Supplemental Digital Content is available in the text.
Abstract
Importance:
Understanding what drives breast cancer (BC) patient’s surgical decision-making and why, as survival continues to improve, are women continuing to choose mastectomy in increasing numbers.
Objective:
We sought to understand better what drives patient choice in surgical decision-making regarding BC treatment options.
Design:
We used a dynamic model, adaptive conjoint–based survey experiment, to assess multiple factors concurrently impacting patient choice, conducted from December 2016 to January 2017 using the Army of Women.
Setting:
Army of Women, is a U.S.–based nation-wide registry of women, both healthy and previous BC patients.
Participants:
An e-mail invitation was sent to the AWOL’s 108,933 members, with 1,233 signing up to participate and 858 responding (548 healthy, 310 previous BC). Two hundred thirty-nine BC patients who underwent treatment > 5 years were excluded due to potential recall bias and changes in BC treatment paradigms. All subjects who did not complete the adaptive conjoint–based survey were also excluded due to inability to calculate preferences. The final sample consisted of 522 healthy women and 71 previous BC patients.
Interventions or Exposures:
Study of patient preference and decision drivers, without, interventions or exposures.
Main Outcome(s) and Measure(s):
Shares of preferences for various surgical treatment options were calculated using the highest-ranked factors, by the importance that drove patient decision-making.
Results:
Survey response rate was 69.5%. Among healthy women, the most important of the 9 factors in making a surgical choice were doctor’s recommendation at 21.4% (SD, 13.6%) and overall survival (OS) at 20.5% (SD, 9.8%) while among previous BC patients, the most important factor was OS at 19% (SD, 9%) and doctor’s recommendation at 17.2% (SD, 10.3%).
Conclusion and Relevance:
While OS accounted for the largest single driver of patient choice at ~20 %, it is notable that 80% of patient decision-making was driven by factors unrelated to survival such as cost, intensity and recovery time, and breast image. By understanding what drives choice, we can provide better patient-centric education and treatments.
BACKGROUND
Breast cancer (BC) is the most common type of cancer, accounting for nearly 14.6%1 of all newly diagnosed cancers in the United States with an estimated 249,6601 new cases in 2016. The median age at diagnosis was 61 years, with 19% of women younger than 50 years.2 The 5-year relative survival for BC (2006–2012) 89.7%1 with estimated deaths from BC in 2016 at 40,450,1 representing 6.8%1 of all cancer deaths.
While survival for BC has improved dramatically over the past 20 years, in large part due to improved systemic therapies and earlier stage at diagnosis, surgery remains the cornerstone of BC care.3 Without addressing the axilla, there are 2 basic surgical approaches (1) breast-conserving surgery (BCS) and (2) mastectomy.2 BCS is the preservation of the breast and combines lumpectomy with breast radiation,2 producing similar survival to mastectomy.4 Mastectomy is the removal of the entire breast gland with variations on the degree of skin preservation. There are 3 basic types of mastectomy: (1) simple mastectomy, (maximal removal of overlying skin), (2) skin-sparing mastectomy, preservation of the skin envelope less the nipple areolar complex; and (3) nipple-sparing mastectomy, preservation of the entire skin envelope.2
While the treatment options for BC continue to expand the decision-making process for the patient becomes more complex. There is a multitude of emotions and concerns anyone diagnosed with BC must face, compounding the difficulty of decision-making. Most other cancers (eg, bowel, ovarian, or lung) have almost no choice in surgical approach beyond to proceed or not and perhaps minimally invasive versus open techniques; the extent of tissue to be removed is determined by the surgeon.5
BC is salient in its impact on a patient’s sense of wellbeing and attractiveness.6,7 Asymmetry can be very significant to some and less important to others.8 The endeavors to both understand the biology of the disease and the impact of BC surgery was played out in the 1970s to 1990s as treatment transitioned9 from the Halstead radical mastectomy to the BCS of today, primarily due to Dr. Bernard Fisher’s National Surgical Adjuvant Breast Project clinical trials B-0410 and B-06.11
So, even with the improvements in treatment and survival, why do we continue to see more women not only choosing mastectomy,12 but also contralateral prophylactic mastectomy?13 Current evidence suggests several factors that may be leading to increased use of more aggressive surgical treatments including younger age, race, higher education levels, and increased peace of mind.13 We need to ask where our patients fit into our decision-making and what endpoints should be used when considering the risks and benefits of treatment. Is survival the only benefit that matters? Given the evidence shows similar survival for most patient populations, regardless of surgical treatment approach,4 BCS or mastectomy, what is driving patient choice? It is unclear whether patients understand their treatment options and the trade-offs that accompany various surgical approaches. Are the options and information presented in ways that relate to patients? Are patients aware of the rights afforded by the Women’s Health and Cancer Rights Act14 of 1998?
There is a large amount of evidence around what factors may influence the choice for mastectomy, but the research has primarily been conducted in the form of simple surveys asking single questions15–18 or via decision-making tools19,20 evaluated for usefulness. Doctor’s recommendation, use of radiation, number of surgeries, educational status, and body image are just some of the factors influencing the decision-making process.13–18 Despite the usefulness of such research, the evidence to date cannot quantify the importance of such factors relative to each other.
