Abstract
Patient socioeconomic data is not usually included in medical records nor easily accessible to clinicians, yet socioeconomic disadvantage can be an important guide to disease management. This study evaluated the neighborhood-level Area Deprivation Index (ADI), a measure of neighborhood socioeconomic disadvantage, as a factor in diabetes mellitus prevalence. Electronic health records at an academic hospital system identified 4,770 Medicare beneficiaries. Logistic regression of diabetes diagnosis (ICD9=250.x) against ADI quintile, age, gender, and race/ethnicity found all these patient characteristics to be significantly associated. Diabetes prevalence was lowest in the least disadvantaged quintile of neighborhoods after adjusting for age, gender, and race/ethnicity. The positive non-linear association of diabetes prevalence with ADI demonstrates the power of this index to practically quantify socioeconomic disadvantage. The ADI may be suitable for clinical decision support, and for informing the policy changes which are needed to reduce socioeconomic disparities in diabetes prevalence and other health outcomes.
Introduction
Epidemiological significance of diabetes mellitus
One twelfth of the world’s population has diabetes mellitus, including 10.8% of Americans1. In the United States (US) alone, diagnosed diabetes costs $176 billion annually in direct medical costs and another $69 billion annually in decreased productivity2. Diabetes incidence rates are rising, with 1.9 million US adults newly diagnosed with diabetes in 20103.
Education, occupation and income are independently associated with a 25-30% decreased risk of type 2 diabetes4. Lower subjective social status (the individual’s perception of his or her position in the social hierarchy) is also associated with increased risk of diabetes5, as are depression6 and lower self-efficacy and social support7.
Prevalence of the disease varies by ethnic group8, but disparities are more strongly associated with socioeconomic status than with race or ethnicity9. The least well-off suffer a disproportionate share of the burden of diabetes10, and children who live in poverty are more likely to develop type II diabetes as adults and more likely to die from it earlier11,12. The association between socioeconomic status and diabetes mellitus is worldwide, in low-income countries as well as high-income countries13.
Limitations of existing approaches
Clinicians need additional training and tools to assess and respond to social determinants of health at the point of care14. However, because patient income and education are often not part of the medical record, nor often discussed directly during care delivery, clinicians must infer socioeconomic status from available data, such as patient neighborhood of residence. The Area Deprivation Index (ADI), is a geographic, area-based measure of the socioeconomic deprivation to which census-defined neighborhoods (i.e. census block groups) are exposed15. Addition of this socioeconomic risk factor to more traditional individual-level clinical data such as age, gender, and race/ethnicity could improve the understanding of diabetes risks in individual patients and patient populations.
Objective of the current study
The objective of this study was to develop and evaluate a clinically useful tool for more practically identifying the social determinants which impact diabetes prevalence in a patient population.
Methods
Study population and setting
The study population comprised 4,770 primary-care patients16 at the University of Missouri who were 65 years or older and enrolled in Medicare (US federal health insurance for the elderly and disabled17) on September 1, 2014. All patient diagnoses, demographics, and other clinical attributes were retrieved from University of Missouri Health System medical records.
Data collection
This study used an updated and refined 2013 ADI developed by the University of Wisconsin School of Medicine and Public Health15 (AJK18). This 2013 ADI uses data from the 2009-2013 American Community Survey19 to construct a factor-based ADI score from 17 census block-group level markers of socioeconomic status for each neighborhood of interest (Table 1).
Table 1.
Components of the Area Deprivation Index (ADI)
| Area Socioeconomic Disadvantage Measure |
|---|
| Percent of the population aged 25 and older with less than 9 years of education |
| Percent of the population aged 25 and older with at least a high school diploma |
| Percent employed persons aged 16 and older in white-collar occupations |
| Median family income in US dollars |
| Income disparity |
| Median home value in US dollars |
| Median gross rent in US dollars |
| Median monthly mortgage in US dollars |
| Percent of owner-occupied housing units |
| Percent of civilian labor force population aged 16 years and older who are unemployed |
| Percent of families below federal poverty level |
| Percent of the population below 150% of the federal poverty threshold |
| Percent of single-parent households with children less than 18 years of age |
| Percent of households without a motor vehicle |
| Percent of households without a telephone |
| Percent of occupied housing units without complete plumbing |
| Percent of households with more than 1 person per room |
Because the ADI is an index rather than a concrete measure such as income or percent of households, it is not associated with a defined unit of measure. Differences between index values must be interpreted in relation to the range of index values in the data set. For these reasons, the possible ADI scores for Missouri were calculated for each Census block group and grouped into quintiles, with both the ADI score and the ADI quintile assigned to each member of the study population. Figure 1 shows the resulting map of ADI quintiles for the state of Missouri.
