Abstract
Mobile health (mHealth) could offer unprecedented opportunity to provide medical support closer to the users. We have selected some relevant criteria to describe 100 apps from Google Play store and Apple’s App Store’s top suggestions in medical category. These characteristics were compared based on the paid or free nature of the apps, the target users: consumers or healthcare professionals, and the platform: Android or iOS. Seventeen provided functionalities and 27 medical subjects covered by these apps were also extracted. Our study shows that even in top rated mHealth apps, a high proportion lacks some basic criteria regarding the quality of the apps including the presence of a privacy policy, describing content sources, participation of the target users in the app development, etc. Paid apps did not ensure better quality compared to free apps. The current mHealth market is not mature enough to be used widely and recommended by healthcare professionals.
Introduction
Mobile health (m-health) is a subdivision of the eHealth phenomenon that is in a perpetual state of active refinement. There is a vast amount of potential for m-health to positively affect health and healthcare processes1. Mobile apps offer an unprecedented opportunity to provide medical support at the time /location of the demand2. This opportunity can be harnessed by the general public (e.g. patients) or health professionals who are in need of various specialized tools (means of interdisciplinary communication, ready access to health and medical information, simple consultation of medical records, and clinical decision-making support systems)3.
Although m-health apps are a relatively recent development, their virtual presence is exploding with no indication of slowing any time soon. There are over 259,000 health-related applications (apps) available in app stores (e.g. Google Play and Apple’s iOS “app store”) for smartphone devices. Approximately 100,000 m-health apps have been added as of the beginning of 20154. Each month, about 1,000 new applications are put on the market5. These apps proffer myriad functionalities, ranging from simple text message reminders to platforms designed for sophisticated disease management. Naturally, the growth of the m-health market correlates with the increase in usage these apps are experiencing. In the next several years, upwards of three million free downloads and circa 300,000 purchased downloads are expected to be made of mHealth applications in the United States alone6. These values exhibit a swift rise in the prevalence of mobile technology in the medical and wellness fields. Being readily accessible and simple to procure ensures that smart devices (smartphones and tablets) are made very attractive in the eyes of medical professionals. We are reaching a turning point in the use of mobile technology in healthcare. There is therefore a pressing need to ensure that patient safety is not compromised post-maturation of the field7. The continually-rising number of mHealth apps and the variety of obtainable functionalities render it burdensome for any kind of user (health professional or patient) to ascertain which apps excel in terms of quality.
There exist a great deal of potential dangers, and the reliability of some mHealth apps was investigated in several works of literature8–10. The involvement of a medical professional in the development of a given application11, the accuracy and reliability of the content as utilized in diagnosis and patient management12, the potential danger of camera functionalities in mobile devices to judge whether skin lesions are suspicious13,14, and deficiencies in self-management applications (in both diabetes15 and asthma16) were called into question by various researchers.
While the growing popularity of m-health is well-documented, its impact is not. The reported implications of mHealth interventions are mixed, with studies exhibiting modest benefits for some clinical diagnosis and management support outcomes1. Furthermore, the information provided in app stores does not permit users to ascertain the quality of apps. The existing five-star rating system currently in use is not a reliable assessment method17. One is faced with a veritable jungle of health-related apps, including very good apps as well as those that endanger patient/physician safety. In order to address to this deficiency in today’s mobile health market, a research study was proposed to assess the current standing of mHealth applications available for download in the United States. We were interested in determining whether or not the current market could be considered a reliable source of medical applications. The main aim of this study was therefore to isolate characteristics of health apps currently available and identify existing gaps.
Methods
In collaboration with medical doctors from France and Stanford University, we have conducted a cross-sectional descriptive study of the top 100 medical applications available in the Google Play store and Apple’s App Store. We selected the top 25 free apps from the App Store followed by 25 of the same from the Google Play Store. When an app appeared in both stores, it was only selected once and passed over in favor of the following app. For the payed apps we employed the opposite strategy, beginning with the Google Play Store and only afterwards the Apple Store. If the reported purpose of the app had no relation to medicine, it was not selected. Other exclusion criteria were that no apps that encapsulated other apps (a mini store of apps) and paid apps more expensive than 70 dollars were not selected.