How does a patient weight the importance of various factors, such as fear of recurrence, use of radiation, breast asymmetry, cost, and continued imaging? Which is more important and how do these factors, when combined, affect patient behavior and preference? Through an understanding of patient trade-offs for the choices of BCS or mastectomy, we can develop more patient-centric education. In this study, we sought to understand patient drivers of choice using an adaptive conjoint survey experiment. This technique is well established in the world of market research,21 assessing which variables impact consumer choice. However, it is a relatively new tool in medicine that has been used to measure preference for various health care activities like prevention, treatment, and education.22–25
Our objective was to assess which factors drive patient decisions in more “real-life” scenarios by conducting a conjoint analysis of BC surgical treatment decisions among a sample of healthy women and previous BC patients hypothetically undergoing the surgical treatment decision-making process.
METHODS
Data Source and Study Design
A web-based survey using an adaptive choice–based conjoint (ACBC) design was used to assess patients’ decision-making regarding the surgical treatment options for BC (see document, Supplemental Digital Content 1, which displays the ACBC Experiment, http://links.lww.com/PRSGO/A730).
The study was conducted between December 2016 and January 2017 using members of the Dr. Susan Love Research Foundation’s Army of Women (AoW).26 The AoW sent out invitation letters to enrolled members including healthy women and previous BC and obtained informed consent before participation. A reminder e-mail was sent a week into the survey. The study took between 45–60 minutes to complete, and the respondents received no compensation. Peace Health’s (Washington), institutional review board approved the study.
Survey Overview
ACBC allows for a more realistic representation of the decision-making process by incorporating a series of factors, each of which may have an impact on the decision process. It combines multiple factors (ie, survival, recurrence, breast look) at a time that act together to influence an individual’s decision-making process, thus better reflecting a real-world scenario where trade-offs must be made. Through several hypothetical scenarios, respondents select among surgical options with real-life variables to ascertain which factors are of greater influence on surgical decision-making. This technique uses computer-adaptive technology to hone-in on the factors that most strongly influence surgical decision-making. The ACBC technique has been successfully used to analyze a variety of health-related decisions. For example, the method was used to measure decisions to escalate care in patients with rheumatoid arthritis, evaluate physicians’ decisions to recommend spinal surgery, understand preferences of doctors and patients in the management of diabetes, and assess the importance of clinical and logistical factors regarding inter-hospital transport of critically ill patients.22–25 This study follows the International Society for Pharmacoeconomic and Outcomes Research.27
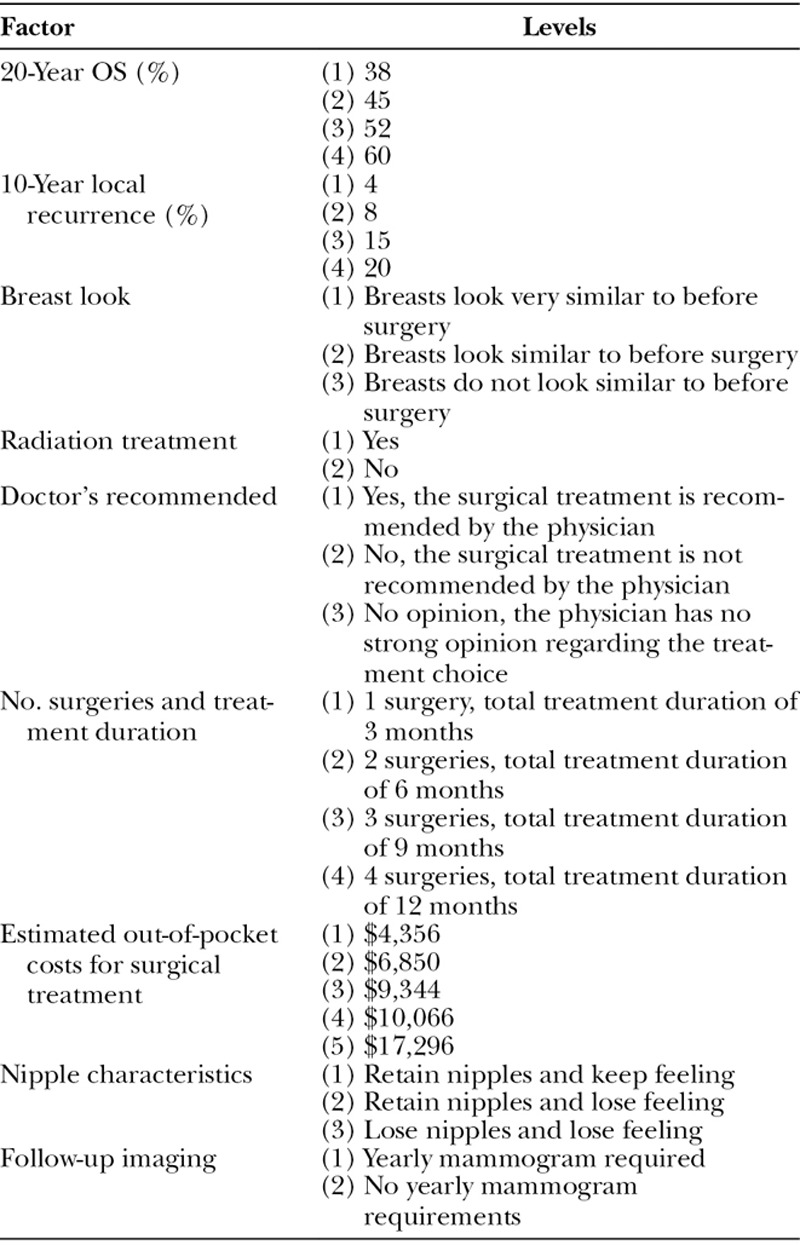
To identify the factors to include in our analysis, we used a focused literature review, patient feedback, and our experience in patient care. The review found several factors including—clinical (survival, recurrence),4,28–40 physical (breast symmetry, shape),41,42 psychosocial (femininity, attractiveness)43 and practical considerations (adjunct therapy, routine imaging, distance to treatment, out-of-pocket costs)15,44 as factors influencing BC surgery decision-making. We consolidated the list down to a total of 9 to keep the survey length manageable and maximize the value of the conjoint analysis.20 The final list of factors selected for inclusion is presented in Table 1 and includes the discrete values tested in the conjoint experiment. A standalone survey on patient demographics and characteristics as well as behaviors and attitudes regarding cancer was also inducted to complement the findings (see survey, Supplemental Digital Content 2, which displays the behavioral and attitudinal survey questions, http://links.lww.com/PRSGO/A731).
