Abstract
Annually, 1.6-3.8 million concussions occur from sports in the United States, which account for 5-9% of all sports injuries. The dangers of concussions include prolonged post-concussive symptoms, increased risk of subsequent concussions, seizures, mental health issues, and in cases of second-impact syndrome (SIS), possible death. Certified Athletic Trainers (ATC) continue to serve an important role in providing assessment and treatments for athletes with sports-related injuries. They provide a critical safety net due to limited knowledge and misconceptions of concussion held by some youth sports coaches and athletes. However, availability of services from ATCs in rural areas is a challenge. In order to help extend coverage to more rural student athletes, we propose designing a telemedicine app following the mHealth development roadmap from the Center for eHealth Research (CeHRes). In this paper we will document contextual inquiry, user requirements capture, design phases, and app evaluation from the targeted user base.
Introduction
There are an estimated 1.6-3.8 million concussions that occur from sports and recreational activity in the United States annually1. Board Certified Athletic Trainers (ATC) provide a critical safety net due to limited knowledge and misconceptions of concussions held by some coaches and athletes. Studies have shown schools with ATCs have lower overall injury rates, and higher rates of concussion diagnoses due to increased reporting and accurate assessment. However, only 55% of athletes in United States public secondary schools have access to a full-time ATC, and only 37% of schools employ a single ATC. Currently 30% of public secondary schools in the US lack an ATC, leading to 24% of sporting events that have no medical coverage2. Due to budget restrictions, many schools resort to contracting an ATC from local physical therapy clinics or hospitals. This is an alternative to hiring a full time ATC, and often the ATC under contract will cover two or more schools. These ATCs have to select which school they will cover when events are held concurrently. This contributes to the overall medical coverage gap. Given the budgetary concerns in many schools, tools that facilitate remote diagnosis and/or treatment of patients by means of telecommunications technology may be one solution; specifically, an mHealth app may be ideal for many schools.
Concussions account for 5-9% of all sports injuries, which often translate into visits to the emergency room3. For most athletes (80-90%) concussions resolve in 7-10 days, however in some cases, symptoms can persist for months or even years1. The dangers of these injuries include prolonged post-concussive symptoms, increased risk of subsequent concussions, seizures, mental health issues including depression, and in rare cases, death. Of particular concern is second-impact syndrome (SIS), which may occur if an athlete returns to activity while still exhibiting concussion symptoms. SIS can cause a rapid increase in intracranial pressure, brain stem herniation, and often death. The most worrying aspect is while still recovering from the initial concussion, an additional impact of lower severity can lead to the onset of SIS. Chronic traumatic encephalopathy (CTE) is emerging as a long-term health concern that may be linked to concussions. The key to minimizing these dangers involves timely diagnosis, comprehensive treatment and rehabilitation plans, and return-to-play guidance from trained medical professionals like ATCs. In the absence of medical professionals on the field, the ER is often the only outlet for athletes with suspected concussions. When reviewing reports from ER visits, a 62% increase in non-fatal traumatic brain injuries occurred between 2001-20091, indicating that ER visits for concussions have been on the rise. It is estimated that 12% of ER visits are non-urgent, and studies have shown that overuse of ER detrimentally impacts the entire hospital4. Unnecessary visits to the ER for non-urgent conditions also carry a risk of nosocomial infections, overtreatment, and lack of continuity of care. Hence, there is an incentive to provide these injured athletes access to medical care without having to escalate that care into a trip to the ER.
