy in context. Nova Science Publishers Inc; New York: 2012. [Google Scholar]
- Putland C., Baum F., Ziersch A., Arthurson K., Pomagalska D. Enabling pathways to health equity: Developing a framework for implementing social capital in practice. BMC Public Health. 2013;13:517. doi: 10.1186/1471-2458-13-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam R.D. Princeton University Press; 1993. Making democracy work: Civic tradition in modern Italy. [Google Scholar]
- Putnam R.D. Tuning in, tuning out: the strange disappearance of social capital in America. Political Science and Politics. 1995;28:664–683. [Google Scholar]
- Putnam R.D. Simon and Schuster; New York: 2000. Bowling alone: The collapse and revival of American community. [Google Scholar]
- Seeman T.E. Social ties and health: The benefits of social integration. Annals of Epidemiology. 1996;6:442–451. doi: 10.1016/s1047-2797(96)00095-6. [DOI] [PubMed] [Google Scholar]
- Sentell T., Braun K.L. Low health literacy, limited english proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. Journal of Health Communication. 2012;17:82–99. doi: 10.1080/10810730.2012.712621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sørensen K., Van den Broucke S., Pelikan J.M., Fullam J., Doyle G., Slonska Z., Kondilis B., Stoffels V., Osborne R.H., Brand H. Measuring health literacy in populations: Illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q) BMC Public Health. 2013:13. doi: 10.1186/1471-2458-13-948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi K., Thuy N.T.M., Poudel K.C., Sakisaka K., Jimba M., Yasuoka J. Social capital and life satisfaction: A cross-sectional study on persons with musculoskeletal impairments in Hanoi, Vietnam. BMC Public Health. 2011;11:1–8. doi: 10.1186/1471-2458-11-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takyi B.K. Religion and women’s health in Ghana: Insights into HIV/AIDs preventive and protective behavior. Social Science Medicine. 2003;56:1221–1234. doi: 10.1016/s0277-9536(02)00122-3. [DOI] [PubMed] [Google Scholar]
- Tokuda T., Doba N., Butler J.P., Passche-Orlow M.K. Health literacy and physical and psychological wellbeing in Japanese adults. Patient Education and Counseling. 2009:75. doi: 10.1016/j.pec.2009.03.031. [DOI] [PubMed] [Google Scholar]
- Twumasi P.A. Ghana Publishing Corporation; 2005. Medical systems in Ghana: A study in medical sociology. [Google Scholar]
- Väänänen A., Murray M., Koskinen A., Vahtera J., Kouvonen A., Kivimäki M. Engagement in cultural activities and cause-specific mortality: Prospective cohort study. Preventive Medicine. 2009;49:142–147. doi: 10.1016/j.ypmed.2009.06.026. [DOI] [PubMed] [Google Scholar]
- Vlassoff C. Gender differences in determinants and consequences of health and illness. Journal of Health Population and Nutrition. 2007;25:47–61. [PMC free article] [PubMed] [Google Scholar]
- von Wagner C., Knight K., Steptoe A., Wardle J. Functional health literacy and health‐promoting behaviour in a national sample of British adults. Journal of Epidemiology and Community Health. 2007;61:1086–1090. doi: 10.1136/jech.2006.053967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2009. Global health risks: Mortality and burden of disease attributable to selected major risks. [Google Scholar]
- WHO . World Health Organisation; Geneva: 2015. Ghana: WHO statistical profile. Country statistics and global health estimate by WHO UN partners. [Google Scholar]
- Witter S., Govender V., Ravindran S.T., Yates R. Minding the gaps: Health financing, universal health coverage and gender. Health Policy and Planning. 2017:1–9. doi: 10.1093/heapol/czx063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamaoka K. Social capital and health and well-being in East Asia: A population-based study. Social Science Medicine. 2008;66:885–899. doi: 10.1016/j.socscimed.2007.10.024. [DOI] [PubMed] [Google Scholar]
- Yeary K.H.-c K., Ounpraseuth S., Moore P., Bursac Z., Greene P. Religion, social capital, and health. Review of Religious Research. 2012;54:331–347. [Google Scholar]