Table 1.
Treatment Factors and Levels
Sample Size and Statistical Analyses
The minimum sample size required to complete a conjoint analysis can depend on the number of factors. These may include the format of the questions, the complexity and desired precision of the results and any required subgroup analyses.27,45 Each participant completed 10 vignettes (t), with typically 3 treatment options, and all had ≤ 5 choices per factor, producing a sample size of n = 83 to conduct the primary analysis. Based on historical conjoint analyses, most studies range from about 150 to 1,200 respondents.46
Respondent demographics, characteristics, attitudes, and behaviors were presented as percentages. For the primary analysis of the importance of factors influencing surgical treatment decision, ACBC used Sawtooth software to calculate part-worth utilities to assess the preference for any factor in the context of varying levels of importance, that is, how important is symmetry when survival is held constant. The preference was then used to rank order the importance of each factor. Multiple scenarios were presented to respondents with 3 possible treatments using different inputs for the factors evaluated. Respondents selected the treatment they preferred for each scenario, and the findings were utilized to estimate the relative importance of each factor based on the selected treatment decision. The importance was expressed as a percentage (total, 100%) to reflect the proportion of the overall treatment decision that was accounted for by each factor.
Also, the part-worth utilities provide the ability to develop a predictive algorithm to estimate patient’s likely surgical choice, given their preference for other related factors. In other words, by assessing patient values, we are better able to predict their surgical choice. Thus, using the conjoint tool with values obtained from the survey respondents, a regression equation was constructed to simulate patient preference levels for hypothetical scenarios involving real-life surgical treatment options. Two separate analyses were conducted to test 2 scenarios, each including 4 unique surgical treatment options with varying levels of the factors described in Table 1. The options described represent factors that reflect potential surgical treatment options to help communicate how the combination of factors informs preference versus each factor measured alone.
RESULTS
Respondent Characteristics
