Abstract
Despite unprecedented spending, US maternal outcomes have worsened drastically over the past decade. In comparison, maternal outcomes of many Low and Middle-Income Countries (LMIC) have improved. Lessons learnt by their success may be applicable to the US. We performed a literature review to identify innovations that had met with success across LMIC, and should be considered for adoption in the US. mHealth and patient facing alerts, Telehealth, patient controlled health records, inclusion of patient relationship data in health information systems and positioning empowered community health workers as catalysts of maternal care delivery were identified as innovations worthy of further evaluation. These innovations were categorized into several themes; knowledge, technology, patient/community empowerment, coordination and process change. Tools that place informed and empowered patients and community members at the center of maternal care has greatly improved maternal outcomes, and are suitable to be considered for the US healthcare system.
Keywords: Global health, Maternal health, Clinical Information Systems, Mobile health, Telemedicine
Introduction
US maternal care is currently in jeopardy. At $111 billion a year, US spending on maternal health is twice that of most other high-income countries [1]. US hospital deliveries may cost up to 8,802 USD per birth, compared to an average 2,050 USD in other OECD countries [2]. Despite this spending, a joint report by the World Health Organization (WHO), United Nations Children’s Emergency Fund (UNICEF), United Nations Population Fund (UNFPA), the World Bank and the United Nations Population Division states that US Maternal Mortality Rates (MMR) have surged by 136% between the years 1990-2013, from 12 per 100,000 live births in 1990 to 28 per 100,000 live births in 2013. [3]. At over 52,000 cases per year, the risk of severe maternal morbidity (SMM) leading to life-long health problems is even greater [4]. American women are more likely to die during childbirth or related complications than women of any other high-income country [5] or middle-income countries such as Bosnia or Macedonia [6]. The main causes of maternal deaths in the US are non-cardiovascular diseases (15.3%), cardiovascular diseases (14.7%), infection or sepsis (12.7%), hemorrhage (11.3%), cardiomyopathy (10.8%), thrombotic pulmonary embolism (9.0%), and hypertensive disorders (7.6%). The main causes of SMM are maternal age, pre-pregnancy obesity, pre-existing chronic medical conditions, and cesarean delivery [7]. There is also significant discrepancy in outcomes across different populations [8] The MMR among African Americans (40.4 per 100,000 live births) is over three times greater than white parents (12.1 per 100,000 live births). MMR among woman of other races are 16.4 per 100,000 live births [9]. MMR rates of US states with high poverty rates were 77% higher than wealthier states [10].
Research indicates that with the exception of malaria and HIV, the main causes of maternal mortality in low and middle income countries (LMIC) are generally similar to those in the US [11, 12]. However, many of these countries have been able to significantly improve their maternal health outcomes. LMIC such as Timor Leste, Bangladesh, Ethiopia, Uruguay, and India have reported between 78% to 65% reductions in maternal mortality during the same 1990–2013 time period that saw US maternal death rates jump by 136%. [3]. Fortunately, evidence suggests that a majority of US based maternal mortality and morbidities are preventable, and can be addressed via early detection and care [13]. This aligns with the three delay model which recognizes three significant barriers women face in achieving timely and effective medical care; the delay in (a) decision to seek care, (b) reaching care, and (c) receiving adequate healthcare [14]. Informatics based solutions can address the three delays, thereby improving maternal health outcomes. Additionally, changes in healthcare delivery across LMIC during this period have included significant investments in healthcare infrastructure and informatics expertise to help mitigate these barriers. Considerable emphasis has been placed on the use of point of care technology, including mobile phones to deliver actionable information to providers, community health workers, caregivers, and patients, allowing them to address the three delays that cause maternal mortality [15]. This indicates that such solutions may have contributed toward improving maternal outcomes. Thus, lessons learnt from LMIC may illustrate approaches to improve maternal outcomes in the US. However, not all innovations may be successful due to significant socio-economic and policy differences between the US and LMIC.
We evaluate maternal care based health informatics interventions adopted by LMIC, and determine which of these could help address maternal care challenges faced by the US. We do not seek to perform comprehensive evaluations of care models or correlating process changes brought about by informatics applications, but to recommend which approaches are most suitable to for consideration to address maternal healthcare needs in the US.
Materials and Methods
An introduction to reverse innovation
Traditionally, technological innovation originated, and was consumed by high-income countries. Such innovations were often considered too expensive or unsuited for LMIC needs. Often, product owners avoided expanding to LMIC as they perceived that marketing their solutions across underserved settings would be unfeasible due to high resource requirements. In many cases, innovations from high-income countries were ‘whittled down’, and produced with limited feature sets for use in low income countries [16]. This environment encouraged innovators from LMIC to develop frugal solutions that were suited for their own needs. However, thanks to qualities of frugality, low operating costs and robustness, innovations meant for LMIC can also be appropriate for adoption elsewhere, particularly in underserved populations in high-income countries. Reverse innovation is the identification of innovations that have already met success in LMIC and adopting these innovations for use in high-income countries [17].
