Abstract
Smoking is the leading cause of preventable death in the United States. Obtaining patients’ smoking status is the first step in delivering smoking cessation counseling. In this study, we assessed the quality of smoking status captured in an electronic health record from a large academic medical center. We analyzed data from structured notes, finding that smoking status was documented in 98% of 64,451 hospital encounters in 2016. 32% hospital encounters had discrepant documentation, and 54.5% of patients had implausible changes (e.g., changes from “current smoker” to “never smoker”). Overall, only 2.9% of patients were documented as active smokers, but 36.4% were documented as “unknown” or had discrepancies in their smoking status. These results suggest that patients that smoke are not appropriately identified. Centralized documentation with clinically actionable smoking status categories and implementation of patient-facing tools that allow patients to directly record their information could improve data quality of smoking status.
Introduction
Smoking is an important risk factor for multiple diseases, including cardiovascular diseases and numerous types of cancer. It remains the number one cause of preventable death in the United States.1 The collection of patients’ smoking status during clinical encounters is critical to providing patients with resources to quit smoking. Smoking cessation can be difficult, and clinical visits are opportunities to intervene and recommend smoking cessation programs and therapies. Obtaining a patient’s smoking status is a crucial step in beginning smoking cessation interventions and monitoring progress.2 It may seem that recording updates to smoking status in a timely and accurate manner would be straightforward using modern electronic health records. This may not be the case for several reasons, including lack of standard terminology and granularity for data collection, shifting cultural attitudes regarding tobacco use, and potentially frequent changes in individuals’ smoking behavior.3,4 As the American author, Mark Twain, famously quipped, “Giving up smoking is the easiest thing in the world. I know because I’ve done it thousands of times.”
Given the clinical importance of smoking status, the “Meaningful Use” financial incentive program for electronic health record (EHR) adoption in the U.S. included a requirement for healthcare providers to capture patients’ smoking status electronically in structured fashion.5 Meaningful Use has helped to standardize data collection of smoking status and other information. However, even with improved standards for representing information, data quality issues have persisted in many patient-provided data types, such as race and ethnicity6,7 and family history.8,9 Previous studies on data quality have shown that clinicians describe a need for free-text documentation for expressiveness of documentation; however, these affordances challenge data reuse.10
Appreciating the challenges associated with data quality and the balance between the expressiveness of free-text and the benefits of structured data, we set out to answer a very simple question: how many of our hospital’s patients are known to be active smokers? We undertook a study to analyze how smoking status is currently being collected in a large academic medical center and to evaluate the quality of this data in EHRs.
Methods
We conducted a retrospective analysis of smoking status related data from the Allscripts Sunrise EHR (Allscripts Corp., Chicago IL) used at NewYork-Presbyterian Hospital/Columbia University Medical Center. We included patients that had at least one hospitalization during 2016, specifically patients that were discharged between January 1, 2016 to December 31, 2016.
The EHR system contained thousands of active templates for documentation. Each of these templates contained one to several hundred discrete observations. An observation could be a text box, a Boolean (e.g., a checkbox or radio button), or numeric value. We identified observations in which the description contained the stemmed words “smok”, “cigar” or “tobacco” and queried the EHR database to identify the number of times each one of these observations have been recorded during the study period. The value can be either textual (e.g. when the parameter is “Cigarettes (packs per day)”) with the response typed into a free-text box, or it can be structured (e.g. selected from a picklist). The picklist is often shown as a set of radio buttons that users can pick one. For example, there is a parameter labeled “Tobacco Use / Smoking Status”, and one possible choice in the picklist is “Never smoker.”
Exploratory analysis showed that 94% of patients had at least one structured smoking status observation recorded in a structured field. Based on this finding, we chose to use only the structured data for the remainder of the analyses. For comparison purposes, we classified smoking status into one out of four possible categories: “Current smoker”, “Former smoker”, “Never smoker”, and “Unknown smoking status” as described in Table 1. Observations such as “n/a for age” or “as per pt” were excluded from the analysis. Differences in smoking status recording were classified into two distinct categories: plausible, when the change is feasible to happen, and implausible, when the conflict is not possible to happen or in cases where there is loss of information. The description of this classification is illustrated in Figure 1. We also calculated the time interval (in days) between smoking status documentations to better understand the distribution of the data during the one-year study period. For example, time interval of zero means that both observations were recorded in the same day, time difference of one means that the second observation was recorded one day after the first one was recorded.