For concussions, the standard of care when evaluating concussions is by a physician or licensed healthcare provider who are specifically trained. Diagnosis of a concussion involves identifying one or more of the following clinical domains: somatic symptoms, cognitive impairment (e.g., slow reaction times), behavioral changes (e.g., irritability), sleep disturbance (e.g., insomnia), and physical symptoms (e.g., balance, amnesia, loss of consciousness)5. To assist with the diagnosis of sports concussions, there are several technological approaches available. Functional neuroimaging is the most popular approach; there is also qualitative EEG, and impact sensors. A computer-based neuropsychological testing tools has been developed called the Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT)6 which is also very popular. Telemedicine and mobile devices are options that have been relatively unexplored as potential tools7. Work by Vargas et al. has proposed a wheel and spoke telehealth approach, centralizing specialists who are available via a telemedicine robot8, but the utilization of an mHealth app solution is largely untapped. There are over 20 mobile concussion assessment apps available on the market, but none of these are part of a telehealth system. Most of these existing apps only assist the user in detecting if a trained healthcare provider should evaluate the individual. A recent systematic review of smartphone and tablet concussion apps raises concerns about the appropriateness of these tools for different groups of end users, and they also found that the apps were not always in compliance with testing guidelines9. There are some validated tools used by medical professionals for concussion evaluations, like the Sport Concussion Assessment Tool 3 (SCAT3)10. When used by a non-medical layperson, the SCAT3 test can be used to help identify signs of concussions, but diagnosis should remain a task left to medical professionals. A less technical sport concussion recognition method, like the Pocket Concussion Recognition11 tool is recommended for anyone without a medical background. This is where we would distinguish our proposed telehealth app. With a user-centric development path, and using ATCs as members of the focus group, the intent is to ensure ATCs remain the nexus of the medical evaluation process. Many of the available apps aim to place the coaches, parents, or athletes into the drivers seat for these decisions. This can be problematic due to biases (an athlete trying to “tough it out” on an injury) or possible conflicts of interest (placing winning over the health of the athlete).
Visual examination during concussion testing is a key component, which is what led us to pursue a telehealth model. There are sections in the SCAT3 test that rely on observing the athlete, like the balance test. It is also important to watch facial expressions to ensure the subject comprehends the question. For example, the ATC will want to make sure they understand all the questions being asked, such as if they are experiencing nausea. Does the athlete know what nausea is, or is there any attempt at evasion during the questions? This begs the question, why not just have the ATC complete the SCAT3 test via Skype, FaceTime, or other similar video conferencing tools? It is possible to do, but not practical. Usability and secure storage of health information are two major obstacles encountered with this approach. An ad hoc solution of conducting the SCAT3 over a conferencing app still would still rely on using paper records. If the video conferencing was integrated into a single app, there are inherent advantages. Currently, the SCAT3 is principally designed to be paper-based tool, where sections of the test are completed via print outs of the test. Any paper based data storage approach is faced with major concerns about issues with readability, data entry errors, retrieval, and backup12,13. Many of these problems can be avoided by performing data collection into a secure HIPAA compliant database, following guided data entry steps with error checking, all into a file attached to a particular individual. These paper files also would have a high likelihood of being stored under lock and key in the ATC’s office in addition with any other medical files. Retrieval is not a problem if both the athlete and the ATC are in that office, but in the rural environment, the ATC is often working remotely. Secure logins and file encryption would ensure the data would be accessible to the ATC as long as they were able to connect online. Using alternate video conferencing tools is a shortcut that would solve the access to medical professionals temporarily, but we feel the complications associated with it would discourage repeat use. Initial conceptualization of th
The primary aim of this paper is to detail the development of this proposed mHealth app following the protocol recommended by the Center for eHealth Research (CeHRes)14, presenting a prototype version of the app, and reviewing its reception by ATCs. Specifically, four primary components of the five stages of the CeHRes roadmap will be conducted: contextual inquiry, value specification, design, and operationalization.
Importance of Research
Telemedicine is an established tool for extending medical coverage to underserved and rural areas15,16 Telestroke17 is one example of a successful telehealth tool that has been able to provide cost-effective18 coverage to rural areas where stroke specialists are lacking19. However, there is a lack of work in developing a telehealth solution for assessing concussions and helping to extend care and treatment options for rural high school athletes7. When looking into application options for this technology, there is a distinct opportunity for rural Nebraska. The distance between rural high schools is a factor impacting the availability of full time ATCs to provide medical coverage. The Nebraska School Activities Association (NSAA) is the organizing body that oversees all interscholastic activity for the state. Table 1 highlights sports in NSAA’s seasonal schedule with increased risk and the number of rural participants in those highlighted sports for that season. The tally was taken from NSAA’s 2014-2015 statewide report of participants per school. Each school was identified as rural or urban by using the Economic Research Service Rural-Urban Commuting Areas (RUCA) for counties with codes 4-10, codes 1-3 were designated as urban20.
Table 1.
