Abstract
Objective
To examine correlates of shared decision making during labor and delivery.
Methods
Data were from a cohort of women who gave birth to their first baby in Pennsylvania, 2009–2011 (N = 3,006). We used logistic regression models to examine the association between labor induction and mode of delivery in relation to women’s perceptions of shared decision making, and to investigate race/ethnicity and SES as potential moderators.
Results
Women who were Black and who did not have a college degree or private insurance were less likely to report high shared decision making, as well as women who underwent labor induction, instrumental vaginal or cesarean delivery. Models with interaction terms showed that the reduction in odds of shared decision making associated with cesarean delivery was greater for Black women than for White women.
Conclusions
Women in marginalized social groups were less likely to report shared decision making during birth and Black women who delivered by cesarean had particularly low odds of shared decision making.
Practice implications
Strategies designed to improve the quality of patient-provider communication, information sharing, and shared decision making must be attentive to the needs of vulnerable groups to ensure that such interventions reduce rather than widen disparities.
Keywords: shared decision making, maternity care, disparities, patient-centered care, cesarean delivery
1. Introduction
Nearly 4 million women give birth in the U.S. each year; 32% deliver by cesarean, and at least 22% give birth following an induction of labor [1,2]. There is broad agreement that cesarean delivery is currently overused in the U.S., given that maternal and neonatal morbidity and mortality have not decreased as cesarean delivery has become more common [3]. Furthermore, cesarean delivery is a major abdominal surgery and carries increased risk of complications for the mother and baby, as well as increased risk of placenta problems in future pregnancies compared to vaginal delivery [3,4]. There is less consensus on whether labor induction is overused, but the major concern is that induction of labor when it is not medically necessary may lead to a higher risk of delivering by cesarean [3,5–7]. Despite these concerns about overuse of obstetric procedures, little is known about how procedure utilization in childbirth relates to women’s involvement in decision making during labor.
Shared decision making, a process in which clinicians and patients work together to make choices about screening, treatment, and other aspects of care, is a dimension of patient-centered care and a key aspect of care quality [8]. While studies have found mixed results of the effects of shared decision making on outcomes [9], some U.S. research has linked shared decision making with higher quality care in a variety of contexts, including depression treatment [10], diabetes management [11], and cancer treatment [12]. Shared decision making in maternity care could have benefits such as reducing decisional conflict, increasing satisfaction with the delivery experience, and generating more positive feelings toward the newborn and fewer depressive symptoms [13], and some maternity care providers have called for more attention to shared decision making as part of increasing the provision of patient-centered care. Advocates of patient-centered care have noted that not all patients may wish to participate in decision-making to the same degree. Although no studies that we are aware of have assessed women’s desire for shared decision making in maternity care specifically, the proportion of patients reporting a desire for shared decision-making in general has been increasing over time [14]. Additionally, some research has shown that patients who participate in decision making report better quality of care and higher quality physician communication regardless of their stated preferences for decision making role [15,16].
Research on decision making in the context of maternity care has focused on women with a prior cesarean delivery and “elective” or “maternal request” cesarean delivery, and found that decision aids or formal counseling programs can increase knowledge and reduce decisional conflict [17–21]. One study conducted at two northern California hospitals found no relationship between women’s perceptions of shared decision making during prenatal care and odds of delivering by cesarean [22]. However, despite the fact that women are actively involved in decisions during the clinical management of labor, no previous research that we are aware of has examined predictors of shared decision making during the intrapartum period of labor and childbirth.
The quality of clinician-patient communication and shared decision making vary by the race/ethnicity and socioeconomic status (SES) of the patient. High-quality communication may be a necessary prerequisite for patients to be involved in making decisions about their care, and racial/ethnic minority patients and lower-SES patients tend to experience poorer-quality communication with clinicians [23–25]. White patients are more likely to experience shared decision making compared to racial/ethnic minority patients [26–30]. Lower-SES patients may have lower levels of health literacy, which can be a barrier to engaging in shared decision making [31]. There are several potential reasons for these disparities in the quality of clinician-patient interaction. For example, there may be greater social separation between clinicians and racial/ethnic minority patients, given that only about 4% of U.S. physicians identify as Black or African American [32]. Greater social separation may contribute to a greater imbalance of power in the patient-clinician relationship, which has been identified as a barrier to shared decision making [33]. Implicit bias among clinicians may also be a factor in communication quality and decision-making style [34]. Minority and lower-SES patients are more likely to be seen in low-resource settings where time pressures may be more intense, which is another barrier to shared decision making [33].
To better understand the relationship between procedure use in childbirth, race/ethnicity and SES, and shared decision making, this study aimed to 1) characterize the association between race/ethnicity, SES and shared decision making during childbirth, 2) examine whether shared decision making varies by use of obstetric procedures such as labor induction and cesarean delivery, and 3) assess whether the relationship between obstetric procedure use and shared decision making is different depending on the woman’s race/ethnicity or SES.