Table 1.
Description of the mapping from smoking status categories as recorded in the EHR to the four clinically actionable categories. Smoking status categories documented in the EHR that utilize the standard criteria defined by the Meaningful Use program are highlighted in bold.
| Clinically Actionable Smoking Status Categories | EHR Documented Categories | Number ofs Observations |
|---|---|---|
| Never Smoker | Never Smoker | 67,052 |
| Smoker (No) | 12,979 | |
| Patient Denies | 560 | |
| Current Smoker | Current every day smoker | 67,052 |
| Current some day smoker | 1,418 | |
| Light smoker | 714 | |
| Heavy Smoker | 267 | |
| Smoker, current status unknown | 676 | |
| Smoker (Yes) | 1,968 | |
| Former Smoker | Former smoker | 16,307 |
| Ex-smoker | 5 | |
| Quit / Stopped | 8,275 | |
| Unknown Smoking Status | Unknown if ever smoked | 16,514 |
| Unknown | 58 | |
| Unable to assess | 63 | |
| N/A/None | 569 |
Figure 1.
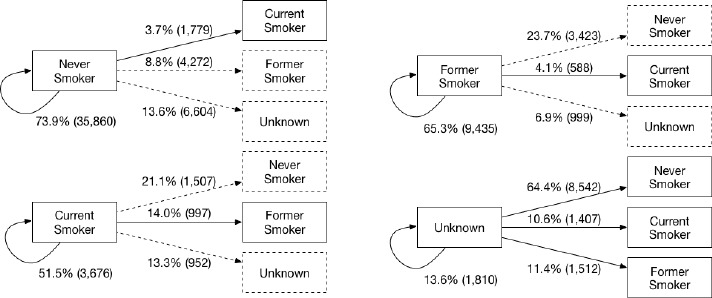
Changes of smoking status overtime. Dashed changes demonstrate implausible discrepancies and continuous lines represent plausible changes in longitudinal data. The number of changes recorded in our sample is reported in parentheses and the percentage it represents for each category is included in the figure.
Furthermore, we analyzed the discrepancies in smoking status reported for the same patient during the same visit, using data from different clinical notes in the EHR. We also investigated the discrepancies of smoking status recorded by different provider types (e.g., nurses, medical doctors, care coordinators, social workers). To analyze if provider types would have an impact in the number of discrepancies observed, we calculated the number of distinct providers’ roles recording smoking status for each admission. We then compared the number of distinct provider roles for patients with and without discrepancies in the smoking status recorded.
Overall, data quality of smoking status was assessed based on the percentage of patients with consistent and informative smoking status available (i.e., not classified as “Unknown” in the database, and not conflicting).
Results
Overall, we reviewed 48,909 patients having 64,451 hospital encounters in the one-year study period. We identified 203,048 observations of smoking status for 47,849 unique patients across 62,988 distinct hospital encounters. No smoking status documentation was identified for 1,463 visits from 1,060 distinct patients, representing 2% of the number of hospital encounters and 2% of the overall number of patients. In other words, 98% of patients and 98% of hospital visits had documentation regarding the patient’s smoking status. Of those records with smoking status, 59,663 visits (93%) from 45,822 patients (94%) had this information recorded in structured format. After preprocessing, 45,771 patients (94%), including 59,593 visits (92%) and 129,134 observations were classified into four distinct smoking status categories. The number of observations and the mapping to the simplified smoking categories are described in Table 1. The description of smoking status data during the one-year study period is described in Table 2. Patients had an average of 1.3 visits/patient during the study period, with the maximum number of visits a single patient being 23 visits.
Table 2.
Description of smoking status data during the one-year study period.
| Descriptor | Sample size |
|---|---|
| Patients | 48,909 |
| Hospital Encounters | 64,451 |
| Encounters with smoking status recorded | 62,988 (98%) |
| Encounters with smoking | 19,176 (30%) |
Longitudinal One-year Review
Overall, 15,048 patients (32.9%) had smoking status recorded in a single note, and 30,723 patients (67.1%) had more than one note with documentation regarding smoking status. Among the patients with more than one note with smoking status documented, we identified 83,363 changes in documented smoking status collected longitudinally during the one-year study period.