2014-15 NSAA High School Sport Schedule and number of rural participants
| Season | Fall | Winter | Spring |
|---|---|---|---|
| Sport | Cross Country | Basketball* | Baseball |
| Football | Swimming | Boys Golf | |
| Softball | Wrestling | Soccer | |
| Boys Tennis | Cheerleading | Girls Tennis | |
| Volleyball | Track and Field | ||
| Girls Golf | |||
| Total High Risk Rural Participants | 9,173 | 13,260 | 1,992 |
*Sports in bold are sports with the highest risk for concussion3
Detailed statistics on the exact number of ATCs covering these athletes in Nebraska is difficult to find. There is a lack of standard reporting to indicate the number of staff ATCs employed by high schools, as discovered by Schwaderer and Unruh21. Some schools administrators recorded full time ATCs in the same fashion as ATCs that were contracted out to multiple schools, making it challenging to identify exact coverage gaps. They were able to build a general ATC coverage map that depicts the disparity of ATC availability between rural and urban areas in Nebraska (Figure 1). The numbers of rural participants at risk for concussion and the large areas of Nebraska with coverage gaps lend itself to exploring a solution through mHealth.
Figure 1.
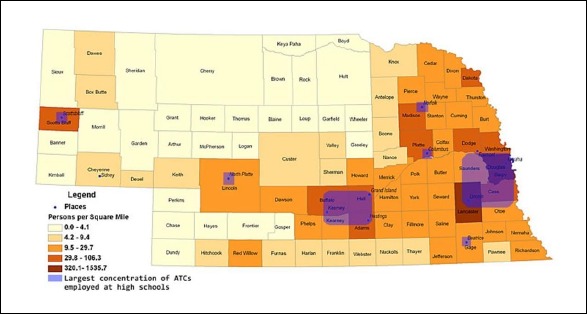
ATC Coverage in Nebraska (image courtesy of Schwaderer & Unruh (a), UNK)
Roadmap
The Center for eHealth Research roadmap was selected as the template for developing this project22,23. One of the primary goals of this app is to make it appealing to the audience we are trying to reach, primarily ATCs and their student athletes. The human-centered design23 of the CeHRes road map helps to achieve this aim.
There are five phases of the road map, with iterative elements to help ensure that improvement is occurring through each stage of the mHealth app development.
Contextual inquiry – the app’s target user perspective is evaluated and the current standard of care is considered.
Value specification – Stakeholders and values are identified and translated into user requirements.
Design – taking the user requirements, developers, stakeholders, and targeted user collaborate in building the app.
Operationalization – once the technology has been built, steps are taken to market the product and integrate it into practice.
Summative evaluation – the final stage is a review of the product, how is it being used and what kind of impact is it having on healthcare.
Research Approach or Methodology
In following the CeHRes roadmap, the first step is to identify key stakeholders and explore the relevance of the idea in the contextual inquiry phase. A focus group comprised of these stakeholders was held as a part of the value specification phase. The output from the focus group helped to guide the development of the app in the design phase of the CeHRes roadmap. The target market for this app is aimed at high school level athletics (grades 9-12). High schools often are faced with restrictive budgets that contribute to the previously described ATC shortages, in comparison to college and university athletics, which have more robust budgets. At of this point, the contextual inquiry, and value specification, and design phases have been completed. The Operationalization stage has started, being with revisiting the requirements captured at the beginning of the process with the focus group and conducting an End-User Computing Satisfaction (EUCS) survey. For the focus group component of the study and the EUCS survey, IRB 206-16-EX was submitted as an exempt educational, behavioral, and social science research review, and was accepted by the UNMC IRB board. The last two components of the CeHRes roadmap, operationalization and summative evaluation will be presented when those stages are complete and field-testing has been completed. These final two stages focus on marketing and market impact once the app has been released. Completion of the design phase provided a tangible product, which we felt presented a natural break in the process that could be shared. Additional details on these plans will be explained later in this paper.
Research question
There are three principal research questions that will be investigated in this paper:
Who has a stake in addressing the healthcare problem of concussions?
How can technologies contribute to a better quality of care, and in what manifestation can technology contribute?
Was the design process able to meet user requirements established by the stakeholders and targeted users?
Results
Contextual inquiry phase: Stakeholder and targeted users
After a literature review and market examination was completed, the authors of this paper conducted a brainstorming session to identify all stakeholders and targeted users. The results from that session generated the following list:
Patients – the student athletes participating in the sporting event, and are suspected of suffering from a concussion.
Certified Athletic Trainers – medical providers assigned to provide coverage for the sporting events. Typically assigned to a particular team or school, for the purpose of this app, these ATCs would be at a different location than the patient.
