Abstract
For patients with breast cancer who must frequent medical centers for care, commuting is a significant burden. This burden could affect their decisions during treatment. We developed a method to use census tracts and zip codes to determine commuting burden for patients with breast cancer with online mapping services, while protecting patient addresses from third parties. We found that patients who lived farther from Vanderbilt had fewer unique appointment days and more appointments scheduled per day. Total burden decreased over time after diagnosis, but advanced stage patients had sustained high levels of commute time until ten months after diagnosis. Additionally, we found that patients who lived far from Vanderbilt were less likely to receive radiotherapy from Vanderbilt. With the amount of work patients put into traveling for care, understanding commuting burden could help healthcare organizations form strategies to improve access to care and compliance with care plans.
Introduction
Traveling to and from a medical center for treatment is a significant burden to many patients with chronic conditions. In 2014, The Center for Disease Control and Prevention showed that 67% of adults in the United States had at least one encounter with the healthcare system within 6 months of the survey1. The percentage of patients who saw a healthcare provider increases significantly for patients with chronic conditions. In 2013, 99% of patients with hypertension had an office-based physician visit and 47% had four or more visits2. Similarly, 55% of patients with diabetes visited a physician four or more times in a year3. Elderly patients, who often have difficulty traveling for care4, had to travel more frequently than the average patient1. In addition to the sheer number of times patients must travel to medical centers for care, patients also perceive commuting as a burden. In a survey of 1053 patients regarding factors that contributed to their treatment burden, 41% expressed that they had difficulty adapting to new routines for care that involved planning and organizing travel5. Additionally, 30% of patients surveyed indicated they had difficulty with access to health care centers citing distance and parking as barriers to receiving care. Interest in treatment burden goes beyond just providing convenient care for patients. Patients who receive care within their means and are not overburdened tend to be more compliant with their treatment plans6 which could lead to better outcomes.
Breast cancer patients experience a high level of treatment burden. In our prior work, we demonstrated that stage I- III breast cancer patients receiving care at Vanderbilt underwent an average of 59 appointments over the course of 18 months after their diagnosis7. During this time, these patients had to travel to the medical center an average of 39 times and spent approximately 49 hours in clinic. Stage III patients experienced the most time in clinic, followed by stage II and stage I patients. One reason for the intensity of treatment burden in breast cancer patients is the complexity of their treatment. Encounters included radiology diagnostics, laboratory tests, surgery, radiation therapy, and chemotherapy. Furthermore, many patients experienced additional treatment burden due to complications to their care that led to hospitalizations or the need for physical therapy.
Traveling for care is a challenge for cancer patients, particularly those living far from metropolitan areas8. Travel also contributes to the burden of treatment through transportation costs. An Australian study showed that the median cancer patient spent 956 Australian dollars (about 727 US dollars) in travel costs over 16 months after diagnosis, which accounted for 71% of all out-of-pocket costs9. Distance traveled could even affect patient treatment choices. One study determined that driving distance from a radiotherapy facility resulted in more patients with breast cancer choosing mastectomy instead of breast conserving surgery10. While our previous studies looked at burden of treatment due to time spent in inpatient and outpatient encounters, we did not factor in the work patients put into traveling to the medical center for those encounters. The goal of this study was to use web services to calculate commuting burden over the course of treatment for patients with breast cancer.
In addition to the duration of the commute to the medical center, the mode of transportation could also be a factor that healthcare providers should consider. Researchers demonstrated United States counties11 and English districts12 where more households had access to a car had a higher rate of screening for cervical cancer. Conversely, breast cancer screening was lower in English districts with higher public transportation usage. While public transportation may be less convenient for patients receiving care for cancer, it may be some patients’ only option. While we assume that most patients who receive care at Vanderbilt arrive by car, we will explore the possibility of commuting by public transportation for our population of breast cancer patients.