Since its conception, reverse innovation has won widespread acceptance, and adopted by brands such as Microsoft, Nokia, Tata Motors, and Nestle. Products and services created through reverse innovations focus on reducing operating costs and bringing equity with minimal effort, both of which are significantly important for the US health care system. Reverse innovation has the potential to inform a wide host of healthcare challenges [18]. However, the applicability of adopting innovations from LMIC for use in the US healthcare system is relatively unknown, and further work, including implementation science research is necessary to advance the understanding and potential of diffusion of reverse innovations.
Study approach
We searched scientific literature to assess the maternal outcomes challenge in the US. However, searches across OVID medline and Web of Science produced a preponderance of evidence reaching thousands of publications and reports of various quality. To identify the most relevant and accurate literature, we focused on a subset of academic, research and development organizations engaged in improving or monitoring maternal outcomes in the US as sources of information. We searched the websites of these organizations to identify formal reports/publications that discussed major causes of mortality and morbidity. The results of this search were refined using content and discourse analysis methods to identify challenges that are most significant to the US. Next, we performed a literature review to identify how LMIC addressed each of these challenges, and what health informatics innovations could be leveraged to do so. By mapping the aforesaid challenges to successful health informatics innovations, we identified those suitable for further evaluation in the US. We elected to perform a literature review rather than a systematic review as a systematic review would be focused on a single research question, while a literature review would allow us to bring together a broad body of information on a given topic to draw our own conclusions [19].
Results
Based on the analysis of well-reputed information sources (Appendix A), we identified five major challenges affecting US maternal health outcomes;
Lack of trained staff: Rural Americans and underserved populations such as American Indians and Alaska natives (AI/AN) suffer from significant shortages of healthcare providers due to (a) existing staff shortages and (b) tendency of physicians to relocate and practice at affluent urban or suburban areas [20, 21].
Limited access to care: Lack of access to care is a significant challenge to African Americans, Latinos and other minority groups [22], at risk populations, immigrants and low-income earners [23]..
Limited sense of ownership/empowerment: Placing an informed patient at the center of their own care can address delays in seeking care, and empower the patient to be an active participants in their own healthcare.
Isolation/lack of community support: Lack of community support and feelings of isolation can lead to depression, stress and inability to manage other life threatening behaviors/conditions [24, 25].
Gaps in patient awareness/education: Lack of awareness leads to risky behavior, inability to manage harmful conditions such as pregnancy related complications [26], and contributes to delays in seeking care.
We performed a rigorous literature review across Ovid Medline, Web of science and EMBASE to evaluate health informatics innovations adopted by LMIC to address these challenges (Appendix B). Search results were refined using the literature inclusion/exclusion strategy presented below (figure 1).
Figure 1.
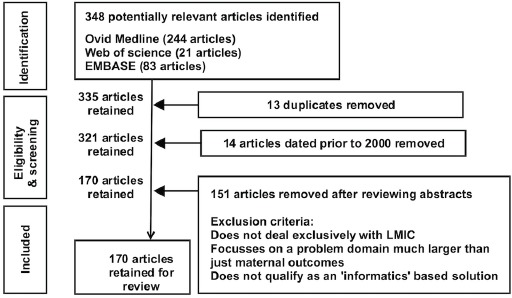
Literature inclusion/exclusion strategy
The literature review indicated that efforts to improve maternal care delivery for LMIC had led to the development of numerous tools and approaches. Many informatics based innovations focused on delivery of actionable information to reduce the three delays. We also considered innovations that had failed due to technology, financial or policy based limitations. In the case of such failures, we assessed why they had failed, and determined if these innovations would survive, and help improve maternal outcomes in the US. These lessons were condensed into technological and system change innovations that could address one or more of the five aforementioned challenges, and were suitable for further evaluation by US based settings; (a) mHealth and Patient Facing Alerts, (b) Telehealth / Telemedicine (c) Patient controlled health records (d) Relationships within Health Information systems (e) empowered Community health workers (CHW) as catalysts of healthcare delivery (table 1).
Table 1.