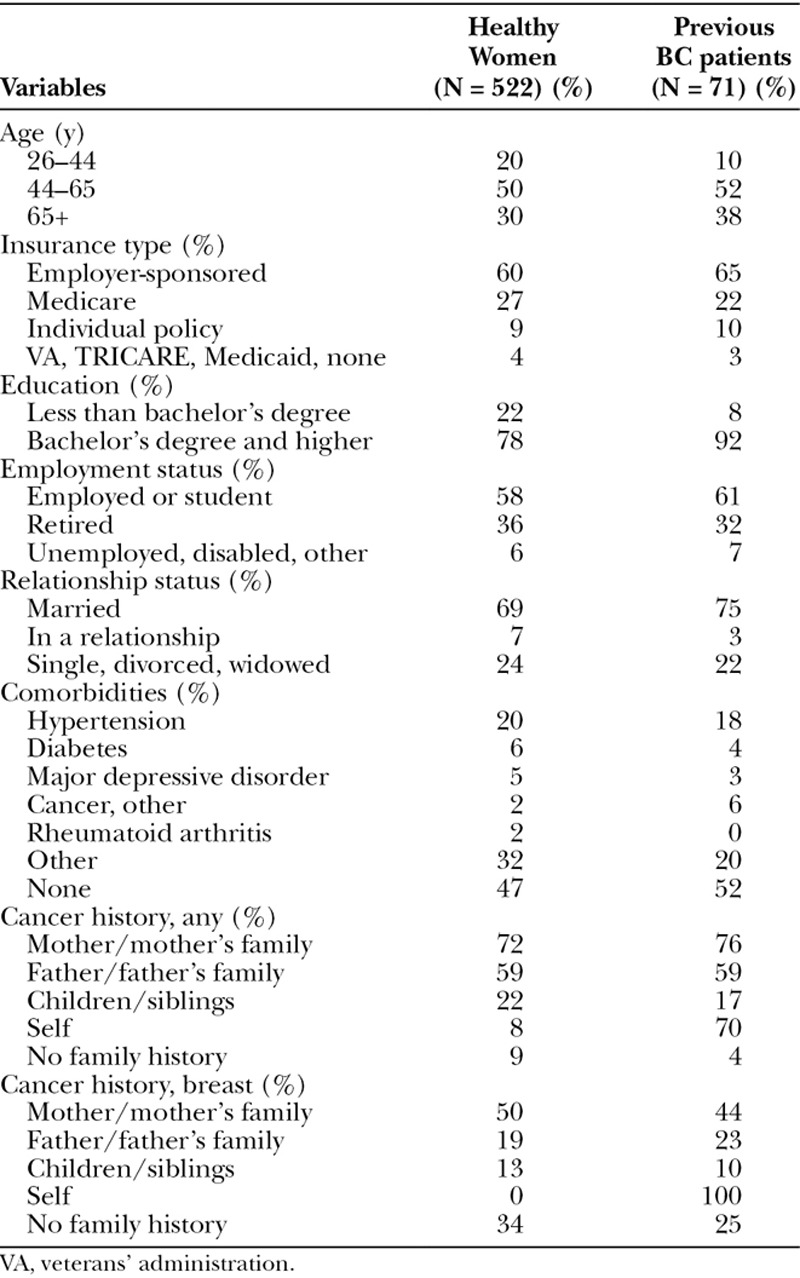
A total of 548 (522 completed all questions in the survey) healthy women and 310 (71 with surgery < 5 years and complete) previous BC patients completed the survey (see image, Supplemental Digital Content 3, which displays the participant flow diagram, http://links.lww.com/PRSGO/A732). Survey response rate was 69.5%. The average age was 55 years, and the majority were Caucasian (> 90%) across both groups, reflective of the 120,000-person AoW registry. Most respondents were employed and privately insured, and most (60–70%) had some family history of cancer. The respondents were from all over the United States, with the majority (~16%) from California. Additional demographics and characteristics are reported in Table 2.
Table 2.
Respondent Demographics and Characteristics
General Views and Beliefs
The majority (88%) of healthy respondents believed that cancers in general, could be cured only “sometimes” or “rarely.” Noted sources of information included medical practitioners (81%), family and friends (76%), internet (70%), media (television, newspapers, magazines; 57%), and cancer support groups (18.8%). Among previous BC respondents, the majority (73%) also believed that cancers in general could be cured only “sometimes” or “rarely.” Previous BC women had similar patterns of accessing information as healthy respondents, including medical practitioners (84%), family and friends (60%), internet (70%), media (10%), and cancer support groups (13%).
A summary of priorities for healthy and previous BC women is presented in Figure 1. Among healthy women, recurrence (92.8%), restrictions on mobility (82.3%), and ensuring financial security (72.4%) were the top concerns when making treatment decisions. Most (85%) healthy women respondents also indicated “very high” or “high” levels of confidence in predicted social support from friends and family. Extensive information gathering before decision-making was most preferred (87%) followed by the use of a “structured process” (11%). Overall, similar trends in priorities were reported among previous BC and healthy women. However, previous BC patients placed avoiding recurrence higher and importance and avoiding pain lower, in priority than did their healthy counterparts (Fig. 1B).
Fig. 1.
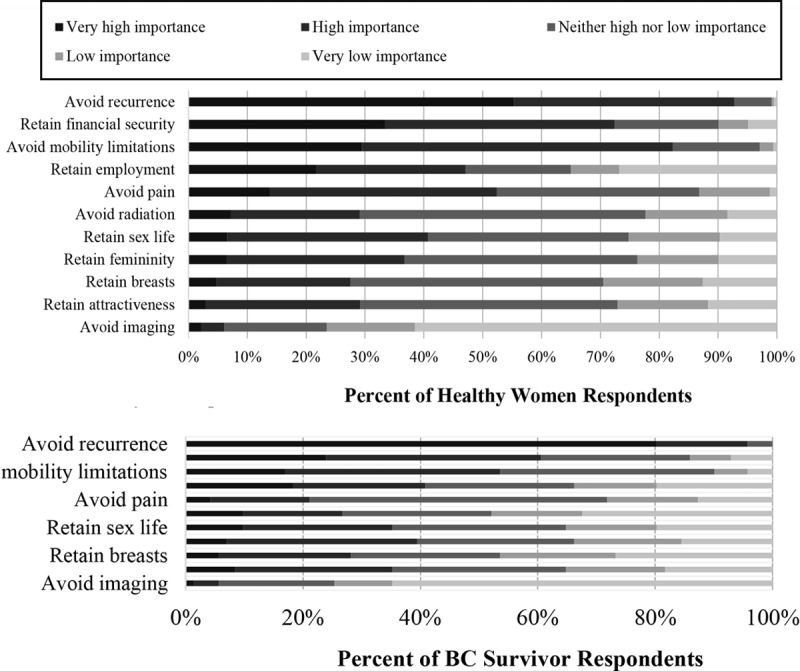
A, BC Treatment Priorities for Healthy Respondents (b) BC Treatment Priorities for Previous BC Respondents.