Healthcare researchers have used mapping web services to improve the delivery of care. One group from the Netherlands used Google Maps to calculate the difference between driving time and helicopter flight time to help paramedics decide the most effective way to transport patients to the hospital13. Services such as Google Maps are excellent at keeping up with changing traffic patterns and new roads that may affect commute times both for driving and public transportation. However, one challenge with using online services in healthcare delivery and research is that sending patient addresses to companies without a Business Associate Agreement (BAA) is a violation of the Health Information Portability and Accountability Act (HIPAA) privacy rules14. Additionally, the American Journal of Public Health released an editorial stating that sending patient addresses to a third party is inappropriate and that some method of geographic imputation should be used to protect patient privacy15. In our calculations of work due to travel burden, we propose a method of geographic imputation using zip codes, census blocks, and bus stops as landmarks to protect personally identifiable information (PII).
Methods
2.1. Validating the Landmarks Method
Our landmarks method is similar to aggregation techniques in public health to anonymize locations16. First, we obtained all zip codes and census tract centroid coordinates publically available on the US Census Bureau website17. Nashville Metropolitan Transit Authority (MTA) granted us access to their application program interface (API) where we could pull the list of bus stops and their coordinates. We queried the Google Maps API (Gmaps) for driving times from every landmark to the Vanderbilt University Medical Center (VUMC) and back. Next, we used the Data Science Toolkit (DSTK) geocoder 18 to determine the latitude-longitude coordinates for each of our patient addresses. The DSTK also returns a confidence level for how sure it is that the address is geocoded correctly. We installed the DSTK on virtual machine that ran on a local Vanderbilt computer, thus eliminating the need to send patient addresses to a third party.
To test this method, and to compare the accuracy of the various landmark sets (zip code, census tract, and bus stops), we applied the procedure to a set of homes for sale in the Nashville area. We queried 500 random and publically available addresses from the Redfin.com real estate listing website on January 30, 2017. Then we compared the coordinates given by the DSTK geocoder with those given by the Gmaps geocoder. Based on the agreement between the DSTK and Gmaps geocoders, we determined a DSTK confidence threshold below which we would not trust. We queried Gmaps for driving times for each of the 500 real estate addresses and compared those to the driving times of each addresses’ respective closest landmark.
2.2. Applying the Landmarks Method to Breast Cancer Patient Commutes
After testing the method on the 500 real estate addresses, we applied the best landmark set on a cohort of breast cancer patients obtained from the Vanderbilt Tumor Registry. We included patients with stage I-III breast cancer diagnosed from January 1, 1998 to June 1, 2014. To capture only patients who received most of their first course of treatment at Vanderbilt, we only included patients who had at least three appointments each with a medical oncologist and oncology surgeon. We compared commute times for patients who lived within 100 miles of the main VUMC campus. Patient commute time for any given appointment day was the time it took to drive a round trip from the landmark closest to their home address to the Vanderbilt facility where their appointment was held. To get a characterization of the total burden of traveling, we calculated the total amount of time patients would have to spend traveling to the medical center by car over 18 months after their date of diagnosis. We also compared the behavior of commuting in patients that were farther than the median distance from VUMC with those which were closer than the median distance. We compared the frequency that patients received radiation therapy at a Vanderbilt facility between patients who were closer and those who were farther. With the coordinates of bus stops in Nashville, we analyzed the number of patients that could have feasibly traveled to their appointments via public transportation. Finally, using average commute times, we estimated the cost of commuting per patient. Assuming an average speed of driving in Nashville of 32.4 miles per hour obtained from Google traffic data19, and a cost of operating a vehicle of 54 cents per mile in 2016, we extrapolated the average total cost of commuting by vehicle per patient. A more accurate method would have been to use direct driving distance based on the Gmaps recommended route. However, due to Gmaps query constraints, we inferred the driving distance using average driving speed. The cost per mile comes from the Internal Revenue Service, which sets mileage rates for the cost of operating a passenger vehicle for charitable and medical purposes20.