US maternal outcome challenges and LMIC based innovations solutions that could address them
| Solutions | ||||||
|---|---|---|---|---|---|---|
| mHealth/Patient Facing Alerts | Telehealth/Telemedicine | Patient controlled health records | Relationships within Health Information systems | CHW as catalysts of healthcare delivery | ||
| Challenges | Lack of trained staff | X | X | X | ||
| Limited sense of ownership/ | X | X | X | |||
| Isolation/lack of community support | X | X | ||||
| Gaps in patient awareness/education | X | X | ||||
mHealth and Patient Facing Alerts
The role of actionable information in improving health outcomes is well documented [27, 28]. The rapid penetration of mobile networks across Africa and Asia has made mHealth efforts a strong success. Examples of success in using mHealth – using mobile devices in health service delivery, to enable maternal care in emergency medical support in Bangladesh, Ghana, Uganda and India, point of care support in Pakistan and Indonesia, and health promotion in Tanzania, Ethiopia, Serbia and Thailand [29–31]. Research indicates that standard care with reminders, disease monitoring and management, and education through cell phone voice and short message service has helped improve health outcomes [32]. mHealth applications also enable better communication between health workers and leverages social networks to improve health outcomes [33]. mHealth based approaches have proved useful in helping address the three delays. mHealth improves maternal outcomes through (a) empowering women to contact health services and access information [34] (b) access emergency obstetric care [35] (c) giving patients knowledge of where to go and (d) enabling lesser trained health workers to provide the ‘right health care’. Despite the success of maternal care applications such as text4baby [36], mHealth and patient alerting tools have failed to undergo widespread penetration in the US due to (a) questions on quality of existing health apps [37]and (b) lack of adequate research to keep pace with ever changing technological progress [38]. However, work in LMIC indicates that a consistent messaging system integrated into the health care delivery model with the right information and a pathway to ‘receive the right care’ has positive impacts on maternal outcomes, especially across underserved populations [31, 39].
Telehealth/Telemedicine
Telehealth/Telemedicine plays an integral role in providing medical care across space and time via telecommunication technologies ranging from the telephone to robotics. It is widely perceived as a method to share medical knowledge in settings where trained staff is scarce. Telehealth is not a new concept to the US. It was widely used by the US military [40]. However, the lack of broadband infrastructure and financial, legal and healthcare policy barriers posed a significant challenge to the early advancement of telemedicine [41], leading health policymakers to relegate Telehealth to a secondary role [42]. However, these barriers are coming down. The Affordable Care Act (ACA) and the American Recovery and Reinvestment Act (ARRA) of 2009 has reduced barriers around the utilization of Telehealth [43]. These together with CMS telemedicine reimbursement changes and state level policy changes promise significant potential for the increased adoption of Telehealth systems [44]. Telehealth is widespread across LMIC, especially for maternal and child health delivery [45, 46]. While we are aware of the significant use of telemedicine within the US, we note that LMIC are creating unique uses for telemedicine using ubiquitous mobile platforms to enable low bandwidth solutions focused on improving maternal care by creating awareness and enabling better care delivery. Based on these advances, we propose that Telehealth, using more ubiquitous platforms such as mobile phones, should be given the place of prominence that it deserves within the US healthcare system.
Patient controlled health records
Patient controlled health records were introduced over two decades ago as a means of creating online repositories where patients could collect and control access to their healthcare data [47]. While revolutionary in its time, projects such as Google Health and Microsoft Health Vault that aimed to operationalize this concept were unsuccessful due to failure to win vendor support, low trust and potential risks [48]. There has been a gradual reemergence of patient portals integrated into the larger health information systems over the past decade. Unfortunately, these do not create longitudinal patient records as they can only access a single health care system. In comparison, LMIC have developed alternate versions of longitudinal patient controlled health records in the form of smart cards or plastic cards that contain an embedded computer chip to store data [49] as well as paper based medical ‘books’ that are retained by the patient. While Europe has embraced smart cards for health care, the network centric nature of the US healthcare culture hampers the widespread adoption of Smart cards [50].
One purpose of granting control of their own health record to the patient is to ensure that they become the locus on control in managing their own healthcare. To do so, healthcare networks must uniquely identify each patient. This necessity led to the development of national patient identifiers and Master Patient Indexes (MPI) that serve as registers and resolvers of patient identities in many LMIC. MPI’s have been successfully implemented across many LMIC [51]. In comparison, the US has chosen to not embrace a universal patient identifier system due to concerns of privacy [52]. However, rejecting a universal patient identifier has led to limitations in interoperability and data sharing. If implemented correctly, patient controlled health records have the potential for improved shared decision-making between the clinician, caregivers and patient. They also enable early recognition of maternal complications and / or warning signs through access and control of patient records, ultimately contributing to the reduction of the three delays.
Relationships within Health Information Systems
Healthcare is a team sport that depends on collaboration between providers, patients, payers, families, health care teams and communities. When a provider identifies a patient’s need, that need might be reported to a different participant who is able to take appropriate action. Cost of healthcare services and lack of trained staff often result in at least some parts of patient care being delegated to members of their immediate family. However, proper communication and collaboration is essential to make such efforts successful. Relationships between health care teams and family members cannot bring value to a patient unless they are easily discoverable within a healthcare system. Many EHR systems lack support to persist structured patient relationship information, a weakness identified and addressed by developers of the OpenMRS platform, an Open Source Medical Record System designed for use across underserved settings. To date, multiple sites in LMIC have adopted this feature for managing patient relationships with success [53]. We perceive that the need to technologically incorporate critical patient, family and provider relationships within health information systems will be increasingly important to the US as it moves toward a more comprehensive quality based care reimbursement mode, and that efforts should be made to capture and manage such data within a patient’s health record.