2. Methods
2.1 Data and Sample
Data were from the First Baby Study, a cohort of 3,006 women who gave birth to a first, singleton baby in a Pennsylvania hospital between 2009 and 2011. Approval for the First Baby Study was granted by the Penn State College of Medicine Institutional Review Board (IRB) and by the IRBs of participating hospitals. Study participants gave informed consent. Women were interviewed in the third trimester of pregnancy and again one month after the birth, and periodically through 36 months postpartum. The primary purpose of the First Baby Study was to assess the relationship between delivery mode and subsequent childbearing. Interview responses were linked to birth certificate and hospital discharge data. This analysis drew variables from the baseline and 1-month interviews, as well as the hospital discharge and birth certificate data. Details about the data source for each measure are available in Appendix 1. We chose to exclude women who delivered by planned cesarean in order to focus on decision making in the context of labor. The analytic sample consisted of women who gave birth vaginally or by unplanned cesarean, and with no missing values on covariates (N=2,787).
2.2 Measures
Delivery Decision Making Scale
The main dependent variable of interest is shared decision making about delivery care, measured with the Delivery Decision Making Scale (DDMS), a scale developed by the principal investigator of the First Baby Study following qualitative interviews of women shortly after childbirth. The scale contains 6 items (shown in Table 1), with response choices of true or false. Scale items focus on women’s perceptions of involvement and satisfaction with the decision making process, rather than the concrete practices constituting formal definitions of shared decision making. We reversed coding for the one negative item, and assigned one point for each “true” response, yielding a scale ranging from 0–6, where scores indicate higher levels of shared decision making. The scale had a Kuder-Richardson score of .69, which is good for a true-false instrument, particularly one with only 6 items. Each of the 6 items contributed appropriately to the total score. More than half of the respondents (64.0%) obtained the maximum possible total score of 6. Therefore, we dichotomized the total scores, comparing those who scored 6 (totally satisfied with delivery decision making) to those with scores of less than 6.
Table 1.
Delivery Decision Making Scale items.
|
Race/ethnicity and SES
This analysis categorized women as White, Black, Latina, or other, based on their self-reported race and ethnicity. We used two measures of socioeconomic status: education level (less than high school, some college, and Bachelor’s degree or higher) and insurance type. Because three-quarters of women in the cohort were privately insured and very few women (<3%) were uninsured, insurance type was measured as private or non-private.
Obstetric procedures: labor induction, cesarean delivery, and assisted vaginal delivery
Women were asked whether a healthcare provider had done anything to cause their labor to begin, and if so, the reason for the induction and what method(s) were used. We initially coded all women as having induced labor if they said that a provider had done something to try to cause their labor to begin, but we used the additional questions to confirm whether it seemed likely that the woman had had a medical induction. Ultimately, women were categorized as induced if they met all of the following criteria: 1) they said they were induced, 2) they reported arriving at the hospital not in labor, 3) if they did not report a reason for induction that suggested that they were augmented rather than induced, and 4) if they reported at least one medical method of induction (artificial rupture of membranes, Pitocin, cervical medication, oral medication, or Foley catheter/balloon methods).
Women were asked whether they delivered vaginally or by cesarean. Women who delivered vaginally were asked whether forceps or a vacuum extractor were used. We created two delivery mode variables. The first had 3 categories: 1) spontaneous vaginal delivery, 2) assisted vaginal delivery, and 3) cesarean delivery. The second compared cesarean delivery to all vaginal births.
Covariates
Covariates included the following socio-demographic characteristics: age (18–24, 25–30, or 31–36), partnership status (married and living together, not married but living with partner, other), nativity (foreign- or US-born), and rural zip code of residence. We also controlled for maternal health conditions, including pre-pregnancy or gestational diabetes, pre-pregnancy or gestational hypertension, and pre-pregnancy obesity. Finally, we included in our models whether the woman was supported in labor by a doula, the baby’s gestational age at birth (less than 37 weeks, 37–38 weeks, 39–40 weeks, 41+ weeks), and whether actual delivery mode aligned with the woman’s prenatal delivery mode preference.
2.3 Analysis
We used two-way tabulation with chi-square tests to assess significant bivariate associations between women’s characteristics and shared decision making. In multivariate analyses, we used logistic regression models to estimate the relationship between race/ethnicity, SES, obstetric procedures, and shared decision making while controlling for covariates. Finally, to explore whether obstetric procedures were differently related to patient shared decision making depending on race/ethnicity or SES (moderation), we added interaction terms to the models. Where the model fit was improved by the inclusion of an interaction term (indicated by a statistically significant coefficient for the interaction term), we calculated predicted probabilities and sample average marginal effects of obstetric procedure use on shared decision making by race/ethnicity, education and insurance type. The marginal effects for each subject in the data were calculated based on their actual covariate values, and then the results were averaged across all subjects [35]. All multivariate models employed clustered standard errors to account for correlation among women giving birth in the same hospital. All analyses were conducted using Stata 14.
3. Results
3.1 Sample Characteristics
Characteristics of participants are shown in Table 2. Eighty-three percent of women were White. About 17% had a high school education or less, 27% had some college, and over 50% had either Bachelor’s degree or higher. Half of the women were between the ages of 25 and 30, and 71% were married. In this cohort of women giving birth for the first time, nearly 25% delivered by unplanned cesarean. About 64% of the participants obtained the maximum score of 6 on the Delivery Decision Making Scale, indicating a high level of shared decision making.