Results
Among the 500 random real estate addresses obtained from Redfin.com, the DSTK geocoder found 495 latitude- longitude coordinates compared to the Gmaps geocoder which found 483. There was generally good agreement between the coordinates found by DSTK and those found by Gmaps. Among the 425 addresses that were found by both the DSTK and Gmaps, 418 had less than a quarter mile straight-line difference between the DSTK and Gmaps coordinates. To exclude addresses that had major disagreement between DSTK and Gmaps, we only verified landmark driving times for addresses where the DSTK geocoder had at least 80% confidence. DSTK geocoded 427 addresses with at least 80% confidence.
For the addresses found by the DSTK with greater than 80% confidence, we compared driving time to VUMC using the true address and the nearest landmark. Figure 2 shows the difference in round trip driving time as calculated by Gmaps using the true address versus using the zip code centroid, census tract centroid, and nearest bus stop coordinates. Using zip codes in place of true addresses tended to overestimate driving time when the true address was close to VUMC and tended to underestimate driving time when the address was farther away. The difference in estimation time was greater than 20 minutes in some circumstances. With census tracts and bus stops, the difference in times compared to the true addresses was generally less than 10 minutes. Differences between bus stop and true address driving times increased as the distance from VUMC increased.
Figure 2.
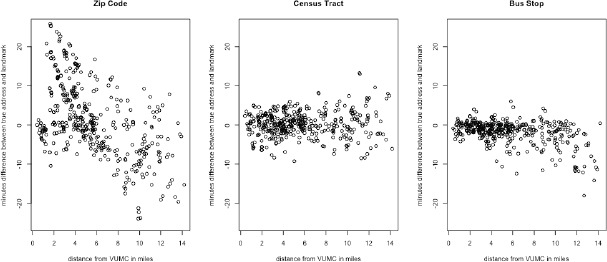
Differences in round trip driving time to VUMC between real estate addresses and nearest zip codes, census tracts, and bus stops.
For our study of commuting burden in breast cancer patients, we used the nearest census track centroid to calculate driving times. The census tract method was more generalizable and robust for addresses far from VUMC than the bus stop method. We used zip codes for patient addresses where the geocoder had less than 80% confidence. There were 768 patient addresses within 100 miles of the main VUMC campus. Among those, we used the nearest census tract to calculate commute time for 644 patients, and used zip code for 124 patients.
The distribution of patients within 100 miles by stage was similar to the overall distribution for all stage I-III patients. There were 374 stage I patients, 273 stage II patients, and 121 stage III patients within 100 miles of the main VUMC campus. Among these patients, there was not much differentiation between stages in the distribution of a single round trip driving time from VUMC. The median driving time to and from VUMC across all stages was 76 minutes and the median straight-line distance from VUMC was 20 miles.
Figure 6 shows that overall burden, consisting of the sum of time in appointments, waiting time between appointments, and driving time, decreased for patients of all stages over the course of 18 months after diagnosis. Stage I and II patients saw peaks in overall burden in the first and fourth months. Overall time spent on encounters reached about 14 hours per month for stage I patients and 15 hours for stage II patients. Stage III patients had more sustained burden through the first eight months of treatment with a peak of seven hours of commute time in month eight.
Figure 6.
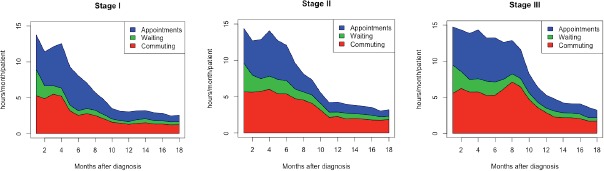
Hours spent in appointments, waiting, and commuting over 18 months after diagnosis by breast cancer stage.
In Figure 7, there is clear differentiation in the number of unique appointment days over 18 months between patients who lived closer and farther than the median distance from VUMC. Patients who lived farther made fewer trips to a Vanderbilt facility compared to their closer counterparts in all three stages. Figure 8 shows that patients farther away also had more appointments per trip to a Vanderbilt facility across all stages.