Empowered Community health workers (CHW) as catalysts of healthcare delivery
The success of adopting health information infrastructure depends on how information derived from these systems is used impact healthcare delivery. While providers play a crucial role in decision-making, their ability to prevent the three delays outside of a healthcare setting is very limited. CHW’s are frontline public health workers with a close understanding of the community they serve. Their links to the community allow them to reach out to patients at their homes and communities, and improve the quality and cultural competence of service delivery. CHW programs are widespread across LMIC, where they are a predominant topic in discussions around primary health-care delivery. Success stories in using CHW’s for improving healthcare are reported from Uganda, Ethiopia and Tanzania [54]. These successes have encouraged the governments of Brazil, Pakistan, and India to make CHWs a cornerstone of scaling up community health delivery, especially for providing maternal care [55].
CHW’s are not an entirely new concept to the US. They have significant potential to improve maternal outcomes in the US, as demonstrated by successful projects driven by the Indian Health Service and Tribally Operated Health Programs such as the Alaska Community Health Aide Program (CHAP) [56]. Unfortunately, many US based CHW initiatives are short-term, grant-funded projects and grassroots volunteer community initiatives [57]. Unlike many developing countries, US health policy administrators have relegated CHW to a secondary role. However, lessons learned from underserved settings offer much promise for the introduction and use of empowered CHW who are capable of reaching out to pregnant women at the grassroots level. CHW also have the potential to be far more cost efficient, and reduce treatment costs via early evaluation and detection, appropriate referrals, and longitudinal support
Discussion
Enabling better seeking of care, access to care, and receiving the right care at the right time can significantly reduce maternal mortality and morbidity across both high-income and low-income settings. In both LMIC and the US, these factors are hindered by the scarcity of economic, physical and human resources, or the inability to make them available to the right people at the right time, While US health information infrastructure is more than capable of supporting high quality care where ample resources are available, it falls short of meeting the needs of underserved populations such as minorities, low-income communities and rural areas.
Our research identified five informatics based solutions successfully adopted by LMIC countries, and suitable for adoption in the US; (a) mHealth and patient facing alerting (b) Telehealth (c) Patient controlled health records (d) Relationships within Health Information systems and (e) Community health workers as catalysts of healthcare delivery. In examining these innovations, we found that some of these had already been considered by the US in the past, but failed/impeded by inherent differences in the US healthcare system. However, recent changes in US infrastructure, law and policy aimed at reducing healthcare costs and making healthcare services more accessible [58] and a commitment to comprehensive care models are breaking down these barriers, and improving the potential of adopting these innovations in the US. We found that many of the proposed solutions were strongly interrelated, and that successful maternal care innovations often consisted of combinations of the aforementioned innovations. As shown before, CHW networks in underserved settings depended on information received and integrated via mHealth solutions to guide much of their work. Similarly, efficient persistence and retrieval of relationships, entered into medical records at the point of care, also helped CHW networks. Having improved patient ownership of clinical data enables better dissemination and data integration for use in clinical care, with CHWs, clinicians, other health providers and family and community members. We also found that, while the five proposed innovations were dependent upon technology, technology was insufficient by itself. Common themes of knowledge, technology, patient and community empowerment, coordination and process change emerged (figure 2).
Figure 2.
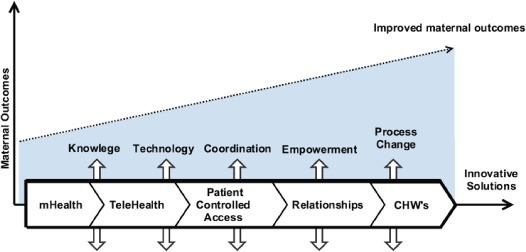
Enabling better maternal care outcomes. Potential innovations and general themes
The findings indicate that the proper use of health information could play a significant role in improving US maternal outcomes, as well as reducing associated healthcare costs. Many of the innovations that we recommended for evaluation in the US could be used for a wide range of healthcare services over and above maternal care delivery. Investigation of the underlying themes show that the key to maternal care is to place informed patients at the center of their own care. Traditionally, US healthcare delivery is known for its rigid health infrastructure, workflows and provider centric care. Clearly, this approach has done little to address worsening US maternal care outcomes. In comparison, successful innovation across LMIC countries seem to focus on creating and empowering informed patients and their communities to act on their own needs. If so, informatics solutions will be expected to play a crucial role in integrating patients and communities into the healthcare delivery process, informing them, and empowering them to take action on their own needs.
