Abstract
Introduction:
Pain of endodontic origin is of concern to both the patient and the clinician. Expectation of a painful experience can increase the patient's anxiety levels, making treatment more difficult. Management of endodontic pain is one of the challenging aspects in endodontics.
Objective:
To evaluate whether the intraligamentary mode of administration of diclogfenac sodium is effective in abating endodontic pain during interappointment visits.
Aim:
The purpose of this clinical trial is to evaluate the analgesic efficacy of diclofenac sodium administered through oral and intraligamentary routes in reducing postendodontic pain.
Materials and Methods:
Thirty patients were randomly allocated into three groups. Group A – placebo (Vitamin B12), Group B – diclofenac sodium (intraligamentary), and Group C – diclofenac sodium tablets. The tablets were given 30 min before the start of the procedure, while the intraligamentary injection was administered before commencing the endodontic procedure. The visual analog scale was used to evaluate the pain score at baseline and 6, 12, 24, and 48 h postoperatively.
Results:
Prophylactic intraligamentary injection of diclofenac sodium was found to be highly effective in reducing postendodontic pain than the oral route of administration.
Conclusion:
In patients with low pain threshold, intraligamentary route of administration is effective in controlling pain of endodontic origin postoperatively.
Keywords: Diclofenac sodium, endodontic treatment, interappointment pain, intraligamentary injection, oral tablet
INTRODUCTION
Interappointment pain is an unavoidable sequel to endodontic treatment. Causative factors include mechanical, chemical, and microbial injuries to the pulp and the periradicular tissues that are induced or exacerbated by root canal treatment. Onset of pain may be within few hours and lasts up to 48 h.[1,2] Anxiety, apprehension, fear of dental treatment, and other psychological factors influence the patients' pain perception and reaction thresholds.[2] A correlation has been indicated between the presence of apprehension before endodontic treatment and postoperative pain.[3,4] Literature reveals that nearly 80% of the patients reporting with a complaint of preoperative pain also experienced severe postoperative pain.[5] Overinstrumentation, periapical extrusion of irrigant/medicament, and restoration in hyperocclusion are chief causes that often provoke an acute inflammatory response, resulting in a mid-treatment flare-up.[4,6,7,8] Anti-inflammatory analgesics, systemic steroids, and anxiolytics are few of the commonly used preoperative drugs used during endodontic practice.[9] Pretreatment analgesia has been defined as an antinociceptive treatment that prevents altered processing of afferent input amplifying postoperative pain.[10] This technique may decrease the establishment of central sensitization, a mechanism whereby spinal neurons increase their responsiveness to peripheral nociceptive input.[11]
The purpose of this clinical trial is to evaluate the analgesic efficacy of diclofenac sodium administered through various routes in reducing postendodontic pain.
MATERIALS AND METHODS
Ethical approval was obtained from the ethical committee of the university. Thirty patients who visited the postgraduate clinic in the department of conservative dentistry and endodontics were enrolled in the study after assessing the criteria for inclusion. The research was approved by the institutional review board according to the national and international specifications.
Criteria for inclusion:
Vital pulp in need of endodontic therapy
Irreversible pulpitis in molar teeth
Age – 18–65 years.
Criteria for exclusion:
History of systemic diseases
History of allergy to nonsteroidal anti-inflammatory drugs (NSAIDs)
Radiographic evidence of periapical pathosis
Pregnant or lactating mothers.
Medical history was recorded and only those patients with no history of systemic illness were considered for this clinical trial. Pulp vitality was determined using thermal testing – heat and cold – followed by an electric pulp tester. Informed consent was obtained from the patients in both English and the regional language in which they were familiar with. The patients who fulfilled all the criteria for inclusion were then randomly divided into three groups by a sequentially numbered, opaque, sealed envelope method.
Group A – Placebo (Vitamin B12 tablets) – Neurobion Forte
Group B – Intraligamentary route of diclofenac sodium (Voveran)
Group C – Oral diclofenac sodium (Voveran 75 mg).
Based on the groups assigned, the patients in Groups A and C were given tablets 30 min before the commencement of endodontic therapy while patients assigned to Group B were administered intraligamentary injection before commencing the procedure.