Figure 7.
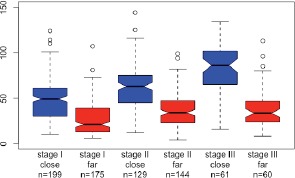
Distribution of unique appointment days over 18 months for patients closer (within 20 miles) and farther (greater than 20 but less than 100 miles) from VUMC by stage.
Figure 8.
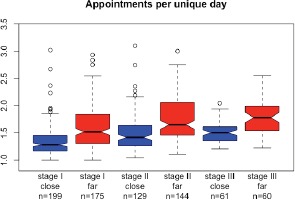
Distribution of mean number appointment per unique appointment day per patient by stage and distance from VUMC.
The percentage of patients who received radiation therapy at Vanderbilt could be indicative of how commute time affected where patients decided to receive care. Table 1 shows the percentage of patients who received radiotherapy at a Vanderbilt facility compared to all patients in that group. Assuming patients within each stage required radiation therapy at approximately the same rate, stage I and stage II patients who lived closer to VUMC received radiation therapy at Vanderbilt at a rate about three times higher than those who lived farther. Stage III patients close to VUMC received radiation therapy at Vanderbilt at a rate five times higher.
Table 1.
Percentage of patients who received radiotherapy at a Vanderbilt facility by stage and distance from VUMC.
| Close (within 20 miles) | Far (>20 and <100 miles) | |
|---|---|---|
| Stage I | 46% | 17% |
| Stage II | 44% | 14% |
| Stage III | 78% | 15% |
For our cohort of patients, 97.5% of appointments take place at facilities accessible by public transportation. However, Table 2 shows how many patients could access public transportation at various walking tolerances, and the percentage of accessible appointments accounted for by those patients.
Table 2.
Number of patients within walking distance of a bus stop at various walking tolerances.
| Patient address distance from bus stop | Patients | % of all appointments accessible |
|---|---|---|
| 100 yards | 25 | 4.52% |
| 200 yards | 49 | 8.26% |
| .25 miles | 124 | 20.2% |
| .5 miles | 171 | 27.4% |
| 1 mile | 223 | 36.2% |
| 2 miles | 263 | 42.2% |
Finally, we performed a cost analysis based on our calculated driving times. As expected, patients closer and with lower stage had less estimated cost of commuting by motor vehicle.
Discussion
Through our attempt to calculate the burden of treatment related to commuting for patients with breast cancer, we succeeded in developing a method for calculating driving times using online mapping services that did not compromise patient PII. When deciding what type of landmark to use in our method, we decided to use a mixture of census block and zip code centroids instead of bus stop coordinates. While Figure 2 shows that bus stops are somewhat more accurate than census blocks for the real estate addresses, the accuracy gets worse the farther the address is from the city center. This effect may be because bus stops fall along major roads which become farther apart in suburban and rural areas. Additionally, since not all cities have a public transportation system, using census tracts and zip codes makes our method more generalizable.
Geomasking methods such as random perturbation or donut masking attempt to hide patient addresses by randomly moving the patient address in a radius around the true address16. These methods of protecting PII have the potential to be more accurate than our landmarks method since the size of the radius is dependent on the population density around the patient’s location. We did not consider using one of these methods since they each require the researcher to define a level of k-anonymity, which is the minimum number of people from which any research subject could be re-identified from21. It is difficult to define such a k-anonymity level that would be necessary to protect patients from an internet service. However unlikely, Google could easily target cancer treatment relevant advertisements to hundreds of people for the 1/k chance that the cancer patient in the area would receive the advertisement. Additionally, geomasking may be more useful in public health studies where spatial precision is necessary to identify sources of outbreaks22, but is less essential for calculating estimated driving times. As demonstrated from the comparison of commute times between true real estate addresses and census blocks, there is only a small effect on the overall commute time.