Table 2.
Characteristics of analytic sample, First Baby Study (N=2,787).
| N | % | |
|---|---|---|
| Race/ethnicity | ||
| White | 2325 | 83.4 |
| Black | 200 | 7.2 |
| Latina | 150 | 5.4 |
| Other, multiple race | 112 | 4.0 |
| Education level | ||
| High school degree or less | 460 | 16.5 |
| Some college | 745 | 26.7 |
| Bachelor's degree or higher | 1582 | 56.8 |
| Insurance type | ||
| Private | 2115 | 75.8 |
| Non-private | 672 | 24.1 |
| Age | ||
| 18–24 | 758 | 27.2 |
| 25–30 | 1365 | 49.0 |
| 31–36 | 664 | 23.8 |
| Partnership status | ||
| Married and living together | 1964 | 70.5 |
| Not married but living with partner | 496 | 17.8 |
| Other | 327 | 11.7 |
| Born outside United States | 171 | 6.1 |
| Rural zipcode of residence | 233 | 8.4 |
| Pre-pregnancy or gestational hypertension | 197 | 7.1 |
| Pre-pregnancy or gestational diabetes | 176 | 6.3 |
| Pre-pregnancy obesity | 549 | 19.7 |
| Labor support from a doula | 185 | 6.6 |
| Gestational age category | ||
| Less than 37 weeks | 111 | 4.0 |
| 37 or 38 weeks | 527 | 18.9 |
| 39–40 weeks | 1708 | 61.3 |
| 41+ weeks | 441 | 15.8 |
| Delivery mode consistent with prenatal preference | 2105 | 75.5 |
| Birth mode | ||
| Spontaneous vaginal | 1842 | 66.1 |
| Assisted vaginal | 257 | 9.2 |
| Cesarean | 688 | 24.7 |
| Labor was induced | 947 | 34.0 |
| High level of shared decision making | 1775 | 63.7 |
3.2 Shared decision making by delivery mode, race/ethnicity and SES
Perceptions of shared decision making varied by race/ethnicity, SES, and obstetric procedure use. A significantly smaller proportion of women in each racial/ethnic minority group reported a high level of shared decision making compared to White women (Table 3). Women with lower levels of education and women without private insurance were also less likely to have a high level of shared decision making, compared to women with more education and those with private insurance. Sixty-nine percent of women with spontaneous vaginal deliveries reported a high level of shared decision making, compared to 61% of women with assisted vaginal deliveries, and 51% of women with cesarean deliveries. Women who had their labor induced were less likely to report a high level of shared decision making compared to women with spontaneous labor (58% vs. 67%).
Table 3.
Unadjusted shared decision making by race/ethnicity, and SES, and obstetric procedure use, First Baby Study (N=2,787).
| High DDMS score | ||
|---|---|---|
|
| ||
| % | p | |
| Race/ethnicity and SES | ||
| Race/ethnicity | <0.001 | |
| White | 66.4 | |
| Black | 42.5 | |
| Latina | 52.0 | |
| Other, multiple race | 60.7 | |
| Education level | <0.001 | |
| High school degree or less | 50.9 | |
| Some college | 60.9 | |
| Bachelor's degree or higher | 68.7 | |
| Insurance type | <0.001 | |
| Private | 67.8 | |
| Public, other or uninsured | 50.9 | |
| Obstetric procedures | ||
| Labor induction | <0.001 | |
| No | 66.7 | |
| Yes | 57.8 | |
| Birth mode | <0.001 | |
| Spontaneous vaginal | 68.7 | |
| Assisted vaginal | 61.1 | |
| Cesarean | 51.3 | |
3.3 Multivariate results estimating odds of high shared decision making
After adjusting for covariates (Table 4), Black women had lower odds of experiencing a high level of shared decision making compared to White women (AOR=0.58, p<0.001), but there was no longer a statistically significant difference in shared decision making between Latina women and White women. The measures of SES were also associated with adjusted odds of high level of shared decision making; women with a Bachelor’s degree had higher odds of experiencing a high level of shared decision making compared to women with a high school degree or less (AOR=1.31, p=0.023), while women with non-private insurance had lower odds (AOR=0.76, p=0.007). Obstetric procedures were associated with lower levels of shared decision making. Women with assisted vaginal delivery (AOR=0.67, p<0.001) and unplanned cesarean delivery (AOR=0.53, p=.008) had lower odds of high level of shared decision making compared to women with spontaneous vaginal delivery. Labor induction was also independently associated with lower odds of high level of shared decision making (AOR=0.77, p=.007).
Table 4.