Among the changes in smoking status documentation, 32,582 (39.1%) had a conflicting smoking status. These discrepancies were observed in records from 15,207 distinct patients, representing 33.2% of our study population. However, because we are working on longitudinal data and smoking status is not a static concept since it can change over time, some of these discrepancies are feasible to happen. For example, someone that never smoked can become a smoker. Others, however, are implausible. For example, a non-smoker cannot become a former smoker, or a current smoker cannot become a never smoker, unless some of the data was recorded incorrectly. Other changes are plausible, however not good from a data quality standpoint. Having a patient with documentation regarding smoking status and later not having smoking status (smoking status as “unknown”) demonstrates loss of information. Implausible changes as well as changes from a well-defined smoking status to uninformative category were considered discrepancies due to data quality issues. We identified 17,757 discrepancies (implausible changes and loss of information changes), which constituted 54.5% of changes, in 10,836 distinct patients. These discrepancies are represented in Figure 1 as dashed lines, while the other changes are represented in continuous lines.
On average the time interval between different smoking status documentation was 11 days, with a minimum of 0 days (same day documentation), and a maximum of 362 days. Most patients (80.6%) had a time interval between documentation events of less than or equal to 10 days, with 61.1% of patients having a subsequent documentation event within one day of the previous event.
Duplicate Assessments During the Same Hospital Encounter
While it is plausible to observe changes in smoking status over the course of one year, smoking status should not change during the same hospital encounter. Given this rationale, we considered all changes during a hospital encounter to reflect a data quality issue, since smoking status should be consistent throughout a single admission. During the study period, we identified 59,663 distinct encounters from 45,822 patients. Of those, 32.2% of the hospital encounters (19,176 visits) had at least one conflicting smoking status recorded, which includes 14,798 patients (32.3% of our cohort of patients).
Discrepancies Among Various Provider Roles
For patients with a smoking status recorded in a structured field, 70.8% were documented as part of nursing notes, 12.9% came from social work notes, 11.6% from physician notes, and the remaining (4.7%) from notes entered by other health care professionals.
Among hospital encounters with more than one assessment of smoking status, encounters with documentation from a single role of provider (e.g., nurse) had fewer discrepancies compared with encounters containing smoking status assessments from providers with disparate roles (Table 3). For example, if multiple nurses documented smoking status during an admission, the number of distinct provider roles would be equal to one. However, if multiple nurses and multiple physicians documented this information, then the number of distinct provider roles would be two.
Table 3.
Description of smoking status data during the one-year study period.
| Number of distinct provider roles | Encounters without discrepancies | Encounters with discrepancies |
|---|---|---|
| 1 | 45.97% (8,791) | 26.15% (6,650) |
| 2 | 48.08% (9,195) | 52.49% (13,345) |
| 3 | 5.91% (1,130) | 20.94% (5,323) |
| >3 | 0.05% (9) | 0% (1) |
How many patients are smokers?
Overall, 54.2% of the patients in our sample were classified as non-smokers, 6.5% as former smokers, 2.9% as current smokers and 3.2% as having unknown smoking status. The remaining 33.2% of patients had at least one discrepant assessment of smoking status documented. We determined that only 63.6% of our study population had a consistent, unchanging smoking status during the one-year study period (Figure 3).
Figure 3.
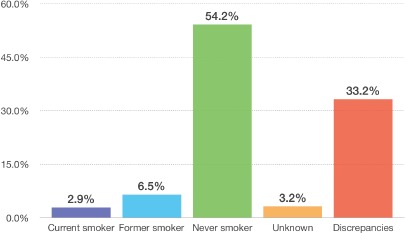
Smoking status of patients seen in 2016.
Discussion
The Centers for Medicare and Medicaid Services (CMS) Meaningful Use program requires participating healthcare providers to record patients’ smoking status in a structured fashion.5 The program specifies eight distinct categories for collecting smoking status: “Current every day smoker”, “Current some day smoker”, “Former smoker”, “Never smoker”, “Smoker, current status unknown”, “Unknown if ever smoked”, “Heavy tobacco smoker” and “Light tobacco smoker”.