All the patients were anesthetized with standard injections 1.8 ml of 2% lidocaine containing 1:80000 epinephrine. The tooth was isolated with the help of a rubber dam. Access opening was done with a Endo-Access Bur (Dentsply Maillefer, Ballaigues, Switzerland), and after locating the orifices, the working lengths were determined for each individual canal with an electronic apex locator (Root ZX, Morita, Tokyo, Japan). The canals were instrumented using Gates Glidden Drills, stainless steel hand K-files, and ProTaper rotary files (Dentsply Maillefer, Ballaigues, Switzerland). All canals were enlarged to the size of a #25 file and continuously irrigated using 3% sodium hypochlorite. The canals were dried with paper points, and calcium hydroxide (RC Cal, Prime Dental) was applied as a medicament for 7 days. Endodontic treatment was performed by the same endodontist. The visual analog scale was used to measure the pain level at baseline and 6, 12, 24, and 48 h postoperatively. A rescue prescription of analgesic (paracetamol 500 mg) was prescribed, and the patients were instructed to take it if they experienced pain and inform the reviewer while assessing the pain score. The intensity of pain after treatment was recorded by a blinded reviewer and was statistically analyzed.
Statistical analysis
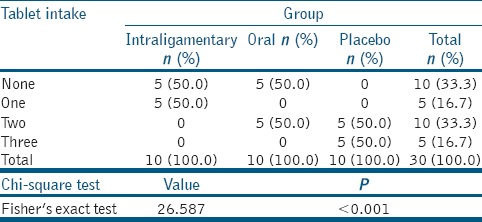
The normality test (Shapiro–Wilk tests and Kolmogorov–Smirnov) results revealed that variable did not follow normal distribution. Therefore, to analyze the data, nonparametric methods were applied. To compare visual analog scale (VAS) pain scores between groups, Kruskal–Wallis test was used followed by Bonferroni adjusted Mann–Whitney test for multiple pairwise comparison [Table 1]. To compare VAS pain scores between time points, Friedman's test for repeated measures was applied, and Kruskal–Wallis test was used followed by adjusted test for multiple pairwise comparison [Table 2]. To compare proportions between study and control groups, Chi-square test is applied; if any expected cell frequency is <5, Fisher's exact test is used [Table 3]. SPSS (IBM SPSS Statistics for Windows, Version 22.0, Armonk, NY:IBM CORP. Released 2013) was used to analyze the data. Significance level was fixed as 5% (α = 0.05) (if P < 0.05, then statistically significant).
Table 1.
Kruskal-Wallis test
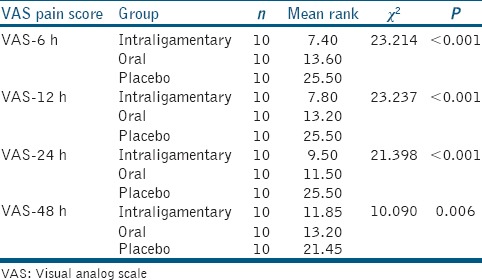
Table 2.
Friedman's test for repeated measures to compare values between time points in each group
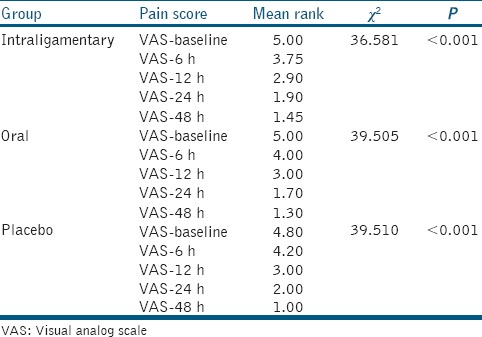
Table 3.
Chi-square test to compare proportions of tablet intake after 48 h
RESULTS
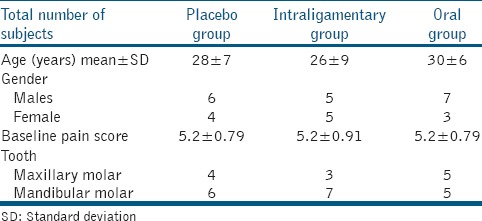
The age, gender, mean initial VAS scores, and tooth type were tabulated, and there were no significant differences (P > 0.05) among the three groups [Table 4].
Table 4.
Comparison of age, gender, and initial visual analog scale scores among the three groups
The results showed that there was a statistical difference in the reduction of pain score among the three groups and within the time periods. The decrease in the median pain score among the three groups is represented Graph 1.
Graph 1.