One major constraint in using online mapping services such as Google Maps for calculating driving distances is that there is a limit on the number of free requests per user. In early 2017 when we performed this study, Google Maps allowed users to make 2,500 free requests per day, with requests over that quota costing $0.50 per 1000 queries23. In order to maintain full de-identification for PII, we had to request driving times from every census tract and zip code centroid to every Vanderbilt location. The constraint of request quotas limited the scope of this project in several ways. Including only patients within 100 miles of Vanderbilt is reasonable since patients who live farther away may not commute daily from home. However, anecdotally, we have seen that patients who live as far as 200 miles away are driving from their homes to Vanderbilt for care. Our method included the 829 census tracts within 100 miles ofVUMC, which could be queried for one Vanderbilt location in one day. This number jumps to 3639 census tracts within 200 miles which would require three days of free queries per Vanderbilt location (driving times to and from a location count as two requests). As we build a database of driving times, future work will include patient addresses that are farther away.
Another interesting question that we could answer with more Google Maps queries is the effect of traffic on patient commute times. One of the reasons we chose not to use open source projects such as the Open Source Routing Machine (OSRM) is because they do not have the means to collect live traffic information. Geographic Information System (GIS) software such as ArcGIS has a live traffic feed available, but only through a paid subscription. One powerful feature of modern web mapping applications is that they track typical traffic patterns to provide driving time predictions that factor in road congestion. However, ten of the census tracts within 100 miles of VUMC had fewer than 20 people living in them according to the 2010 census. The presence of low population census tracts means we would have to query every census tract for every appointment time in order to achieve full anonymity, which would become expensive to do with Google Maps. Future work could gradually save hourly driving times with traffic data to get an idea for how much traffic affects the work patients put into their care. Alternatively, we may establish a BAA with Google or another company that provides live driving time predictions.
Despite the limitations, we made several observations about the effect of commute time on cancer treatment. Aside from confirming that stage III patients experienced a higher treatment burden than stage II and stage I patients, we observed in Figure 6 that the pattern in commute time over months after diagnosis was different for stage III patients. Stage III patients experienced increased commute times in months six through eight after diagnosis despite a decrease in appointment time during that period. This increased commute time, coupled with the decrease in appointment and waiting time, may be associated with the observation that many stage III patients underwent radiation therapy after surgery. Radiation therapy procedures are typically 15 minute appointments that occur daily in rapid succession. The fact that these encounters are short but still require patients to travel to the medical center could explain the increase in commute time relative to appointment time.
Table 1 showed that patients farther from Vanderbilt received radiation therapy less often at Vanderbilt than their counterparts that lived closer. The rate that patients received radiation therapy may be high overall due to our cohort already being biased toward patients who received a majority of their care at Vanderbilt with the constraint that all patients have at least three appointments with a medical oncologist and oncology surgeon. If we assume that patients of a given stage of breast cancer require radiation therapy at approximately the same rate, then we can conclude that more patients who live farther from Vanderbilt are getting radiation therapy at other institutions. This finding supports the conclusion of Goyal et. al. that driving distance to a radiation therapy center influences breast cancer patients’ treatment path decisions10. This type of information would be useful to healthcare organizations that are considering opening new radiation therapy clinics. If a new clinic knew that patients are three to five times more likely to choose to receive radiation therapy at Vanderbilt with a more convenient location, the clinic could plan capacity to meet that demand.
In discussing patient experience for commuting, one important consideration is determining patient capacity to handle a long trip to the doctor. In cities such as Nashville where a typical commute to work was more than 30 minutes in 201424, medical centers may be able to expect patients travel farther for care. However, in a city where traffic is less onerous, patients may be more sensitive to commuting long distances to a medical center regularly. Nevertheless, our calculated round trip to VUMC for the median patient was 76 minutes. This result means that even without traffic, the median patient within 100 miles of VUMC would have to drive longer than the average work commuter during rush hour.