We identified smoking status assessments (either represented in free-text or structured fields) for 98% of patients and 98% of visits. When focusing on structured documentation, we observed that 94% of patients and 92% of visits had at least one structured smoking status observation recorded.
Despite the well-known and well-described importance of collecting smoking status, our institution’s EHR did not have a centralized location to store smoking status information. Smoking status was collected as part of clinical notes, in either structured or free-text format. The fact that disparate healthcare providers recorded this information in several different notes resulted in many inconsistencies across notes. Further complicating the matter, different note templates allowed for different granularities of smoking status data collection. Some templates included a free-text box that allowed clinicians to enter details such as intensity of smoking, number of cigarettes per day, or when the patient stopped smoking. Other templates had only the Meaningful Use-required structured fields embedded.
When analyzing smoking status data in the EHR, we transformed the Meaningful Use categories and other smoking status assessments into four clinically actionable categories: “Current smoker”, “Former smoker”, “Never smoker” and “Unknown smoking status”. We observed that a 33.2% of the patients had inconsistencies in the documented smoking status during the one-year study period and 32.3% of the patients had at least one discrepancy during a single visit. These discrepancies suggest that reliable information on smoking status may not be available for a large number of patients.
Since we used longitudinal data, and smoking status is not a static concept (i.e., it can change over time), we classified smoking status changes into two distinct categories: plausible and implausible. In our study, implausible changes constituted 21.3% of all changes. Previous research has also identified consistency issues regarding tobacco use recorded in different notes in EHR systems. For example, in 2016 a research study used natural language processing to parse clinical notes and extract smoking status from various clinical notes. The authors identified several inconsistencies when comparing smoking status recorded in clinical notes.11
Inconsistencies can be attributed to challenges in the data collection process, including clinician-related and patient-related factors. Clinicians may not inquire at all about a patient’s smoking status, or they might ask the question in a manner that leads to bias in the patient’s answer. Depending on how clinicians phrase the question, patients may not feel comfortable answering. On the other hand, patients may have their own motivations to be less than truthful when providing smoking status information to clinicians, or they may inexplicably provide different smoking status responses depending on the person asking.
We conducted an analysis to identify whether hospital encounters with more than one clinical note without discrepancies were more likely to have documentation from a single provider role than encounters with discrepancies. Interestingly, we identified that encounters with multiple notes documented by the same type of provider had less discrepancies than patients with documentation from multiple types of providers. The difference we observed in discrepancies may be explained by the fact that clinicians usually do not read notes from other clinicians’ roles. Previous studies have shown that most clinical notes are not read by the entire clinical team.12 Instead, clinicians may be more inclined to read clinical notes from their peers (i.e., within the same provider role). While it is important for multiple providers to assess patients’ smoking status, barriers to accessing previously documented information regarding tobacco use by healthcare providers may increase vulnerabilities that allow discrepancies to propagate.
Going back to our initial question of “how many patients are current smokers?” - the answer is, we do not know. Based on the analysis conducted in this study, more than half of the patients during the one-year study period were recorded consistently as non-smokers and just 2.9% were recorded consistently as current smokers. In contrast, other population-based studies estimate that 15.1% of adult Americans smoke.13 One-third of the studied population had inconsistencies in their smoking status, making the determination of tobacco use for these patients difficult. While smoking status was documented in 98% of hospital encounters (and therefore the criteria of Meaningful Use were satisfied), our one-year sample of hospital encounters did not contain consistent smoking status information for 36.4% of patients.