Figure 1.
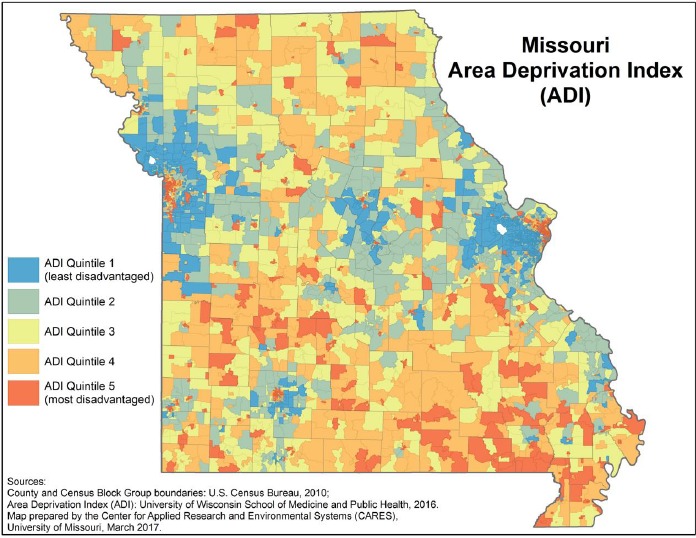
Missouri Area Deprivation Index (ADI) quintile by Census Block Group.
Statistical methodology
Diabetes mellitus, the outcome of interest, was defined as the presence of any 250.x ICD-9 code in a patient’s EHR record. Because that outcome is a binary categorical value (either present or absent), logistic regression was used to test the association between ADI and diabetes, adjusting for patient age, gender, and race. Diagnostic plots of the empirical log-odds of diabetes against ADI quintiles indicated that relationship is not linear, and so ADI was treated as a nominal scale variable. Integer age in years was treated as a continuous variable. Gender was treated as a categorical variable, with “female” and “male” being the only two values recorded for this study population. Race/ethnicity was also treated as a categorical variable with two values, “White/Non-Hispanic”, and “Other”. The data source included eight possible values for race/ethnicity, but because the “White/Non-Hispanic” category included 88% of the study population, all other categories (“American Indian or Alaskan Native”, “Asian”, “Black or African American”, “Hispanic”, “Native Hawaiian or other Pacific Islander”, “Other race”, and “Unknown race”) were reclassified as “Other”.
Results
All the variables tested were found to be statistically significant with p < 0.05, as shown in Table 2.
Table 2.
Analysis of effects on diabetes prevalence in the multivariate logistic regression model
| Effect | Odds Ratio | Pr > Chi-Square |
|---|---|---|
| Intercept | -- | 0.0191* |
| ADI quintile 1 (least disadvantaged) | 1.37 | <0001*** |
| Age (integer years) | 0.99 | 0.0003*** |
| Gender (female) | 0.81 | 0.0011** |
| Race/ethnicity (White/Non-Hispanic) | 0.44 | <0001*** |
* p<0.05, ** p<0.01, *** p<0.001
A graphic visualization of the percent of patients with diabetes mellitus (DM) within each ADI quintile (see Figure 2) clearly shows a positive but non-linear association of increasing DM prevalence (ranging from less than 25% to more than 35% in the study population) with increasing ADI (i.e., increasing neighborhood deprivation,).
Figure 2.
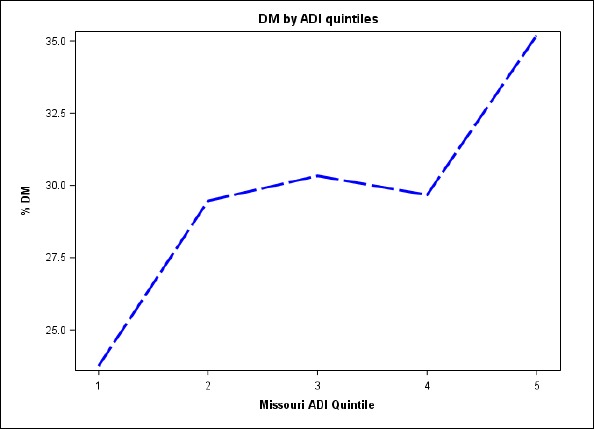
Percent of patients with diabetes mellitus (DM) by Area Deprivation Index (ADI) quintile within Missouri
Figure 2 shows visible differences in diabetes prevalence between patients from the least disadvantage neighborhoods (quintile 1), from the most disadvantaged neighborhoods (quintile 5), and from neighborhoods in the middle (quintiles 2-4). However, pairwise comparison of the five quintiles found statistical differences only between quintile 1 and all other quintiles, as shown in the Table 3.