Figures 7 and 8 have implications for care coordination in patients with cancer. The fact that patients within each stage who were farther from VUMC had fewer unique appointment days and more days per appointment suggest that some effort is being made to coordinate appointments to occur on the same day for patients who live farther away. While it may be hard to determine whether the patient or medical center staff is putting in the coordination effort, being able to track outpatient appointment coordination allows organizations to identify areas for improvement. It might be prudent for patient care coordinators or navigators to examine upward outliers in Figure 8 to see what strategies are working for patients who average more than three appointments per visit.
There are several assumptions we made in in our study. First, we assumed that patient addresses in the tumor registry were accurate at the time of their diagnosis, and that patients did not move during the first 18 months of treatment. We also assumed that patients traveled from their home address each unique appointment day. It is possible that patients stayed in hotels or with relatives during the more intense parts of their treatment, which would cut down on burden related to commuting. It is also possible that the patient traveled to VUMC from their work address. There were some locations listed in the appointment record that were not primary Vanderbilt locations and thus, we did not have driving time data for them. These appointments were excluded from our analysis. Only one patient had more than 7 appointments at a non-Vanderbilt listed location. That patient still received 89% of their appointments at a Vanderbilt facility and so the influence of this outlier should negligible.
With regards to public transportation in patient commuting, the main takeaway from Table 2 is that only a small proportion of Vanderbilt’s breast cancer population would be able to take advantage of public transportation. Even if patients were willing to walk two miles to their nearest bus stop, only 263 patients would have access to public transportation. Future work might consider what is the maximum reasonable distance to expect patients with different conditions such as cancer to walk before and after their appointments. Additionally, it would be interesting to see whether there is improved access to healthcare facilities via public transportation in more densely populated cities.
Healthcare organizations could also use this method to predict patient commute times on the day of patients’ appointment. These predictions can be used to warn patients who may need to leave their homes earlier in order to avoid traffic, or to anticipate which patients may be late due to abnormal traffic conditions. Informaticians can also use calculations of commuting burden to develop tools that benefit patients. Providing patients with a mobile application to automatically calculate travel time to appointments would require consent to track their locations. However, such an application could help to alert patients of when they should leave their homes to arrive at their appointments on time. With real-time traffic conditions integrated with the appointment record, an online navigation service could recommend a driving route that avoids traffic and minimizes commuting burden.
Finally, being able to track work related to driving could also allow organizations to identify patients who may be overburdened. For example, patients who are high outliers for overall burden from appointments and procedures may benefit from a home visit from a nurse in lieu of outpatient appointment. In addition to the time requirements of cancer care, financial costs for cancer patients may lead to extreme financial distress and worse outcomes, a phenomenon known as financial toxicity25. Foundations such as Susan G. Komen provide support to breast cancer patients who have difficulty affording their care26. One of the programs provides financial relief to qualified breast cancer patients by giving them gas card vouchers. A healthcare organization could use information from T able 3 to request a grant from the Komen Foundation for patients under their care based on stage of cancer and travel distance.
Conclusion
We developed a generalizable method to calculate approximate driving times from patient addresses to VUMC locations using a third party online mapping service without sending PII to that third party. We used this method to determine the burden of treatment related to commuting for patients with breast cancer receiving care at VUMC. We found that radiation therapy made a significant impact on commuting burden due to the frequency of treatment. Also, patient’s living farther from VUMC tended to receive radiation therapy more at other medical facilities compared to those living closer to VUMC. We discovered that patients farther from VUMC had more appointments per unique appointment day, showing that their care was better coordinated. Future applications for travel time computation could equip organizations to better address the needs of their patients and help patients reduce the disruption of treatment on their lives.
Figure 1.