Adjusted odds of high level of shared decision making by birth mode and other characteristics, First Baby Study (N=2,787).
| OR | p | |
|---|---|---|
| Race/ethnicity | ||
| White | 1.00 | |
| Black | 0.58 | <0.001 |
| Latina | 0.73 | 0.196 |
| Other, multiple race | 0.82 | 0.287 |
| Education level | ||
| High school degree or less | 1.00 | |
| Some college | 1.16 | 0.155 |
| Bachelor's degree or higher | 1.31 | 0.023 |
| Insurance type | ||
| Private | 1.00 | |
| Public, other or uninsured | 0.76 | 0.007 |
| Delivery mode | ||
| Spontaneous vaginal | 1.00 | |
| Assisted vaginal | 0.67 | <0.001 |
| Unplanned cesarean | 0.53 | 0.008 |
| Labor induction | 0.77 | 0.007 |
odels adjust for age, partnership status, nativity, rurality, diabetes, hypertension, obesity, doula support, gestational age, and consistency of delivery mode with prenatal preference
3.4 Models with interaction terms
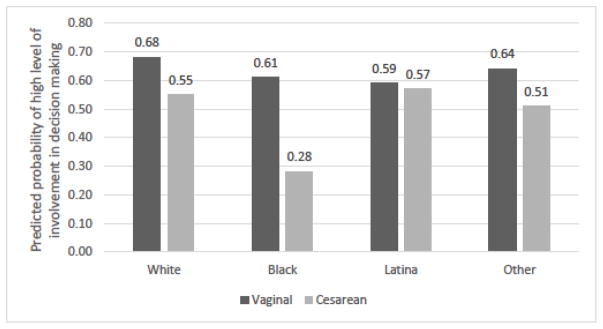
Finally, we investigated whether the association between delivery mode and shared decision making varied by race/ethnicity and SES. To simplify these models, we compared cesarean delivery to vaginal delivery without distinguishing between spontaneous and assisted vaginal delivery. There was a statistically significant interaction between Black race/ethnicity and cesarean delivery (not shown), so we calculated predicted probabilities to investigate this interaction (Figure 1). White women who delivered vaginally had a predicted probability of high level of shared decision making of 0.68, while White women who delivered by cesarean had a predicted probability of high level of shared decision making of 0.55 – a difference of 13 percentage points. For Black women, cesarean delivery was associated with a significantly larger reduction in the predicted probability of high level of shared decision making: Black women who delivered vaginally had a predicted probability of high level of shared decision making of 0.61, and Black women who delivered by cesarean had a predicted probability of high level of shared decision making of 0.28 – a difference of 33 percentage points. These findings indicate that the magnitude of the reduction in the chance of reporting a high level of shared decision making associated with cesarean delivery was much larger for Black women than for White women.
Figure 1.
Predicted probability of high level of shared decision making by delivery mode and race/ethnicity, from models including interaction terms.
4. Discussion and Conclusion
4.1 Discussion
Most first-time mothers in this study felt very involved in the delivery decision-making process, with 64% reporting the highest possible score on the scale assessing decision-making involvement. However, women reporting lower levels of shared decision making were disproportionately likely to be from racial/ethnic minority groups, less educated, and to lack private insurance. These patterns persisted in multivariate models, revealing a disproportionately less engaged decision experience for pregnant patients in more marginalized social groups. Additionally, after controlling for other characteristics, obstetric procedure use continued to be a strong predictor of women’s perceptions of involvement in decision making, with labor induction, assisted vaginal delivery, and cesarean delivery all independently contributing to lower perceived involvement. An earlier study found no association between women’s perceptions of shared decision making in prenatal care and cesarean delivery [22]; the difference in our findings may have to do with the fact that decision making in prenatal care is more distal from the intrapartum experience and the clinical decision to deliver by cesarean. Furthermore, we used a newly-established measure of shared decision making, which is tailored to the childbirth experience and captured women’s satisfaction with the delivery decision making. Standardized measures and routinely collected data on women’s maternity care experiences, including shared decision making, communication quality, and other aspects of patient-centered care, may enhance the ability of stakeholders in the maternity care system to examine quality of care across patient settings and over time.
Despite attention to shared decision making as an important component of patient-centered care, most research and interventions have focused on ambulatory or outpatient care in the clinic, not on the context of acute care in the hospital, such as the intrapartum period. This study found that women with obstetric interventions including induction of labor, assisted vaginal delivery, and unplanned cesarean delivery reported lower levels of shared decision making. Even when these procedures are medically necessary, many situations are not the type of emergency that would preclude taking the time to involve the woman in the decision-making process. However, increasing women’s shared decision making during childbirth (or patient shared decision making in other types of inpatient care) requires some adaptations to existing procedures to achieve higher levels of shared decision making.
For example, decision aids are an effective way of ensuring that patients are provided balanced information prior to making a decision [36], and have been shown to be effective at increasing women’s knowledge and reducing decisional conflict for several scenarios in pregnancy and birth [20,21,37]. However, decision aids may not be practical for the scenario of an unplanned cesarean delivery during labor, where there may be wide variation in the potential reasons for considering a cesarean delivery and the woman is experiencing labor. Communication skills training for clinicians that is specifically targeted toward intrapartum care and that incorporates principles of shared decision making may be useful to enhance the quality of the decision-making process without the use of formal decision aids [38]. Decision aids might be appropriate for making decisions about common reasons for inducing labor (such as pregnancy continuing beyond 41 weeks), and organizations like the California Maternal Quality Care Collaborative and a partnership between Childbirth Connection and the Informed Medical Decisions Foundation have projects underway to develop and pilot decision aids to promote shared decision making in more maternity care situations [39,40].