The order of apps on the top lists are very subject to change. In the beginning of January 2017, we selected our apps in compliance with the aforementioned criteria. We did not alter our choices over the course of the study. The working group was composed of four physicians invested in medical informatics. The apps were installed on a relevant mobile device and analyzed one by one by each group member.
In order to define the criteria used over the course of the study, we hypothesized that we could utilize key elements of the mHealth Quality (mHQ) process18. We have isolated from said process the most relevant criteria to assess the American market. The extraction criteria included informative and assessment criteria.
Apart from the characteristics of the app, we have analyzed each app to evaluate the use cases (functionalities) imparted by the app according to a previously published model of use cases for mHealth apps3. We have also determined the relevant medical subject/specialty related to each app.
Each member of the working group had an Excel table to fill for each app. We organized a weekly meeting to discuss differing opinions and reach a consensus.
Descriptive data were provided for each criterion. The characteristics of both free and paid apps were compared according to their target demographic (consumers or health professionals) as well as the platform (iOS and Android). Chi-Square test was used to determine whether there was a significant difference between the elements of the information in the categories and P < 0.05 was considered statistically significant.
Results
Half of the analyzed apps were installed on Android phones, and the other half were installed on iOS ones. From each platform 25 paid apps and 25 free apps were selected. Whilst performing the selections, three apps were excluded from the study due to their non-medical nature. One app was not selected due to its high price and two others were excluded because they were essentially a mini store of apps.
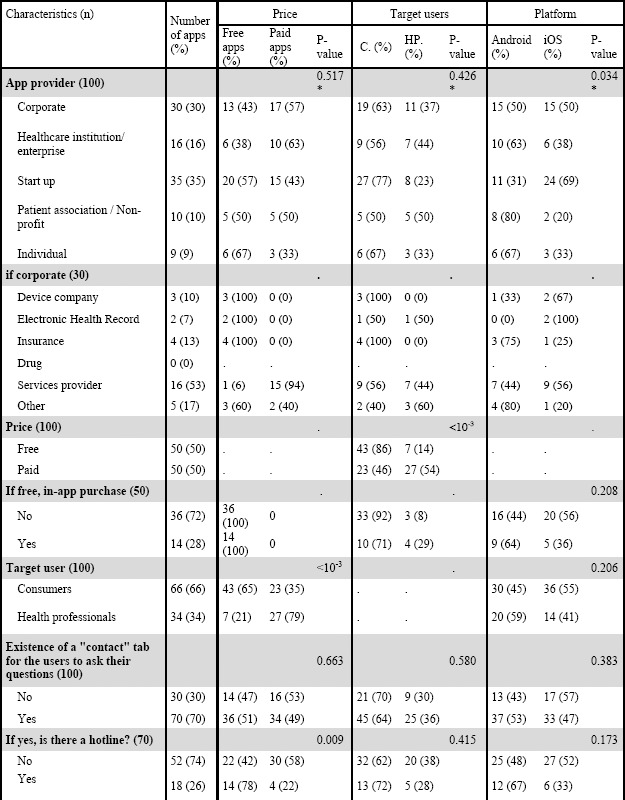
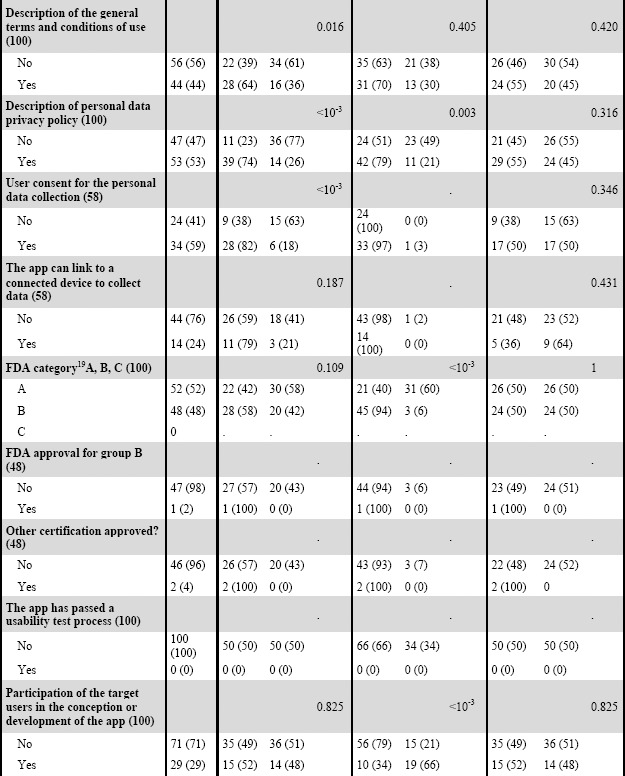
The selected criteria were divided into informative elements and assessment elements. The informative elements include type of owner (start-up, corporation, patient association, etc.), target user, the topic the app was attempting to address, whether or not it belonged to the appendix A, B or C of the FDA document on Mobile Medical Applications19, etc. Assessment elements include the existence of general terms and conditions of use, existence of privacy policy, presence of a health professional during app development, citation of content sources, etc. T able 1 provides descriptive explanations of various criteria and distribution of apps.