Emergency Medical Technician (EMT) – EMTs occasionally have been hired to provide medical coverage for these sporting events.
School nurses – school provided medical professional.
Parents & Guardians – due to the targeted patients for this app are high school aged athletes, many would be considered minors, and thus require their involvement for this mHealth app.
Coaches, Staff, and Game Officials – individuals that are involved with the patient’s sports team, or are involved with the officiating of the match.
Principals, Athletic Directors, High School administration – many of the matches and practice sessions where a potential concussion could occur happen on school property.
The primary user base was designated as ATCs who work with rural athletes, and the coaches of those rural athletes, and thus were critical to the design stage. Other stakeholders could be approached once the app was developed.
Value specification phase: focus group
The focus group was conducted on May 25th, 2016 for 90 minutes. Five members were included in this ininterview session. Four of the members are certified athletic trainers with various backgrounds and levels of experience, and one member was a developer with medical software applications experience. The first ATC is practicing at a local high school in the Omaha metropolitan area. The second ATC is employed at the University and is involved in an athletic training education program. This program offers both undergraduate and graduate degrees in athletic training. The third ATC previously worked at the collegiate level, and now works at a medical center as director for sports medicine in addition to being member of the national certification board for athletic training. The fourth ATC is a director of operations for a clinic that subcontracts out ATCs and holds an executive role in the Nebraska State Athletic Trainers’ Association (NSATA), part of the National Athletic Trainers’ Association (NATA). This provided a wide range of views and perspectives to draw from.
The focus group was recorded and transcribed into a word document to serve as input for app requirements. The transcripts and artifacts generated by the focus group were used to guide efforts in the design stage. The paper versions of the definitions of the “10 E’s in e-health”24 and a print out version of the preliminary app mock-up (Fig. 2) were collected after the session was complete.
Eysenbach’s “10 E’s” are used to help establish a clear vision for the mHealth app. They are values that encompass what e-Health should aim for:
Efficiency
Empowerment
Enabling
Ethics
Enhancing quality
Encouragement
Extending
Equity
Evidence based
Education
In Eysenbach’s paper, each of these terms is explained in more depth. However, having the focus group define these values in context of the mHealth app helped to identify what elements are most desired from the final product. Following up and having the group pick the top three after the definitions are complete provided insight to what was desired the most from the mHealth app. These documents were treated as additional research artifacts, which contained notes, and questions that the participants had during the focus group interview.
Guidelines for designing a telehealth concussion app
To help elucidate the design guidelines, there needs to be a clear directive captured from the stakeholders in the focus group. These were specified as values, and helps to establish the boundaries and directions our development work should take when building the app. To help identify the key values for this project, the focus group reviewed Eysenbach’s list of “10 E’s”. From the list, three stood apart from the rest: enhancing quality of care, efficiency, and extending the scope of care.
The focus group was encouraged to define what these terms mean, ‘in their own words’, when discussing how an mHealth app could aid in remote concussion assessment. For enhancing quality of care, the emphasis was more on follow up care over the initial assessment. As one member stated: “There is value for using this tool on the sidelines, but I think it would be more helpful when we check up on them later.” The consensus of the group was that this would not be a tool that they would expect either athletes or coaches to pull out and use in the middle of a match. After the match or practice was seen as the more likely opportunity for the mHealth app to come into play. This also was reflected in how the group defined efficiency. Eysenbach states that efficiency decreases cost, by either cutting unnecessary or duplicate diagnostic interventions. The focus group felt that efficiency was more along terms of time saved. By allowing ATCs to follow up with athletes across town, or in another town entirely, the time spent traveling to those locations could be reduced. Often, when ATCs are contracted out to multiple locations, they spread their visits out across the week. It is possible that an athlete may have to wait a few days before the ATC is scheduled to visit their location. This exchange was particularly enlightening because our initial vision for the app was a real time assessment tool. However, these stakeholders helped us refine the vision for the app to more of a post match assessment tool. As they explained, it is not uncommon for athletes to shake off signs of concussions as just wear and tear of the sporting event, only to notify ATCs when they haven’t fully recovered over the next 24-48 hours.
The third major value was extending the scope of care. Both the focus group and Eysenbach frame this value in terms of overcoming geographic barriers. Finding times to be available for a teleconference using the mHealth app would be much easier than trying to plan actual trips to each location. Following this path would also help to overcome potential technical hurdles, such as wireless signal strength. If the app helps the health care provider with their scheduling, it would be possible for both the athlete and the ATC to meet at a time where both can ensure strong Internet connections.