Importance of Factors
Based on the scenarios evaluated, the relative importance of each of the factors for the healthy women respondents, from highest to lowest, are reported in Figure 2. The findings indicate that doctor’s recommendation, 20-year survival, number of surgeries and recovery time, 10-year recurrence, and out-of-pocket costs, were the primary factors in selecting a surgical treatment, accounting for 21.35%, 20.48%, 14.26%, 14.00%, and 8.67%, respectively.
Fig. 2.
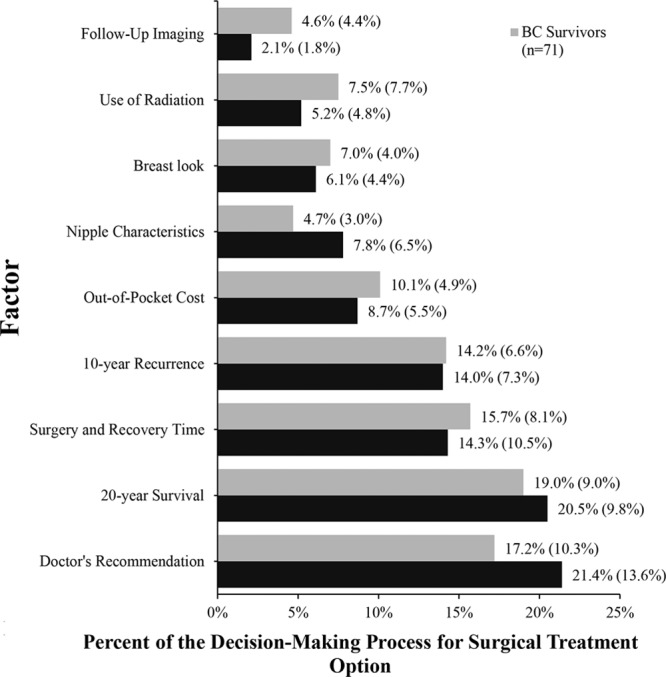
Mean (SD) Importance of Factors.
Among previous BC women, the overall relative importance of each of the factor was similar except previous BC women weighed survival highest (19%) and doctor’s recommendation second (17.2%). Also, these women allocated a numerically greater percentage of decision-making importance to avoiding follow-up imaging, radiation, and maintaining breast look. Previous BC women also assigned a lower importance to retaining nipples and nipple sensitivity relative to the healthy women. Stratifications by age, race, relationship status, employment status, and education level showed results that were consistent with the overall population indicating that the importance of various treatment factors held across different demographics.
Respondent Preference for Surgical Treatments
The focus of the analysis was to understand better what drives patient choice. This study allowed us to ascertain the importance of different factors and the impact of how these factors combine to drive and define patient preference. We combined, the part-worth utilities and weights of each factor estimated from the conjoint analysis experiment to provide a regression equation that can be used to simulate patient surgical preferences. Hypothetical surgical treatment options were broken into 2 analyses to demonstrate the diversity in responses. One analysis focused on health-related factors such as survival and recurrence while the other focused on nonhealth–related factors such as out of pocket costs, nipple preservation, and breast look. A list of the factors and levels defining each of the analyses and surgical treatment options can be found in Figures 3A, B.
Fig. 3.
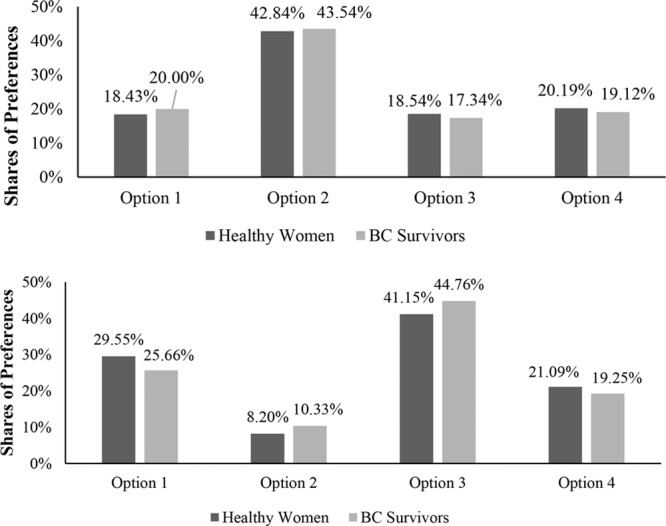
A, Preference for Hypothetical Surgical Decision When Changing Clinical Factors. B, Preference for Hypothetical Surgical Decision When Changing Non-Clinical Factors.
Assuming varying rates of 20-year survival, doctor’s recommendation, and recurrence while leaving other factors equal, the preferred surgical option was focused on reducing recurrence (option 2 at 43%) while the remaining options were equally preferred at ~18–20%. In contrast, with survival constant and varying the nonclinical factors such as out of pocket cost, the number of surgeries, and breast image, the preference was far more variable. If survival is held constant, the data (option 3 at 41%) suggests that the number of surgeries and out of pocket costs are the greatest patient drivers.