It could be argued that the US still suffers from significantly lesser maternal mortality and morbidity than LMIC despite of the 136% rise in maternal outcomes from 1990-2013, and that many LMIC reported significant improvements in maternal outcomes during this same period starting from comparatively high baseline measures. In other OECD countries, the same measures have remained relatively constant with significantly lower costs of care, suggesting that the rise in maternal mortality and morbidity is a significant concern. More so because a majority of these outcomes were preventable, and because health outcomes worsened despite of significant increases in financial spending in the US, which indicates the need to re-think current healthcare focus areas. Additionally, health IT based interventions have demonstrated their ability to reduce preventable maternal mortality and morbidity in LMIC [59, 60], indicating that they may be able to do the same in the US. Furthermore, every challenge identified in table 1 could be addressed via health informatics innovations. Another possible area for debate would be contextual changes between LMIC settings and the US. US based healthcare is far more expensive than LMIC or even other high-income countries. However, the most adversely hit populations in the US are at-risk populations and the poor, who also benefit from compatible state funded health programs. Additionally, maternal care is very well funded, with multiple welfare/aid options for those in need. Therefore, adaptions of LMIC based approaches for the US is feasible. As future steps and further validation of our findings, we propose the evaluation of each of the innovations identified by our study using the Technology Acceptance Model (TAM) [61]. The TAM model presents how target users accept and use a given technology, and thus, will further evaluate the potential of successfully adopting such innovations across the US.
Conclusion
Our study identified significant potential for adopting reverse innovations to help address weak maternal care outcomes in the US. Many restrictions that historically hampered these innovations have already been removed, leading to improved chances for their success. Recent US policy and administrative changes aimed at reducing healthcare costs and creating comprehensive health care delivery models are also making these solutions more realistic. General themes that drive these innovations indicate that the key to better maternal care outcomes is to place patients at the center of their own care by empowering informed patients and their community to act on their own needs. While the role of these factors and themes in enabling improved health outcomes is widely recognized, the importance of a holistic model that includes, but is not limited to informatics is often disregarded. We highlight the intersections of technology and process changes that have been shown to improve care in LMICs. We believe that there is ongoing evaluation and future work in this area that needs to occur, including a rigorous comparison of multicountry implementations, and an evaluation of the return on investment of these identified innovations. However, recognizing that LMIC have developed appropriate technological and process solutions that can benefit underserved settings in high-income countries is critical. Adversity itself can be a springboard for innovation. In many cases, technological solutions developed and lessons learned in LMIC are applicable and beneficial to the high-income countries. It behooves us to identify, evaluate and incorporate appropriate solutions, regardless of their origin, as we continue to seek global health equity.
Appendix A
| Organization | Type of publications/reports |
|---|---|
| World Health Organization (WHO) | Various reports that include assessments on US maternal outcomes |
| United Nations [55] | The United Nation Children’s Fund (UNICEF) and the United Nations Population Fund (UNFPA) publish annual reports and strategic plans. |
| Centers for Disease Control and Prevention (CDC) | Annual and weekly reports, data and statistics, reports on major conditions/illnesses |
| US Department of Health and Human Services | National surveys, State and national data, research reports |
| Indian Health Service (IHS) | Reports to Congress, various publications |
| The American Congress of Obstetricians and Gynecologists (ACOG) | Committee opinions, department publications and endorsed documents, journals, position statements, advisories and bulletins. |
| The National Academies of Sciences, Engineering, and Medicine | Various reports/publications from the Institute of Medicine (IOM) |
| Agency for Healthcare Research and Quality (AHRQ) | Maternal care reports an analytical data reports |
Appendix B
(a) OVID Medline database
| Expression no. | Searches | Results |
|---|---|---|
| 1 | exp Developing Countries/or underserved nations.mp. | 68199 |
| 2 | "low and middle income countries".mp. | 6458 |
| 3 | lmic.mp. | 756 |
| 4 | exp Africa/ | 221998 |
| 5 | exp Asia/ | 663253 |
| 6 | exp Latin America/ | 9580 |
| 7 | electronic medical record.mp. or exp Electronic Health Records/ | 15919 |
| 8 | exp Medical Records Systems, Computerized/ | 32097 |
| 9 | exp Information Systems/ | 200066 |
| 10 | exp Maternal Health Services/or maternal care.mp. | 42930 |
| 11 | exp Maternal Health/or exp Maternal Mortality/or exp Pregnancy Complications/ | 390150 |
| 12 | exp Pregnancy Complications/or exp Postpartum Hemorrhage/or exp Hypertension, Pregnancy-Induced/or “maternal morbidity”.mp. or exp Pre- Eclampsia/ | 386419 |
| 13 | 1 or 2 or 3 or 4 or 5 or 6 | 914247 |
| 14 | 7 or 8 or 9 | 211821 |
| 15 | 10 or 11 or 12 | 418002 |
| 16 | 13 and 14 and 15 | 279 |
| 17 | Remove duplicates from 16 | 244 |
(b) EMBASE: No. of unique results: 83
‘electronic medical record’/exp OR ‘medical information system’/exp OR ‘hospital information system’/exp AND (‘developing country’/exp OR ‘south and central america’/exp OR ‘africa’/exp OR ‘asia’/exp) AND (‘maternal care’/exp OR ‘maternal welfare’/exp OR ‘maternal mortality’/exp OR ‘maternal morbidity’/exp)
(c) Web of Science: No. of results: 21
Due to the limited number of publications retrieved, we searched for all publications that discussed maternal complications and health information systems, and filtered publications that dealt with LMIC via manual review.