These results also indicate that eliminating racial/ethnic and SES disparities in the receipt of patient-centered care and in obstetric procedures should be a priority. Women who delivered by cesarean reported being less involved in decisions about their delivery overall, but Black women who delivered by cesarean reported strikingly lower levels of shared decision making compared to White women. This suggests that the decision-making process leading up to cesarean delivery was more likely to be problematic for Black women. These disparities could have to do with systemic factors that differentially affect the choices and outcomes black women face. For example, it could be related to the quality of the hospitals where women of different racial/ethnic groups give birth (i.e. Black women may be more likely to deliver in lower quality hospitals) [41], or due to differential treatment within the same hospital [34]. This could also relate to the cumulative and intergenerational risks of racism that interact with socioeconomic and educational opportunities across the life course [42]. The reproductive and maternal health decrements that black women, in particular, suffer in the US manifest via disparate access to family planning, preventive services, and prenatal care and result in disproportionate rates of maternal morbidity and mortality [43–45]. These patterns have their roots in a long history of exploitation of black women in reproductive and maternal health research and services access [46,47].
Latina women were less likely to report a high level of shared decision making compared to White women, but this difference was no longer significant in multivariate models. Additionally, the association between delivery mode and shared decision making appeared to be weaker among Latina women than among White women, although the difference in association was not statistically significant. There is substantial heterogeneity among individuals who identify as Latina, in ways that can affect childbirth experiences. For example, one study that assessed chances of cesarean among low-risk women by detailed maternal ethnicity found that women of certain Latina ethnic groups had similar odds of cesarean compared to White women, while women in other Latina ethnic groups had elevated odds of cesarean compared to White women [48]. Prior studies explicitly documenting racial/ethnic differences in shared decision making have demonstrated statistically meaningful Black-White differences [26–28], and have also shown differences between racial/ethnic minority groups (combined), in comparison to Whites [29] Future studies should examine delivery decision-making among Latina women, including relevant subgroups of Latinas.”
In this study population, Black and Latina women had elevated odds of cesarean delivery compared to White women, even after accounting for medical risk factors such as diabetes, hypertension, obesity, and gestational age at birth[49] , consistent with prior studies [50,51]. Greater use of obstetric procedures among Black and Latina women, compared with Whites may be another piece of the broader picture of disparities in delivery decision-making.
While this study produced novel and important findings, there are also limitations to consider. First, this study used a new scale developed specifically to assess women’s experiences with decision making during delivery. A 6-item scale with true/false response choices may not be optimal, and we found that the scale was highly skewed, with the majority of women in this study scoring at the top of the scale. Several studies have compared patient reports of shared decision making and observer report, and found that there are substantial differences in the prevalence of shared decision making depending on which measure is used [52–54]. However, disagreement was almost universally in the direction of the patient reporting more involvement in the decision-making process compared to the observer rating. Assuming that women’s reports in the First Baby Study were likewise inflated, this would attenuate the associations with shared decision making, suggesting that the associations identified in this study may be underestimates. Future research should work to develop a valid and reliable instrument to measure shared decision making that is relevant for women’s childbirth experiences specifically. Second, the First Baby Study cohort over-represents women from more socially privileged groups compared to the population of first-time mothers in Pennsylvania [55], and thus it is possible that the results are not generalizable to all childbearing women. Finally, women who delivered by cesarean may have reported less satisfaction with decision making simply because they had hoped for a vaginal delivery. However, our models controlled for the alignment between women’s prenatal delivery mode preferences and actual delivery mode, addressing this concern.
4.2 Conclusions
This analysis found that women in marginalized social groups were less likely to experience shared decision making during birth, as were women who underwent labor induction or cesarean delivery. Black women delivered by cesarean had particularly low odds of experiencing shared decision making.
4.3 Practice Implications
Efforts are needed to improve the decision-making process for women in labor, including in cases where obstetric interventions are medically necessary, and to increase equity in maternity care. Some states have considered or enacted legislation that encourages or requires the use of shared decision making (e.g. through the use of a certified decision aid) as part of informed consent for certain medical decisions [56]; if adapted to the maternity care context, such requirements could help to ensure that shared decision making is more uniformly adopted across healthcare settings. Additionally, strategies designed to improve the quality of patient-provider communication, information sharing, and shared decision making must be attentive to the needs of vulnerable groups to ensure that such interventions reduce rather than widen disparities [57].
Highlights.
Few studies have examined shared decision making in the childbirth context
Obstetric procedure use was associated with less shared decision making
Shared decision making was less common among lower-SES women and women of color
Black women who delivered by cesarean had strikingly low shared decision making
Acknowledgments
Funding
The First Baby Study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH (R01 HD052990). Dr. Attanasio’s effort on this study was supported by a dissertation grant from the Agency for Healthcare Research and Quality (R36HS024215-01).