DISCUSSION
This analysis is unique and valuable in 2 ways: (1) it uses a dynamic statistical analysis (ACBC) to assess how a multitude of real-life factors interrelate to affect women’s surgical preference and decision-making; and (2) it looked at both women with and without a history of BC to assess how they would make decisions from a nonthreatening position of either never having had cancer or having already completed treatment. It represents a more realistic assessment of the multifaceted process influencing BC surgical decision-making. While our data agree with earlier published studies on patient choice, showing that survival, as expected, is the largest single driver of patient choice at 20%, the vast majority (80%) of decisions were based on nonclinical factors such as doctor’s recommendation, number of surgeries, recover, breast look, and out of pocket cost. While our study does not definitely address why the incidence of mastectomy continues to increase, it provides insights into factors that may be influencing this rise. Our study found that factors such as the risk of recurrence (~14% of treatment decision), use of radiation therapy (~7% of the treatment decision), and out of pocket costs (~9–10% of treatment decision) are likely factors influencing treatment choice and differentiating BCS from mastectomy. Such factors do play a role in the decision and may be contributing to greater use of mastectomy. Again, while survival and doctor recommendation remain the strongest drivers of patient choice they do not account for over 50% of the other factors influencing patient choice. Further, we found that the importance of any 1 issue is not held across all respondents. In other words, preference for any 1 choice is not held constant across all individuals—what is the right surgical choice for 1 woman may not be correct for another.
This study provides valuable evidence to address potential limitations of current patient education and presents an opportunity to empower patients to understand the choices available to ensure the decision-making process is shared between provider and patient.
The findings from our survey on attitudes and behaviors demonstrate that previous BC women put a greater priority on avoiding recurrence as compared with healthy women, reinforcing that women faced with BC may benefit from more education on recurrence risks before making a BC surgical treatment. Additionally, our data show that women are driven by financial concerns and will forgo preferred surgery based on ability to pay. Incorporating the importance of financial concerns, maintaining employment and out of pocket expenses were key factors in the decision-making process. Women are sophisticated in their decisions, and our data emphasize the need for providers to be cognizant of other drivers of choice and consider patient values in our approach to education. A better understanding of decision-making like cost, the intensity of treatment, expected recovery time, financial burden, and the impact of breast surgery on self-esteem, are critical to understanding the national trends, we are currently witnessing in patients’ surgical choices. By combining these factors with patient education, we can help better assist our patients to make informed decisions that are in line with their values and expectations.
Lastly, when key drivers like survival, doctor’s recommendation, and recurrence are held equal, the surgical choice remains quite heterogeneous among women, and there is no “one size fits all.” However, most (healthy women, 78.9%) and (previous BC, 80.7%) respondents preferred some form of cosmetic preservation, whether a simple oncoplastic approach to lumpectomy or reconstruction, reflecting improved patient awareness and empowerment. This finding is particularly relevant to all providers of BC care and reflects the importance of patient choice and quality of life as uniquely assessed by the individual. These data suggest that making decisions solely based on survival or doctor’s recommendation ignores many other factors women take into consideration. Thus, understanding the complicated, multifaceted, and patient-centric decision process is key to our ability to support and educate women undergoing cancer care.
Several limitations of the study are worth noting. First, the study represents a possible set of scenarios with a predefined set of factors that may not encompass all possible realities faced by BC patients. Second, the primary cohort consists of healthy women with a small subset of previous BC patients for face validity. Despite the use of healthy women, the results among the healthy women and previous BC patients were quite similar. Third, our study population was very homogeneous and may not be generalizable to all BC patients. The mean age of the respondents, both healthy women and previous BC patients, was 55 compared with the median age at diagnosis of 61 years old.2 The sample was also skewed toward the state of California ~16%, where the AoW is based, and predominantly Caucasian, despite California having a diverse racial and ethnic distribution. Future research is needed to ensure the findings of this study can be considered representative of the BC population. Lastly, the study was conducted as an English only web-based survey which may introduce selection bias regarding socioeconomic status, race, and ethnicity. To address all the described limitations, we hope to focus future efforts on patients during and just before the decision-making process. Also, future research should attempt to enhance the generalizability of these findings relevant to racial, ethnic, socioeconomic, and geographic distributions seen among the U.S. BC population.
Supplementary Material
Footnotes
Published online 20 April 2018.
Disclosure: This study was sponsored by LifeCell Corporation (an Allergan affiliate), Bridgewater, N.J. All authors met the ICMJE authorship criteria. Neither honoraria nor payments were made for authorship. Dr. Toni Storm-Dickerson is a speaker for Allergan and a consultant for Invuity. Dr. Allen Gabriel is a consultant for Allergan and Acelity. Dave Macarios is an employee of Allergan and owns stock or stock options. Lopamudra Das, Matthew Gitlin, and Jorge Farias received research funding from LifeCell Corporation (an Allergan affiliate). The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.ACS. Cancer Treatment & Survivorship Facts & Figures 2016–2017. 2016Atlanta, Ga.: American Cancer Society. [Google Scholar]
- 2.ACS. Surgery for breast cancer. 2016. Available at https://www.cancer.org/cancer/breast-cancer/treatment/surgery-for-breast-cancer.html.