Most app criteria were evaluated in all 100 of the analyzed apps. However, some criteria were not applicable to all apps. For example, “user consent to personal data collection” and “ability to link to a connected device in order to collect data” were rendered obsolete for apps whose purpose was not to collect personal health data. The aforementioned criteria were only applicable to 58 apps. Another example is “citation of the content sources or bibliographic references” and “medical content is kept up to date” because only 71 of selected apps include medical content.
The pecuniary nature of some apps caused a significant difference (p<0.001) between those addressed to consumers and those targeting healthcare professionals. Apps whose target demographic consisted mostly of healthcare professionals were less likely to be free to download. However, 28% of free apps had in-app integrated purchases.
We did not find a significant difference between target users of Android vs. iOS apps, none of the two major markets is oriented more towards consumers or healthcare professionals.
Seventy apps presented a means of contacting the owner via email. There was no significant difference between free and paid apps, between those addressed to consumers vs. healthcare professionals, or between the two platforms. 26% of selected apps provide a hotline to address users’ potential queries. There was a significant difference (p < 0.009) between free and paid apps: free apps provide more hotline services than paid ones.
More than half of the apps did not provide general terms and conditions of use. We found no substantial difference in availability between Android/iOS apps or between consumer-targeted/healthcare-professional-targeted ones. However, a larger amount of free applications offer general terms and conditions in juxtaposition with paid apps (p<0.016). This phenomenon occurs once again with the availability of privacy policies. Free apps include privacy policies more frequently than paid apps (p<0.001).
Only 59% of the apps collecting user health data require the explicit consent of their users pre-collection, and free apps were once again superior (p<0.001). No difference was found when we compared the two major platforms and target users.
There was only one app that boasted an ethical chart. This app was free, meant for healthcare professionals, and available in the Top 25 of both the Google Play and App stores (in compliance with the aforementioned selection criteria we studied the iOS version).
Seventeen disparate use cases were discovered in the 100 analyzed apps according to the Yasini and Marchand Model3. Six use cases were related to health professionals and eleven to consumers. We discovered 226 use cases in these apps, meaning that the average number of use cases provided by each app is 2.26. Table 2 illustrates the various uses cases and their frequency in the selected apps.
Table 2.