The focus group also discussed requirements that they would like to see for how the app operated. The SCAT3 exam is a validated tool, but only when used by properly trained individuals. In order to help keep the evaluation under the control of the medical professionals, it was suggested that the app have different tiers of access. Some of the more technical questions that move beyond the basic capture of the mechanism of injury and who was involved should be handled by the ATC. To accomplish this request, the idea was to have initial screening data that could be entered by a layman (another athlete, a parent, or a coach). That data would be forwarded on to the ATC for them to make the call if the evaluation should continue. These additional conversations helped to outline key values for the end-user of this application. 1) Ease of use. 2) Confidentiality of athlete records. 3) Timely notifications and information retrieval.
The focus group established that the mHealth app should be defined as a success or failure if it could measurably increase the detection of concussions in comparison to events where medical supervision was absent. Although beyond the current scope of the project, the intent is to continue development to reach a point where clinical data can be captured with the app in order to measure this metric.
App concept
The app was built using agile development methods with student developers from the University of Nebraska at Omaha. Agile development cycles were tracked using the web collaboration tool Trello. The initial vision for this app centers on converting the SCAT3 test to a mobile platform. The process flow (Fig. 3) was an output from the focus group session.
Player information can be captured prior to participation in a sporting event, helping expedite the submission process. The SCAT3 has eight primary sections, with additional data entry for mechanisms of injury, athlete background, and signs of concussions. Accessing the system does require log in for any user. Two primary accounts types will be available, a limited access account restricted to data entry and review of their own submitted reports (coach view), and an account with both submission and retrieval access to complete the report reserved for medical professionals (trainer view). A third account type (administrator), will be used to create new users and maintain the sytesm. Once logged in, the layperson can complete three initial sections of the SCAT3. The first section is titled “Potential signs of concussion”, which ask simple yes/no questions for the observer of the injury (e.g., “Any loss of consciousness?”). The second section is the Maddocks Score test25, which helps to identify situational awareness by asking the athlete simply memory tests like “What team did you play last week?”. The final section includes the injured athlete’s background (demographics, any history of concussions, etc.). This data capture is consistent with what information is collected in the Pocket Concussion recognition tool, and this does not require medical expertise.
When complete, a report would then be sent to the database, and notification will be forwarded on to an ATC of its entry. The ATC would then log into the system via the website, retrieve and review the report, and make a decision. At this point, if they decide no further intervention is needed, they can log the report for follow up later and clear the athlete to return to play. Alternatively, they can decide to continue the evaluation, and complete the additional six elements remaining on the SCAT3 test in order to generate a score. Return to play decisions are on a 6-point graduated scale ranging from abstaining from all activity, to allowing light aerobic exercise and incrementally increasing activity levels until culminating at clearance for normal game play5.
The database for the app was developed in PostgresQL and is currently not HIPAA compliant. Prostgres can easily be converted into a MySQL or Miscrosoft SQL database if needed. Before any real patient data can be entered, the app will need to be ported to a more secure platform. Details about this task are addressed in the future work section of the paper. As suggested by the developers, this project was broken in three phases. The first phase was building the core elements of the app for data capture, storage and retrieval between multiple users, which is now complete. The next phase would be porting it over to a secure, HIPAA compliant platform, and the final piece would be the video feed integration, since it would be the most technically challenging, and expensive component.
Evaluation phase
With a useable prototype complete, the app could be shared for feedback from ATCs and athletic training students (individuals who have not yet taken the certification exam). The focus group was invited to review the app and see if it met the three initial key metrics: 1) the app’s ease of use 2) maintaining confidentiality of athlete records 3) timely notifications and information retrieval. Additional users were encouraged to download either an Android or iOS version of the app, build their own test cases, and provide feedback and complete an End-User Computing Satisfaction (EUCS) survey. EUCS is a validated tool designed to evaluate factors impacting user satisfaction, content, format, accuracy, timeliness, and ease of use6. The tool has also been used to evaluate other medical systems26,27.
Conclusions
At this current phase of this project, we have a functional Android, iOS, and web based version of the app. We were able to define the requirements with the insight from the focus group. In addition, the process helped to construct answers to our primary research questions. Funds were not sufficient at this time to construct the videoconferencing element as originally proposed. This was a disappointing development, but as this was our first effort in mHealth app development, learning about cost limitations was an important takeaway. Pricing out bids for app development prior to the focus group session would have avoided this set back. Grant funding will be pursued to cover the additional costs associated with the development of the video component at a later date.