Appendix 1. Data source for measures used in analysis
| Measure | Data source |
|---|---|
| Delivery decision making scale | 1-month postpartum interview |
| Race/ethnicity | Baseline interview |
| Education | Baseline interview |
| Insurance type | Hospital discharge record |
| Labor induction | 1-month postpartum interview |
| Cesarean delivery | 1-month postpartum interview |
| Age | Baseline interview |
| Partnership status | Baseline interview |
| Nativity | Baseline interview |
| Rural zip code | Baseline interview |
| Diabetes | Baseline interview |
| Hypertension | Baseline interview |
| Obesity | Baseline interview |
| Labor support from a doula | 1-month postpartum interview |
| Baby's gestational age at birth | Birth certificate |
| Delivery mode alignment with prenatal preferences | Baseline interview and 1-month postpartum interview |
Footnotes
Contribution to authorship
All authors were involved in the design of the study; LBA conducted the data analysis and drafted the manuscript. All authors reviewed the manuscript for intellectual content and approved the final submitted version
Disclosure of interests
The authors have no competing interests to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hamilton BE, Martin JA, Osterman J, Curtin SC, Mathews T, Martin JA, Osterman MJ, Curtin SC, Mathews T. Births: Final Data for 2014. Natl Vital Stat Reports. 2015;64:1–104. [PubMed] [Google Scholar]
- 2.Osterman MJK, Martin JA. Recent Declines in Induction of Labor by Gestational Age. NCHS Data Br No. 2014;155:1–8. [PubMed] [Google Scholar]
- 3.American College of Obstetricians and Gynecologists. Safe prevention of the primary cesarean delivery. Obstetric Care Consensus No. 1. Obstet Gynecol. 2014;123:693–711. doi: 10.1097/01.AOG.0000444441.04111.1d. [DOI] [PubMed] [Google Scholar]
- 4.Healthy People 2020 Topics and Objectives: Maternal, Infant and child Health. 2010 http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=26.
- 5.Ehrenthal DB, Jiang X, Strobino DM. Labor induction and the risk of a cesarean delivery among nulliparous women at term. Obstet Gynecol. 2010;116:35–42. doi: 10.1097/AOG.0b013e3181e10c5c. [DOI] [PubMed] [Google Scholar]
- 6.Miller NR, Cypher RL, Foglia LM, Pates JA, Nielsen PE. Elective Induction of Labor Compared With Expectant Management of Nulliparous Women at 39 Weeks of Gestation: A Randomized Controlled Trial. Obstet Gynecol. 2015;126:1258–64. doi: 10.1097/AOG.0000000000001154. [DOI] [PubMed] [Google Scholar]
- 7.Kjerulff KH, Attanasio LB, Edmonds JK, Kozhimannil KB, Repke JT. Labor induction and cesarean delivery: A prospective cohort study of first births in Pennsylvania, USA. Birth. 2017;44:252–261. doi: 10.1111/birt.12286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Committee on Quality of Health Care in America. Crossing the Quality Chasm:A New Health System for the 21st Century. 2001. [Google Scholar]
- 9.Clayman ML, Bylund CL, Chewning B, Makoul G. The Impact of Patient Participation in Health Decisions Within Medical Encounters: A Systematic Review. Med Decis Mak. 2015 doi: 10.1177/0272989X15613530. 0272989X15613530. [DOI] [PubMed] [Google Scholar]
- 10.Clever SL, Ford DE, Rubenstein LV, Rost KM, Meredith LS, Sherbourne CD, Wang N-Y, Arbelaez JJ, Cooper LA. Primary Care Patients’ Involvement in Decision-Making Is Associated With Improvement in Depression. Med Care. 2006;44:398–405. doi: 10.1097/01.mlr.0000208117.15531.da. [DOI] [PubMed] [Google Scholar]
- 11.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17:243–252. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andersen MR, Urban N. Involvement in decision-making and breast cancer survivor quality of life. Heal Psychol. 2009;28:29–37. doi: 10.1037/0278-6133.28.1.29. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg H. Informed decision making in maternity care. J Perinat Educ. 2009;18:32–40. doi: 10.1624/105812409X396219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Légaré F, Thompson-Leduc P. Twelve myths about shared decision making. Patient Educ Couns. 2014;96:281–286. doi: 10.1016/j.pec.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 15.Kehl KL, Landrum MB, Arora NK, Ganz Pa, van Ryn M, Mack JW, Keating NL. Association of Actual and Preferred Decision Roles With Patient-Reported Quality of Care. JAMA Oncol. 2015;1:50–58. doi: 10.1001/jamaoncol.2014.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martinez KA, Resnicow K, Williams GC, Silva M, Abrahamse P, Shumway DA, Wallner LP, Katz SJ, Hawley ST. Does physician communication style impact patient report of decision quality for breast cancer treatment? Patient Educ Couns. 2016;99:1947–1954. doi: 10.1016/j.pec.2016.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Montgomery AA, Emmett CL. Two decision aids for mode of delivery among women with previous caesarean section : randomised controlled trial. Br Med J. 2007;334:1305–1309. doi: 10.1136/bmj.39217.67101955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shorten A, Shorten B, Keogh J, West S, Morris J. Making choices for childbirth: a randomized controlled trial of a decision-aid for informed birth after cesarean. Birth. 2005;32:252–61. doi: 10.1111/j.0730-7659.2005.00383.x. [DOI] [PubMed] [Google Scholar]