Frequency of various uses cases in the top apps of the two major US stores.
| Use Cases | number | % |
|---|---|---|
| C. Calculate and/or interpret data | 30 | 13,3 |
| C. Communicate/share information, social network | 7 | 3,1 |
| C. Database (drug, image, nutrition…) | 21 | 9,3 |
| C. Diagnostic/measurement tool | 12 | 5,3 |
| C. Health news | 4 | 1,8 |
| C. Information/Scientific popularization/Therapeutic patient education | 19 | 8,4 |
| C. Interaction with a health institution (Scheduling an appointment, Drug ordering…) | 17 | 7,5 |
| C. Locating a health service | 18 | 8,0 |
| C. Looking for information on health professionals/institutions | 10 | 4,4 |
| C. Tracking a physiopathological state | 29 | 12,8 |
| C. Treatment reminder/Managing the drug stock | 6 | 2,7 |
| HP. Clinical cases/serious gaming/Reviewing previously given exams | 8 | 3,5 |
| HP. Database (drug, image, bibliography…) | 22 | 9,7 |
| HP. Decision support system, calculate and/or interpret data | 3 | 1,3 |
| HP. Diagnostic/measurement tool | 1 | 0,4 |
| HP. Managing professional activities (searching for job offers, calculating the fees…) | 1 | 0,4 |
| HP. Text book, journal, guidelines and synthesis of medical knowledge | 18 | 8,0 |
| Total | 226 | 100 |
C: Consumers, HP: Healthcare Professionals
We were able to classify the chosen apps in 27 subject groups, of which 15 were consumer-oriented and 12 targeted health professionals. For consumer-targeted applications the most well-covered subject was general health status (29%), most often exhibited by apps attempting to centralize all patient data in order to provide a comprehensive synthesis of such. We also noted that an integral portion of consumer apps (18%) focused upon women’s health issues such as menstrual cycles and pregnancy concerns. The subject of eight apps (12%) was managing the use and cost optimization of medications.
For apps directed towards healthcare professionals, atlases of anatomy dominated (26%). Second place was held by applications that could be harnessed by professionals of all medical specialties (20%) (e.g. drug databases). 17% of apps specifically for healthcare workers dealt with emergency medicine, and 11% of apps were created to aid students’ exam preparation. Figure 1 portrays the various subjects and their relative frequency.
Figure 1.
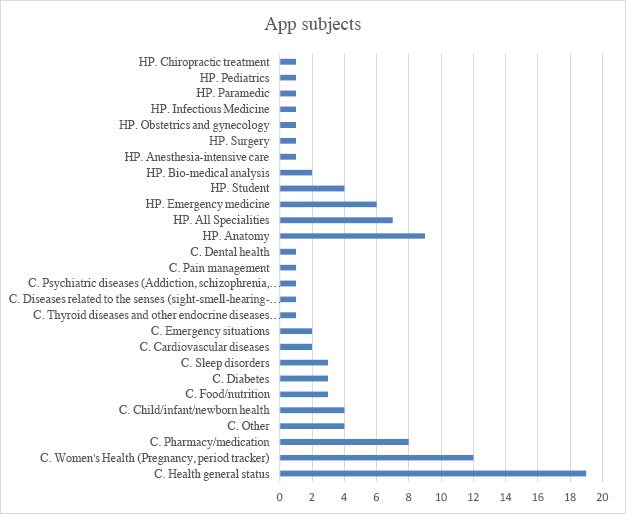
Distributions of applications in different subjects. (HP: Healthcare Professionals, C: Consumers)
Discussion
In this study, we analyzed 100 US mHealth applications available in the medical category of the Google Play store and Apple’s iOS App Store. We described some of the characteristics of these apps including the app’s target user, the app provider, presence of a physician in the core team of the company owning the app, providing the content sources when relevant, and providing terms and conditions of use and privacy policy. We also extracted the subjects they dealt with and their various use cases.
Although we have only analyzed the apps in the medical category, we have excluded three apps because of nonrelevant topic to medicine. One of these apps was a music app and two others were games (that were not considered as serious medical related games). This shows that even in the top-rated apps in the market stores, some apps are not well categorized.
Contrary to our impression, paid apps did not provide a more qualified profile compared to free apps based on the evaluated criteria. This may be explained by the fact that mobile apps are often used by providers as another marketing tool to create loyal users. mHealth market is still in the phase that the app providers want to build their brand image and get their name out. Therefore, most of the providers select free apps to increase the download rate and potentially provide more qualified apps to keep their users continually.