TITLE: (maternal health* OR maternal care* OR maternal mortality* OR maternal morbidity* OR Pregnancy Complications* OR Postpartum Hemorrhage* OR Pre-Eclampsia*) AND TITLE: (electronic health record* OR health information system* OR clinical information system* OR computer*)
References
- 1.International Federation of Health Plans. 2010 comparative price report: Medical and hospital fees by country. 2010. [cited 2016]. Available from: http://ifhp.com/documents/IFHP_Price_Report2010ComparatrvePriceReport29n2010.pdf.
- 2.Thomson Healthcare. The healthcare costs of having a baby: Thomson HealthCare Firm. 2007.
- 3.Unicef. T rends in maternal mortality: 1990 to 2013. 2014.
- 4.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the united states. Obstetrics & Gynecology. 2012;120(5):1029–36. doi: 10.1097/aog.0b013e31826d60c5. [DOI] [PubMed] [Google Scholar]
- 5.MacDorman MF, Matthews T, Mohangoo AD, Zeitlin J. International comparisons of infant mortality and related factors: United states and europe, 2010. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2014;63(5):1–6. [PubMed] [Google Scholar]
- 6.The World Bank. Maternal mortality ratio (modeled estimate, per 100,000 live births) 2015. Available from: http://data.worldbank.org/indicator/SH.STA.MMRT.
- 7.Control CfD, Prevention. Severe maternal morbidity in the united states. Atlanta, GA: Author Retrieved from www cdc gov/reproductivehealth/MaternallnfantHealth/SevereMaternalMorbidity html. 2014.
- 8.Tucker MJ, Berg CJ, Callaghan WM, Hsia J. The black-white disparity in pregnancy-related mortality from 5 conditions: Differences in prevalence and case-fatality rates. American Journal of Public Health. 2007;97(2):247–51. doi: 10.2105/AJPH.2005.072975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Pregnancy mortality surveillance system. 2017. [cited 2017]. Available from: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html.
- 10.Amnesty International. Amnesty International Publications; 2010. Deadly delivery: The maternal health care crisis in the USA. [Google Scholar]
- 11.Kinney MV, Kerber KJ, Black RE, Cohen B, Nkrumah F, Coovadia H, et al. Sub-saharan africa’s mothers, newborns, and children: Where and why do they die? PLoS Med. 2010;7(6):e1000294. doi: 10.1371/journal.pmed.1000294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bingham D, Strauss N, Coeytaux F. Maternal mortality in the united states: A human rights failure. Contraception. 2011;83(3):189–93. doi: 10.1016/j.contraception.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 13.Main EK, Menard MK. Maternal mortality: Time for national action. Obstetrics & Gynecology. 2013;122(4):735–6. doi: 10.1097/AOG.0b013e3182a7dc8c. [DOI] [PubMed] [Google Scholar]
- 14.Thaddeus S, Maine D. Too far to walk: Maternal mortality in context. Social science & medicine. 1994;38(8):1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 15.Kay M, Santos J, Takane M. Mhealth: New horizons for health through mobile technologies. World Health Organization. 2011;64(7):66–71. [Google Scholar]
- 16.Govindarajan V, Trimble C. Harvard Business Press; 2013. Reverse innovation: Create far from home, win everywhere. [Google Scholar]
- 17.Govindarajan V, Trimble C. Reverse innovation: A global growth strategy that could pre-empt disruption at home. Strategy & Leadership. 2012;40(5):5–11. [Google Scholar]
- 18.Syed SB, Dadwal V, Martin G. Reverse innovation in global health systems: Towards global innovation flow. Globalization and health. 2013;9(1):1. doi: 10.1186/1744-8603-9-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bettany-Saltikov J. Learning how to undertake a systematic review: Part 1. Nursing Standard. 2010;24(40):47–55. doi: 10.7748/ns2010.08.24.50.47.c7939. [DOI] [PubMed] [Google Scholar]
- 20.Pathman DE, Konrad TR, Dann R, Koch G. Retention of primary care physicians in rural health professional shortage areas. American journal of public health. 2004;94(10):1723–9. doi: 10.2105/ajph.94.10.1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilson N, Couper I, Vries De E, Reid S, Fish T, Marais B. Inequitable distribution of healthcare professionals to rural and remote areas. Rural and remote health. 2009;9(1060) [PubMed] [Google Scholar]
- 22.Copeland VC. African americans: Disparities in health care access and utilization. Health & Social Work. 2005;30(3):265. doi: 10.1093/hsw/30.3.265. [DOI] [PubMed] [Google Scholar]
- 23.Ku L, Matani S. Left out: Immigrants’ access to health care and insurance. Health Affairs. 2001;20(1):247–56. doi: 10.1377/hlthaff.20.1.247. [DOI] [PubMed] [Google Scholar]
- 24.Ip WY. Relationships between partner’s support during labour and maternal outcomes. Journal of Clinical nursing. 2000;9(2):265–72. doi: 10.1046/j.1365-2702.2000.00358.x. [DOI] [PubMed] [Google Scholar]
- 25.Ireys HT, Chernoff R, DeVet KA, Kim Y. Maternal outcomes of a randomized controlled trial of a community-based support program for families of children with chronic illnesses. Archives of pediatrics & adolescent medicine. 2001;155(7):771–7. doi: 10.1001/archpedi.155.7.771. [DOI] [PubMed] [Google Scholar]