- 19.Cleary-Goldman J, Cornelisse K, Simpson LL, Robinson JN. Previous Cesarean Delivery: Understanding and Satisfaction with Mode of Delivery in a Subsequent Pregnancy in Patients Participating in a Formal Vaginal Birth After Cesarean Counseling Program. Am J Perinatol. 2005;22:217–221. doi: 10.1055/s-2005-866606. [DOI] [PubMed] [Google Scholar]
- 20.Dugas M, Shorten A, Dubé E, Wassef M, Bujold E, Chaillet N. Decision aid tools to support women’s decision making in pregnancy and birth: a systematic review and meta-analysis. Soc Sci Med. 2012;74:1968–78. doi: 10.1016/j.socscimed.2012.01.041. [DOI] [PubMed] [Google Scholar]
- 21.Say R, Robson S, Thomson R. Helping pregnant women make better decisions: a systematic review of the benefits of patient decision aids in obstetrics. BMJ Open. 2011;1:e000261. doi: 10.1136/bmjopen-2011-000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hessol NA, Odouli R, Escobar GJ, Stewart AL, Fuentes-Afflick E. Interpersonal Processes of Care and Cesarean Delivery in Two Health Care Settings. Am J Public Health. 2012;102:1722–1728. doi: 10.2105/AJPH.2011.300549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bertakis KD, Azari R. Determinants and outcomes of patient-centered care. Patient Educ Couns. 2011;85:46–52. doi: 10.1016/j.pec.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 24.Willems S, De Maesschalck S, Deveugele M, Derese a, De Maeseneer J. Socioeconomic status of the patient and doctor-patient communication: does it make a difference? Patient Educ Couns. 2005;56:139–46. doi: 10.1016/j.pec.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 25.Street RL, Gordon H, Haidet P. Physicians’ communication and perceptions of patients: is it how they look, how they talk, or is it just the doctor? Soc Sci Med. 2007;65:586–98. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cooper-Patrick L, Gallo JJ, Gonzales JJ, Powe NR, Nelson C, Ford DE. Race, Gender and Partnership in the Patient-Physician Relationship. JAMA. 1999;282:583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 27.Peek ME, Odoms-Young A, Quinn MT, Gorawara-Bhat R, Wilson SC, Chin MH. Race and shared decision-making: Perspectives of African-Americans with diabetes. Soc Sci Med. 2010;71:1–9. doi: 10.1016/j.socscimed.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levinson W, Hudak PL, Feldman JJ, Frankel RM, Kuby A, Bereknyei S, Braddock CH., III It’s not what you say...: Racial disparities in communication between orthopedic surgeons and patients. Med Care. 2008;46:410–416. doi: 10.1016/j.surg.2006.10.010.Use. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ratanawongsa N, Zikmund-Fisher BJ, Couper MP, Van Hoewyk J, Powe NR. Race, ethnicity, and shared decision making for hyperlipidemia and hypertension treatment: the DECISIONS survey. Med Decis Making. 2010;30:65S–76S. doi: 10.1177/0272989X10378699. [DOI] [PubMed] [Google Scholar]
- 30.Lin MY, Kressin NR. Race/ethnicity and Americans’ experiences with treatment decision making. Patient Educ Couns. 2015;98:1636–1642. doi: 10.1016/j.pec.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 31.McCaffery KJ, Smith SK, Wolf M. The challenge of shared decision making among patients with lower literacy: a framework for research and development. Med Decis Mak. 2010;30:35–44. doi: 10.1177/0272989X09342279. [DOI] [PubMed] [Google Scholar]
- 32.Nivet MA, Castillo-Page L. Diversity in the Physician Workforce: Facts & Figures 2014. 2014 http://aamcdiversityfactsandfigures.org/
- 33.Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns. 2014;94:291–309. doi: 10.1016/j.pec.2013.10.031. [DOI] [PubMed] [Google Scholar]
- 34.van Ryn M, Burgess DJ, Dovidio JF, Phelan SM, Saha S, Malat J, Griffin JM, Fu SS, Perry S. The Impact of Racism on Clinician Cognition, Behavior, and Clinical Decision Making. Du Bois Rev Soc Sci Res Race. 2011;8:199–218. doi: 10.1017/S1742058X11000191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karaca-Mandic P, Norton EC, Dowd B. Interaction terms in nonlinear models. Health Serv Res. 2012;47:255–74. doi: 10.1111/j.1475-6773.2011.01314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stacey D, Légaré F, Col N, Bennett C, Barry M, Eden K, Homes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Thomson R, Trevena L, Wu J. Decision aids for people facing health treatment or screening decisions (Review) Cochrane Database Syst Rev. 2014 doi: 10.1002/14651858.CD001431.pub4. [DOI] [PubMed] [Google Scholar]
- 37.Vlemmix F, Warendorf JK, Rosman AN, Kok M, Mol BWJ, Morris JM, Nassar N. Decision aids to improve informed decision-making in pregnancy care: A systematic review. BJOG An Int J Obstet Gynaecol. 2013;120:257–266. doi: 10.1111/1471-0528.12060. [DOI] [PubMed] [Google Scholar]
- 38.Coxeter P, Del Mar CB, McGregor L, Beller EM, Hoffmann TC. Interventions to facilitate shared decision making to address antibiotic use for acute respiratory infections in primary care. Cochrane Database Syst Rev. 2015:CD010907. doi: 10.1002/14651858.CD010907.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Main E, Castles A, Peterson N, Werkmeister K. Statewide Initiative to Support Vaginal Birth & Reduce Primary Cesareans. 2016 https://www.cmqcc.org/sites/default/files/_/uploads/CMQCC CS Initiative.pdf.