Various mHealth apps collect and offer critical and private patient data. The data may be entered directly by the user, collected with the built-in features of the smart device (e.g., camera, microphone), an external sensor, or a connected device (e.g., connected thermometer). These data need a special focus on information security and privacy of mHealthapps. Potential damage to users through information security and privacy infringements have been discussed in various studies20–22. Our study shows that still about half of the analyzed apps do not provide terms and conditions of use or privacy policy. The situation becomes more dramatic when we consider that the analyzed apps come from the top of the App Stores.
The involvement of healthcare professionals in mHealth apps development processes is another important criterion that ensures the reliability of health information17,23,24. This study showed that 61% of the studied apps were produced with the participation of a health professional in the core team of the app owner. Other studies in the literature reported the rate of this involvement between 12.8% to 48% of analyzed apps20,24. Although in our sample of apps we found a higher rate of professional involvement in the development of the apps, this is not yet satisfying particularly for the top listed apps of the App Stores.
It is critical that medical applications provide content that are accurate and reliable25 because patients and healthcare professionals can make critical decisions based on information provided by an app. We did not find the content source for 44% of apps that provide medical information to their target users. When mHealth apps disseminate medical information, which was the case for 71% of the analyzed apps, the information must be developed on the basis of reliable information resources and references. This study showed that 44% of these apps did not mention their sources. This lack of transparency of the apps about the sources is in line with other studies in the literature who call in to question the adherence of the apps to established guidelines20,24,25.
None of the studied apps could be considered as a medical device according to FDA classification19. However, half of these apps were considered as borderline apps (group B). The need for regulating the apps is a real challenge of today’s mHealth market. The percentage of apps that resort to FDA authorization or other existing certifications (like European CE for medical devices) is too low. This shows that the market is not yet enough mature to the assessment and certification processes.
Various apps were multifunctional and provided various use cases in different medical fields. This indicates that the iOS and Android App Stores offer a wide selection of mHealth apps with a real diversity of usages that makes mobile devices ready to do almost everything in every medical specialty. However, this diversity prevents a “one size fits all” approach to ensuring the quality of these apps and information security18,21.
One of the limitations of our study was the number of studied apps. The top-rated apps in the App Stores are based on the five-star rating that the users provide, number of downloads and some other criteria. However, the number of downloads may differ according to the target users of the apps (an app for diabetic patients may be downloaded more than an app that is addressed to the patients affected with a rare disease) and the five-star rating is not a reliable assessment system17,26. In this study, we have selected all the studied apps from US App Stores. Further research with a multi country design and a more important number of apps to analyze is the real solution to validate these results.
Conclusion
mHealth apps could provide seamless access to adapted and context oriented health information and have the potential to decrease global health burdens. However, despite these promising potentials, there are some barriers and risks that prevent the users to trust mHealth apps. Recognizing these elements by all the stakeholders including app providers, app stores and users may lead to removal of these risks step by step. We are faced with a plethora and diversity of available mHealth apps. Therefore, implications for assuring the quality, security and privacy seem to be unclear and complex. Our study shows that the current situation of mHealth apps in general is not yet enough mature to be used widely and recommended by health professionals in the US market. Further research and development efforts are required to facilitate the wide range integration of mHealth apps in the real clinical pathways. These efforts could be designed in various axes including disseminating related guidelines for the users or app developers, implementing regulatory certification programs, designing adapted studies to reveal clinical evidence of mHealth apps considering the fast-paced nature of technology, and educating and encouraging app providers to protect their apps from information security and privacy and to test the usability and ergonomic aspects of their apps. Taking the right strategies in the future will help to benefit from the potential of mHealth apps to transform and improve the health care ecosystem and limit the barriers and risks.
Table 1.