-
Who has a stake in addressing the healthcare problem of concussions?
We were able to provide a detailed list of stakeholders in the results section who have a vested interest in improving detection of concussions. From this list, we identified a primary user base of ATCs working with rural athletes and the coaches of those athletes. Success or failure of this mHealth app would depend on our ability to properly deliver a tool that meets the needs for this group.
-
How can technology contribute to better quality of care and in what manifestation can technology contribute?
By offering a solution that integrates telehealth and mHealth into an already accepted and validated concussion tool, we don’t have to worry about re-inventing the wheel. The augmentation of the SCAT3 will require testing to ensure that the mHealth app works to the same degree as its paper based iteration, but this change offers many advantages. Data capture and retrieval would be improved over the paper versions of the tests. Follow-up on athletes suspected or verified to have a concussion can be simplified and can occur more frequently.
-
Was the design process able to meet user requirements established by the stakeholders and targeted users?
The focus group was satisfied with the progress of the project so far. All three key metrics were deemed satisfactory, although there are noted points for improvement on some “ease of use” elements. This feedback will be incorporated into the next version of the app, which will be shared again with the focus group. Additional data was planned based off the results from the EUCS survey, but delays due to launching the app on Google Play and Apple iTunes prevented us from reaching our goal of 20+ completed surveys. Participation in the survey is still being solicited, and additional iterations of the app will use EUCS to measure progress.
One of the big lessons learned from this project so far has been the transition away from a concept of immediate access to a healthcare professional, toward more of a tool that can facilitate increased contact between the athlete and ATC. By following the CeHRes roadmap, there have been structured guidelines that helped us reach these new insights. Without taking the time to work through these stages, the app development would have most assuredly been built with the focus on sideline interventions. While the tool built with these specifications may have been effective in it is aims and deliver on its goals, adoption of the tool may have never taken off. It is not uncommon for an athlete to suspect something is wrong the day after a concussion, when symptoms have still persisted. As highlighted by the focus group, this app would be beneficial to extend care to those athletes too. There are two suggestions we would provide for enhancing the CeHRes roadmap, an emphasis on budget building/cost analysis and guidance for launching an app on either an Android or iOS platform. Overall, it is a very effective tool, and one recommend by us to others, with the caveat for these two areas. We would emphasize on having a clear handle on building costs before entering the value specification phase of CeHRes. Also, launching our app in beta proved to be a significant hurdle, one that should not be overlooked in planning for a successful mHealth app. The certificate, keys, and profile generation steps required for launching the app on the Apple iTunes store and Google’s Play store has a sizeable learning curve if it is the first time a user is publishing their app. Developer accounts also are required by the user (at the time of publication, $25 for a lifetime license on Android, and $99 per year for Apple’s iOS).
Both the Google Play store and Apple iTunes have mechanisms to run closed and open beta tests. Beta testing via the Google Play store is fairly simple, it is managed from the Google Play Console and only requires users to have a gmail account to participate. Apple beta testing follows a different framework, which should be accounted for in planning for testing phases. Apple uses a program called Testflight for beta tests. Before beginning the beta testing program, the app needs to pass evaluation from Apple, and reviews are targeted to be complete 24-48 hours after submission. Once the app has passed review, beta testers can be added via their Apple ID. Users first need to download the Testflight app. Once their account has been added to the beta testing list, the app will appear inside of the Testflight app. Additional time should be budgeted for this overall process on top of helping beta testers who might not be familiar with the process themselves.
Future work
In April of 2017, the group in charge of SCAT skipped over SCAT4 and released the latest version, SCAT528. We plan on reviewing this latest version and adjusting our app as needed. Additional EUCS survey results will continue to be collected for further feedback on the app. There are three major goals remaining for this project: converting it over to a HIPAA-compliant environments for secure patient data storage (most likely using REDCap29), building the video conferencing component of the app and eventually conducting a randomized control trial study to test the app in the field. Using FaceTime or Skype APIs are the most likely solution, since they offer encryption and security options needed for medical consultations. The purpose would be to evaluate the app’s effectiveness in detecting concussions in practice. We are excited by the stakeholder’s interest when discussing this project and plan on using our prototype to secure additional funding to support future development.