- 26.Leddy MA, Power ML, Schulkin J. The impact of maternal obesity on maternal and fetal health. Rev Obstet Gynecol. 2008;1(4):170–8. [PMC free article] [PubMed] [Google Scholar]
- 27.Fiks AG, Grundmeier RW, Biggs LM, Localio AR, Alessandrini EA. Impact of clinical alerts within an electronic health record on routine childhood immunization in an urban pediatric population. Pediatrics. 2007;120(4):707–14. doi: 10.1542/peds.2007-0257. [DOI] [PubMed] [Google Scholar]
- 28.Teich JM, Osheroff JA, Pifer EA, Sittig DF, Jenders RA. Clinical decision support in electronic prescribing: Recommendations and an action plan. Journal of the American Medical Informatics Association. 2005;12(4):365–76. doi: 10.1197/jamia.M1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tamrat T, Kachnowski S. Special delivery: An analysis of mhealth in maternal and newborn health programs and their outcomes around the world. Maternal and child health journal. 2012;16(5):1092–101. doi: 10.1007/s10995-011-0836-3. [DOI] [PubMed] [Google Scholar]
- 30.Medhanyie AA, Little A, Yebyo H, Spigt M, Tadesse K, Blanco R, et al. Health workers’ experiences, barriers, preferences and motivating factors in using mhealth forms in ethiopia. Human Resources for Health [Electronic Resource] 2015;13:2. doi: 10.1186/1478-4491-13-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tamrat T, Kachnowski S. Special delivery: An analysis of mhealth in maternal and newborn health programs and their outcomes around the world. Maternal and child health journal. 2012:1–10. doi: 10.1007/s10995-011-0836-3. [DOI] [PubMed] [Google Scholar]
- 32.Krishna S, Boren SA, Balas EA. Healthcare via cell phones: A systematic review. Telemedicine and e-Health. 2009;15(3):231–40. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 33.Braa K, Purkayastha S. Sustainable mobile information infrastructures in low resource settings. Studies in health technology and informatics. 2009;157:127–32. [PubMed] [Google Scholar]
- 34.Lund S. Profile/Global Health. Copenhagen: University of Copenhagen; 2009. Mobile phones can save lives; pp. 18–9. [Google Scholar]
- 35.Fournier P, Dumont A, Tourigny C, Dunkley G, Dramé S. Improved access to comprehensive emergency obstetric care and its effect on institutional maternal mortality in rural mali. Bulletin of the World Health Organization. 2009;87(1):30–8. doi: 10.2471/BLT.07.047076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Evans WD, Abroms LC, Poropatich R, Nielsen PE, Wallace JL. Mobile health evaluation methods: The text4baby case study. Journal of health communication. 2012;17(sup1):22–9. doi: 10.1080/10810730.2011.649157. [DOI] [PubMed] [Google Scholar]
- 37.Powell AC, Landman AB, Bates DW. In search of a few good apps. Jama. 2014;311(18):1851–2. doi: 10.1001/jama.2014.2564. [DOI] [PubMed] [Google Scholar]
- 38.Nilsen W, Kumar S, Shar A, Varoquiers C, Wiley T, Riley WT, et al. Advancing the science of mhealth. Journal of health communication. 2012;17(sup1):5–10. doi: 10.1080/10810730.2012.677394. [DOI] [PubMed] [Google Scholar]
- 39.Akter S, Ray P. Mhealth-an ultimate platform to serve the unserved. Yearb Med Inform. 2010;2010:94–100. [PubMed] [Google Scholar]
- 40.Poropatich R, Lai E, McVeigh F, Bashshur R. The us army telemedicine and m-health program: Making a difference at home and abroad. Telemedicine and e-Health. 2013;19(5):380–6. doi: 10.1089/tmj.2012.0297. [DOI] [PubMed] [Google Scholar]
- 41.Alverson DC, Shannon S, Sullivan E, Prill A, Effertz G, Helitzer D, et al. Telehealth in the trenches: Reporting back from the frontlines in rural america. Telemedicine Journal & e-Health. 2004;10(Supplement 2):S-95–S-109. [PubMed] [Google Scholar]
- 42.Mamlin BW, Tierney WM. The promise of information and communication technology in healthcare: Extracting value from the chaos. The American Journal of the Medical Sciences. 2016;351(1):59–68. doi: 10.1016/j.amjms.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 43.LeRouge C, Garfield MJ. Crossing the telemedicine chasm: Have the us barriers to widespread adoption of telemedicine been significantly reduced? International journal of environmental research and public health. 2013;10(12):6472–84. doi: 10.3390/ijerph10126472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thomas L, Capistrant G. State telemedicine gaps analysis: Coverage and reimbursement. American Telemedicine Association. 2015 [Google Scholar]
- 45.Oh TH, Lim HS, Besar R. Telemedicine in malaysia and indonesia: The importance, opportunities and challenges. Journal of Mechanics in Medicine and Biology. 2006;6(04):337–48. [Google Scholar]
- 46.World Health Organization. Ehealth and innovation in women’s and children’s health: A baseline review. 2014. Available from: http://apps.who.int/iris/bitstream/10665/111922/1/9789241564724_eng.pdf.