Characteristics description of the health apps available on the US market.
 |
 |
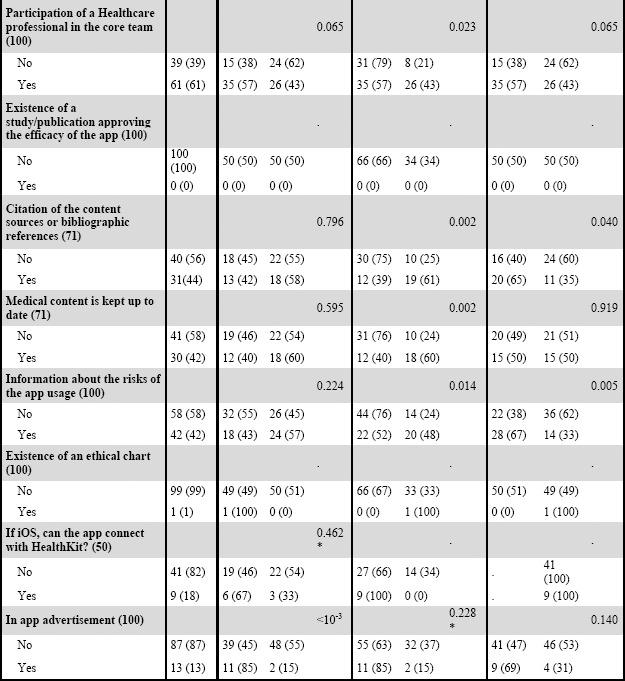 |
* with Yates correction, C: Consumers, HP: Healthcare Professionals
References
- 1.Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Med. 2013;10(1):e1001363. doi: 10.1371/journal.pmed.1001363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boulos MNK, Brewer AC, Karimkhani C, Buller DB, Dellavalle RP. Mobile medical and health apps: state of the art, concerns, regulatory control and certification. Online J Public Health Inform. 2014;5(3):229. doi: 10.5210/ojphi.v5i3.4814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yasini M, Marchand G. Toward a use case based classification of mobile health applications. Stud Health Technol Inform. 2015;210:175–9. [PubMed] [Google Scholar]
- 4.research2guidance - The mHealth apps market is getting crowded. [Internet] [cited 2017 Feb 28]. Available from: https://research2guidance.com/mhealth-app-market-getting-crowded-259000-mhealth-apps-now/
- 5.Becker S, Miron-Shatz T, Schumacher N, Krocza J, Diamantidis C, Albrecht U-V. mHealth 2.0: Experiences, Possibilities, and Perspectives. JMIR MHealth UHealth. 2014;2(2):e24. doi: 10.2196/mhealth.3328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de la Vega R, Miro J. mHealth: A Strategic Field without a Solid Scientific Soul. A Systematic Review of Pain-Related Apps. [cited 2014 Nov 28];PLoS ONE [Internet] 2014 Jul 7;9(7) doi: 10.1371/journal.pone.0101312. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085095/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lewis TL, Wyatt JC. mHealth and Mobile Medical Apps: A Framework to Assess Risk and Promote Safer Use. J Med Internet Res. 2014 Sep 15;16(9):e210. doi: 10.2196/jmir.3133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buijink AWG, Visser BJ, Marshall L. Medical apps for smartphones: lack of evidence undermines quality and safety. Evid Based Med. 2013 Jun;18(3):90–2. doi: 10.1136/eb-2012-100885. [DOI] [PubMed] [Google Scholar]
- 9.McCartney M. How do we know whether medical apps work? BMJ. 2013;346:f1811. doi: 10.1136/bmj.f1811. [DOI] [PubMed] [Google Scholar]
- 10.Cummings E, Borycki EM, Roehrer E. Issues and considerations for healthcare consumers using mobile applications. Stud Health Technol Inform. 2013;183:227–31. [PubMed] [Google Scholar]
- 11.O’Neill S, Brady RR. Clinical involvement and transparency in medical apps; not all apps are equal. Colorectal Dis Off J Assoc Coloproctology G B Irel. 2013 Jan;15(1):122. doi: 10.1111/codi.12086. [DOI] [PubMed] [Google Scholar]
- 12.Visvanathan A, Hamilton A, Brady RRW. Smartphone apps in microbiology--is better regulation required? Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2012 Jul;18(7):E218–220. doi: 10.1111/j.1469-0691.2012.03892.x. [DOI] [PubMed] [Google Scholar]