Table 3.
Analysis of effects in the logistic regression model
| ADI Quintile Comparison | Odds Ratio | Pr > |t| |
|---|---|---|
| 1 v 2 | 1.3198 | 0.0013** |
| 1 v 3 | 1.3461 | 0.0012** |
| 1 v 4 | 1.2928 | 0.0171* |
| 1 v 5 | 1.3886 | 0.0261* |
| 2 v 3 | 0.9804 | 0.8307 |
| 2 v 4 | 1.0208 | 0.8487 |
| 2 v 5 | 0.9505 | 0.7304 |
| 3 v 4 | 1.0412 | 0.7176 |
| 3 v 5 | 0.9694 | 0.8355 |
| 4 v 5 | 0.9311 | 0.6532 |
* p<0.05, ** p<0.01
The low statistical significance of the apparent increase in diabetes prevalence for quintile 5 may be partly due to the relatively small sample size of this quintile, comprising only 5.7% of the study population. This limits power significantly.
Discussion
Fulfillment of study objective
The positive non-linear association of diabetes mellitus prevalence with neighborhood disadvantage, as measured by the Area Deprivation Index (ADI), indicates that ADI could be a useful tool for converting patient address into a significant predictor of diabetes prevalence in a patient population.
Additional findings
In this study population, the prevalence of diabetes in the least disadvantaged neighborhoods (ADI quintile 1) is significantly lower than all other neighborhood quintiles after adjusting for age, gender, and race/ethnicity. Quintiles 2 through 5 were not statistically different. The statistical equivalence of quintile 5 with quintiles 2 through 4 may be due to relatively small size of quintile 5, or may show an approximate equivalence between diabetes prevalence at moderate and high levels of neighborhood socioeconomic disadvantage.
Limitations of the current study
Because the study was limited to a single academic health center in mid-Missouri, and to Medicare enrollees over 65 years of age, these results may not be generalizable to other populations. Because nearly 90% of the study population was non-Hispanic White, the important characteristics of race and ethnicity may not adequately tested by this study. Furthermore, as previously stated, relatively small sample size in the most disadvantaged neighborhood quintile limits our statistical power and our ability to draw conclusion for this group.
Directions for future research
Repeating this study with a larger patient population, and with a population sample more representative of the entire US, may add to the understanding on how neighborhood disadvantage by ADI could be harnessed in diabetes care and population health efforts.
Conclusion
This study demonstrates the power of the Area Deprivation Index (ADI) to quantify neighborhood socioeconomic deprivation into a single index for use in predictive analytics. The ADI may be suitable for clinical decision support, as well as for informing the policy changes which are needed to reduce socioeconomic disparities in diabetes prevalence and other health outcomes. In addition to confirming the existing literature in finding an association between neighborhood socioeconomic deprivation and the prevalence of diabetes mellitus, this application of the ADI adds new findings to our understanding of health disparities. Most strikingly, the association of neighborhood socioeconomics with good health was strong in this population only for those residing within the highest levels of privileged neighborhoods; middle-class neighborhood status granted no measurable protection from the diabetes health disparities that affected residents of the poorest and least privileged neighborhoods. Clinicians and population health managers armed with a simple and unobtrusive measure of neighborhood socioeconomic status, based not on private financial data but simply on patient address, may be able to more effectively screen for, prevent, and manage diabetes in individual patients and managed populations. This is an important idea worthy of future research and study.
Acknowledgements
This work was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number R01MD010243 (PI: Amy Kind).
References
- 1.The World Bank. Diabetes prevalence (% of population ages 20 to 79) [Internet]. Diabetes prevalence (% of population ages 20 to 79) | Data. The World Bank Group; 2016 [cited 2017Feb28] Available from: http://data.worldbank.org/indicator/SH.STA.DIAB.ZS?end=2015&name_desc=true&start=2015&view=bar.