- 47.Szolovits P, Doyle J, Long WJ, Kohane I, Pauker SG. Guardian angel: Patient-centered health information systems: Massachusetts Institute of Technology. Laboratory for Computer Science. 1994 [Google Scholar]
- 48.Spil T, Klein R, editors. System Sciences (HICSS), 2014 47th Hawaii International Conference on. IEEE; 2014. Personal health records success: Why google health failed and what does that mean for microsoft healthvault? [Google Scholar]
- 49.Lagomarsino G, Garabrant A, Adyas A, Muga R, Otoo N. Moving towards universal health coverage: Health insurance reforms in nine developing countries in africa and asia. The Lancet. 2012;380(9845):933–43. doi: 10.1016/S0140-6736(12)61147-7. [DOI] [PubMed] [Google Scholar]
- 50.Vezina K. Medical smart cards find their niche 2011. Available from: https://www.technologyreview.com/s/424281/medical-smart-cards-find-their-niche/ [Google Scholar]
- 51.Stroetmann KA, editor. IST-Africa Conference Proceedings, 2014. IEEE; 2014. Scoping global good ehealth platforms: Implications for sub-saharan africa. [Google Scholar]
- 52.Butler M. Finding john doe: Patient matching and the need for a national health safety identifier. 2016 Available from: http://bok.ahima.org/doc?oid=301386 -.WV5eIrYrJ0s. [PubMed] [Google Scholar]
- 53.Kasthurirathne S, Mamlin B, Cullen T. Leveraging the value of human relationships to improve health outcomes. Applied Clinical Informatics. 2017;8(1):108–21. doi: 10.4338/ACI-2016-08-RA-0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lunsford SS, Fatta K, Stover KE, Shrestha R. Supporting close-to-community providers through a community health system approach: Case examples from ethiopia and tanzania. Human Resources for Health [Electronic Resource] 2015;13:12. doi: 10.1186/s12960-015-0006-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu A, Sullivan S, Khan M, Sachs S, Singh P. Community health workers in global health: Scale and scalability. Mount Sinai Journal of Medicine: A Journal of Translational and Personalized Medicine. 2011;78(3):419–35. doi: 10.1002/msj.20260. [DOI] [PubMed] [Google Scholar]
- 56.Landon B, Loudon J, Selle M, Doucette S. Factors influencing the retention and attrition of community health aides/practitioners in alaska. The Journal of Rural Health. 2004;20(3):221–30. doi: 10.1111/j.1748-0361.2004.tb00032.x. [DOI] [PubMed] [Google Scholar]
- 57.Balcazar H, Lee Rosenthal E, Nell Brownstein J, Rush CH, Matos S, Hernandez L. Community health workers can be a public health force for change in the united states: Three actions for a new paradigm. American journal of public health. 2011;101(12):2199–203. doi: 10.2105/AJPH.2011.300386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Orszag PR, Emanuel EJ. Health care reform and cost control. New England Journal of Medicine. 2010;363(7):601–3. doi: 10.1056/NEJMp1006571. [DOI] [PubMed] [Google Scholar]
- 59.Bukachi F, Pakenham-Walsh N. Information technology for health in developing countries. Chest Journal. 2007;132(5):1624–30. doi: 10.1378/chest.07-1760. [DOI] [PubMed] [Google Scholar]
- 60.Piette JD, Lun K, Moura Jr LA, Fraser HS, Mechael PN, Powell J, et al. Impacts of e-health on the outcomes of care in low-and middle-income countries: Where do we go from here? Bulletin of the World Health Organization. 2012;90(5):365–72. doi: 10.2471/BLT.11.099069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lee Y, Kozar KA, Larsen KR. The technology acceptance model: Past, present, and future. Communications of the Association for information systems. 2003;12(1):50. [Google Scholar]