- 3.NCCN. Updated NCCN guidelines for breast cancer discourages prophylactic mastectomy in women other than those at high risk. 2009. Available at http://www.nccn.org/about/news/newsinfo.asp?NewsID=226. Accessed 07-12, 2016.
- 4.Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–1241.. [DOI] [PubMed] [Google Scholar]
- 5.Kocak E, Carruthers KH, McMahan JD. A reliable method for the preoperative estimation of tissue to be removed during reduction mammaplasty. Plast Reconstr Surg. 2011;127:1059–1064.. [DOI] [PubMed] [Google Scholar]
- 6.Arora NK, Gustafson DH, Hawkins RP, et al. Impact of surgery and chemotherapy on the quality of life of younger women with breast carcinoma: a prospective study. Cancer. 2001;92:1288–1298.. [DOI] [PubMed] [Google Scholar]
- 7.Taylor KL, Lamdan RM, Siegel JE, et al. Treatment regimen, sexual attractiveness concerns and psychological adjustment among African American breast cancer patients. Psychooncology. 2002;11:505–517.. [DOI] [PubMed] [Google Scholar]
- 8.Waljee JF, Hu ES, Ubel PA, et al. Effect of esthetic outcome after breast-conserving surgery on psychosocial functioning and quality of life. J Clin Oncol. 2008;26:3331–3337.. [DOI] [PubMed] [Google Scholar]
- 9.Moxley JH, 3rd, Allegra JC, Henney J, et al. Treatment of primary breast cancer. Summary of the National Institutes of Health Consensus Development Conference. JAMA. 1980;244:797–800.. [DOI] [PubMed] [Google Scholar]
- 10.Fisher B, Wolmark N, Redmond C, et al. Findings from NSABP Protocol No. B-04: comparison of radical mastectomy with alternative treatments. II. The clinical and biologic significance of medial-central breast cancers. Cancer. 1981;48:1863–1872.. [DOI] [PubMed] [Google Scholar]
- 11.Fisher B, Bauer M, Margolese R, et al. Five-year results of a randomized clinical trial comparing total mastectomy and segmental mastectomy with or without radiation in the treatment of breast cancer. N Engl J Med. 1985;312:665–673.. [DOI] [PubMed] [Google Scholar]
- 12.Kummerow KL, Du L, Penson DF, et al. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg. 2015;150:9–16.. [DOI] [PubMed] [Google Scholar]
- 13.Tuttle TM, Habermann EB, Grund EH, et al. Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J Clin Oncol. 2007;25:5203–5209.. [DOI] [PubMed] [Google Scholar]
- 14.Women’s Health and Cancer Rights Act (WHCRA) required coverage for reconstructive surgery following mastectomies. 1998.
- 15.Collins ED, Moore CP, Clay KF, et al. Can women with early-stage breast cancer make an informed decision for mastectomy? J Clin Oncol. 2009;27:519–525.. [DOI] [PubMed] [Google Scholar]
- 16.Mastaglia B, Kristjanson LJ. Factors influencing women’s decisions for choice of surgery for Stage I and Stage II breast cancer in Western Australia. J Adv Nurs. 2001;35:836–847.. [DOI] [PubMed] [Google Scholar]
- 17.Benedict S, Cole DJ, Baron L, et al. Factors influencing choice between mastectomy and lumpectomy for women in the Carolinas. J Surg Oncol. 2001;76:6–12.. [DOI] [PubMed] [Google Scholar]
- 18.Nold RJ, Beamer RL, Helmer SD, et al. Factors influencing a woman’s choice to undergo breast-conserving surgery versus modified radical mastectomy. Am J Surg. 2000;180:413–418.. [DOI] [PubMed] [Google Scholar]
- 19.Molenaar S, Oort F, Sprangers M, et al. Predictors of patients’ choices for breast-conserving therapy or mastectomy: a prospective study. Br J Cancer. 2004;90:2123–2130.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goel V, Sawka CA, Thiel EC, et al. Randomized trial of a patient decision aid for choice of surgical treatment for breast cancer. Med Decis Making. 2001;21:1–6.. [DOI] [PubMed] [Google Scholar]
- 21.Green PE, Srinivasan V. Conjoint analysis in marketing: new developments with implications for research and practice. J Marketing. 1990:3–19.. [Google Scholar]
- 22.Kievit W, van Hulst L, van Riel P, et al. Factors that influence rheumatologists’ decisions to escalate care in rheumatoid arthritis: results from a choice-based conjoint analysis. Arthritis Care Res (Hoboken). 2010;62:842–847.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bederman SS, Mahomed NN, Kreder HJ, et al. In the eye of the beholder: preferences of patients, family physicians, and surgeons for lumbar spinal surgery. Spine (Phila Pa 1976). 2010;35:108–115.. [DOI] [PubMed] [Google Scholar]
- 24.Porzsolt F, Clouth J, Deutschmann M, et al. Preferences of diabetes patients and physicians: a feasibility study to identify the key indicators for appraisal of health care values. Health Qual Life Outcomes. 2010;8:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Lieshout EJ, de Vos R, Binnekade JM, et al. Decision making in interhospital transport of critically ill patients: national questionnaire survey among critical care physicians. Intensive Care Med. 2008;34:1269–1273.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.AoW. Army of women: history and FAQs. Available at https://researchers.armyofwomen.org/armyfaqresearchers. Accessed August 2017.