One limitation of our analysis was the use of data from only a single year and from only a single healthcare system. During a one-year period within our EHR system, we found that 33.2% of patients had discrepancies in documentation of smoking status. Furthermore, 54.5% of those inconsistencies were deemed implausible (Figure 1). Most patients had changes recorded within 10 days of the previous smoking status assessment. Given the short time difference between documentation events, even plausible changes (e.g., converting from “current smoker” to “former smoker”) seem unlikely. These data quality issues demonstrate just some of the considerable challenges healthcare providers and secondary users of EHR data. If we have difficulty in identifying a single meaningful and consistent smoking status using only one-year worth of data, the use and sharing of multiple years of data present even bigger challenges. For example, for encounters with conflicting smoking statuses, which one should be used in a clinical decision support system related to smoking cessation? Or which one should be reported to external organizations? Efforts using smoking status information from EHRs, including future smoking cessation initiatives, should further investigate patients identified as “Unknown smoking status” as well as patients with discrepancies in smoking status.
Recommendations
In this study, we observed that smoking status is currently being collected as part of clinical notes by multiple healthcare providers, and for almost all patients. The categories used are not consistent across clinical notes, recording smoking status in different granularities. We propose the use of four distinct clinically actionable categories: “Never smoker”, “Current smoker”, “Former smoker” and “Unknown smoking status”. More detailed information for each one of these could also be collected in a standardized fashion, such as “packs/day” and start and quit date. Currently, this additional information is being captured in free-text format and inconsistent across notes (e.g. some use packs/day while other record this information as cigarettes/day).
In our institution, smoking status is not stored in a centralized location, but is rather being collected as part of disparate clinical notes. The current system of data collection of smoking status presents challenges consistently collecting this information. While it is important for multiple providers to collect patients’ tobacco use information, the fact that this information is collected and stored in various notes without standardization makes it challenging for clinicians to know if the patient already provided their smoking status to other clinicians, and whether this information is longitudinally consistent. In an attempt to solve these challenges, we propose to store patients’ smoking status in a centralized fashion and having clinicians verifying this information in every encounter by asking patients about tobacco use.
One way to improve the consistency and correctness of patient-reported information, such as smoking status, is to allow patients to review and update their own information. This task can be facilitated by health information technology in many ways, including the use of patient portals and tablet computers for this task. Patient-facing tools have been used for collection of multiple patient-provided data types such as race and ethnicity, family history, symptoms, medication reconciliation and adherence. These studies have shown that patients are willing to provide and review their information14-16, that EHR data is often incomplete or inaccurate6–8,17–23 and that patients can identify discrepancies, provide useful information and help keeping records up-to-date. 18,24–26 Studies have also shown that there are many benefits of involving patients in their care, including improving patient engagement, patient satisfaction, health behaviors and health status as well as helping to attract and retain patients.27–31 With patient-facing tools, patients could provide their smoking status based of the four clinically actionable categories, as described above. Patients providing this information to a computer could also mitigate the potential biases introduced by clinicians asking the question.
Conclusion
In summary, while 98% of hospital encounters at our institution during 2016 contained information regarding the patients’ smoking status, 32% of the encounters had discrepancies in smoking status information. For encounters with more than one clinical note documenting smoking status information, 54% of the subsequent documentation events had implausible changes. While other sources suggest that approximately 15% of adult Americans smoke, only 2.9% of our patients were consistently documented as current smokers. This finding demonstrates that while Meaningful Use has improved data collection of smoking status in terms of completeness, we may not be appropriately identifying patients that smoke. Centralized documentation with clinically actionable smoking status categories available for data collection, and implementation of patient-facing tools that allow patients to directly record their information, may help improve data quality of smoking status in EHRs.
Figure 2.
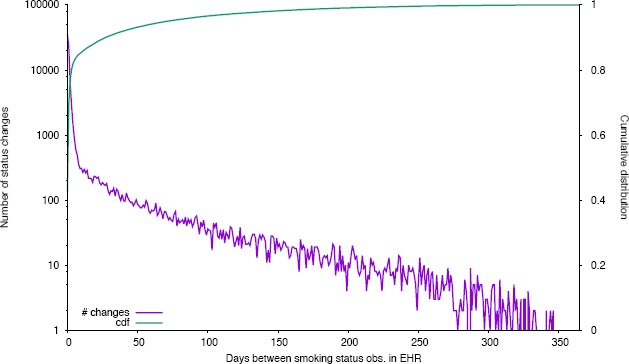
Number of smoking status changes by time interval documentation. Time interval is measured in days. Number of status changes is represented in logarithmic scale. CDF = cumulative distribution function.