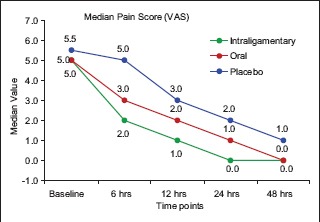
Decrease in median pain score among the three groups
DISCUSSION
Perception of pain is highly subjective and influenced by many factors, which make the precise definition of different discomfort categories and detailed description of pain difficult.[12] While pain during therapy is usually controlled by local anesthesia, postoperative pain control is often and may contribute to the development of hyperalgesia leading to increase in pain later.[13,14] Pain control in endodontic patients should be efficacious with minimum side effects. Posttreatment pain in endodontics had been reported to occur in 25%–40% of all endodontic patients.[11] Most of the investigators have found that there is a strong relationship between preoperative and postoperative pain.[4,15,16]
Evaluation of pain intensity was done using the verbal descriptor scale as well as visual analog scale ranged from 0 to 10.[17] Patients who experienced moderate-to-severe pain were included as preoperative pain has been established as a major determinant of postoperative pain or flare-up.[1,18] Most of the patients experienced pain in the first 24 h after initiation of root canal treatment.[4] Therefore, 48 h period for assessment was chosen in this study even though the drugs tested would not be expected to provide ongoing analgesia for this entire period owing to their relative short plasma half-lives.
Endodontic treatment can cause the release of inflammatory mediators into the surrounding periapical tissues.[19] Thus, pain fibers are directly stimulated or sensitized by prostaglandins in situ.[20] In addition, the vascular dilation and increased permeability as consequences of periradicular inflammation cause edema and increased interstitial tissue response.[19] Considering the role of prostaglandins on endodontic pain, a possible strategy for reduction of postoperative endodontic pain might be the local use of an anti-inflammatory agents adjacent to the inflamed tooth to decrease the production of inflammatory mediators[19,21] and improve the efficacy of local anesthetics.
Various methods have been advocated to reduce pain, namely opioids, glucocorticoids, long-acting local anesthetics, and NSAIDs. For pain of moderate intensity, NSAIDs are prescribed. Diclofenac sodium is a NSAID that acts by inhibition of prostaglandin synthesis by inhibition of cyclooxygenase pathway. It also exhibits bacteriostatic action by inhibition of bacterial DNA synthesis.[22] The onset of action of diclofenac sodium is 10 min, and as the drug persists in the tissue fluids for 11 h, the action of a single dose is for 6–8 h, which is the half-life of the drug.[23]
Anesthetizing tooth with irreversible pulpitis poses a challenge as the voltage-gated sodium channels are resistant to local anesthetic relatively.[24] Sodium channels are sensitized by prostaglandins that suggest that pretreatment administration increases the efficacy of local anesthetic in patients with odontogenic pain.[25,26] Prostaglandins lower the activation threshold and increase the flow of sodium ions in the channel by sensitization of the tetrodotoxin-resistant channels.[27]
Oral route of diclofenac sodium administration is known to cause gastrointestinal problems; thus, intraligamentary injection helps overcome this side effect.[24] The intraligamentary route helps bypass the first-pass metabolism in the liver; thus, the availability of the drug is 100% at the odontogenic region while the bioavailability of the oral route of administration is around 50% due to the first-pass metabolism in the liver. Combination of inferior alveolar nerve block and intraligamentary injection of diclofenac sodium helps in significantly reducing pain due to the anti-inflammatory action of the drug that helps in reducing the inflammatory mediators, thereby reducing the pain.[24] Intraligamentary injections pose the risk of prolonged ischemia of the interdental papilla, followed by sloughing and exposure of the crestal bone along with swelling and discoloration of the soft tissues.[11,28] No such complication was experienced during the course of this study.
Pain intensity was evaluated using the visual analog scale as this scale has been used in most of the previous studies that analyzed pain after endodontic treatment.[4,6,29,30,31] Limitations of the visual analog scale included providing it on paper or electronically. The failure of VAS is between 4% and 11%, but it can be eliminated if the tool is carefully explained to the patients.[30,32]
Further research must be undertaken with a larger sample size and by comparing with other NSAIDs by the routes of administration to zero in on the drug and mode of administration for effective interappointment pain relief in endodontic treatment.