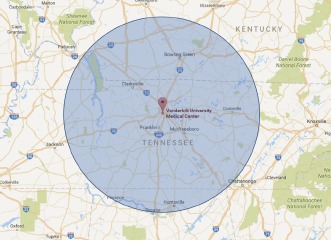
Patient addresses from the Vanderbilt Tumor Registry within 100 miles of VUMC were included in driving time calculations.
Figure 3.
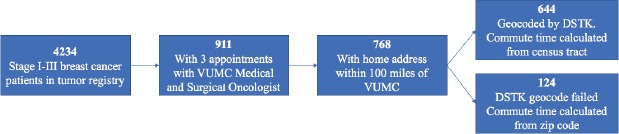
Cohort selection
Figure 4-5.
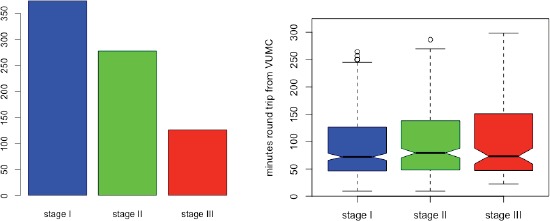
Number of patients per stage included in analysis and distribution of round trip driving times from patient addresses to main VUMC campus.
Table 3.
Estimated cost of vehicle expenses per patient over 18 months after diagnosis by stage and distance from VUMC. Mean (range).
| Close (within 20 miles) | Far (>20 and <100 miles) | |
|---|---|---|
| Stage I | $609 ($51.06 -$954.76) | $1047 ($238.02 -$3187.27) |
| Stage II | $824 ($77.25 -$3125.06) | $1455 ($198.29 -$4958.17) |
| Stage III | $1050 ($198.29 -$4958.17) | $1625 ($294.48 -$4779.91) |
Acknowledgments
Alex Cheng was supported by the T15LM007450-13 training grant from the National Library of Medicine.
References
- 1.CDC. Summary health statistics: National Health Interview Survey, 2014 [Internet] CDC. Available from: https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2014_SHS_Table_A-18.pdf.
- 2.CDC. Age differences in visits to office-based physicians by adults with hypertension: United States, 2013 [Internet] [cited 2017 Feb 7]. Available from: https://www.cdc.gov/nchs/products/databriefs/db263.htm. [PubMed]
- 3.CDC. Age differences in visits to office-based physicians by patients with diabetes: United States, 2010 [Internet] [cited 2017 Feb 7]. Available from: https://www.cdc.gov/nchs/data/databriefs/db161.htm. [PubMed]
- 4.Haley WE. Family caregivers of elderly patients with cancer: understanding and minimizing the burden of care. J Support Oncol. 2003;1(4) Suppl 2:25–9. [PubMed] [Google Scholar]
- 5.Tran V-T, Barnes C, Montori VM, Falissard B, Ravaud P. Taxonomy of the burden of treatment: a multi-country web-based qualitative study of patients with chronic conditions. [cited 2016 Mar 1];BMC Med [Internet] 2015 Dec;13(1) doi: 10.1186/s12916-015-0356-x. Available from: http://www.biomedcentral.com/1741-7015/13/115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.May C, Montori VM, Mair FS. We need minimally disruptive medicine. BMJ. 2009 Aug 11;339(aug11) 2:b2803–b2803. doi: 10.1136/bmj.b2803. [DOI] [PubMed] [Google Scholar]
- 7.Cheng A, Levy M. Data driven approach to burden of treatment measurement: A study of patients with breast cancer. 2016 In Chicago, IL. [PMC free article] [PubMed] [Google Scholar]
- 8.Zucca A, Boyes A, Newling G, Hall A, Girgis A. Travelling all over the countryside: Travel-related burden and financial difficulties reported by cancer patients in New South Wales and Victoria. Aust J Rural Health. 2011 Dec;19(6):298–305. doi: 10.1111/j.1440-1584.2011.01232.x. [DOI] [PubMed] [Google Scholar]
- 9.Gordon L, Ferguson M, Chambers S, Dunn J. Fuel, beds, meals and meds: out-of-pocket expenses for patients with cancer in rural Queensland. InCancer Forum. 2009;33(3):204. [Google Scholar]