- 40.Romano A. The First National Maternity Care Shared Decision Making Initiative. 2013:1–7. http://informedmedicaldecisions.org/wp-content/uploads/2012/05/First_Natl_Maternity_SDM.pdf.
- 41.Howell EA, Egorova NN, Balbierz A, Zeitlin J, Hebert PL. Site of delivery contribution to black-white severe maternal morbidity disparity. Am J Obstet Gynecol. 2016;215:143–152. doi: 10.1016/j.ajog.2016.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lu MC, Kotelchuck M, Hogan V, Jones L, Wright K, Halfon N. Closing the Black-White gap in birth outcomes: A life-course approach. Ethn Dis. 2010;20:1–26. doi: 10.1300/J010v20n01_05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Committee on Health Care for Underserved Women. Racial and Ethnic Disparities in Obstetrics and Gynecology. Committee Opinion No 649. Obstet Gynecol. 2015;126:e130–e134. doi: 10.1097/AOG.0000000000001213. http://www.acog.org/-/media/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/co649.pdf?dmc=1&ts=20170409T1604052814. [DOI] [PubMed] [Google Scholar]
- 44.Howell EA, Egorova N, Balbierz A, Zeitlin J, Hebert PL. Black-white differences in severe maternal morbidity and site of care. Am J Obstet Gynecol. 2016;214:122.e1–7. doi: 10.1016/j.ajog.2015.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Callaghan WM, Creanga AA, Kuklina EV. Severe Maternal Morbidity Among Delivery and Postpartum Hospitalizations in the United States. Obstet Gynecol. 2012;120:1. doi: 10.1097/AOG.0b013e31826d60c5. [DOI] [PubMed] [Google Scholar]
- 46.Roberts D. Vintage. New York: 1997. Killing the Black Body: Race, Reproduction, and the Meaning of Liberty. [Google Scholar]
- 47.Eichelberger KY, Doll K, Ekpo GE, Zerden ML. Black lives matter: Claiming a space for evidence-based outrage in obstetrics and gynecology. Am J Public Health. 2016;106:1771–1772. doi: 10.2105/AJPH.2016.303313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Edmonds JK, Hawkins SS, Cohen BB. The Influence of Detailed Maternal Ethnicity on Cesarean Delivery: Findings from the U.S. Birth Certificate in the State of Massachusetts. Birth. 2014;41:290–298. doi: 10.1111/birt.12108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Attanasio LB, Hardeman RR, Kozhimannil KB, Kjerulff KH. Prenatal attitudes toward vaginal delivery and actual delivery mode: Variation by race/ethnicity and socioeconomic status. Birth. 2017:1–9. doi: 10.1111/birt.12305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Janevic T, Loftfield E, Savitz Da, Bradley E, Illuzzi J, Lipkind H. Disparities in cesarean delivery by ethnicity and nativity in new york city. Matern Child Health J. 2014;18:250–7. doi: 10.1007/s10995-013-1261-6. [DOI] [PubMed] [Google Scholar]
- 51.Getahun D, Strickland D, Lawrence JM, Fassett MJ, Koebnick C, Jacobsen SJ. Racial and ethnic disparities in the trends in primary cesarean delivery based on indications. Am J Obstet Gynecol. 2009;201:422.e1–7. doi: 10.1016/j.ajog.2009.07.062. [DOI] [PubMed] [Google Scholar]
- 52.Pass M, Belkora J, Moore D, Volz S, Sepucha K. Patient and observer ratings of physician shared decision making behaviors in breast cancer consultations. Patient Educ Couns. 2012;88:93–99. doi: 10.1016/j.pec.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 53.Kasper J, Heesen C, Kopke S, Fulcher G, Geiger F. Patients’ and observers’ perceptions of involvement differ. Validation study on inter-relating measures for shared decision making. PLoS One. 2011;6 doi: 10.1371/journal.pone.0026255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Saba GW, Wong ST, Schillinger D, Fernandez A, Somkin CP, Wilson CC, Grumbach K. Shared decision making and the experience of partnership in primary care. Ann Fam Med. 2006;4:54–62. doi: 10.1370/afm.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kjerulff KH, Velott DL, Zhu J, Chuang CH, Hillemeier MM, Paul IM, Repke JT. Mode of first delivery and women’s intentions for subsequent childbearing: findings from the First Baby Study. Paediatr Perinat Epidemiol. 2013;27:62–71. doi: 10.1111/ppe.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shafir A, Rosenthal J. Shared Decision Making : Advancing Patient-Centered Care through State and Federal Implementation. Washington, D.C: 2012. [Google Scholar]
- 57.Durand MA, Carpenter L, Dolan H, Bravo P, Mann M, Bunn F, Elwyn G. Do interventions designed to support shared decision-making reduce health inequalities? A systematic review and meta-analysis. PLoS One. 2014;9:e94670. doi: 10.1371/journal.pone.0094670. [DOI] [PMC free article] [PubMed] [Google Scholar]