CONCLUSION
Within the limitations of this study, it can be concluded that diclofenac sodium is effective in allaying the endodontic pain experienced by the patients and intraligamentary route of delivery is more efficacious in abating pain for up to 48 h.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Torabinejad M, Kettering JD, McGraw JC, Cummings RR, Dwyer TG, Tobias TS, et al. Factors associated with endodontic interappointment emergencies of teeth with necrotic pulps. J Endod. 1988;14:261–6. doi: 10.1016/S0099-2399(88)80181-X. [DOI] [PubMed] [Google Scholar]
- 2.Seltzer S, Naidorf IJ. Flare-ups in endodontics: I. Etiological factors 1985. J Endod. 2004;30:476–81. doi: 10.1097/00004770-200407000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Morse DR, Koren LZ, Esposito JV, Goldberg JM, Belott RM, Sinai IH, et al. Asymptomatic teeth with necrotic pulps and associated periapical radiolucencies: Relationship of flare-ups to endodontic instrumentation, antibiotic usage and stress in three separate practices at three different time periods. Int J Psychosom. 1986;33:5–87. [PubMed] [Google Scholar]
- 4.Torabinejad M, Cymerman JJ, Frankson M, Lemon RR, Maggio JD, Schilder H, et al. Effectiveness of various medications on postoperative pain following complete instrumentation. J Endod. 1994;20:345–54. doi: 10.1016/S0099-2399(06)80098-1. [DOI] [PubMed] [Google Scholar]
- 5.Ali SG, Mulay S, Palekar A, Sejpal D, Joshi A, Gufran H, et al. Prevalence of and factors affecting post-obturation pain following single visit root canal treatment in Indian population: A prospective, randomized clinical trial. Contemp Clin Dent. 2012;3:459–63. doi: 10.4103/0976-237X.107440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Attar S, Bowles WR, Baisden MK, Hodges JS, McClanahan SB. Evaluation of pretreatment analgesia and endodontic treatment for postoperative endodontic pain. J Endod. 2008;34:652–5. doi: 10.1016/j.joen.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 7.Genet JM, Hart AA, Wesselink PR, Thoden van Velzen SK. Preoperative and operative factors associated with pain after the first endodontic visit. Int Endod J. 1987;20:53–64. doi: 10.1111/j.1365-2591.1987.tb00590.x. [DOI] [PubMed] [Google Scholar]
- 8.Gyanani H, Chhabra N, Parmar GR. Comparative assessment of efficacy of two different pretreatment single oral doses of betamethasone on inter-appointment and postoperative discomfort: An in vivo clinical evaluation. J Conserv Dent. 2016;19:564–8. doi: 10.4103/0972-0707.194022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sethi P, Agarwal M, Chourasia HR, Singh MP. Effect of single dose pretreatment analgesia with three different analgesics on postoperative endodontic pain: A randomized clinical trial. J Conserv Dent. 2014;17:517–21. doi: 10.4103/0972-0707.144574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kissin I. Preemptive analgesia. Anesthesiology. 2000;93:1138–43. doi: 10.1097/00000542-200010000-00040. [DOI] [PubMed] [Google Scholar]
- 11.Joshi N, Mathew S, George JV, Hegde S, Bhandi S, Madhu KS, et al. Comparative evaluation of the efficacy of two modes of delivery of Piroxicam (Dolonex(®)) for the management of postendodontic pain: A randomized control trial. J Conserv Dent. 2016;19:301–5. doi: 10.4103/0972-0707.186454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mulhern JM, Patterson SS, Newton CW, Ringel AM. Incidence of postoperative pain after one-appointment endodontic treatment of asymptomatic pulpal necross in single-rooted teeth. J Endod. 1982;8:370–5. doi: 10.1016/s0099-2399(82)80197-0. [DOI] [PubMed] [Google Scholar]
- 13.Gordon SM, Dionne RA, Brahim J, Jabir F, Dubner R. Blockade of peripheral neuronal barrage reduces postoperative pain. Pain. 1997;70:209–15. doi: 10.1016/s0304-3959(96)03315-5. [DOI] [PubMed] [Google Scholar]
- 14.Gordon SM, Brahim JS, Rowan J, Kent A, Dionne RA. Peripheral prostanoid levels and nonsteroidal anti-inflammatory drug analgesia: Replicate clinical trials in a tissue injury model. Clin Pharmacol Ther. 2002;72:175–83. doi: 10.1067/mcp.2002.126501. [DOI] [PubMed] [Google Scholar]
- 15.Genet JM, Wesselink PR, Thoden van Velzen SK. The incidence of preoperative and postoperative pain in endodontic therapy. Int Endod J. 1986;19:221–9. doi: 10.1111/j.1365-2591.1986.tb00482.x. [DOI] [PubMed] [Google Scholar]