- 2.Centers for Disease Control and Prevention. Chronic Disease Overview [Internet]. Chronic Disease Overview. Centers for Disease Control and Prevention; 2016 [cited 2017Feb28] Available from: https://www.cdc.gov/chronicdisease/overview/index.htm.
- 3.Centers for Disease Control and Prevention. Atlanta, GA: U.S National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States; 2011. Department of Health and Human Services, Centers for Disease Control and Prevention. 2011. [Google Scholar]
- 4.Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011 Jun;40(3):804–18. doi: 10.1093/ije/dyr029. [DOI] [PubMed] [Google Scholar]
- 5.Tang KL, Rashid R, Godley J, Ghali WA. Association between subjective social status and cardiovascular disease and cardiovascular risk factors: a systematic review and meta-analysis. BMJ Open. 2016 Mar 18;6(3):e010137. doi: 10.1136/bmjopen-2015-010137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Egede LE, Bishu KG, Walker RJ, Dismuke CE. Impact of diagnosed depression on healthcare costs in adults with and without diabetes: United States. J Affect Disord. 2016 May;195:119–26. doi: 10.1016/j.jad.2016.02.011. 2004-2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walker RJ, Smalls BL, Egede LE. Social determinants of health in adults with type 2 diabetes--Contribution of mutable and immutable factors. Diabetes Res Clin Pract. 2015 Nov;110(2):193–201. doi: 10.1016/j.diabres.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oldroyd J, Banerjee M, Heald A, Cruickshank K. Diabetes and ethnic minorities. Postgrad Med J. 2005 Aug;81(958):486–90. doi: 10.1136/pgmj.2004.029124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karlamangla AS, Merkin SS, Crimmins EM, Seeman TE. Socioeconomic and ethnic disparities in cardiovascular risk in the United States. Ann Epidemiol. 2010 Aug;20(8):617–28. doi: 10.1016/j.annepidem.2010.05.003. 2001-2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Everson SA, Maty SC, Lynch JW, Kaplan GA. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. J Psychosom Res. 2002 Oct;53(4):891–5. doi: 10.1016/s0022-3999(02)00303-3. [DOI] [PubMed] [Google Scholar]
- 11.Raphael D. Poverty in childhood and adverse health outcomes in adulthood. Maturitas. 2011 May;69(1):22–6. doi: 10.1016/j.maturitas.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 12.Tamayo T, Christian H, Rathmann W. Impact of early psychosocial factors (childhood socioeconomic factors and adversities) on future risk of type 2 diabetes, metabolic disturbances and obesity: a systematic review. BMC Public Health. 2010 Sep 1;10:525. doi: 10.1186/1471-2458-10-525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leone T, Coast E, Narayanan S, de Graft Aikins A. Diabetes and depression comorbidity and socio-economic status in low and middle income countries (LMICs): a mapping of the evidence. Global Health. 2012 Nov 26;8:39. doi: 10.1186/1744-8603-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walker RJ, Strom Williams J, Egede LE. Influence of race, ethnicity and social determinants of health on diabetes outcomes. Am J Med Sci. 2016 Apr;351(4):366–73. doi: 10.1016/j.amjms.2016.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kind AJ, Jencks S, Brock J, Yu M, Bartels C, Ehlenbach W, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: A retrospective cohort study. Ann Intern Med. 2014;161:765–774. doi: 10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Popejoy LL, Jaddoo J, Sherman J, Howk C, Nguyen R, Parker JC. Monitoring Resource Utilization in a Health Care Coordination Program. Prof Case Manag. 2015 Nov-Dec;20(6):310–20. doi: 10.1097/NCM.0000000000000120. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Medicare and Medicaid Services. What’s Medicare [Internet]. What’s Medicare. Centers for Medicare and Medicaid Services; 2016 [cited 2017Feb28] Available from: https://www.medicare.gov/sign-up-change-plans/decide-how-to-get-medicare/whats-medicare/what-is-medicare.html.
- 18.For additional information on the ADI or to access ADI data sets, please contact Amy Kind, MD, PhD. at the University of Wisconsin School of Medicine and Public Health. at ajk@medicine.wisc.edu.
- 19.United States Census Bureau. American Community Survey (ACS) [Internet]. American Community Survey (ACS). US Department of Commerce; 2016 [cited 2017Feb28]. Available from: https://www.census.gov/programs-surveys/acs/