Figure 2.
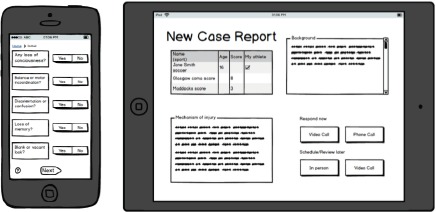
App mock-up screens depicting data entry and data retrieval screens
Figure 3.
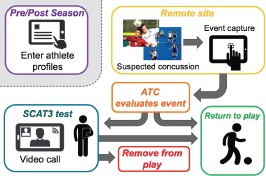
ATC telehealth mHealth app process flow
Figure 4.
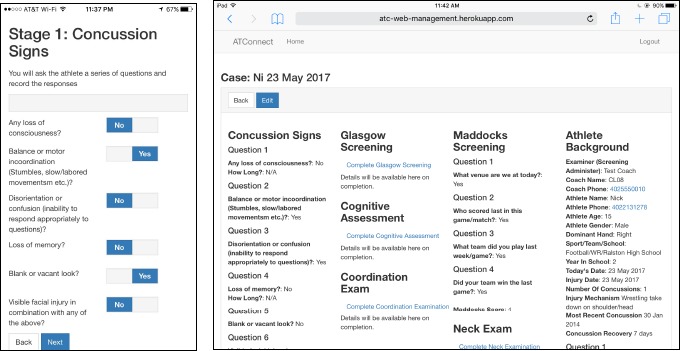
App data capture (via an app on a smart phone) and retrieval screens (via website on a tablet)
References
- 1.Broglio SP, Pontifex MB, O’Connor P, Hillman CH. The persistent effects of concussion on neuroelectric indices of attention. Journal of neurotrauma. 2009;26(9):1463–70. doi: 10.1089/neu.2008.0766. [DOI] [PubMed] [Google Scholar]
- 2.Pryor RR, Casa DJ, Vandermark LW, Stearns RL, Attanasio SM, Fontaine GJ, et al. Athletic training services in public secondary schools: a benchmark study. Journal of athletic training. 2015;50(2):156–62. doi: 10.4085/1062-6050-50.2.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lincoln AE, Caswell SV, Almquist JL, Dunn RE, Norris JB, Hinton RY. Trends in concussion incidence in high school sports a prospective 11-year study. The American journal of sports medicine. 2011;39(5):958–63. doi: 10.1177/0363546510392326. [DOI] [PubMed] [Google Scholar]
- 4.Fletcher EN, McKenzie LB, Comstock RD. Epidemiologic comparison of injured high school basketball athletes reporting to emergency departments and the athletic training setting. Journal of athletic training. 2014;49(3):381. doi: 10.4085/1062-6050-49.3.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCrory P, Meeuwisse WH, Aubry M, Cantu B, Dvorak J, Echemendia RJ, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. British journal of sports medicine. 2013;47(5):250–8. doi: 10.1136/bjsports-2013-092313. [DOI] [PubMed] [Google Scholar]
- 6.Abdinnour - Helm SF, Chaparro BS, Farmer SM. Using the end-user computing satisfaction (EUCS) instrument to measure satisfaction with a web site. Decision Sciences. 2005;36(2):341–64. [Google Scholar]
- 7.Kutcher JS, McCrory P, Davis G, Ptito A, Meeuwisse WH, Broglio SP. What evidence exists for new strategies or technologies in the diagnosis of sports concussion and assessment of recovery? British journal of sports medicine. 2013;47(5):299–303. doi: 10.1136/bjsports-2013-092257. [DOI] [PubMed] [Google Scholar]
- 8.Vargas BB, Shepard M, Hentz JG, Kutyreff C, Hershey LG, Starling AJ. Feasibility and accuracy of teleconcussion for acute evaluation of suspected concussion. Neurology. 2017;88(16):1580–3. doi: 10.1212/WNL.0000000000003841. [DOI] [PubMed] [Google Scholar]
- 9.Lee H, Sullivan SJ, Schneiders AG, Ahmed OH, Balasundaram AP, Williams D, et al. Smartphone and tablet apps for concussion road warriors (team clinicians): a systematic review for practical users. British journal of sports medicine. 2015;49(8):499–505. doi: 10.1136/bjsports-2013-092930. [DOI] [PubMed] [Google Scholar]
- 10.Guskiewicz KM, Register-Mihalik J, McCrory P, McCrea M, Johnston K, Makdissi M, et al. Evidence-based approach to revising the SCAT2: introducing the SCAT3. British journal of sports medicine. 2013;47(5):289–93. doi: 10.1136/bjsports-2013-092225. [DOI] [PubMed] [Google Scholar]
- 11.FLAGS R. Pocket CONCUSSION RECOGNITION TOOL™. 2013 [Google Scholar]