- 27.Bridges JF, Hauber AB, Marshall D, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14:403–413.. [DOI] [PubMed] [Google Scholar]
- 28.Litière S, Werutsky G, Fentiman IS, et al. Breast conserving therapy versus mastectomy for stage I-II breast cancer: 20 year follow-up of the EORTC 10801 phase 3 randomised trial. Lancet Oncol. 2012;13:412–419.. [DOI] [PubMed] [Google Scholar]
- 29.Blichert-Toft M, Nielsen M, Düring M, et al. Long-term results of breast conserving surgery vs. mastectomy for early stage invasive breast cancer: 20-year follow-up of the Danish randomized DBCG-82TM protocol. Acta Oncol. 2008;47:672–681.. [DOI] [PubMed] [Google Scholar]
- 30.Simone NL, Dan T, Shih J, et al. Twenty-five year results of the national cancer institute randomized breast conservation trial. Breast Cancer Res Treat. 2012;132:197–203.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347:1227–1232.. [DOI] [PubMed] [Google Scholar]
- 32.Arriagada R, Lê MG, Guinebretière JM, et al. Late local recurrences in a randomised trial comparing conservative treatment with total mastectomy in early breast cancer patients. Ann Oncol. 2003;14:1617–1622.. [DOI] [PubMed] [Google Scholar]
- 33.Group. EBCTC. Effects of radiotherapy and surgery in early breast cancer. An overview of the randomized trials. Early Breast Cancer Trialists’ Collaborative Group. New Engl J Med. 1995;333:1444–1455.. [DOI] [PubMed] [Google Scholar]
- 34.Jatoi I, Proschan MA. Randomized trials of breast-conserving therapy versus mastectomy for primary breast cancer: a pooled analysis of updated results. Am J Clin Oncol. 2005;28:289–294.. [DOI] [PubMed] [Google Scholar]
- 35.van der Hage JA, Putter H, Bonnema J, et al. ; EORTC Breast Cancer Group. Impact of locoregional treatment on the early-stage breast cancer patients: a retrospective analysis. Eur J Cancer. 2003;39:2192–2199.. [DOI] [PubMed] [Google Scholar]
- 36.Veronesi U, Salvadori B, Luini A, et al. Breast conservation is a safe method in patients with small cancer of the breast. Long-term results of three randomised trials on 1,973 patients. Eur J Cancer (Oxford, England: 1990). 1995;31A:1574–1579.. [DOI] [PubMed] [Google Scholar]
- 37.Arriagada R, Lê MG, Rochard F, et al. Conservative treatment versus mastectomy in early breast cancer: patterns of failure with 15 years of follow-up data. Institut Gustave-Roussy Breast Cancer Group. J Clin Oncol. 1996;14:1558–1564.. [DOI] [PubMed] [Google Scholar]
- 38.Fisher B, Anderson S, Redmond CK, et al. Reanalysis and results after 12 years of follow-up in a randomized clinical trial comparing total mastectomy with lumpectomy with or without irradiation in the treatment of breast cancer. N Engl J Med. 1995;333:1456–1461.. [DOI] [PubMed] [Google Scholar]
- 39.Jacobson JA, Danforth DN, Cowan KH, et al. Ten-year results of a comparison of conservation with mastectomy in the treatment of stage I and II breast cancer. N Engl J Med. 1995;332:907–911.. [DOI] [PubMed] [Google Scholar]
- 40.van Dongen JA, Voogd AC, Fentiman IS, et al. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst. 2000;92:1143–1150.. [DOI] [PubMed] [Google Scholar]
- 41.Laurberg T, Lyngholm C, Alsner P, et al. Long-term age dependent failure pattern after BCT vs. mastectomy in low-risk breast cancer patients. 2016, 2016Paper presented at: ESTRO. [DOI] [PubMed] [Google Scholar]
- 42.Liu YJ, Thomson JG. Ideal anthropomorphic values of the female breast: correlation of pluralistic aesthetic evaluations with objective measurements. Ann Plast Surg. 2011;67:7–11.. [DOI] [PubMed] [Google Scholar]
- 43.Margolis GJ, Goodman RL, Rubin A, et al. Psychological factors in the choice of treatment for breast cancer. Psychosomatics. 1989;30:192–197.. [DOI] [PubMed] [Google Scholar]
- 44.Celaya MO, Rees JR, Gibson JJ, et al. Travel distance and season of diagnosis affect treatment choices for women with early-stage breast cancer in a predominantly rural population (United States). Cancer Causes Control. 2006;17:851–856.. [DOI] [PubMed] [Google Scholar]
- 45.Johnson RM, Orme BK. How many questions should you ask in choice-based conjoint studies. 1996.
- 46.Orme B. Getting Started with Conjoint Analysis: Strategies for Product Design and Pricing Research. 2006Research Publ. Llc.. [Google Scholar]