References
- 1.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US) 2014. [PubMed]
- 2.Caplan L, Stout C, Blumenthal DS. Training physicians to do office-based smoking cessation increases adherence to PHS guidelines. J Community Health. 2011 Apr;36(2):238–43. doi: 10.1007/s10900-010-9303-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Committee on the Recommended Social and Behavioral Domains and Measures for Electronic Health Records, Board on Population Health and Public Health Practice, Institute of, Medicine. Washington (DC): National Academies Press (US); 2015. Jan 8, Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. [PubMed] [Google Scholar]
- 4.Winden TJ, Chen ES, Wang Y, Sarkar IN, Carter EW, Melton GB. Towards the Standardized Documentation of E-Cigarette Use in the Electronic Health Record for Population Health Surveillance and Research. AMIA Jt Summits Transl Sci Proc. 2015;2015:199–203. [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Medicare & Medicaid Services (CMS) Eligible Professional Meaningful Use Core Measures Measure 9 of 13. 2014. May 27, pp. 1–2.
- 6.Klinger EV, Carlini SV, Gonzalez I, Hubert SS, Linder JA, Rigotti NA, et al. Accuracy of race, ethnicity, and language preference in an electronic health record. J Gen Intern Med. 2015 Jun;30(6):719–23. doi: 10.1007/s11606-014-3102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee SJC, Grobe JE, Tiro JA. Journal of the American Medical Informatics Association: JAMIA. 3. Vol. 23. The Oxford University Press; 2015. Dec 11, Assessing race and ethnicity data quality across cancer registries and EMRs in two hospitals; pp. 627–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Polubriaginof F, Tatonetti NP, Vawdrey DK. An Assessment of Family History Information Captured in an Electronic Health Record. AMIA Annu Symp Proc. 2015;2015:2035–42. [PMC free article] [PubMed] [Google Scholar]
- 9.Powell KP, Christianson CA, Hahn SE, Dave G, Evans LR, Blanton SH, et al. Collection of family health history for assessment of chronic disease risk in primary care. N C Med J. 2013 Jul;74(4):279–86. [PubMed] [Google Scholar]
- 10.Rosenbloom ST, Denny JC, Xu H, Lorenzi N, Stead WW, Johnson KB. Data from clinical notes: a perspective on the tension between structure and flexible documentation. Journal of the American Medical Informatics Association: JAMIA. (2011 ed) 2011 Mar;18(2):181–6. doi: 10.1136/jamia.2010.007237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Y, Chen ES, Pakhomov S. Investigating Longitudinal Tobacco Use Information from Social History and Clinical Notes in the Electronic Health Record. AMIA Annu Symp Proc. 2016 [PMC free article] [PubMed] [Google Scholar]
- 12.Hripcsak G, Vawdrey DK, Fred MR, Bostwick SB. Use of electronic clinical documentation: time spent and team interactions. Journal of the American Medical Informatics Association. 2011 Mar 1;18(2):112–7. doi: 10.1136/jamia.2010.008441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current Cigarette Smoking Among Adults - United States, 2005-2015. MMWR Morb Mortal Wkly Rep. 2016 Nov 11;65(44):1205–11. doi: 10.15585/mmwr.mm6544a2. [DOI] [PubMed] [Google Scholar]
- 14.Pyper C, Amery J, Watson M, Crook C. Patients’ experiences when accessing their on-line electronic patient records in primary care. Br J Gen Pract. Royal College of General Practitioners. 2004 Jan;54(498):38–43. [PMC free article] [PubMed] [Google Scholar]
- 15.Weingart SN, Hamrick HE, Tutkus S, Carbo A, Sands DZ, Tess A, et al. Medication safety messages for patients via the web portal: The MedCheck intervention. International Journal of Medical Informatics. 2008 Mar;77(3):161–8. doi: 10.1016/j.ijmedinf.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 16.Dullabh P, Sondheimer N, Katsh E, Evans MA. How Patients Can Improve the Accuracy of their Medical Records. eGEMs (Generating Evidence & Methods to improve patient outcomes) 2014 Oct 1;2(3):1–15. doi: 10.13063/2327-9214.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ball MJ, Lillis J. E-health: transforming the physician/patient relationship. International Journal of Medical Informatics. 2001 Apr;61(1):1–10. doi: 10.1016/s1386-5056(00)00130-1. [DOI] [PubMed] [Google Scholar]