- 13.Wolf JA, Moreau JF, Akilov O, Patton T, English JC, Ho J, et al. Diagnostic inaccuracy of smartphone applications for melanoma detection. JAMA Dermatol. 2013 Apr;149(4):422–6. doi: 10.1001/jamadermatol.2013.2382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferrero NA, Morrell DS, Burkhart CN. Skin scan: a demonstration of the need for FDA regulation of medical apps on iPhone. J Am Acad Dermatol. 2013 Mar;68(3):515–6. doi: 10.1016/j.jaad.2012.10.045. [DOI] [PubMed] [Google Scholar]
- 15.Demidowich AP, Lu K, Tamler R, Bloomgarden Z. An evaluation of diabetes self-management applications for Android smartphones. J Telemed Telecare. 2012 Jun;18(4):235–8. doi: 10.1258/jtt.2012.111002. [DOI] [PubMed] [Google Scholar]
- 16.McKinstry B. Currently available smartphone apps for asthma have worrying deficiencies. Evid Based Med. 2013 Jan 10;18(5):e45–e45. doi: 10.1136/eb-2012-101194. [DOI] [PubMed] [Google Scholar]
- 17.Yasini M, Marchand G. Mobile Health Applications, in the Absence of an Authentic Regulation, Does the Usability Score Correlate with a Better Medical Reliability? Stud Health Technol Inform. 2015;216:127–31. [PubMed] [Google Scholar]
- 18.Yasini M, Beranger J, Desmarais P, Perez L, Marchand G. mHealth Quality: A Process to Seal the Qualified Mobile Health Apps. Stud Health Technol Inform. 2016;228:205–9. [PubMed] [Google Scholar]
- 19.Mobile Medical Applications Guidance for Industry and Food and Drug Administration Staff [Internet] FDA. 2015. Available from: http://www.fda.gov/downloads/MedicalDevices/…/UCM263366.pdf.
- 20.Saeedi MG, Kalhori SRN, Nouria R, Yasini M. Persian mHealth Apps: A Cross Sectional Study Based on Use Case Classification. Stud Health Technol Inform. 2016;228:230–4. [PubMed] [Google Scholar]
- 21.Dehling T, Gao F, Schneider S, Sunyaev A. Exploring the Far Side of Mobile Health: Information Security and Privacy of Mobile Health Apps on iOS and Android. JMIR MHealth UHealth. 2015 Jan 19;3(1):e8. doi: 10.2196/mhealth.3672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martinez-Pérez B, de la Torre-Díez I, López-Coronado M. Privacy and security in mobile health apps: a review and recommendations. J Med Syst. 2015 Jan;39(1):181. doi: 10.1007/s10916-014-0181-3. [DOI] [PubMed] [Google Scholar]
- 23.Singh K, Drouin K, Newmark LP, Rozenblum R, Lee J, Landman A, et al. Developing a Framework for Evaluating the Patient Engagement, Quality, and Safety of Mobile Health Applications. Issue Brief Commonw Fund. 2016 Feb;5:1–11. [PubMed] [Google Scholar]
- 24.Hamilton AD, Brady RRW. Medical professional involvement in smartphone “apps” in dermatology. Br J Dermatol. 2012 Jul;167(1):220–1. doi: 10.1111/j.1365-2133.2012.10844.x. [DOI] [PubMed] [Google Scholar]
- 25.Mobasheri MH, Johnston M, King D, Leff D, Thiruchelvam P, Darzi A. Smartphone breast applications - what’s the evidence? Breast Edinb Scotl. 2014 Oct;23(5):683–9. doi: 10.1016/j.breast.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 26.Powell AC, Torous J, Chan S, Raynor GS, Shwarts E, Shanahan M, et al. Interrater Reliability of mHealth App Rating Measures: Analysis of Top Depression and Smoking Cessation Apps. JMIR MHealth UHealth. 2016;4(1):e15. doi: 10.2196/mhealth.5176. [DOI] [PMC free article] [PubMed] [Google Scholar]