- 16.Harrison JW, Baumgartner JC, Svec TA. Incidence of pain associated with clinical factors during and after root canal therapy. Part 2. Postobturation pain. J Endod. 1983;9:434–8. doi: 10.1016/S0099-2399(83)80259-3. [DOI] [PubMed] [Google Scholar]
- 17.Makkar S, Kaler N, Dhawan R, Mann N, Pasricha S. Efficacy of ibuprofen and paracetamol and diclofenac sodium and paracetamol combination on postoperative pain following root canal preparation in a randomized placebo-controlled study. Indian J Oral Sci. 2012;3:19. [Google Scholar]
- 18.Walton R, Fouad A. Endodontic interappointment flare-ups: A prospective study of incidence and related factors. J Endod. 1992;18:172–7. doi: 10.1016/S0099-2399(06)81413-5. [DOI] [PubMed] [Google Scholar]
- 19.Mehrvarzfar P, Shababi B, Sayyad R, Fallahdoost A, Kheradpir K. Effect of supraperiosteal injection of dexamethasone on postoperative pain. Aust Endod J. 2008;34:25–9. doi: 10.1111/j.1747-4477.2007.00076.x. [DOI] [PubMed] [Google Scholar]
- 20.Shahi S, Mokhtari H, Rahimi S, Yavari HR, Narimani S, Abdolrahimi M, et al. Effect of premedication with ibuprofen and dexamethasone on success rate of inferior alveolar nerve block for teeth with asymptomatic irreversible pulpitis: A randomized clinical trial. J Endod. 2013;39:160–2. doi: 10.1016/j.joen.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 21.Aggarwal V, Singla M, Rizvi A, Miglani S. Comparative evaluation of local infiltration of articaine, articaine plus ketorolac, and dexamethasone on anesthetic efficacy of inferior alveolar nerve block with lidocaine in patients with irreversible pulpitis. J Endod. 2011;37:445–9. doi: 10.1016/j.joen.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 22.Penniston SG, Hargreaves KM. Evaluation of periapical injection of ketorolac for management of endodontic pain. J Endod. 1996;22:55–9. doi: 10.1016/S0099-2399(96)80272-X. [DOI] [PubMed] [Google Scholar]
- 23.Fowler PD, Shadforth MF, Crook PR, John VA. Plasma and synovial fluid concentrations of diclofenac sodium and its major hydroxylated metabolites during long-term treatment of rheumatoid arthritis. Eur J Clin Pharmacol. 1983;25:389–94. doi: 10.1007/BF01037953. [DOI] [PubMed] [Google Scholar]
- 24.Raksha B, Ganesh B, Shetty A, Shruti B, Hegde M. Evaluation of the efficiency of intraligamentary diclofenac sodium in reducing post operative endodontic pain in patients with irreversible pulpitis. Int Res J Pharm. 2013;3:237. [Google Scholar]
- 25.Clem WH. Posttreatment endodontic pain. J Am Dent Assoc. 1970;81:1166–70. doi: 10.14219/jada.archive.1970.0364. [DOI] [PubMed] [Google Scholar]
- 26.Gold MS, Reichling DB, Shuster MJ, Levine JD. Hyperalgesic agents increase a tetrodotoxin-resistant Na+current in nociceptors. Proc Natl Acad Sci U S A. 1996;93:1108–12. doi: 10.1073/pnas.93.3.1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hargreaves KM, Reader AL, Nusstein JM, Marshall G, Gibbs JL. Pharmacologic management of endodontic pain. In: Ingles JI, Bakland LK, Baumgartner JC, editors. Ingle's Endodontics. 6th ed. Hamilton: B.C. Decker Inc; 2008. pp. 721–3. [Google Scholar]
- 28.Atbaei A, Mortazavi N. Prophylactic intraligamentary injection of piroxicam (feldene) for the management of post-endodontic pain in molar teeth with irreversible pulpitis. Aust Endod J. 2012;38:31–5. doi: 10.1111/j.1747-4477.2010.00274.x. [DOI] [PubMed] [Google Scholar]
- 29.Ryan JL, Jureidini B, Hodges JS, Baisden M, Swift JQ, Bowles WR, et al. Gender differences in analgesia for endodontic pain. J Endod. 2008;34:552–6. doi: 10.1016/j.joen.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 30.Metri M, Hegde S, Bhandi S. Effect of pretreatment diclofenac sodium on postendodontic pain: A randomised controlled trial. J Conserv Dent. 2016;19:7–10. doi: 10.4103/0972-0707.173183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Menhinick KA, Gutmann JL, Regan JD, Taylor SE, Buschang PH. The efficacy of pain control following nonsurgical root canal treatment using ibuprofen or a combination of ibuprofen and acetaminophen in a randomized, double-blind, placebo-controlled study. Int Endod J. 2004;37:531–41. doi: 10.1111/j.1365-2591.2004.00836.x. [DOI] [PubMed] [Google Scholar]
- 32.Williamson A, Hoggart B. A review of three commonly used pain rating scales. J Clin Nurs. 2005;14:798–804. doi: 10.1111/j.1365-2702.2005.01121.x. [DOI] [PubMed] [Google Scholar]