- 12.Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, et al. Use of electronic health records in US hospitals. New England Journal of Medicine. 2009;360(16):1628–38. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 13.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Annals of internal medicine. 2006;144(10):742–52. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 14.Van Velsen L, Wentzel J, Van Gemert-Pijnen JE. Designing eHealth that matters via a multidisciplinary requirements development approach. JMIR research protocols. 2013;2(1):e21. doi: 10.2196/resprot.2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rogers FB, Ricci M, Caputo M, Shackford S, Sartorelli K, Callas P, et al. The use of telemedicine for realtime video consultation between trauma center and community hospital in a rural setting improves early trauma care: preliminary results. Journal of Trauma and Acute Care Surgery. 2001;51(6):1037–41. doi: 10.1097/00005373-200112000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Morland LA, Greene CJ, Rosen CS, Foy D, Reilly P, Shore J, et al. Telemedicine for anger management therapy in a rural population of combat veterans with posttraumatic stress disorder: a randomized noninferiority trial. The Journal of clinical psychiatry. 2010;71(7) 1:478–863. doi: 10.4088/JCP.09m05604blu. [DOI] [PubMed] [Google Scholar]
- 17.Levine SR, Gorman M. “Telestroke” The Application of Telemedicine for Stroke. Stroke. 1999;30(2):464–9. doi: 10.1161/01.str.30.2.464. [DOI] [PubMed] [Google Scholar]
- 18.Demaerschalk BM, Hwang H-M, Leung G. Cost analysis review of stroke centers, telestroke, and rt-PA. The American journal of managed care. 2010;16(7):537–44. [PubMed] [Google Scholar]
- 19.Hess DC, Wang S, Gross H, Nichols FT, Hall CE, Adams RJ. Telestroke: extending stroke expertise into underserved areas. The Lancet Neurology. 2006;5(3):275–8. doi: 10.1016/S1474-4422(06)70377-5. [DOI] [PubMed] [Google Scholar]
- 20.Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in US epidemiologic studies. Journal of Urban Health. 2006;83(2):162–75. doi: 10.1007/s11524-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schwaderer C, Unruh S. Assessment of Emergency Readiness and Delivery of Althetic Healthcare at Nebraska High Schools. National Conference on Undergraduate Research;; 2014 April 3-4; University of Kentucky. [Google Scholar]
- 22.Nijland N. Grounding eHealth: towards a holistic framework for sustainable eHealth technologies: University of Twente. 2011 [Google Scholar]
- 23.van Gemert-Pijnen JE, Nijland N, van Limburg M, Ossebaard HC, Kelders SM, Eysenbach G, et al. A holistic framework to improve the uptake and impact of eHealth technologies. Journal of medical Internet research. 2011;13(4):e111. doi: 10.2196/jmir.1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eysenbach G. What is e-health? J Med Internet Res. 2001;3(2):e20. doi: 10.2196/jmir.3.2.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maddocks DL, Dicker GD, Saling MM. The assessment of orientation following concussion in athletes. Clinical Journal of Sport Medicine. 1995;5(1):32–5. doi: 10.1097/00042752-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Aggelidis VP, Chatzoglou PD. Hospital information systems: Measuring end user computing satisfaction (EUCS) Journal of biomedical informatics. 2012;45(3):566–79. doi: 10.1016/j.jbi.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 27.Ajami S, Mohammadi-Bertiani Z. Training and its impact on hospital information system (HIS) success. Journal of Information Technology & Software Engin. 2013;2012 [Google Scholar]
- 28.Echemendia RJ, Meeuwisse W, McCrory P, Davis GA, Putukian M, Leddy J, et al. The Sport Concussion Assessment Tool 5th Edition (SCAT5) Br J Sports Med. 2017 doi: 10.1136/bjsports-2017-097506. bjsports-2017-097506. [DOI] [PubMed] [Google Scholar]
- 29.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]