- 10.Goyal S, Chandwani S, Haffty BG, Demissie K. Effect of travel distance and time to radiotherapy on likelihood of receiving mastectomy. Ann Surg Oncol. 2015 Apr;22(4):1095–101. doi: 10.1245/s10434-014-4093-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coughlin SS, King J. Breast and cervical cancer screening among women in metropolitan areas of the United States by county-level commuting time to work and use of public transportation, 2004 and 2006. BMC Public Health. 2010;10(1):146. doi: 10.1186/1471-2458-10-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang C. The impact of car ownership and public transport usage on cancer screening coverage: Empirical evidence using a spatial analysis in England. J Transp Geogr. 2016 Oct;56:15–22. doi: 10.1016/j.jtrangeo.2016.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weerheijm DV, Wieringa MH, Biert J, Hoogerwerf N. Optimizing transport time from accident to hospital: When to drive and when to fly? ISRN Emerg Med. 2012;2012:1–5. [Google Scholar]
- 14.HHS UH and HS. The HIPAA Privacy Rule [Internet] HHS.gov. 2008. [cited 2017 Feb 1]. Available from: https://www.hhs.gov/hipaa/for-professionals/privacy/index.html.
- 15.Bader MDM, Mooney SJ, Rundle AG. Protecting personally identifiable information when using online geographic tools for public health research. Am J Public Health. 2016 Feb;106(2):206–8. doi: 10.2105/AJPH.2015.302951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zandbergen PA. Ensuring confidentiality of geocoded health data: Assessing geographic masking strategies for individual-level data. Adv Med. 2014;2014:1–14. doi: 10.1155/2014/567049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.US Census Bureau. U.S. Gazetteer Files record layouts [Internet] 2016. [cited 2017 Feb 9]. Available from: https://www.census.gov/geo/maps-data/data/gazetteer2016.html.
- 18.Warden P. Data Science Toolkit [Internet] [cited 2017 Feb 9]. Available from: http://www.datasciencetoolkit.org/about.
- 19.How fast is your city? [Internet] [cited 2017 Mar 3]. Available from: http://infinitemonkeycorps.net/projects/cityspeed/
- 20.IRS. 2016 standard mileage rates for business, medical and moving announced [Internet] [cited 2017 Mar 3]. Available from: https://www.irs.gov/uac/newsroom/2016-standard-mileage-rates-for-business-medical-and-moving-announced.
- 21.Cassa CA, Grannis SJ, Overhage JM, Mandl KD. A context-sensitive approach to anonymizing spatial surveillance data: impact on outbreak detection. J Am Med Inform Assoc. 2006 Mar 1;13(2):160–5. doi: 10.1197/jamia.M1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayubi SUA. A framework of spreading disease monitoring system model. In: International Conference on Instrumentation, Communication, Information Technology, and Biomedical Engineering 2009. 2009:1–5. [Google Scholar]
- 23.Google Maps geocoding API usage limits [Internet] Google Developers. [cited 2017 Mar 4]. Available from: https://developers.google.com/maps/documentation/geocoding/usage-limits.
- 24.Brown J. Commuting takes longer for many in Nashville [Internet] The Tennessean. [cited 2017 Mar 1]. Available from: http://www.tennessean.com/story/news/local/2014/10/10/commuting-takes-longer-many-nashville/16805109/
- 25.Yousuf Zafar S. Financial toxicity of cancer care: It’s time to intervene. J Natl Cancer Inst. 2016 May;108(5):djv370. doi: 10.1093/jnci/djv370. [DOI] [PubMed] [Google Scholar]
- 26.Susan G. Komen Foundation. [cited 2017 Mar 4];Funding priorities [Internet] Available from: http://komeneasttennessee.org/funding-priorities-2/ [Google Scholar]