- 18.Staroselsky M, Volk LA, Tsurikova R, Pizziferri L, Lippincott M, Wald J, et al. Improving electronic health record (EHR) accuracy and increasing compliance with health maintenance clinical guidelines through patient access and input. International Journal of Medical Informatics. 2006 Oct;75(10-11):693–700. doi: 10.1016/j.ijmedinf.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 19.Qureshi N, Wilson B, Santaguida P, Little J, Carroll J, Allanson J, et al. NIH State-of-the Science Conference: Family History and Improving Health 2009. Evidence Report/Technology. 2009 [PMC free article] [PubMed] [Google Scholar]
- 20.Kaplan JB. The Quality of Data on “Race” and ‘Ethnicity’: Implications for Health Researchers, Policy Makers, and Practitioners. Race Soc Probl. 2014 May 30;6(3):214–36. [Google Scholar]
- 21.Welch BM, Dere W, Schiffman JD. Family Health History. JAMA. 2015 May 5;313(17):1711–2. doi: 10.1001/jama.2015.2417. [DOI] [PubMed] [Google Scholar]
- 22.Kressin NR. Race/Ethnicity Identification: Vital for Disparities Research, Quality Improvement, and Much More Than “Meets the Eye”. Medical care. 2015 Aug;53(8):663–5. doi: 10.1097/MLR.0000000000000409. [DOI] [PubMed] [Google Scholar]
- 23.Douglas MD, Dawes DE, Holden KB, Mack D. Missed policy opportunities to advance health equity by recording demographic data in electronic health records. Am J Public Health. 2015 Jul;105 Suppl 3(S3):S380–8. doi: 10.2105/AJPH.2014.302384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Staroselsky M, Volk LA, Tsurikova R, Newmark LP, Lippincott M, Litvak I, et al. An effort to improve electronic health record medication list accuracy between visits: Patients’ and physicians’ response. International Journal of Medical Informatics. 2008 Mar;77(3):153–60. doi: 10.1016/j.ijmedinf.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 25.Wu RR, Himmel TL, Buchanan AH, Powell KP, Hauser ER, Ginsburg GS, et al. Quality of family history collection with use of a patient facing family history assessment tool. BMC Family Practice. BMC Family Practice. 2014 Feb 13;15(1):1–8. doi: 10.1186/1471-2296-15-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arsoniadis EG, Tambyraja R, Khairat S, Jahansouz C, Scheppmann D, Kwaan MR, et al. Characterizing Patient-Generated Clinical Data and Associated Implications for Electronic Health Records. Stud Health Technol. 2015 [PubMed] [Google Scholar]
- 27.Epstein RM, Fiscella K, Lesser CS, Stange KC. Why The Nation Needs A Policy Push On Patient-Centered Health Care. Health Aff (Millwood) 2010 Aug 2;29(8):1489–95. doi: 10.1377/hlthaff.2009.0888. [DOI] [PubMed] [Google Scholar]
- 28.Arar N, Seo J, Abboud HE, Parchman M, Noel P. Veterans’ experience in using the online Surgeon General’s family health history tool. Per Med. 2011 Sep;8(5):523–32. doi: 10.2217/pme.11.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dwamena F, Rovner MH. Interventions for providers to promote a patient-centred approach in clinical consultations. The Cochrane …. 2012 doi: 10.1002/14651858.CD003267.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Otte-Trojel T, de Bont A, Rundall TG, van de Klundert J. Journal of the American Medical Informatics Association: JAMIA. 4. Vol. 21. The Oxford University Press;; 2014. Jul, How outcomes are achieved through patient portals: a realist review; pp. 751–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davis Giardina T, Menon S, Parrish DE, Sittig DF, Singh H. Journal of the American Medical Informatics Association: JAMIA. 4. Vol. 21. The Oxford University Press; 2014. Jul, Patient access to medical records and healthcare outcomes: a systematic review; pp. 737–41. [DOI] [PMC free article] [PubMed] [Google Scholar]


